Dynamic Echocardiographic Assessments Reveal Septal E/e’ Ratio as Independent Predictor of Intradialytic Hypotension in Maintenance for Hemodialysis Patients with Preserved Ejection Fraction
Abstract
1. Introduction
2. Materials and Methods
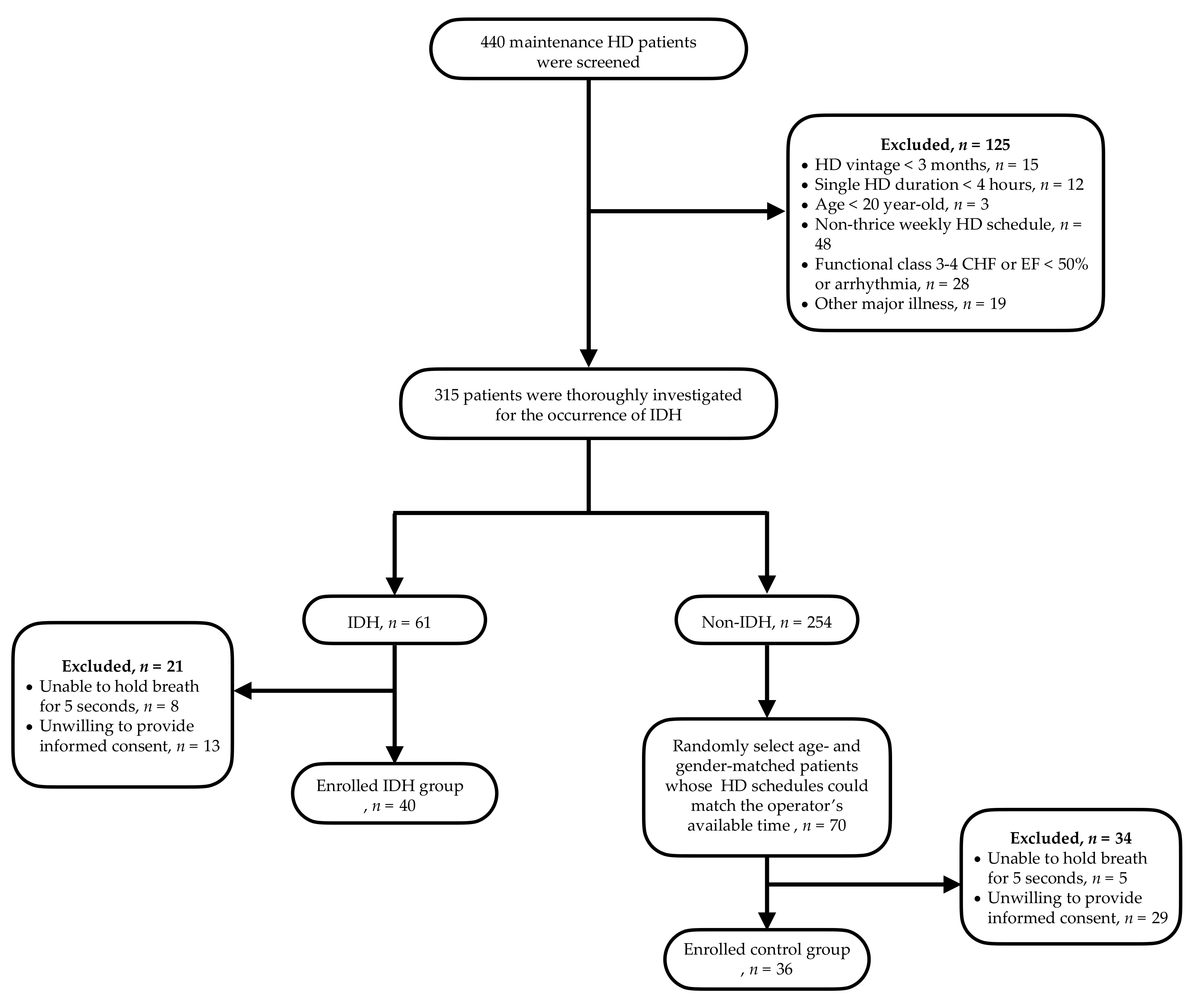
2.1. The Study Population
2.2. Transthoracic 2D Echocardiography Measurements
2.3. Statistical Analysis
3. Results
3.1. Subject Characteristics
3.2. Hemodynamic Characteristics between Groups
3.3. Dynamic Heart Function Assessments between Groups
3.4. Two-Way Repeated Measures ANOVA to Confirm the Differences of Cardiac Performance over Time between Groups
3.5. Resampling Analysis Using a Subset of Patients with Diabetes Mellitus
3.6. Echocardiographic Predictors of IDH
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Flythe, J.E.; Xue, H.; Lynch, K.E.; Curhan, G.C.; Brunelli, S.M. Association of mortality risk with various definitions of intradialytic hypotension. J. Am. Soc. Nephrol. JASN 2015, 26, 724–734. [Google Scholar] [CrossRef] [PubMed]
- Kanbay, M.; Ertuglu, L.A.; Afsar, B.; Ozdogan, E.; Siriopol, D.; Covic, A.; Basile, C.; Ortiz, A. An update review of intradialytic hypotension: Concept, risk factors, clinical implications and management. Clin. Kidney J. 2020, 13, 981–993. [Google Scholar] [CrossRef] [PubMed]
- Shoji, T.; Tsubakihara, Y.; Fujii, M.; Imai, E. Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int. 2004, 66, 1212–1220. [Google Scholar] [CrossRef] [PubMed]
- Stefansson, B.V.; Brunelli, S.M.; Cabrera, C.; Rosenbaum, D.; Anum, E.; Ramakrishnan, K.; Jensen, D.E.; Stalhammar, N.O. Intradialytic hypotension and risk of cardiovascular disease. Clin. J. Am. Soc. Nephrol. CJASN 2014, 9, 2124–2132. [Google Scholar] [CrossRef]
- Silbiger, J.J. Pathophysiology and Echocardiographic Diagnosis of Left Ventricular Diastolic Dysfunction. J. Am. Soc. Echocardiogr. 2019, 32, 216–232.e2. [Google Scholar] [CrossRef]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F., 3rd; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef]
- Shah, A.M.; Cikes, M.; Prasad, N.; Li, G.; Getchevski, S.; Claggett, B.; Rizkala, A.; Lukashevich, I.; O’Meara, E.; Ryan, J.J.; et al. Echocardiographic Features of Patients with Heart Failure and Preserved Left Ventricular Ejection Fraction. J. Am. Coll. Cardiol. 2019, 74, 2858–2873. [Google Scholar] [CrossRef]
