Spontaneous Bladder Rupture after Normal Vaginal Delivery: Description of a Rare Complication and Systematic Review of the Literature
Abstract
:1. Introduction
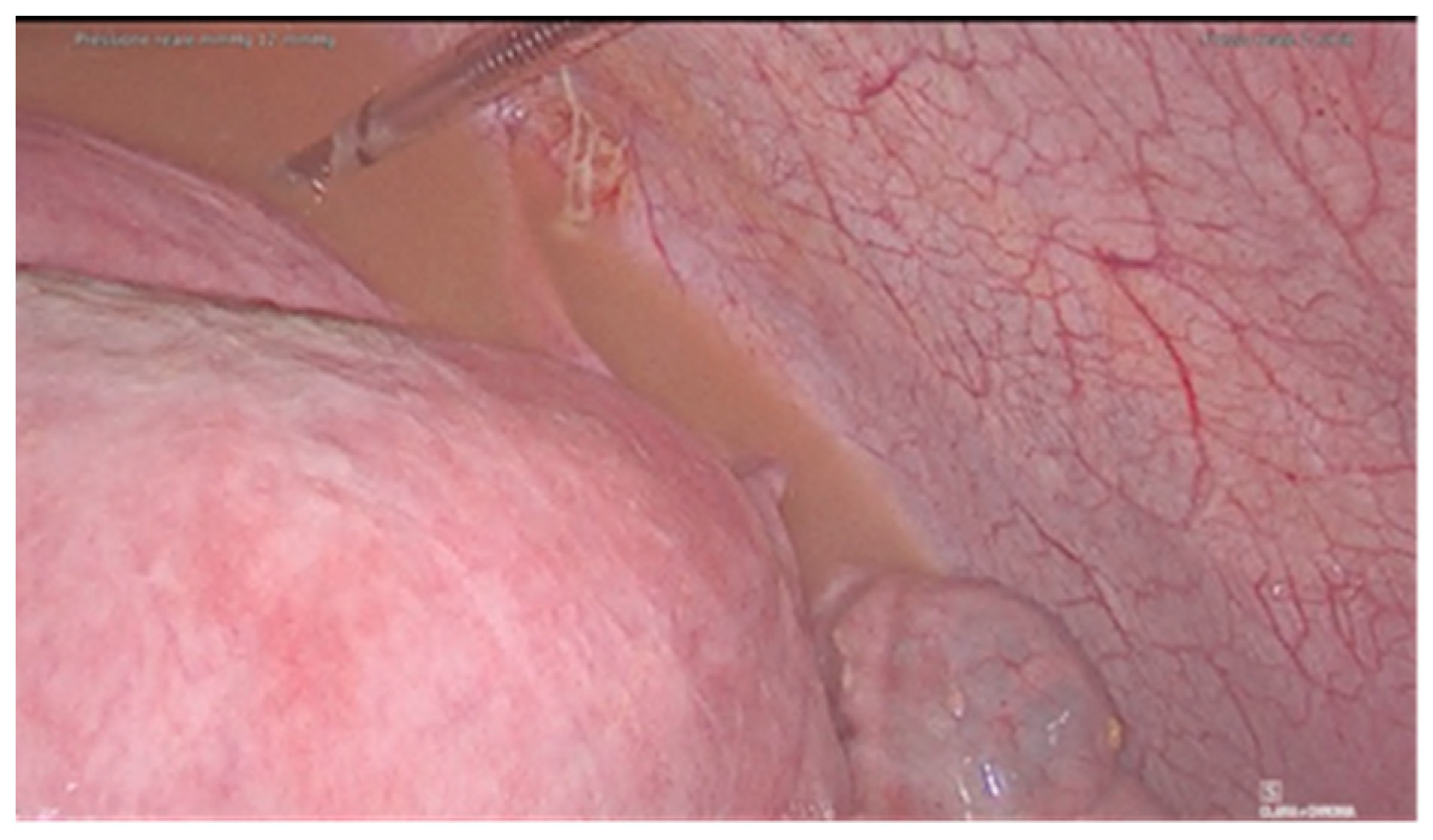
2. Case
3. Materials and Methods
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| D1. | Were patient’s demographic characteristics clearly described? |
| D2. | Was the patient’s history clearly described and presented as a timeline? |
| D3. | Was the current clinical condition of the patient on presentation clearly described? |
| D4. | Were diagnostic tests or assessment methods and the results clearly described? |
| D5. | Was the intervention(s) or treatment procedure(s) clearly described? |
| D6. | Was the post-intervention clinical condition clearly described? |
| D7. | Were adverse events (harms) or unanticipated events identified and described? |
| D8. | Does the case report provide takeaway lessons? |
References
- Farahzadi, A.; Mohammadipour, S. A Late Presentation of Spontaneous Bladder Rupture During Labor. Urol. Case Rep. 2016, 8, 24–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hadian, B.; Nazarpoor, S.; Garshasebi, M.; Mohtashami, A.Z. Missed bladder rupture following vaginal delivery: Possible role of assessing ascitic fluid creatinine levels? Clin. Case Rep. 2020, 8, 1247–1250. [Google Scholar] [CrossRef] [PubMed]
- Wandabwa, J.; Otim, T.; Kiondo, P. Spontaneous rupture of bladder in puerperium. Afr. Health Sci. 2004, 4, 138–139. [Google Scholar]
- Mark, A.; Meister, M.; Opara, B.; Chow, R. Nontraumatic urinary bladder rupture presenting as renal pseudo-failure and ascites. Radiol. Case Rep. 2017, 12, 304–307. [Google Scholar] [CrossRef]
- Faraj, R.; O’Donovan, P.; Jones, A.; Hill, S. Spontaneous rupture of urinary bladder in second trimester of pregnancy: A case report. Aust. N. Z. J. Obstet. Gynaecol. 2008, 48, 520. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Prospero International Prospective Register of Systematic Reviews. Available online: https://www.crd.york.ac.uk/prospero/ (accessed on 9 October 2020).
- Roberts, C.; Oligbo, N.; Swinhoe, J. Spontaneous bladder rupture following normal vaginal delivery: A postpartum emergency. BJOG Int. J. Obstet. Gynaecol. 1996, 103, 381–382. [Google Scholar] [CrossRef] [PubMed]
- Puri, M.; Pathania, O.P.; Pasrija, S.; Dholakia, M. Asymptomatic bladder rupture in a primigravida: Late manifestation and delayed diagnosis. Aust. N. Z. J. Obstet. Gynaecol. 2005, 45, 535–536. [Google Scholar] [CrossRef]
- Pal, D.K.; Bag, A.K. Spontaneous rupture of urinary bladder in puerperium. Indian J. Surg. 2005, 67, 325. [Google Scholar]
- Dueñas-García, O.F.; Rico, H.; Gorbea-Sanchez, V.; Herrerias-Canedo, T. Bladder Rupture Caused by Postpartum Urinary Retention. Obstet. Gynecol. 2008, 112, 481–482. [Google Scholar] [CrossRef]
- Png, K.S.; Chong, Y.L.; Ng, C.K. Two cases of intraperitoneal bladder rupture following vaginal delivery. Singap. Med. J. 2008, 49, e327–e329. [Google Scholar] [CrossRef]
