A Preliminary Study on the Prognostic Impact of Neutrophil to Lymphocyte Ratio of the Bronchoalveolar Lavage Fluid in Patients with Lung Cancer
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Data Collection
2.3. Bronchoalveolar Lavage Processing
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
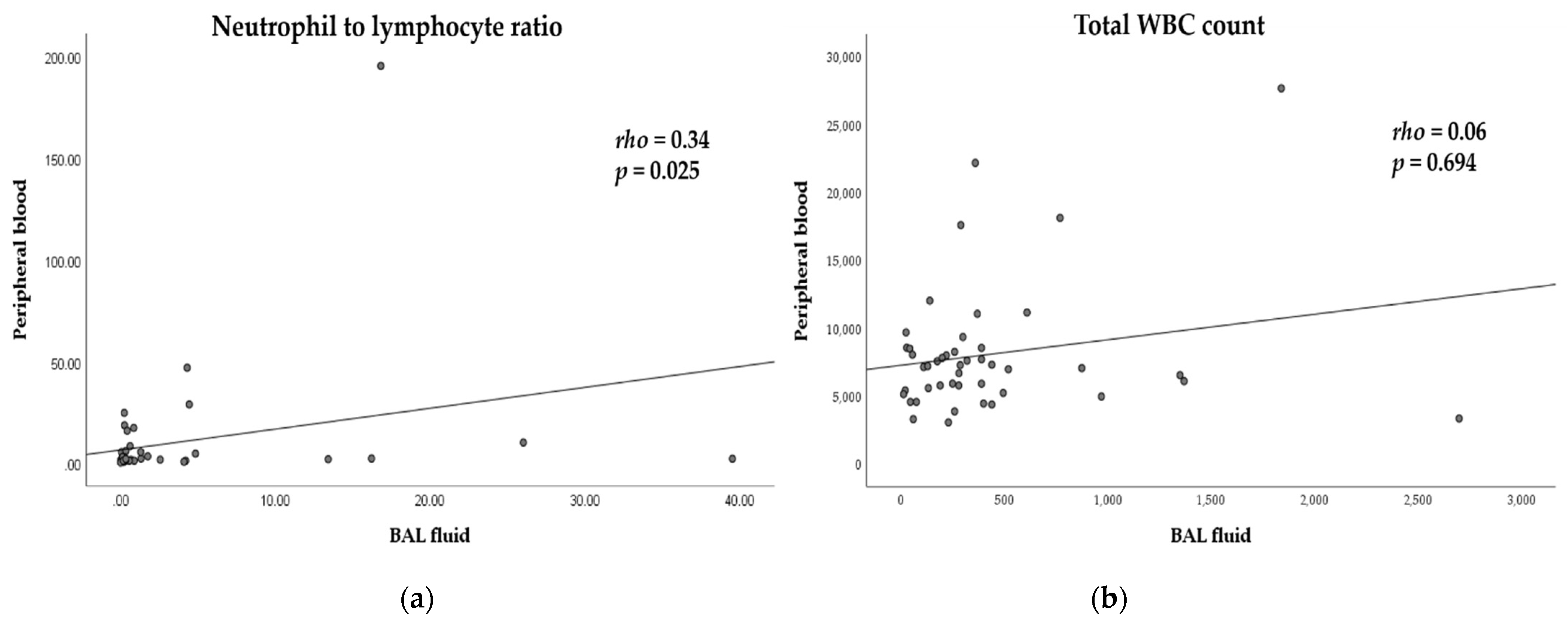
3.2. Differential Cell Counts and Correlations with BAL Fluid and Peripheral Blood
3.3. Neutrophil to Lymphocyte Ratio and Overall Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Balkwill, F.; Mantovani, A. Inflammation and cancer: Back to Virchow? Lancet 2001, 357, 539–545. [Google Scholar] [CrossRef]
- Grivennikov, S.I.; Greten, F.R.; Karin, M. Immunity, Inflammation, and Cancer. Cell 2010, 140, 883–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mantovani, A.; Allavena, P.; Sica, A.; Balkwill, F. Cancer-related inflammation. Nat. Cell Biol. 2008, 454, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aggarwal, B.B.; Vijayalekshmi, R.V.; Sung, B. Targeting Inflammatory Pathways for Prevention and Therapy of Cancer: Short-Term Friend, Long-Term Foe. Clin. Cancer Res. 2009, 15, 425–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guthrie, G.J.; Charles, K.A.; Roxburgh, C.S.; Horgan, P.G.; McMillan, D.C.; Clarke, S.J. The systemic inflammation-based neutrophil–lymphocyte ratio: Experience in patients with cancer. Crit. Rev. Oncol. Hematol. 2013, 88, 218–230. [Google Scholar] [CrossRef]
- Lagiou, P.; Trichopoulos, D. Inflammatory Biomarkers and Risk of Lung Cancer. J. Natl. Cancer Inst. 2011, 103, 1073–1075. [Google Scholar] [CrossRef]
- Templeton, A.J.; Mcnamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocana, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Solid Tumors: A Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef] [Green Version]
- Jeong, M.J.; Park, J.H.; Hur, S.Y.; Kim, C.J.; Nam, H.S.; Lee, Y.S. Preoperative Neutrophil-to-Lymphocyte Ratio as a Prognostic Factor in Uterine Sarcoma. J. Clin. Med. 2020, 9, 2898. [Google Scholar] [CrossRef]
- Cupp, M.A.; Cariolou, M.; Tzoulaki, I.; Aune, D.; Evangelou, E.; Berlanga-Taylor, A.J. Neutrophil to lymphocyte ratio and cancer prognosis: An umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med. 2020, 18, 360. [Google Scholar] [CrossRef]
- Yu, Y.; Qian, L.; Cui, J. Value of neutrophil-to-lymphocyte ratio for predicting lung cancer prognosis: A meta-analysis of 7219 patients. Mol. Clin. Oncol. 2017, 7, 498–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gu, X.-B.; Tian, T.; Tian, X.-J.; Zhang, X.-J. Prognostic significance of neutrophil-to-lymphocyte ratio in non-small cell lung cancer: A meta-analysis. Sci. Rep. 2015, 5, 12493. [Google Scholar] [CrossRef] [Green Version]