- Yang, N.I.; Wang, C.H.; Hung, M.J.; Chen, Y.C.; Wu, I.W.; Lee, C.C.; Wu, M.S.; Kuo, L.T.; Cheng, C.W.; Cherng, W.J. Real-time three-dimensional echocardiography provides advanced haemodynamic information associated with intra-dialytic hypotension in patients with autonomic dysfunction. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 2010, 25, 249–254. [Google Scholar] [CrossRef][Green Version]
- Nette, R.W.; van den Dorpel, M.A.; Krepel, H.P.; Ie, E.H.; van den Meiracker, A.H.; Poldermans, D.; Weimar, W.; Zietse, R. Hypotension during hemodialysis results from an impairment of arteriolar tone and left ventricular function. Clin. Nephrol. 2005, 63, 276–283. [Google Scholar] [CrossRef]
- Kolb, J.; Kitzler, T.M.; Tauber, T.; Morris, N.; Skrabal, F.; Kotanko, P. Proto-dialytic cardiac function relates to intra-dialytic morbid events. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 2011, 26, 1645–1651. [Google Scholar] [CrossRef][Green Version]
- Chao, C.T.; Huang, J.W.; Yen, C.J. Intradialytic hypotension and cardiac remodeling: A vicious cycle. BioMed Res. Int. 2015, 2015, 724147. [Google Scholar] [CrossRef]
- Kooman, J.; Basci, A.; Pizzarelli, F.; Canaud, B.; Haage, P.; Fouque, D.; Konner, K.; Martin-Malo, A.; Pedrini, L.; Tattersall, J.; et al. EBPG guideline on haemodynamic instability. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 2007, 22 (Suppl. S2), ii22–ii44. [Google Scholar] [CrossRef]
- Schocken, D.D.; Benjamin, E.J.; Fonarow, G.C.; Krumholz, H.M.; Levy, D.; Mensah, G.A.; Narula, J.; Shor, E.S.; Young, J.B.; Hong, Y.; et al. Prevention of heart failure: A scientific statement from the American Heart Association Councils on Epidemiology and Prevention, Clinical Cardiology, Cardiovascular Nursing, and High Blood Pressure Research; Quality of Care and Outcomes Research Interdisciplinary Working Group; and Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation 2008, 117, 2544–2565. [Google Scholar] [CrossRef]
- Owan, T.E.; Hodge, D.O.; Herges, R.M.; Jacobsen, S.J.; Roger, V.L.; Redfield, M.M. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N. Engl. J. Med. 2006, 355, 251–259. [Google Scholar] [CrossRef]
- Redfield, M.M.; Jacobsen, S.J.; Burnett, J.C., Jr.; Mahoney, D.W.; Bailey, K.R.; Rodeheffer, R.J. Burden of systolic and diastolic ventricular dysfunction in the community: Appreciating the scope of the heart failure epidemic. JAMA 2003, 289, 194–202. [Google Scholar] [CrossRef]