- Sahoo, R.K.; Sabat, D.K.; Panigrahi, P.K.; Acharya, M.; Sahu, M.C. Spontaneous puerperal extraperitoneal bladder wall rupture in young woman with diagnostic dilemma. J. Fam. Med. Prim. Care 2015, 4, 601–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habek, D.; Marton, I.; Luetic, A.T.; Prka, M.; Kuljak, Z.; Živković, K.; Cenkovčan, M.; Mazuran, B. Acute Abdomen Syndrome Due To Spontaneous Intraperitoneal Bladder Rupture Following Vaginal Delivery. Z. Geburtshilfe Neonatol. 2017, 222, 34–36. [Google Scholar] [CrossRef] [PubMed]
- Qiao, P.; Tian, D.; Bao, Q. Delayed diagnosis of spontaneous bladder rupture: A rare case report. BMC Women’s Health 2018, 18, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekuma-Nkama, E.N.; Garg, V.K.; Barayan, S. Spontaneous rupture of bladder in a primipara. Ann. Saudi Med. 1997, 17, 646–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barroso, F.M.D.S.; Maués, C.A.D.; de Castro, G.L.; Alves, R.A.D.C.; de Vasconcelos, E.L.C.; Clair, J.P.G.S. Surgical management of spontaneous post-partum bladder rupture in an Amazonian emergency hospital. Urol. Case Rep. 2020, 33, 101376. [Google Scholar] [CrossRef] [PubMed]
- Dammann, H.G.; Hagemann, J.; Runge, M. In vivo diagnosis of massive hepatic infarction by computed tomography. Dig. Dis. Sci. 1982, 27, 73–79. [Google Scholar] [CrossRef]
- Gyang, A.; Kalu, E.; Fakokunde, A.; Whitlow, B. Ascites in the puerperium: A missed diagnosis of acute postpartum pancreatitis. Arch. Gynecol. Obstet. 2005, 272, 238–240. [Google Scholar] [CrossRef] [PubMed]
- Albareda, J.; Albi, M.V.; Sosa, G.; Cano, A.; Macello, M.E.; Martin, B.A. Puerperal ileal perforation secondary to endometriosis: Case report and literature review. Taiwan. J. Obstet. Gynecol. 2016, 55, 121–124. [Google Scholar] [CrossRef] [Green Version]
- Aksoy, H.; Özyurt, S.; Aksoy, Ü.; Açmaz, G.; Karadag, O.I.; Karadag, M.A. Ovarian torsion in puerperium: A case report and review of the literature. Int. J. Surg. Case Rep. 2014, 5, 1074–1076. [Google Scholar] [CrossRef] [Green Version]
- Muneer, M.; Abdelrahman, H.; El-Menyar, A.; Zarour, A.; Awad, A.; Al-Thani, H. Spontaneous Atraumatic Urinary Bladder Rupture Secondary to Alcohol Intoxication: A Case Report and Review of Literature. Am. J. Case Rep. 2015, 16, 778–781. [Google Scholar] [CrossRef] [Green Version]
- Mischianu, D.; Bratu; Ilie, C.; Madan, V. Notes concerning the peritonitis of urinary aetiology. J. Med. Life 2008, 1, 66–71. Available online: http://www.ncbi.nlm.nih.gov/pubmed/20108482 (accessed on 7 May 2020).
- Heyns, C.F.; Rimington, P.D. Intraperitoneal Rupture of the Bladder Causing the Biochemical Features of Renal Failure. Br. J. Urol. 1987, 60, 217–222. [Google Scholar] [CrossRef]
- Dees, A.; Kluchert, S.A.; Van Vliet, A.C. Pseudo-renal failure associated with internal leakage of urine. Neth. J. Med. 1990, 37, 197–201. Available online: http://europepmc.org/abstract/MED/2074911 (accessed on 7 May 2020).
- Kibel, A.S.; Staskin, D.R.; Grigoriev, V.E. Intraperitoneal Bladder Rupture After Normal Vaginal Delivery. J. Urol. 1995, 153, 725–727. [Google Scholar] [CrossRef]
- Markou, G.; Metaxas, G.; Vautier-Rit, S.; Muray, J.-M.; Poncelet, C. Découverte d’une rupture de la vessie dans le post-partum immédiat. Quel est l’intérêt du dosage de la créatininémie? Gynécol. Obs. Fertil. 2016, 44, 607–608. [Google Scholar] [CrossRef] [PubMed]