- Lu, Y.; Jiang, J.; Ren, C. The clinicopathological and prognostic value of the pretreatment neutrophil-to-lymphocyte ratio in small cell lung cancer: A meta-analysis. PLoS ONE 2020, 15, e0230979. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K.C.; Raghu, G.; Baughman, R.P.; Brown, K.K.; Costabel, U.; Du Bois, R.M.; Drent, M.; Haslam, P.L.; Kim, D.S.; Nagai, S.; et al. An Official American Thoracic Society Clinical Practice Guideline: The Clinical Utility of Bronchoalveolar Lavage Cellular Analysis in Interstitial Lung Disease. Am. J. Respir. Crit. Care Med. 2012, 185, 1004–1014. [Google Scholar] [CrossRef]
- Du Bois, R.M.; Drent, M.; Nagai, S.; Rottoli, P. The Clinical Utility of Bronchoalveolar Lavage Cellular Analysis in Interstitial Lung Disease: An ATS Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2012, 185, 1004–1014, on-line supplement. [Google Scholar]
- D’alessandro, M.; Bergantini, L.; Carleo, A.; Cameli, P.; Perrone, A.; Fossi, A.; Sestini, P.; Bargagli, E. Neutrophil-to-lymphocyte ratio in bronchoalveolar lavage from IPF patients: A novel prognostic biomarker? Minerva Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.H.; Kim, M.J.; Jeon, S.-H.; Park, M.H.; Kim, W.Y.; Lee, M.; Kim, J.H.; Kim, J.S.; Kim, Y.S.; Kim, L.; et al. The optimal sequence of bronchial brushing and washing for diagnosing peripheral lung cancer using non-guided flexible bronchoscopy. Sci. Rep. 2020, 10, 1036. [Google Scholar] [CrossRef] [PubMed]
- Goldstraw, P.; Chansky, K.; Crowley, J.; Rami-Porta, R.; Asamura, H.; Eberhardt, W.E.; Nicholson, A.G.; Groome, P.; Mitchell, A.; Bolejack, V.; et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2016, 11, 39–51. [Google Scholar] [CrossRef] [Green Version]
- Du Rand, I.A.; Blaikley, J.; Booton, R.; Chaudhuri, N.; Gupta, V.; Khalid, S.; Mandal, S.; Martin, J.; Mills, J.; Navani, N.; et al. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: Accredited by NICE. Thorax 2013, 68 (Suppl. 1), i1–i44. [Google Scholar] [CrossRef] [Green Version]
- Hothorn, T.; Lausen, B. On the exact distribution of maximally selected rank statistics. Comput. Stat. Data Anal. 2003, 43, 121–137. [Google Scholar] [CrossRef]
- University of Alabama at Birmingham; National Institutes of Health (NIH). Autoantibody Reduction Therapy in Patients with Idiopathic Pulmonary Fibrosis (ART-IPF); National Library of Medicine (US): Bethesda, MA, USA, 2018. [CrossRef]