- Sun, M.; Cao, X.; Guo, Y.; Tan, X.; Dong, L.; Pan, C.; Shu, X. Long-term impacts of hemodialysis on the right ventricle: Assessment via 3-dimensional speckle-tracking echocardiography. Clin. Cardiol. 2018, 41, 87–95. [Google Scholar] [CrossRef]
- Daugirdas, J.T. Pathophysiology of dialysis hypotension: An update. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2001, 38, S11–S17. [Google Scholar] [CrossRef]
- Ritz, E.; Ruffmann, K.; Rambausek, M.; Mall, G.; Schmidli, M. Dialysis hypotension--is it related to diastolic left ventricular malfunction? Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 1987, 2, 293–297. [Google Scholar]
- Ruffmann, K.; Mandelbaum, A.; Bommer, J.; Schmidli, M.; Ritz, E. Doppler echocardiographic findings in dialysis patients. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 1990, 5, 426–431. [Google Scholar] [CrossRef]
- Pabst, S.; Hammerstingl, C.; Hundt, F.; Gerhardt, T.; Grohe, C.; Nickenig, G.; Woitas, R.; Skowasch, D. Pulmonary hypertension in patients with chronic kidney disease on dialysis and without dialysis: Results of the PEPPER-study. PLoS ONE 2012, 7, e35310. [Google Scholar] [CrossRef]
- Parfrey, P.S.; Foley, R.N.; Harnett, J.D.; Kent, G.M.; Murray, D.C.; Barre, P.E. Outcome and risk factors for left ventricular disorders in chronic uraemia. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 1996, 11, 1277–1285. [Google Scholar] [CrossRef]
- Oh, J.K.; Park, S.J.; Nagueh, S.F. Established and novel clinical applications of diastolic function assessment by echocardiography. Circ. Cardiovasc. Imaging 2011, 4, 444–455. [Google Scholar] [CrossRef]
- Barefield, D.; Sadayappan, S. Phosphorylation and function of cardiac myosin binding protein-C in health and disease. J. Mol. Cell. Cardiol. 2010, 48, 866–875. [Google Scholar] [CrossRef]
- Kass, D.A.; Solaro, R.J. Mechanisms and use of calcium-sensitizing agents in the failing heart. Circulation 2006, 113, 305–315. [Google Scholar] [CrossRef]
- Fraysse, B.; Weinberger, F.; Bardswell, S.C.; Cuello, F.; Vignier, N.; Geertz, B.; Starbatty, J.; Kramer, E.; Coirault, C.; Eschenhagen, T.; et al. Increased myofilament Ca2+ sensitivity and diastolic dysfunction as early consequences of Mybpc3 mutation in heterozygous knock-in mice. J. Mol. Cell. Cardiol. 2012, 52, 1299–1307. [Google Scholar] [CrossRef]
