Prognostic Accuracy of the qSOFA Score for In-Hospital Mortality in Elderly Patients with Obstructive Acute Pyelonephritis: A Multi-Institutional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Covariates
2.3. Calculation of the qSOFA and SIRS Scores
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Patient Distribution by the qSOFA Score
3.3. Prognostic Accuracy of the qSOFA Score
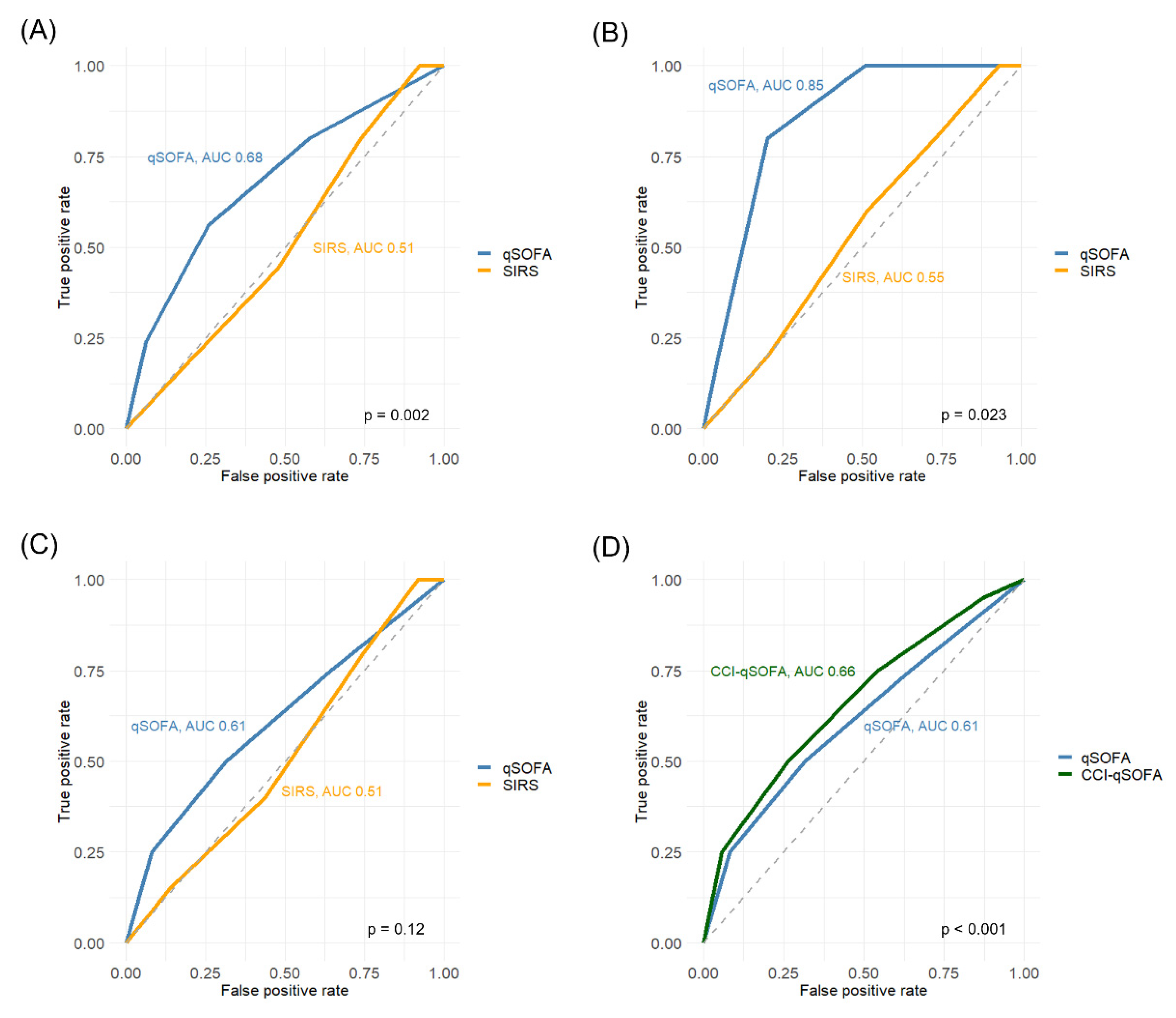
3.4. Independent Predictors for In-Hospital Mortality
3.5. Impact of Age on Prognostic Accuracy of the qSOFA Score
3.6. Development of the CCI-Incorporated qSOFA Score for Elderly Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Seymour, C.W.; Rea, T.D.; Kahn, J.M.; Walkey, A.J.; Yealy, D.M.; Angus, D.C. Severe sepsis in pre-hospital emergency care: Analysis of incidence, care, and outcome. Am. J. Respir. Crit. Care Med. 2012, 186, 1264–1271. [Google Scholar] [CrossRef] [Green Version]
- Bone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.; Sibbald, W.J. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992, 101, 1644–1655. [Google Scholar] [CrossRef] [Green Version]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Raith, E.P.; Udy, A.A.; Bailey, M.; McGloughlin, S.; MacIsaac, C.; Bellomo, R.; Pilcher, D.V. Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE). Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017, 317, 290–300. [Google Scholar]
- Freund, Y.; Lemachatti, N.; Krastinova, E.; Van Laer, M.; Claessens, Y.E.; Avondo, A.; Occelli, C.; Feral-Pierssens, A.L.; Truchot, J.; Ortega, M.; et al. French Society of Emergency Medicine Collaborators Group. Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients With Suspected Infection Presenting to the Emergency Department. JAMA 2017, 317, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.Y.; Jo, I.J.; Lee, S.U.; Lee, T.R.; Yoon, H.; Cha, W.C.; Sim, M.S.; Shin, T.G. Low Accuracy of Positive qSOFA Criteria for Predicting 28-Day Mortality in Critically Ill Septic Patients During the Early Period After Emergency Department Presentation. Ann. Emerg. Med. 2018, 71, 1–9.e2. [Google Scholar] [CrossRef]
- Tusgul, S.; Carron, P.N.; Yersin, B.; Calandra, T.; Dami, F. Low sensitivity of qSOFA.; SIRS criteria and sepsis definition to identify infected patients at risk of complication in the prehospital setting and at the emergency department triage. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 108. [Google Scholar] [CrossRef] [Green Version]
- Askim, Å.; Moser, F.; Gustad, L.T.; Stene, H.; Gundersen, M.; Åsvold, B.O.; Dale, J.; Bjørnsen, L.P.; Damås, J.K.; Solligård, E. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality-a prospective study of patients admitted with infection to the emergency department. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 56. [Google Scholar] [CrossRef]