- Jambet, S.; Facy, O.; Landreau, P.; Duperron, C.; Kretz, B. Intraperitoneal Rupture of the Bladder after Urinary Catheterization. Clin. Pr. 2011, 1, 239. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Convie, L.; Mark, M.; McClure, M. An unusual cause of abdominal distension: Intraperitoneal bladder perforation secondary to intermittent self-catheterisation. BMJ Case Rep. 2015, 2015, bcr2014207097. [Google Scholar] [CrossRef] [Green Version]
- Pifarotti, P.; Gargasole, C.; Folcini, C.; Gattei, U.; Nieddu, E.; Sofi, G.; Buonaguidi, A.; Meschia, M. Acute post-partum urinary retention: Analysis of risk factors, a case–control study. Arch. Gynecol. Obstet. 2014, 289, 1249–1253. [Google Scholar] [CrossRef] [PubMed]
- Zetterström, J.; López, A.; Anzén, B.; Norman, M.; Holmström, B.; Mellgren, A. Anal sphincter tears at vaginal delivery: Risk factors and clinical outcome of primary repair. Obstet. Gynecol. 1999, 94, 21–28. [Google Scholar] [CrossRef]
- Sartore, A.; De Seta, F.; Maso, G.; Ricci, G.; Alberico, S.; Borelli, M.; Guaschino, S. The effects of uterine fundal pressure (Kristeller maneuver) on pelvic floor function after vaginal delivery. Arch. Gynecol. Obstet. 2012, 286, 1135–1139. [Google Scholar] [CrossRef] [PubMed]
- Kane, N.M.; Francis, I.R.; Ellis, J.H. The value of CT in the detection of bladder and posterior urethral injuries. Am. J. Roentgenol. 1989, 153, 1243–1246. [Google Scholar] [CrossRef] [Green Version]
- Muggia, R.A.; Mowschenson, P.; Chopra, S. Urinary ascites in the immediate postpartum period. Am. J. Gastroenterol. 1992, 87, 1196–1197. [Google Scholar] [PubMed]
- Corriere, J.N. Trauma to the Lower Urinary Tract, 2nd ed.; Adult and Pediatric Urology; Gillenwater, J.Y., Grayhack, J.T., Howards, S.S., Mitchell, M.E., Eds.; Year Book Medical: Philadelphia, PA, USA, 1991; pp. 501–503. [Google Scholar]
- Stabile, G.; Zinicola, G.; Romano, F.; Buonomo, F.; Mangino, F.P.; Ricci, G. Management of Non-Tubal Ectopic Pregnancies: A Single Center Experience. Diagnostics 2020, 10, 652. [Google Scholar] [CrossRef] [PubMed]
- Gomel, V. From laparotomy to laparoscopy to in vitro fertilization. Fertil. Steril. 2019, 112, 183–196. [Google Scholar] [CrossRef]
- Milingos, S.D.; Kallipolitis, G.K.; Loutradis, D.C.; Liapi, A.G.; Hassan, E.A.; Mavrommatis, C.G.; Miaris, S.G.; Michalas, S.P. Laparoscopic Treatment of Hydrosalpinx: Factors Affecting Pregnancy Rate. J. Am. Assoc. Gynecol. Laparosc. 2000, 7, 355–361. [Google Scholar] [CrossRef]
- Ryan, G.B.; Grobéty, J.; Majno, G. Postoperative peritoneal adhesions. A study of the mechanisms. Am. J. Pathol. 1971, 65, 117–148. Available online: https://pubmed.ncbi.nlm.nih.gov/5315369 (accessed on 7 May 2020). [PubMed]
- Romano, F.; Rizzo, M.; Stabile, G.; Di Lorenzo, G.; Liguori, G.; Trombetta, C.; Ricci, G. Laparoscopic and laparotomic guided ureteral stenting during gynecological surgery without use of imaging: Safety and feasibility in a single institutional case series. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 251, 125–128. [Google Scholar] [CrossRef] [PubMed]





| Title | Author, Year | D1 | D2 | D3 | D4 | D5 | D6 | D7 | D8 |
|---|---|---|---|---|---|---|---|---|---|