- McMillan, D.C. The systemic inflammation-based Glasgow Prognostic Score: A decade of experience in patients with cancer. Cancer Treat. Rev. 2013, 39, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Pine, S.R.; Mechanic, L.E.; Enewold, L.; Chaturvedi, A.K.; Katki, H.A.; Zheng, Y.-L.; Bowman, E.D.; Engels, E.A.; Caporaso, N.E.; Harris, C.C. Increased Levels of Circulating Interleukin 6, Interleukin 8, C-Reactive Protein, and Risk of Lung Cancer. J. Natl. Cancer Inst. 2011, 103, 1112–1122. [Google Scholar] [CrossRef] [PubMed]
- Gooden, M.J.; de Bock, G.H.; Leffers, N.; Daemen, T.; Nijman, H.W. The prognostic influence of tumour-infiltrating lymphocytes in cancer: A systematic review with meta-analysis. Br. J. Cancer 2011, 105, 93–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engels, E.A. Inflammation in the development of lung cancer: Epidemiological evidence. Expert Rev. Anticancer. Ther. 2008, 8, 605–615. [Google Scholar] [CrossRef]
- O’Callaghan, D.S.; O’Donnell, D.; O’Connell, F.; O’Byrne, K.J. The Role of Inflammation in the Pathogenesis of Non-small Cell Lung Cancer. J. Thorac. Oncol. 2010, 5, 2024–2036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Domagala-Kulawik, J. The relevance of bronchoalveolar lavage fluid analysis for lung cancer patients. Expert Rev. Respir. Med. 2020, 14, 329–337. [Google Scholar] [CrossRef]
- Domagała-Kulawik, J.; Guzman, J.; Costabel, U. Immune Cells in Bronchoalveolar Lavage in Peripheral Lung Cancer—Analysis of 140 Cases. Respiration 2003, 70, 43–48. [Google Scholar] [CrossRef]
- Vaguliene, N.; Zemaitis, M.; Lavinskiene, S.; Miliauskas, S.; Sakalauskas, R. Local and systemic neutrophilic inflammation in patients with lung cancer and chronic obstructive pulmonary disease. BMC Immunol. 2013, 14, 36. [Google Scholar] [CrossRef] [Green Version]
- Siravegna, G.; Marsoni, S.; Siena, S.; Bardelli, A. Integrating liquid biopsies into the management of cancer. Nat. Rev. Clin. Oncol. 2017, 14, 531–548. [Google Scholar] [CrossRef]
- Michela, B. Liquid Biopsy: A Family of Possible Diagnostic Tools. Diagnostics 2021, 11, 1391. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Nam, H.-S.; Lim, J.H.; Kim, J.S.; Moon, Y.; Cho, J.H.; Ryu, J.-S.; Kwak, S.M.; Lee, H.L. Prognostic impact of a new score using neutrophil-to-lymphocyte ratios in the serum and malignant pleural effusion in lung cancer patients. BMC Cancer 2017, 17, 557. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.U.; Yeo, C.D.; Kim, H.W.; Kang, H.S.; Park, C.K.; Kim, J.S.; Kim, J.W.; Kim, S.J.; Lee, S.H. Pleural Neutrophil-to-Lymphocyte Ratio May Be Associated with Early Disease Progression in Stage IV Non-small Cell Lung Cancer. Vivo 2020, 34, 2179–2185. [Google Scholar] [CrossRef] [PubMed]