- Naber, K.G. Urogenital infections: The pivotal role of the urologist. Eur. Urol. 2006, 50, 657–659. [Google Scholar] [CrossRef] [PubMed]
- Brun-Buisson, C. The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000, 26, S64–S74. [Google Scholar] [CrossRef]
- Hamasuna, R.; Takahashi, S.; Nagae, H.; Kubo, T.; Yamamoto, S.; Arakawa, S.; Matsumoto, T. Obstructive pyelonephritis as a result of urolithiasis in Japan: Diagnosis; treatment and prognosis. Int. J. Urol. 2015, 22, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Fujita, K.; Nakazawa, S.; Hayashi, T.; Tanigawa, G.; Imamura, R.; Hosomi, M.; Wada, D.; Fujimi, S.; Yamaguchi, S. Clinical characteristics and risk factors for septic shock in patients receiving emergency drainage for acute pyelonephritis with upper urinary tract calculi. BMC Urol. 2012, 12, 4. [Google Scholar] [CrossRef] [Green Version]
- Tambo, M.; Taguchi, S.; Nakamura, Y.; Okegawa, T.; Fukuhara, H. Presepsin and procalcitonin as predictors of sepsis based on the new Sepsis-3 definitions in obstructive acute pyelonephritis. BMC Urol. 2020, 20, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukushima, H.; Kobayashi, M.; Kawano, K.; Morimoto, S. Performance of Quick Sequential (Sepsis Related) and Sequential (Sepsis Related) Organ Failure Assessment to Predict Mortality in Patients with Acute Pyelonephritis Associated with Upper Urinary Tract Calculi. J. Urol. 2018, 199, 1526–1533. [Google Scholar] [CrossRef]
- Frenkel, W.J.; Jongerius, E.J.; Mandjes-van Uitert, M.J.; van Munster, B.C.; de Rooij, S.E. Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: A prospective cohort study. J. Am. Geriatr. Soc. 2014, 62, 342–346. [Google Scholar] [CrossRef]
- Fernbach, S.K.; Maizels, M.; Conway, J.J. Ultrasound grading of hydronephrosis: Introduction to the system used by the Society for Fetal Urology. Pediatr. Radiol. 1993, 23, 478–480. [Google Scholar] [CrossRef] [PubMed]
- Remelli, F.; Castellucci, F.; Vitali, A.; Mattioli, I.; Zurlo, A.; Spadaro, S.; Volpato, S. Predictive value of geriatric-quickSOFA in hospitalized older people with sepsis. BMC Geriatr. 2021, 21, 241. [Google Scholar] [CrossRef]
- Boonmee, P.; Ruangsomboon, O.; Limsuwat, C.; Chakorn, T. Predictors of Mortality in Elderly and Very Elderly Emergency Patients with Sepsis: A Retrospective Study. West. J. Emerg. Med. 2020, 21, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Falsetti, L.; Martino, M.; Zaccone, V.; Viticchi, G.; Raponi, A.; Moroncini, G.; Fioranelli, A.; di Pentima, C.; Martini, A.; Nitti, C.; et al. SOFA and qSOFA usefulness for in-hospital death prediction of elderly patients admitted for suspected infection in internal medicine. Infection 2020, 48, 879–887. [Google Scholar] [CrossRef]