| Spontaneous bladder rupture after normal vaginal delivery: a postpartum emergency [8] | Roberts C et al., 1996 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Spontaneous rupture of bladder in puerperium [3] | Wandabwa J et al., 2004 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Asymptomatic bladder rupture in a primigravida: late manifestation and delayed diagnosis [9] | Puri M et al., 2005 | No | Yes | Yes | Yes | Unclear | Unclear | Yes | Unclear |
| Spontaneous rupture of urinary bladder in puerperium [10] | Pal DK et al., 2005 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Bladder rupture caused by postpartum urinary retention [11] | Dueñas-García OF et al., 2008 | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Two cases of intraperitoneal bladder rupture following vaginal delivery [12] | Png KS et al., 2008 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Spontaneous puerperal extraperitoneal bladder wall rupture in young woman with diagnostic dilemma [13] | Sabat D et al., 2015 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| A late presentation of spontaneous bladder rupture during labor [1] | Farahzadi A et al., 2016 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Acute abdomen syndrome due to spontaneous intraperitoneal bladder rupture following vaginal delivery [14] | Habek D et al., 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Delayed diagnosis of spontaneous bladder rupture: a rare case report [15] | Qiao D et al., 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Spontaneous rupture of bladder in a primipara [16] | Ekuma-Nkama EN et al., 2019 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Surgical management of spontaneous post-partum bladder rupture in an Amazonian emergency hospital [17] | Marcos da Silva Barroso F et al., 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Missed bladder rupture following vaginal delivery: Possible role of assessing ascitic fluid creatinine levels? [2] | Hadian B et al., 2020 | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes |
| Title | Author, Year | Age | Time to Rupture (Days) | Baby Weight (g) | Parity (Postpartum) | Type of Delivery | Previous Surgery | Catheterization | Catheterization during Labor | Symptoms | Diagnosis | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spontaneous bladder rupture after normal vaginal delivery: a postpartum emergency [8] | Roberts C et al., 1996 | 29 | 3 | 3400 | 2 | VD | No | Yes | NA | Increasing abdominal pain | XR + catheterization + LPT | LPT |
| Spontaneous rupture of bladder in puerperium [3] | Wandabwa J et al., 2004 | 20 | 9 | 2800 | 1 | VD | NA | Yes | NA | Severe lower abdominal pain, abdominal distension, fever, difficulty in breathing | US + LPT | LPT |
| Asymptomatic bladder rupture in a primigravida: late manifestation and delayed diagnosis [9] | Puri M et al., 2005 | NA | 4 | NA | NA | VD | NA | NA | NA | Urinary Retention, abdominal distension | XR + cystogram + LPT | LPT |
| Spontaneous rupture of urinary bladder in puerperium [10] | Pal DK et al., 2005 | 23 | 1 | NA | 1 | VD | None | Yes | NA | Distended abdomen, vomiting and ol- iguria | CT + cystography + LPT | LPT |
| Bladder rupture caused by postpartum urinary retention [11] | Dueñas-García OF et al., 2008 | NA | 3 | NA | 1 | VD | NA | Yes | NA | Abdominal pain, oliguria, hematuria | XR + US + LPT | LPT |