| Variables | No. (%) | NLR of BAL Fluid | ||
|---|---|---|---|---|
| n = 45 | Low (≤0.2) | High (>0.2) | p-Value | |
| Age | 0.236 | |||
| <65 | 20 (44.4) | 9 | 11 | |
| ≥65 | 25 (55.6) | 7 | 18 | |
| Sex | 0.031 | |||
| Male | 29 (64.4) | 7 | 22 | |
| Female | 16 (35.6) | 9 | 7 | |
| Smoking | 0.007 | |||
| Current + Former | 26 (57.8) | 5 | 21 | |
| Never | 19 (42.2) | 11 | 8 | |
| ECOG PS | 0.382 | |||
| 0–1 | 26 (57.8) | 11 | 15 | |
| 2–4 | 19 (42.2) | 5 | 14 | |
| Histology | 0.228 | |||
| ADC | 33 (73.3) | 13 | 20 | |
| SQC | 9 (20.0) | 3 | 6 | |
| Others NSC | 3 (6.7) | 0 | 3 | |
| T stage | 0.433 | |||
| T1–2 | 19 (42.2) | 8 | 11 | |
| T3–4 | 26 (57.8) | 8 | 18 | |
| N stage | 0.799 | |||
| N0–1 | 18 (40.0) | 6 | 12 | |
| N2–3 | 27 (60.0) | 10 | 17 | |
| M stage | 0.360 | |||
| M0 | 21 (46.7) | 6 | 15 | |
| M1 | 24 (53.3) | 10 | 14 | |
| pbNLR | 0.022 | |||
| Low (≤2.03) | 18 (40.0) | 10 | 8 | |
| High (>2.03) | 27 (60.0) | 6 | 21 | |
| Hemoglobin (g/dl) * | 0.577 | |||
| <12.0 (13.1) | 25 (55.6) | 8 | 17 | |
| ≥12.0 (13.1) | 20 (44.4) | 8 | 12 | |
| Platelet (109/L) * | 0.999 | |||
| <150 | 6 (13.3) | 2 | 4 | |
| ≥150 | 39 (86.7) | 14 | 25 | |
| CRP (mg/dl) * | 0.236 | |||
| ≤0.5 | 20 (44.4) | 9 | 11 | |
| >0.5 | 25 (55.6) | 7 | 18 | |
| Albumin (g/dl) * | 0.127 | |||
| <3.5 | 18 (40.0) | 4 | 14 | |
| ≥3.5 | 27 (60.0) | 12 | 15 | |
| LDH (IU/L) * | 0.645 | |||
| ≤211 | 6 (16.7) | 3 | 3 | |
| >211 | 30 (83.3) | 10 | 20 | |
| Variable | Bronchoalveolar Lavage Fluid | Peripheral Blood |
|---|---|---|
| Total WBC count, cell/µL | 281.0 (131.5–440.0) | 7140.0 (5325.0–8525.0) |
| Neutrophils, % | 7.0 (2.0–23.5) | 63.6 (51.8–78.7) |
| Lymphocytes, % | 14.0 (8.0–37.5) | 26.3 (13.4–34.9) |
| Monocytes, % | 3.0 (1.0–12.0) | 5.3 (4.0–6.7) |
| Macrophages, % | 26.0 (8.5–69.5) | |
| Neutrophils count, cell/µL | 9.5 (4.6–54.5) | 4244.5 (2920.9–6441.4) |
| Lymphocytes count, cell/µL | 31.2 (17.6–101.3) | 1642.1 (894.9–2334.0) |
| Monocytes count, cell/µL | 8.0 (2.4–28.9) | 344.4 (280.3–486.93) |
| Macrophages count, cell/µL | 84.7 (20.7–150.3) | |
| Neutrophil to lymphocyte ratio | 0.33 (0.15–2.15) | 2.41 (1.62–5.60) |
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | AHR | 95% CI | p-Value | |
| Age | 0.187 | |||||
