Sonoanatomy and Stepwise/Systematic Ultrasound Examination of the Extrinsic/Intrinsic Wrist Ligaments
Abstract
:1. Introduction
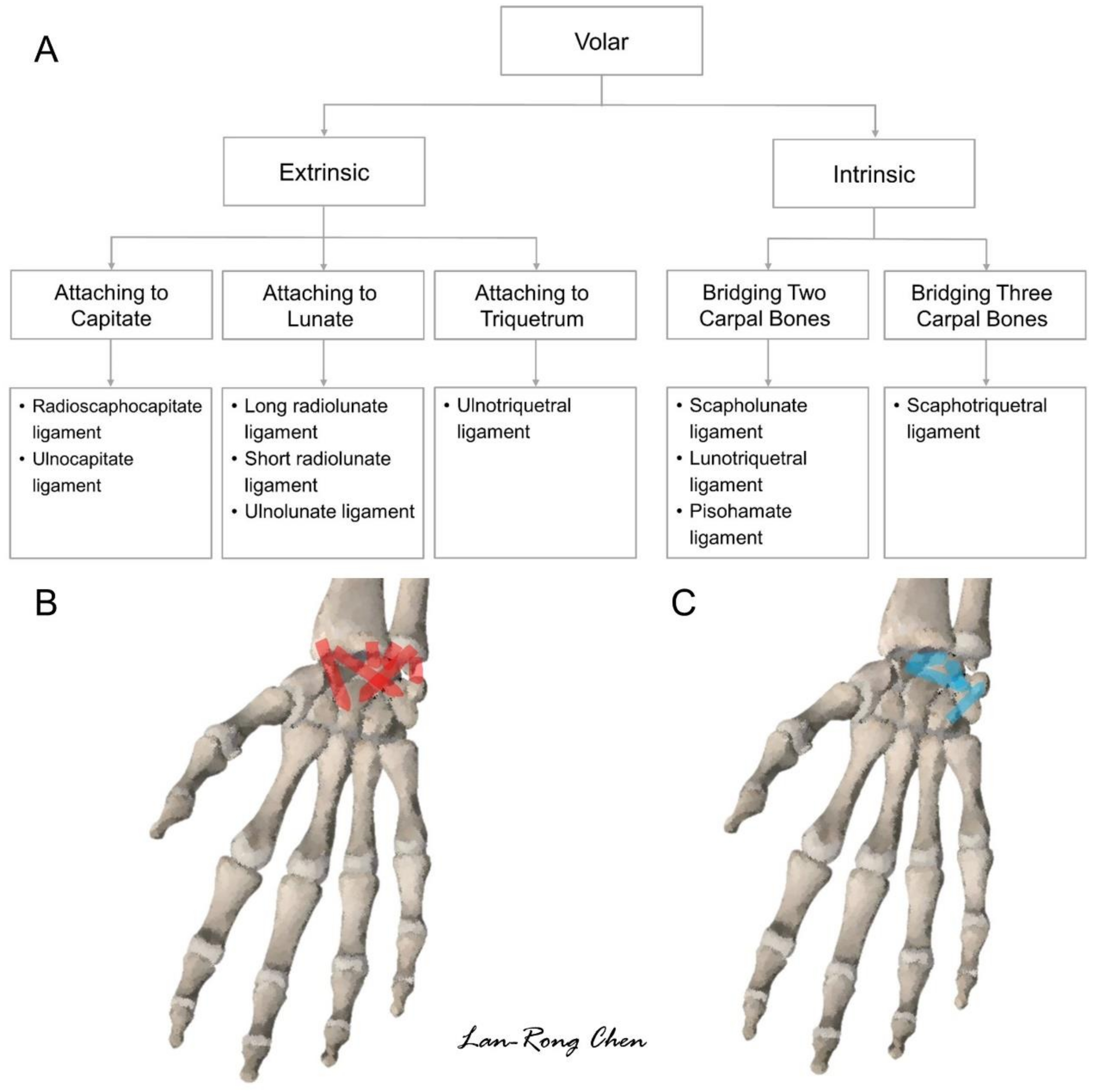
2. Sonoanatomy of Carpal Bones
3. Sonoanatomy of Volar Extrinsic Carpal Ligaments
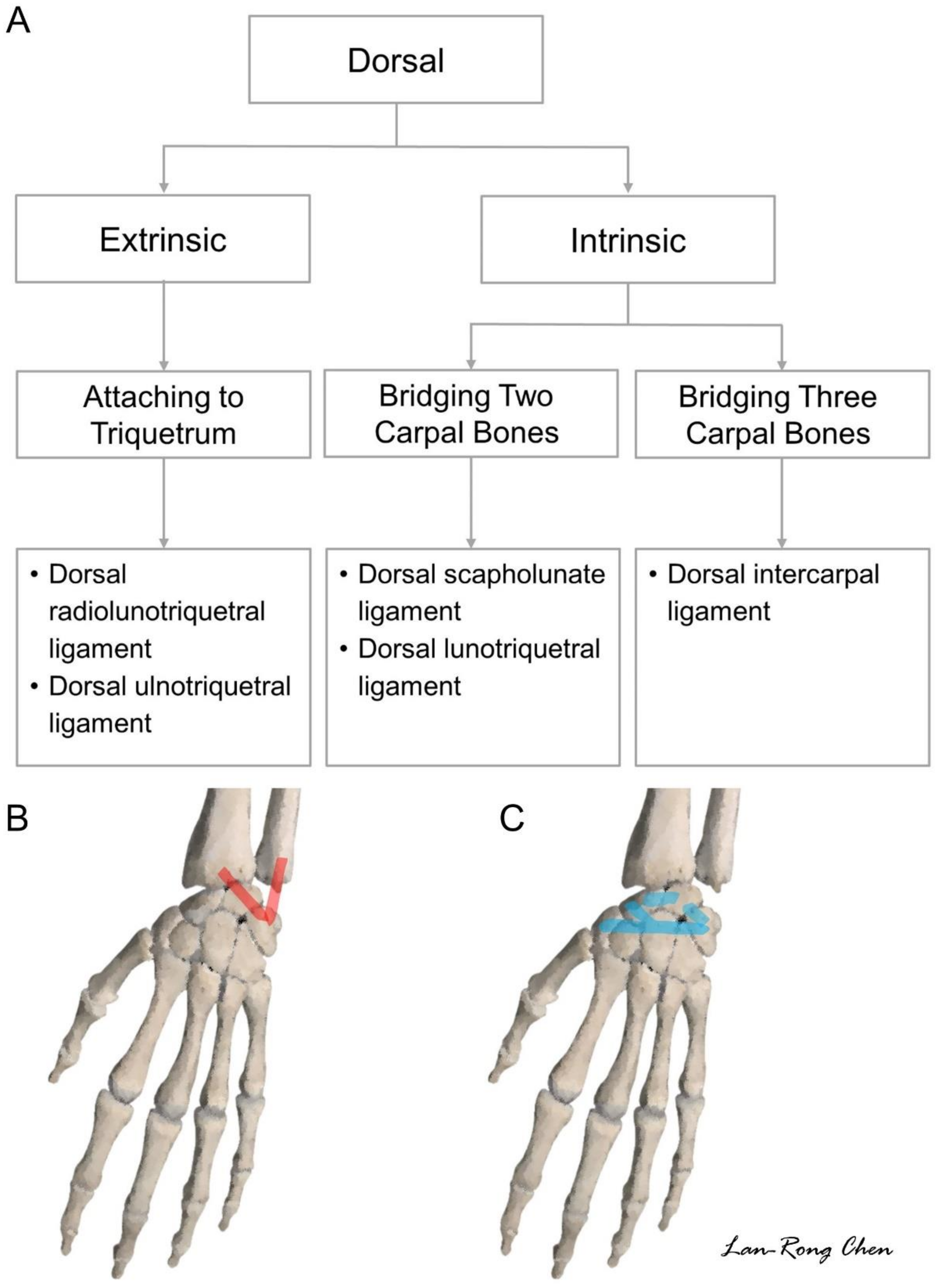
3.1. Attachment to the Capitate
3.2. Attachment to the Lunate
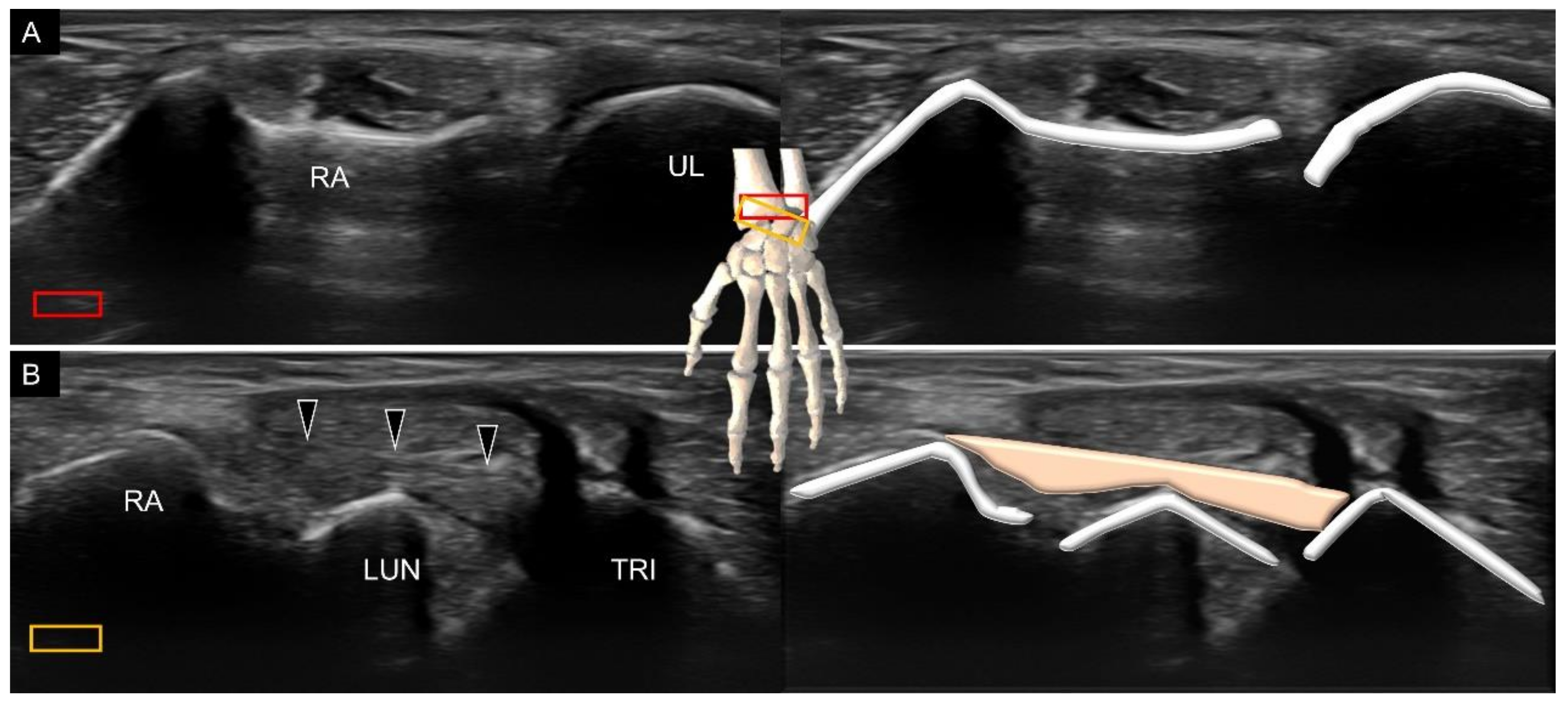
3.3. Attachment to the Triquetrum
4. Sonoanatomy of Volar Intrinsic Carpal Ligaments
5. Sonoanatomy of Dorsal Extrinsic Carpal Ligaments
Attachment to the Triquetrum
6. Sonoanatomy of Dorsal Intrinsic Carpal Ligaments
7. Sonoanatomy of Wrist Collateral Ligaments
8. Pathology
9. Strength and Limitation of the Present Article
10. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hung, C.Y.; Chang, K.V.; Ozcakar, L. Dynamic and Doppler Ultrasound Imaging for the Diagnosis of Triangular Fibrocartilage Complex Injury and Ulnocarpal Wrist Instability. Am. J. Phys. Med. Rehabil. 2016, 95, e111–e112. [Google Scholar] [CrossRef]
- Chang, K.V.; Hung, C.Y.; Ozcakar, L. Snapping Thumb and Superficial Radial Nerve Entrapment in De Quervain Disease: Ultrasound Imaging/Guidance Revisited. Pain Med. 2015, 16, 2214–2215. [Google Scholar] [CrossRef]
- Chang, K.V.; Hung, C.Y.; Ozcakar, L. Ultrasound imaging for precise diagnosis and injection of isolated extensor pollicis brevis tenosynovitis: It is not always a simple de Quervain disease. Am. J. Phys. Med. Rehabil. 2015, 94, 255. [Google Scholar] [CrossRef]