- Asai, N.; Ohashi, W.; Kishino, T.; Sakanashi, D.; Shibata, Y.; Kato, H.; Shiota, A.; Hagihara, M.; Koizumi, Y.; Yamagishi, Y.; et al. The combined score of quick SOFA and the charlson comorbidity index could be a poor prognostic indicator for in-hospital mortality among patients with necrotizing fasciitis. J. Infect. Chemother. 2021, 27, 919–923. [Google Scholar] [CrossRef]
- Williams, A.; Griffies, T.; Damianopoulos, S.; Fatovich, D.; Macdonald, S. Effect of age and comorbidity on the ability of quick-Sequential Organ Failure Assessment score to predict outcome in emergency department patients with suspected infection. Emerg. Med. Australas. 2021, 33, 679–684. [Google Scholar] [CrossRef]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef] [Green Version]
- Bateni, S.B.; Johns, A.J.; Gingrich, A.A.; Gholami, S.; Bold, R.J.; Canter, R.J.; Kirane, A.R. Elderly Age Is Associated With More Conservative Treatment of Invasive Melanoma. Anticancer Res. 2020, 40, 2895–2903. [Google Scholar] [CrossRef] [PubMed]
- Saeed, F.; Adams, H.; Epstein, R.M. Matters of life and death: Why do older patients choose conservative management? Am. J. Nephrol. 2020, 51, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Pandey, S.; Sankhwar, S.N.; Goel, A.; Kumar, M.; Aggarwal, A.; Sharma, D.; Agarwal, S.; Pandey, T. Quick Sequential (Sepsis Related) Organ Failure Assessment: A high performance rapid prognostication tool in patients having acute pyelonephritis with upper urinary tract calculi. Investig. Clin. Urol. 2019, 60, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Madrazo, M.; López-Cruz, I.; Zaragoza, R.; Piles, L.; Eiros, J.M.; Alberola, J.; Artero, A. Prognostic accuracy of Quick SOFA in older adults hospitalised with community acquired urinary tract infection. Int. J. Clin. Pract. 2021, 75, e14620. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total, n (%) | Young, n (%) | Elderly, n (%) | p Value | |
|---|---|---|---|---|---|
| No. of patients | 369 (100) | 178 (48) | 191 (52) | ||
| Sex | Females | 258 (70) | 130 (73) | 128 (67) | 0.21 |
| Males | 111 (30) | 48 (27) | 63 (33) | ||
| CCI | 0–1 | 145 (39) | 92 (52) | 53 (28) | <0.001 |
| ≥2 | 224 (61) | 86 (48) | 138 (72) | ||
| DM | Yes | 76 (21) | 36 (20) | 40 (21) | 0.86 |
| No | 293 (79) | 142 (80) | 151 (79) | ||
| CVD | Yes | 106 (29) | 40 (22) | 66 (35) | 0.01 |
| No | 263 (71) | 138 (78) | 125 (65) | ||
| Stroke | Yes | 65 (18) | 19 (11) | 46 (24) | <0.001 |
| No | 304 (82) | 159 (89) | 145 (76) | ||
| Malignancy | Yes | 71 (19) | 29 (16) | 42 (22) | 0.17 |
| No | 298 (81) | 149(84) | 149 (78) | ||
| Immunosuppression | Yes | 26 (7) | 18 (10) | 8 (4) | 0.026 |
| No | 343 (93) | 160 (90) | 183 (96) | ||
| WBC (103/μL), median (range) | 12.4 (0.800–61.5) | 12.6 (1.2–61.5) | 12 (0.8–39.2) | 0.41 | |
| Platelet (104/μL), median (range) | 15.7 (0.2–57.0) | 16.6 (0.2–53.8) | 14.9 (1.3–57) | 0.088 | |