- Maack, C.; Bohm, M. Targeting mitochondrial oxidative stress in heart failure throttling the afterburner. J. Am. Coll. Cardiol. 2011, 58, 83–86. [Google Scholar] [CrossRef]
- Kass, D.A.; Bronzwaer, J.G.; Paulus, W.J. What mechanisms underlie diastolic dysfunction in heart failure? Circ. Res. 2004, 94, 1533–1542. [Google Scholar] [CrossRef]
- Jeong, E.M.; Dudley, S.C., Jr. New diagnostic and therapeutic possibilities for diastolic heart failure. Rhode Isl. Med. J. 2014, 97, 35–37. [Google Scholar]
- Lv, W.; Booz, G.W.; Fan, F.; Wang, Y.; Roman, R.J. Oxidative Stress and Renal Fibrosis: Recent Insights for the Development of Novel Therapeutic Strategies. Front. Physiol. 2018, 9, 105. [Google Scholar] [CrossRef]
- Maharaj, R. Diastolic dysfunction and heart failure with a preserved ejection fraction: Relevance in critical illness and anaesthesia. J. Saudi Heart Assoc. 2012, 24, 99–121. [Google Scholar] [CrossRef]
- Reed, A.L.; Tanaka, A.; Sorescu, D.; Liu, H.; Jeong, E.M.; Sturdy, M.; Walp, E.R.; Dudley, S.C., Jr.; Sutliff, R.L. Diastolic dysfunction is associated with cardiac fibrosis in the senescence-accelerated mouse. Am. J. Physiol. Heart Circ. Physiol. 2011, 301, H824–H831. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.T.; Levin, N.W.; Chertow, G.M.; Larive, B.; Schulman, G.; Kotanko, P.; Frequent Hemodialysis Network Daily Trial Group. Determinants of cardiac autonomic dysfunction in ESRD. Clin. J. Am. Soc. Nephrol. CJASN 2010, 5, 1821–1827. [Google Scholar] [CrossRef] [PubMed]
- Duby, J.J.; Campbell, R.K.; Setter, S.M.; White, J.R.; Rasmussen, K.A. Diabetic neuropathy: An intensive review. Am. J. Health-Syst. Pharm. AJHP Off. J. Am. Soc. Health-Syst. Pharm. 2004, 61, 160–173. [Google Scholar] [CrossRef] [PubMed]
- Soomro, Q.H.; Charytan, D.M. Cardiovascular autonomic nervous system dysfunction in chronic kidney disease and end-stage kidney disease: Disruption of the complementary forces. Curr. Opin. Nephrol. Hypertens. 2021, 30, 198–207. [Google Scholar] [CrossRef]
| Characteristics | IDH (n = 40) | Controls (n = 36) | p Value |
|---|---|---|---|
| Age | 62.53 ± 12.32 | 62.28 ± 11.14 | 0.927 |
| Male Gender (%) | 11 (27.5) | 17 (47.2) | 0.075 |
| Body mass index | 22.4 ± 3.3 | 22.7 ± 2.6 | 0.308 |
| Comorbidities | |||
| Diabetes mellitus (%) | 23 (40) | 9 (25) | 0.012 * |
| Hypertension (%) | 21 (52.5) | 17 (47.2) | 0.538 |