- Lin, M.T.; Chang, K.V.; Wu, W.T.; Ozcakar, L. Postfracture loss of extension of the interphalangeal joint of the right thumb: What can a musculoskeletal ultrasound tell us? J. Res. Med. Sci. 2020, 25, 2. [Google Scholar] [CrossRef]
- Chang, K.V.; Hung, C.Y.; Ozcakar, L. Ultrasound imaging for the extensor pollicis brevis tendon: When martial arts caused partial rupture. Am. J. Phys. Med. Rehabil. 2015, 94, e22. [Google Scholar] [CrossRef] [PubMed]
- Ozcakar, L.; Kara, M.; Chang, K.V.; Carl, A.B.; Akkaya, N.; Tok, F.; Chen, W.S.; Wang, T.G.; Tekin, L.; Ulasl, A.M.; et al. Nineteen reasons why physiatrists should do musculoskeletal ultrasound: EURO-MUSCULUS/USPRM recommendations. Am. J. Phys. Med. Rehabil. 2015, 94, e45–e49. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Thukral, C.L.; Gupta, K. Tendo-ligamentous pathologies of the wrist joint: Can ultrasonography replace magnetic resonance imaging? Egypt. J. Radiol. Nucl. Med. 2017, 48, 653–660. [Google Scholar] [CrossRef]
- Ozcakar, L.; Kara, M.; Chang, K.V.; Ulasli, A.M.; Hung, C.Y.; Tekin, L.; Wu, C.H.; Tok, F.; Hsiao, M.Y.; Akkaya, N.; et al. EURO-MUSCULUS/USPRM Basic Scanning Protocols for wrist and hand. Eur J. Phys. Rehabil. Med. 2015, 51, 479–484. [Google Scholar]
- Chang, K.V.; Mezian, K.; Nanka, O.; Wu, W.T.; Lou, Y.M.; Wang, J.C.; Martinoli, C.; Ozcakar, L. Ultrasound Imaging for the Cutaneous Nerves of the Extremities and Relevant Entrapment Syndromes: From Anatomy to Clinical Implications. J. Clin. Med. 2018, 7, 457. [Google Scholar] [CrossRef] [Green Version]