| CRP (mg/dL), median (range) | 14.3 (0.0–52.1) | 14.1 (0–52.1) | 14.5 (0.1–43.6) | 0.45 | |
| Albumin (g/dL), median (range) | 3.1 (1.5–4.9) | 3.3 (1.7–4.9) | 2.9 (1.5–4.7) | <0.001 | |
| Creatinine (mg/dL), median (range) | 1.2 (0.3–8.0) | 1.2 (0.3–8.0) | 1.2 (0.3–8.0) | 0.87 | |
| Midstream urine culture | Positive | 279 (76) | 137 (77) | 141 (74) | 0.48 |
| Negative | 80 (22) | 38 (21) | 42 (22) | ||
| None | 10 (3) | 3 (2) | 7 (4) | ||
| Blood culture | Positive | 143 (39) | 55 (31) | 88 (46) | 0.010 |
| Negative | 160 (43) | 89 (50) | 71 (37) | ||
| None | 66 (18) | 34 (19) | 32 (17) | ||
| Position of obstruction | Renal calyx or pelvis | 9 (2) | 3 (2) | 6 (3) | 0.33 |
| Pelvic ureteral junction | 53 (14) | 30 (17) | 23 (12) | ||
| Upper ureter | 168 (45) | 78 (44) | 90 (47) | ||
| Mid ureter | 47 (13) | 27 (15) | 20 (10) | ||
| Lower ureter | 82 (22) | 37 (21) | 45 (24) | ||
| Unknown | 10 (3) | 3 (2) | 7 (4) | ||
| Laterality | Right | 165 (45) | 81 (46) | 84 (44) | 0.049 |
| Left | 194 (53) | 96 (54) | 98 (51) | ||
| Bilateral | 10 (3) | 1 (1) | 9 (5) | ||
| Hydronephrosis | Low grade (0–2) | 219 (59) | 116 (65) | 103 (54) | 0.026 |
| High grade (3–4) | 146 (40) | 60 (34) | 86 (45) | ||
| Unknown | 4 (1) | 2 (1) | 2 (1) | ||
| Cause of obstruction | Calculus | 344 (93) | 167 (94) | 177 (93) | 0.93 |
| Tumor | 6 (2) | 3 (1.7) | 3 (2) | ||
| Others | 15 (4) | 6 (3) | 9 (5) | ||
| Unknown | 4 (1) | 2 (1) | 2 (1) | ||
| Method of drainage | Nephrostomy | 118 (32) | 60 (34) | 58 (31) | 0.39 |
| Ureteral stent | 186 (50) | 93 (53) | 93 (50) | ||
| None | 65 (18) | 24 (14) | 35 (19) | ||
| DIC | Yes | 93 (25) | 43 (24) | 50 (26) | 0.66 |
| No | 276 (75) | 135 (76) | 141 (74) | ||
| ICU admission | Yes | 70 (19) | 29 (16) | 41 (21) | 0.21 |
| No | 299 (81) | 149 (84) | 150 (79) | ||
| In-hospital mortality | Yes | 25 (7) | 5 (3) | 20 (10) | 0.003 |
| No | 344 (93) | 173 (97) | 171 (90) |
| Variables | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| p Value | OR | 95%CI | p Value | ||
| Sex | Males vs. females | 0.81 | |||
| Age | Elderly vs. young | 0.002 | 2.8 | 1.1–8.8 | 0.032 |
| CCI | ≥2 vs. 0–1 | <0.001 | 5.6 | 1.6–35.7 | 0.005 |
| DM | Yes vs. No | 0.67 | |||
| CVD | Yes vs. No | 0.21 | |||
| Stroke | Yes vs. No | 0.022 | |||
| Malignancy | Yes vs. No | 0.32 | |||
| Immunosuppression | Yes vs. No | 0.36 | |||
| Cause of obstruction | Calculus vs. Others | 0.81 | |||
| Tumor vs. Others | 0.36 | ||||
| Laterality | Right vs. Left | 0.62 | |||
| Hydronephrosis | Low grade (0–2) vs. High grade (3–5) | 0.55 | |||
| CRP | ≥14.3 vs. <14.3 | 0.54 | |||
| Platelet | <15.7 vs. ≥15.7 | 0.058 | |||
| WBC | ≥12.4 vs. <12.4 | 0.54 | |||
| Cre | ≥1.2 vs. <1.2 | 0.060 | |||
| Drainage | Nephrostomy vs. None | 0.49 | |||
| Ureteral stent vs. None | 0.97 | ||||