| Heart failure (%) | 5 (12.5) | 4 (11.1) | 0.564 |
| Coronary artery disease (%) | 5 (12.5%) | 2 (5.7%) | 0.438 |
| Stroke (%) | 3 (7.5) | 3 (8.3) | 0.561 |
| Laboratory data | |||
| Hemoglobin (g/dL) | 10.6 ± 1.1 | 10.2 ± 1.1 | 0.136 |
| Albumin (g/dL) | 3.8 ± 0.3 | 3.7 ± 0.4 | 0.547 |
| C-reactive protein (mg/L) | 7.2 ± 12.0 | 24.0 ± 62.8 | 0.102 |
| Calcium (mg/dL) | 9.6 ± 0.9 | 9.5 ± 0.9 | 0.496 |
| Phosphate (mg/dL) | 5.0 ± 0.4 | 5.0 ± 0.4 | 0.978 |
| i-PTH (pg/mL) | 332 ± 351 | 267 ± 328 | 0.407 |
| FGF23 (RU/mL) | 50,743 ± 41,448 | 54,665 ± 40,721 | 0.825 |
| Bilirubin (mg/dL) | 0.620 ± 0.13 | 0.96 ± 1.71 | 0.215 |
| Total cholesterol (mg/dL) | 186 ± 36 | 178 ± 42 | 0.361 |
| Medications | |||
| ACEI | 0 (%) | 1 (2.9%) | 1 |
| ARB | 4 (11.8%) | 5 (17.2%) | 0.721 |
| Beta blockers | 4 (14.8%) | 7 (20.6%) | 0.479 |
| Diuretics | 2 (6.9%) | 5 (14.7%) | 0.437 |
| Dialysis parameters | |||
| Dialysate temperature (oC) | 35.8 ± 0.5 | 35.8 ± 0.5 | 0.916 |
| Dialysate conductivity | 141.0 ± 1.4 | 140.8 ± 1.4 | 0.542 |
| Low calcium dialysate, n (%) | 11 (27.5%) | 9 (25%) | 0.805 |
| Glucose containing dialysate, n (%) | 34 (85%) | 16 (44%) | <0.001 * |
| Interdialytic weight gain (kg) | 2.6 ± 1.2 | 2.1 ± 1.1 | 0.059 |
| Dry weight (kg) | 56.3 ± 12.9 | 57.3 ± 9.0 | 0.684 |
| Ultrafiltration rate (mL/min) | 11.2 ± 5.4 | 9.2 ± 3.8 | 0.074 |
| Blood Flow (mL/min) | 256 ± 39 | 267 ± 46 | 0.265 |
| Kt/V | 1.88 ± 0.46 | 1.79 ± 0.34 | 0.373 |
| Dialysis vintage, month | 76 ± 39 | 60 ± 35 | 0.058 |
| IDH (n = 40) | Controls (n = 36) | p (Time * Group) | p (Time) | |
|---|---|---|---|---|
| Systolic pressure(mmHg) | 0.043 * | 0.041 * | ||
| Pre-HD | 145.9 ± 30.8 | 145.2 ± 30.7 | ||
| During HD | 98.9 ± 23.8 | 132.5 ± 31.2 | ||
| Post-HD | 120.1 ± 28.1 | 135.7 ± 24.8 | ||
| Diastolic pressure(mmHg) | 0.256 | 0.178 | ||
| Pre-HD | 73.6 ± 11.4 | 77.69 ± 16.3 | ||
| During HD | 55.7 ± 11.0 | 68.3 ± 18.1 | ||
| Post-HD | 67.7 ± 15.0 | 72.9 ± 12.0 | ||
| IDH (n = 40) | CON (n = 36) | p (Time * Group) | p (Time) | IDH (n = 40) | CON (n = 36) | p (Time * Group) | p (Time) | ||
|---|---|---|---|---|---|---|---|---|---|
| Systolic parameters | |||||||||
| mIVS/PW | 0.571 | 0.514 | △mIVS/PW | 0.514 | 0.414 | ||||
| Pre-HD | 1.34 ± 1.68 | 1.09 ± 0.33 | △1 | (−0.28) ± 1.72 | 0.06 ± 0.34 | ||||
| During HD | 1.06 ± 0.31 | 1.17 ± 0.30 | △2 | (−0.03) ± 0.37 | (−0.07) ± 0.44 | ||||