- Wu, W.T.; Chang, K.V.; Mezian, K.; Nanka, O.; Yang, Y.C.; Hsu, Y.C.; Hsu, P.C.; Ozcakar, L. Ulnar Wrist Pain Revisited: Ultrasound Diagnosis and Guided Injection for Triangular Fibrocartilage Complex Injuries. J. Clin. Med. 2019, 8, 1540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beeker, R.W.; Rehman, U.H. Carpal Ligament Instability. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2021. [Google Scholar]
- Boutry, N.; Lapegue, F.; Masi, L.; Claret, A.; Demondion, X.; Cotten, A. Ultrasonographic evaluation of normal extrinsic and intrinsic carpal ligaments: Preliminary experience. Skelet. Radiol. 2005, 34, 513–521. [Google Scholar] [CrossRef]
- Taljanovic, M.S.; Goldberg, M.R.; Sheppard, J.E.; Rogers, L.F. US of the intrinsic and extrinsic wrist ligaments and triangular fibrocartilage complex--normal anatomy and imaging technique. Radiographics 2011, 31, e44. [Google Scholar] [CrossRef] [Green Version]
- Helms, J.T.; Maldonado, K.A.; Burns, B. Anatomy, Shoulder and Upper Limb, Hand Radiocarpal Joint. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2021. [Google Scholar]
- Gitto, S.; Messina, C.; Mauri, G.; Aliprandi, A.; Sardanelli, F.; Sconfienza, L.M. Dynamic high-resolution ultrasound of intrinsic and extrinsic ligaments of the wrist: How to make it simple. Eur. J. Radiol. 2017, 87, 20–35. [Google Scholar] [CrossRef] [PubMed]
- Gitto, S.; Draghi, F. Normal Sonographic Anatomy of the Wrist With Emphasis on Assessment of Tendons, Nerves, and Ligaments. J. Ultrasound Med. 2016, 35, 1081–1094. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.A.; Landsmeer, J.M. The palmar radiocarpal ligaments: A study of adult and fetal human wrist joints. J. Hand Surg. 1990, 15, 847–854. [Google Scholar] [CrossRef] [Green Version]