| SIRS | ≥1 vs. 0 | 0.035 | |||
| qSOFA | ≥2 vs. 0–1 | 0.002 | 2.8 | 1.2–6.6 | 0.019 |
| Total Cohort | |||||
|---|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | ||
| qSOFA | ≥1 | 80% | 42% | 9% | 97% |
| ≥2 | 56% | 74% | 14% | 96% | |
| ≥3 | 24% | 94% | 21% | 94% | |
| SIRS | ≥1 | 100% | 8% | 7% | 100% |
| ≥2 | 80% | 26% | 7% | 95% | |
| ≥3 | 44% | 52% | 6% | 93% | |
| ≥4 | 16% | 83% | 6% | 93% | |
| Young patients | |||||
| Sensitivity | Specificity | PPV | NPV | ||
| qSOFA | ≥1 | 100% | 49% | 5% | 100% |
| ≥2 | 80% | 80% | 10% | 99% | |
| ≥3 | 20% | 95% | 11% | 98% | |
| SIRS | ≥1 | 100% | 7% | 3% | 100% |
| ≥2 | 80% | 27% | 3% | 98% | |
| ≥3 | 60% | 49% | 3% | 98% | |
| ≥4 | 20% | 80% | 3% | 97% | |
| Elderly patients | |||||
| Sensitivity | Specificity | PPV | NPV | ||
| qSOFA | ≥1 | 75% | 36% | 12% | 92% |
| ≥2 | 50% | 68% | 16% | 92% | |
| ≥3 | 25% | 92% | 26% | 91% | |
| SIRS | ≥1 | 100% | 8% | 11% | 100% |
| ≥2 | 80% | 25% | 11% | 91% | |
| ≥3 | 40% | 56% | 10% | 89% | |
| ≥4 | 15% | 86% | 11% | 90% | |
| CCI-qSOFA | ≥1 | 95% | 13% | 11% | 96% |
| ≥2 | 75% | 46% | 14% | 94% | |
| ≥3 | 50% | 74% | 18% | 93% | |
| ≥4 | 25% | 94% | 33% | 91% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishikawa, Y.; Fukushima, H.; Tanaka, H.; Yoshida, S.; Yokoyama, M.; Matsuoka, Y.; Sakai, Y.; Otsuka, Y.; Takazawa, R.; Yano, M.; et al. Prognostic Accuracy of the qSOFA Score for In-Hospital Mortality in Elderly Patients with Obstructive Acute Pyelonephritis: A Multi-Institutional Study. Diagnostics 2021, 11, 2277. https://doi.org/10.3390/diagnostics11122277
Ishikawa Y, Fukushima H, Tanaka H, Yoshida S, Yokoyama M, Matsuoka Y, Sakai Y, Otsuka Y, Takazawa R, Yano M, et al. Prognostic Accuracy of the qSOFA Score for In-Hospital Mortality in Elderly Patients with Obstructive Acute Pyelonephritis: A Multi-Institutional Study. Diagnostics. 2021; 11(12):2277. https://doi.org/10.3390/diagnostics11122277
Chicago/Turabian StyleIshikawa, Yudai, Hiroshi Fukushima, Hajime Tanaka, Soichiro Yoshida, Minato Yokoyama, Yoh Matsuoka, Yasuyuki Sakai, Yukihiro Otsuka, Ryoji Takazawa, Masataka Yano, and et al. 2021. "Prognostic Accuracy of the qSOFA Score for In-Hospital Mortality in Elderly Patients with Obstructive Acute Pyelonephritis: A Multi-Institutional Study" Diagnostics 11, no. 12: 2277. https://doi.org/10.3390/diagnostics11122277
APA StyleIshikawa, Y., Fukushima, H., Tanaka, H., Yoshida, S., Yokoyama, M., Matsuoka, Y., Sakai, Y., Otsuka, Y., Takazawa, R., Yano, M., Tsukamoto, T., Okuno, T., Noro, A., Nagahama, K., Kamata, S., & Fujii, Y. (2021). Prognostic Accuracy of the qSOFA Score for In-Hospital Mortality in Elderly Patients with Obstructive Acute Pyelonephritis: A Multi-Institutional Study. Diagnostics, 11(12), 2277. https://doi.org/10.3390/diagnostics11122277