| Post-HD | 1.03 ± 0.27 | 1.10 ± 0.34 | △3 | (−0.31) ± 1.69 | 0.01 ± 0.47 | ||||
| mLVmass (g/m2) | 0.466 | 0.42 | △mIVS/PW | 0.466 | 0.236 | ||||
| Pre-HD | 201 ± 84 | 206 ± 80 | △1 | (−21.53) ± 69.23 | (−6.11) ± 58 | ||||
| During HD | 180 ± 87 | 200 ± 84 | △2 | 1.9 ± 55.32 | 1.49 ± 55.94 | ||||
| Post-HD | 183 ± 92 | 201 ± 84 | △3 | (−18.44) ± 62.32 | (−2.31) ± 60.96 | ||||
| mLVESV (mL) | 0.657 | 0027 * | △mLVESV (mL) | 0.554 | 0.137 | ||||
| Pre-HD | 40 ± 20 | 35 ± 15 | △1 | (−4.25) ± 16.32 | (−1.0) ± 14.82 | ||||
| During HD | 36 ± 24 | 34 ± 14 | △2 | 5.05 ± 16.47 | 1.78 ± 17.62 | ||||
| Post-HD | 41 ± 29 | 36 ± 21 | △3 | 0.79 ± 23.15 | 0.78 ± 16.59 | ||||
| EF (%) | 0.077 | <0.001 * | △EF (%) | 0.024 * | 0.478 | ||||
| Pre-HD | 58.1 ± 8.7 | 59.2 ± 7.8 | △1 | (−2.29) ± 7.49 | 2.39 ± 7.46 | ||||
| During HD | 77.1 ± 13.4 | 61.6 ± 7.0 | △2 | (−1.46) ± 8.92 | (−1.02) ± 9.05 | ||||
| Post-HD | 54.6 ± 9.7 | 60.6 ± 9.8 | △3 | (−3.41) ± 8.34 | 1.29 ± 9.93 | ||||
| Tei | 0.507 | 0.08 | △Tei | 0.507 | 0.013 * | ||||
| Pre-HD | 0.28 ± 0.10 | 0.28 ± 0.10 | △1 | 0.06 ± 0.17 | 0.05 ± 0.12 | ||||
| During HD | 0.33 ± 0.14 | 0.34 ± 0.10 | △2 | (−0.01) ± 0.14 | 0.02 ± 0.19 | ||||
| Post-HD | 0.32 ± 0.13 | 0.35 ± 0.20 | △3 | 0.04 ± 0.14 | 0.08 ± 0.22 | ||||
| Diastolic parameters | |||||||||
| MLA size (g/m2) | 0.434 | <0.001 * | △MLA size (g/m2) | 0.434 | <0.001 * | ||||
| Pre-HD | 38.2 ± 7.2 | 40.7 ± 6.9 | △1 | (−4.73) ± 5.6 | (−3.83) ± 5.82 | ||||
| During HD | 33.5 ± 6.2 | 36.6 ± 7.9 | △2 | 6.90 ± 32.19 | 0.88 ± 6.13 | ||||
| Post-HD | 40.2 ± 31.6 | 38.2 ± 8.0 | △3 | 2.13 ± 32.63 | (−2.66) ± 7.15 | ||||
| Mitral E/A ratio | 0.140 | <0.001 * | △Mitral E/A ratio | 0.14 | <0.001 * | ||||
| Pre-HD | 0.8 ± 0.2 | 1.0 ± 0.7 | △1 | (−0.15) ± 0.24 | (−0.27) ± 0.61 | ||||
| During HD | 0.7 ± 0.2 | 0.8 ± 0.3 | △2 | 0.05 ± 0.25 | 0.02 ± 0.34 | ||||
| Post-HD | 0.7 ± 0.3 | 0.8 ± 0.4 | △3 | (−0.10) ± 0.29 | (−0.25) ± 0.38 | ||||
| mLVEDV (mL) | 0.142 | 0.536 | △mLVEDV (mL) | 0.142 | 0.536 | ||||
| Pre-HD | 101 ± 38 | 108 ± 36 | △1 | (−12.38) ± 32.72 | 10.00 ± 79.67 | ||||
| During HD | 89 ± 35 | 118 ± 76 | △2 | 8.64 ± 28.21 | (−14.64) ± 65.83 | ||||
| Post-HD | 98 ± 36 | 103 ± 37 | △3 | (−3.77) ± 37.62 | (−4.64) ± 33.18 | ||||
| DT (ms) | 0.024 * | 0.013 * | △DT (ms) | 0.038 * | 0.009 * | ||||
| Pre-HD | 240 ± 77 | 230 ± 75 | △1 | 32.36 ± 91.48 | 28.26 ± 70.07 | ||||