- Bianchi, S.; Beaulieu, J.Y.; Poletti, P.A. Ultrasound of the ulnar-palmar region of the wrist: Normal anatomy and anatomic variations. J. Ultrasound 2020, 23, 365–378. [Google Scholar] [CrossRef] [PubMed]
- Sennwald, G.R.; Zdravkovic, V.; Oberlin, C. The anatomy of the palmar scaphotriquetral ligament. J. Bone Jt. Surgery. Br. Vol. 1994, 76, 147–149. [Google Scholar] [CrossRef]
- Mitsuyasu, H.; Patterson, R.M.; Shah, M.A.; Buford, W.L.; Iwamoto, Y.; Viegas, S.F. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J. Hand Surg. 2004, 29, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Türker, T.; Sheppard, J.E.; Klauser, A.S.; Johnston, S.S.; Amerongen, H.; Taljanovic, M.S. The radial and ulnar collateral ligaments of the wrist are true ligaments. Diagn. Interv. Radiol. 2019, 25, 473–479. [Google Scholar] [CrossRef]
- Yang, Y.C.; Wu, W.T.; Chang, K.V.; Ozcakar, L. Ultrasonographic Imaging of Entrapment of the Palmar Cutaneous Branch of the Ulnar Nerve due to Accessory Abductor Digiti Minimi Muscle. Am. J. Phys. Med. Rehabil. 2020, 99, e136–e137. [Google Scholar] [CrossRef]
- Grimshaw, L.-A. Scanning the wrist for ligament injuries. Ultrasound Med. Biol. 2019, 45, S75–S76. [Google Scholar] [CrossRef]
- Freire, V.; Guérini, H.; Campagna, R.; Moutounet, L.; Dumontier, C.; Feydy, A.; Drapé, J.-L. Imaging of Hand and Wrist Cysts: A Clinical Approach. Am. J. Roentgenol. 2012, 199, W618–W628. [Google Scholar] [CrossRef] [PubMed]