| Two cases of intraperitoneal bladder rupture following vaginal delivery [12] | Png KS et al., 2008 | 34 | 2 | 2685 | 1 | VD | NA | Yes | NA | Abdominal distension, acute renal failure | XR + CT + LPT | LPT |
| Spontaneous puerperal extraperitoneal bladder wall rupture in young woman with diagnostic dilemma [13] | Sabat D et al., 2015 | 20 | 6 | 2830 | NA | VD | NA | Yes | Yes | Abdominal pain and distension, oliguria | Paracentesis, US, CT, LPT | LPT |
| A late presentation of spontaneous bladder rupture during labor [1] | Farahzadi A et al., 2016 | 25 | 20 | NA | 1 | VD | NA | Yes | Yes | Abdominal pain and distension | US + LPT | LPT |
| Acute abdomen syndrome due to spontaneous intraperitoneal bladder rupture following vaginal delivery [14] | Habek D et al., 2017 | 28 | 4 | 3350 | 1 | VD | NA | Yes | Yes | Acute abdomen syndrome, diarrhea and oedema | US + CT + LPT | LPT |
| Delayed diagnosis of spontaneous bladder rupture: a rare case report [15] | Qiao D et al., 2018 | 23 | 5 | 3600 | 2 | VD | NA | Yes | NA | Fever, oliguria, massive ascites | US, MRI, CT, cystoradiography and cystoscopy, LPT | LPT |
| Spontaneous rupture of bladder in a primipara [16] | Ekuma-Nkama EN et al., 2019 | 30 | 3 | 3254 | 1 | VD | NA | Yes | Yes | Severe abdominal pain, oliguria and hematuria | XR + US + LPT | LPT |
| Surgical management of spontaneous post-partum bladder rupture in an Amazonian emergency hospital [17] | Marcos da Silva Barroso F et al., 2020 | 30 | 3 | 3200 | 2 | VD | No | NA | NA | Sudden abdominal pain, vomiting | US + CT + LPT | LPT |
| Missed bladder rupture following vaginal delivery: Possible role of assessing ascitic fluid creatinine levels? [2] | Hadian B et al., 2020 | 27 | 3 | NA | 1 | VD | No | NA | NA | Drowsiness and abdominal distention | CT + LPT | LPT |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stabile, G.; Cracco, F.; De Santo, D.; Zinicola, G.; Romano, F.; De Manzini, N.; Scomersi, S.; Ricci, G. Spontaneous Bladder Rupture after Normal Vaginal Delivery: Description of a Rare Complication and Systematic Review of the Literature. Diagnostics 2021, 11, 1885. https://doi.org/10.3390/diagnostics11101885
Stabile G, Cracco F, De Santo D, Zinicola G, Romano F, De Manzini N, Scomersi S, Ricci G. Spontaneous Bladder Rupture after Normal Vaginal Delivery: Description of a Rare Complication and Systematic Review of the Literature. Diagnostics. 2021; 11(10):1885. https://doi.org/10.3390/diagnostics11101885
Chicago/Turabian StyleStabile, Guglielmo, Francesco Cracco, Davide De Santo, Giulia Zinicola, Federico Romano, Nicolò De Manzini, Serena Scomersi, and Giuseppe Ricci. 2021. "Spontaneous Bladder Rupture after Normal Vaginal Delivery: Description of a Rare Complication and Systematic Review of the Literature" Diagnostics 11, no. 10: 1885. https://doi.org/10.3390/diagnostics11101885
APA StyleStabile, G., Cracco, F., De Santo, D., Zinicola, G., Romano, F., De Manzini, N., Scomersi, S., & Ricci, G. (2021). Spontaneous Bladder Rupture after Normal Vaginal Delivery: Description of a Rare Complication and Systematic Review of the Literature. Diagnostics, 11(10), 1885. https://doi.org/10.3390/diagnostics11101885