| During HD | 271 ± 87 | 257 ± 80 | △2 | 3.77 ± 85.85 | (−42.2) ± 84.69 | ||||
| Post-HD | 275 ± 78 | 218 ± 84 | △3 | 36.13 ± 96.73 | (−14.97) ± 86.63 | ||||
| Septal E/e’ | 0.007 * | <0.001 * | △Septal E/e’ | 0.007 * | <0.001 * | ||||
| Pre-HD | 20.5 ± 12.9 | 19.1 ± 0.6 | △1 | (−6.48) ± 10.91 | (−3.26) ± 6.30 | ||||
| During HD | 14.0 ± 5.7 | 16.9 ± 8.0 | △2 | 4.04 ± 8.67 | (−2.21) ± 6.81 | ||||
| Post-HD | 18.0 ± 10.6 | 14.7 ± 6.7 | △3 | (−2.45) ± 7.93 | (−4.44) ± 9.32 | ||||
| IVCCI (%) | 0.062 | 0.581 | △ IVCCI (%) | 0.067 | 0.64 | ||||
| Pre-HD | 35.83 ± 19.14 | 40.57 ± 15.55 | △1 | 5.89 ± 20.12 | (−3.40) ± 18.10 | ||||
| During HD | 41.72 ± 19.10 | 37.17 ± 17.98 | △2 | 3.30 ± 24.86 | (−0.07) ± 21.32 | ||||
| Post-HD | 45.01 ± 18.66 | 37.11 ± 18.38 | △3 | 9.19 ± 26.35 | (−3.47) ± 22.73 | ||||
| p Value * | p Value ** | |
|---|---|---|
| mLVEDD (cm) | 0.102 | 0.121 |
| EF (%) | 0.243 | 0.306 |
| Deceleration time (ms) | 0.096 | 0.155 |
| Septal E/e’ | 0.016 $ | 0.076 |
| IDH (n = 23) | Controls (n = 9) | p (Time * Group) | p (Time) | |
|---|---|---|---|---|
| Age, years | 66 ± 12 | 65 ± 11 | 0.825 | |
| Ultrafiltration, kg | 2.9 ± 1.4 | 2.2 ± 1.0 | 0.187 | |
| BMI | 23.3 ± 3.7 | 23.2 ± 2.8 | 0.953 | |
| Systolic parameters | ||||
| LVEDV (mL) | ||||
| Pre-HD | 99.1 ± 36 | 101.1 ± 31 | 0.154 | 0.327 |
| During HD | 91.3 ± 39 | 155.7 ± 14 | ||
| Post-HD | 105 ± 38 | 115 ± 45 | ||
| LVESV (mL) | ||||
| Pre-HD | 40.9 ± 20 | 38 ± 13.2 | 0.839 | 0.034 * |
| During HD | 39.3 ± 28 | 35.2 ± 16.6 | ||
| Post-HD | 47.9 ± 32.5 | 48.3 ± 29.7 | ||
| LVSV (mL) | ||||
| Pre-HD | 58.2 ± 22.9 | 63.1 ± 22 | 0.156 | 0.292 |
| During HD | 52.0 ± 20.7 | 120 ± 14.7 | ||
| Post-HD | 67.3 ± 19.7 | 67.3 ± 19.7 | ||
| EF (%) | ||||
| Pre-HD | 56± 9 | 58 ± 7 | 0.174 | 0.018 * |
| During HD | 54 ± 10 | 61 ± 6 | ||
| Post-HD | 52 ± 11 | 54 ± 7 | ||
| Diastolic parameters | ||||
| Mitral E/A ratio | 0.271 | 0.037 * | ||
| Pre-HD | 0.76 ± 0.3 | 1.01 ± 0.4 | ||
| During HD | 0.63 ± 0.2 | 0.91 ± 0.3 | ||
| Post-HD | 0.67 ± 0.3 | 0.78 ± 0.3 | ||
| Deceleration time (ms) | 0.06 | 0.385 | ||
| Pre-HD | 231 ± 83 | 235 ± 78 | ||
| During HD | 254 ± 86 | 258 ± 11 | ||
| Post-HD | 284 ± 81 | 204 ± 78 | ||
| Septal E/e’ | 0.075 | 0.026 * | ||
| Pre-HD | 24.2 ± 15.7 | 25.3 ± 16 | ||
| During HD | 15.1 ± 5.8 | 20.6 ± 9.9 | ||
| Post-HD | 21.2 ± 12.8 | 16.4 ± 4.1 |