- Margulies, I.G.; Xu, H.; Gopman, J.M.; Freeman, M.D.; Dayan, E.; Taub, P.J.; Melamed, E. Narrative Review of Ligamentous Wrist Injuries. J. Hand Microsurg. 2021, 13, 55–64. [Google Scholar] [CrossRef]
- Ricci, V.; Özçakar, L. Ultrasound Imaging for Dorsal Radiolunotriquetral Ligament Possibly Causing Wrist Impingement. Am. J. Phys. Med. Rehabil. 2019, 98, e17. [Google Scholar] [CrossRef] [PubMed]


















Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.-C.; Wu, W.-T.; Chang, K.-V.; Chen, L.-R.; Nakashima, Y.; Özçakar, L. Sonoanatomy and Stepwise/Systematic Ultrasound Examination of the Extrinsic/Intrinsic Wrist Ligaments. Diagnostics 2021, 11, 1834. https://doi.org/10.3390/diagnostics11101834
Wang J-C, Wu W-T, Chang K-V, Chen L-R, Nakashima Y, Özçakar L. Sonoanatomy and Stepwise/Systematic Ultrasound Examination of the Extrinsic/Intrinsic Wrist Ligaments. Diagnostics. 2021; 11(10):1834. https://doi.org/10.3390/diagnostics11101834
Chicago/Turabian StyleWang, Jia-Chi, Wei-Ting Wu, Ke-Vin Chang, Lan-Rong Chen, Yuko Nakashima, and Levent Özçakar. 2021. "Sonoanatomy and Stepwise/Systematic Ultrasound Examination of the Extrinsic/Intrinsic Wrist Ligaments" Diagnostics 11, no. 10: 1834. https://doi.org/10.3390/diagnostics11101834
APA StyleWang, J.-C., Wu, W.-T., Chang, K.-V., Chen, L.-R., Nakashima, Y., & Özçakar, L. (2021). Sonoanatomy and Stepwise/Systematic Ultrasound Examination of the Extrinsic/Intrinsic Wrist Ligaments. Diagnostics, 11(10), 1834. https://doi.org/10.3390/diagnostics11101834