| <65 | reference | |||||
| ≥65 | 1.60 | 0.80–3.21 | ||||
| Sex | 0.285 | |||||
| Male | 0.67 | 0.33–1.39 | ||||
| Female | reference | |||||
| Smoking | 0.021 | |||||
| Current + Former | 2.33 | 1.13–4.80 | ||||
| Never | reference | |||||
| ECOG PS | <0.001 | 0.023 | ||||
| 0–1 | reference | reference | ||||
| 2–4 | 3.43 | 1.69–6.99 | 3.593 | 1.20–10.80 | ||
| Histology | 0.062 | |||||
| ADC | reference | |||||
| SQC | 1.19 | 0.51–2.80 | ||||
| Other NSC | 4.19 | 1.16–15.15 | ||||
| T stage | 0.022 | |||||
| T1–2 | reference | |||||
| T3–4 | 2.47 | 1.14–5.37 | ||||
| N stage | 0.010 | |||||
| N0–1 | reference | |||||
| N2–3 | 2.75 | 1.28–5.92 | ||||
| M stage | 0.041 | 0.035 | ||||
| M0 | reference | reference | ||||
| M1 | 2.14 | 1.03–4.46 | 4.78 | 1.12–20.42 | ||
| pbNLR | <0.001 | 0.008 | ||||
| ≤2.03 | reference | reference | ||||
| >2.03 | 5.54 | 2.35–13.08 | 4.16 | 1.46–11.92 | ||
| bNLR | 0.011 | 0.016 | ||||
| ≤0.2 | reference | reference | ||||
| >0.2 | 2.71 | 1.22–6.03 | 3.50 | 1.27–9.67 | ||
| Hemoglobin (g/dl) * | 0.082 | |||||
| <12.0 | 1.87 | 0.92–3.79 | ||||
| ≥12.0 | reference | |||||
| Platelet (109/L) * | 0.167 | |||||
| <150 | 1.88 | 0.77–4.62 | ||||
| ≥150 | reference | |||||
| CRP (mg/dl) * | 0.002 | |||||
| ≤0.5 | reference | |||||
| >0.5 | 3.24 | 1.55–6.77 | ||||
| Albumin (g/dl) * | 0.019 | |||||
| <3.5 | 2.30 | 1.15–4.62 | ||||
| ≥3.5 | reference | |||||
| LDH (IU/L) * | 0.254 | |||||
| ≤211 | reference | |||||
| >211 | 1.86 | 0.64–5.41 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ryu, W.K.; Moon, Y.; Park, M.H.; Lim, J.H.; Kim, Y.S.; Lee, K.-H.; Kwak, S.M.; Kim, C.; Nam, H.-S. A Preliminary Study on the Prognostic Impact of Neutrophil to Lymphocyte Ratio of the Bronchoalveolar Lavage Fluid in Patients with Lung Cancer. Diagnostics 2021, 11, 2201. https://doi.org/10.3390/diagnostics11122201
Ryu WK, Moon Y, Park MH, Lim JH, Kim YS, Lee K-H, Kwak SM, Kim C, Nam H-S. A Preliminary Study on the Prognostic Impact of Neutrophil to Lymphocyte Ratio of the Bronchoalveolar Lavage Fluid in Patients with Lung Cancer. Diagnostics. 2021; 11(12):2201. https://doi.org/10.3390/diagnostics11122201
Chicago/Turabian StyleRyu, Woo Kyung, Yeonsook Moon, Mi Hwa Park, Jun Hyeok Lim, Young Sam Kim, Kyung-Hee Lee, Seung Min Kwak, Changhwan Kim, and Hae-Seong Nam. 2021. "A Preliminary Study on the Prognostic Impact of Neutrophil to Lymphocyte Ratio of the Bronchoalveolar Lavage Fluid in Patients with Lung Cancer" Diagnostics 11, no. 12: 2201. https://doi.org/10.3390/diagnostics11122201