| Variables | Univariate Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| Crude OR (95% CI) | p | Adjusted OR (95% CI) | p | |
| Age | 1.002 (0.964–1.041) | 0.926 | - | |
| Male Gender (vs. Women) | 0.424 (0.163–1.100) | 0.078 | 0.299 (0.084–1.064) | 0.062 |
| Ultrafiltration rate (mL/min) | 1.37 (1.046–1.796) | 0.072 | 1.621 (1.004–2.615) | 0.048 * |
| Diabetes (vs. no) | 3.908 (1.462–10.452) | 0.007 | 2.886 (0.945–8.817) | 0.063 |
| mLVESV (mL) | 1.016 (0.990–1.043) | 0.236 | - | |
| EF (%) | 0.984 (0.931–1.040) | 0.560 | - | |
| Tei | 1.067 (0.009–1.235) | 0.979 | - | |
| mLVEDD (cm) | 0.999 (0.938–1.063) | 0.965 | - | |
| Deceleration time (ms) | 1.002 (0.996–1.008) | 0.589 | - | |
| Mitral E/A ratio | 1 (0.952–1.051) | 0.987 | - | |
| Septal E/e’ | 0.171 (0.028–1.028) | 0.054 | 0.040 (0.003–0.606) | 0.02 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-Y.; Yang, N.-I.; Lee, C.-C.; Hung, M.-J.; Cherng, W.-J.; Hsu, H.-J.; Sun, C.-Y.; Wu, I.-W. Dynamic Echocardiographic Assessments Reveal Septal E/e’ Ratio as Independent Predictor of Intradialytic Hypotension in Maintenance for Hemodialysis Patients with Preserved Ejection Fraction. Diagnostics 2021, 11, 2266. https://doi.org/10.3390/diagnostics11122266
Chen C-Y, Yang N-I, Lee C-C, Hung M-J, Cherng W-J, Hsu H-J, Sun C-Y, Wu I-W. Dynamic Echocardiographic Assessments Reveal Septal E/e’ Ratio as Independent Predictor of Intradialytic Hypotension in Maintenance for Hemodialysis Patients with Preserved Ejection Fraction. Diagnostics. 2021; 11(12):2266. https://doi.org/10.3390/diagnostics11122266
Chicago/Turabian StyleChen, Chun-Yu, Ning-I Yang, Chin-Chan Lee, Ming-Jui Hung, Wen-Jin Cherng, Heng-Jung Hsu, Chiao-Yin Sun, and I-Wen Wu. 2021. "Dynamic Echocardiographic Assessments Reveal Septal E/e’ Ratio as Independent Predictor of Intradialytic Hypotension in Maintenance for Hemodialysis Patients with Preserved Ejection Fraction" Diagnostics 11, no. 12: 2266. https://doi.org/10.3390/diagnostics11122266
APA StyleChen, C.-Y., Yang, N.-I., Lee, C.-C., Hung, M.-J., Cherng, W.-J., Hsu, H.-J., Sun, C.-Y., & Wu, I.-W. (2021). Dynamic Echocardiographic Assessments Reveal Septal E/e’ Ratio as Independent Predictor of Intradialytic Hypotension in Maintenance for Hemodialysis Patients with Preserved Ejection Fraction. Diagnostics, 11(12), 2266. https://doi.org/10.3390/diagnostics11122266







