State-of-Art in the Age Determination of Venous Thromboembolism: A Systematic Review
Abstract
:1. Introduction
1.1. Pathophysiology
1.2. Clinical Presentation
1.3. Relevance in the Forensic Setting
1.4. Objectives of the Study
2. Materials and Methods
2.1. Inclusion Criteria
- Patients: bodies subjected to autopsy with evidence of deep vein thrombosis (DVT) and/or pulmonary arterial thromboembolism (PTE);
- Intervention: autoptic thromboembolic material sampling and immunohistochemistry investigation for age determination;
- Comparison: Fineschi et al. classification based on histological method;
- Outcome: accuracy of method and indicators used, correspondence with histological results, concordance of different studies on pulmonary thromboembolism dating.
2.2. Exclusion Criteria
- Studies based on animal models.
2.3. Information Source and Search Process
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias
3.4. Main Findings from Reviewed Articles
4. Discussion
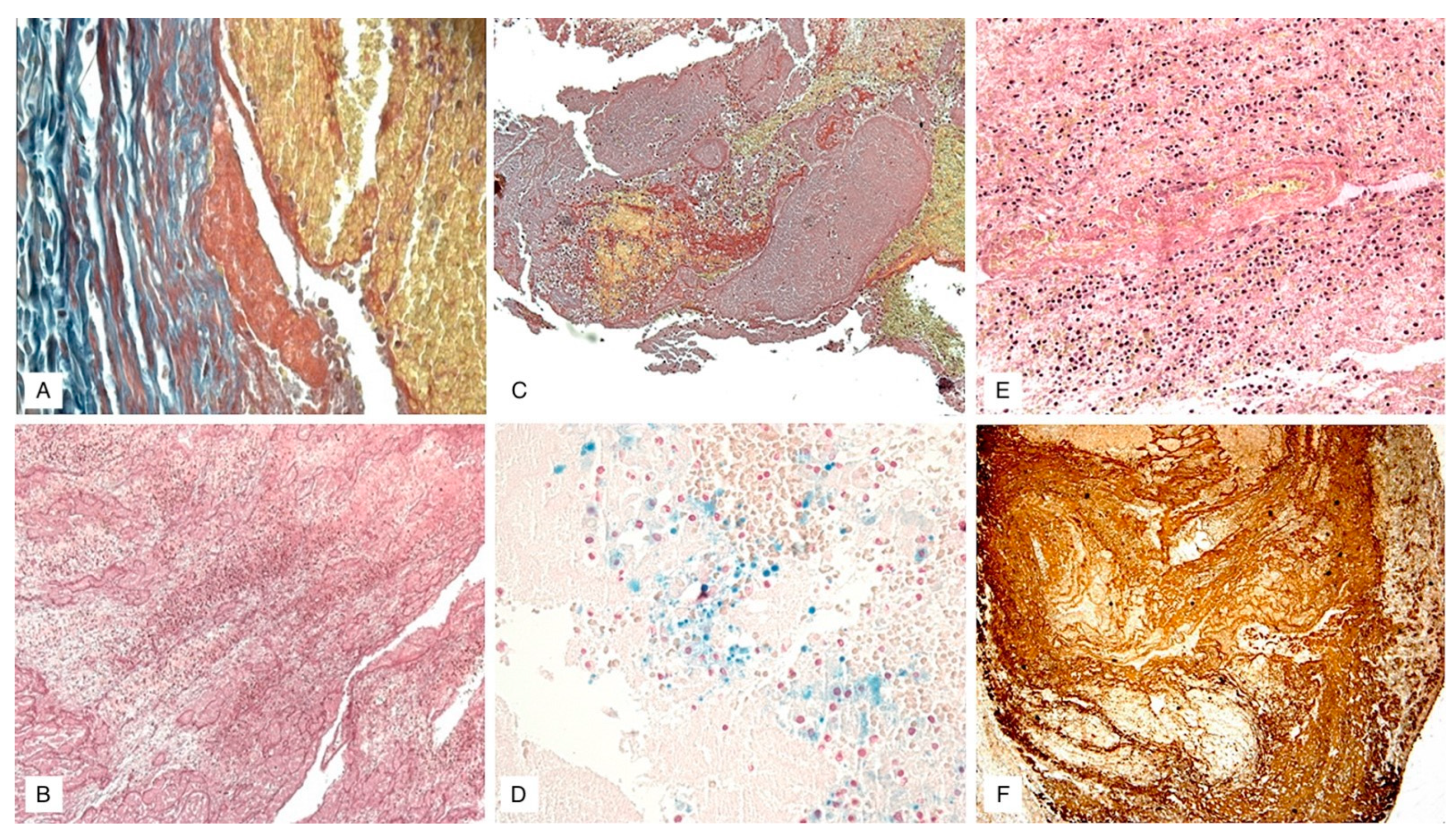
Immunohistochemical Findings
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldhaber, S.Z. Venous thromboembolism: Epidemiology and magnitude of the problem. Best Pract. Res. Clin. Haematol. 2012, 25, 235–242. [Google Scholar] [CrossRef]
- Giordano, N.J.; Jansson, P.S.; Young, M.N.; Hagan, K.A.; Kabrhel, C. Epidemiology, Pathophysiology, Stratification, and Natural History of Pulmonary Embolism. Tech. Vasc. Interv. Radiol. 2017, 20, 135–140. [Google Scholar] [CrossRef]
- Konstantinides, S.V.; Torbicki, A.; Agnelli, G.; Danchin, N.; Fitzmaurice, D.; Galiè, N.; Gibbs, J.S.; Huisman, M.V.; Humbert, M.; Kucher, N.; et al. ESC Guidelines on the diagnosis and management of acute pulmonary embolism: The Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC) Endorsed by the European Respiratory Society (ERS). Eur. Heart J. 2014, 35, 3033–3080. [Google Scholar]
- Heit, J.A.; Spencer, F.A.; White, R.H. The epidemiology of venous thromboembolism. J. Thromb. Thrombolysis 2016, 41, 3–14. [Google Scholar] [CrossRef] [Green Version]
- Cohen, A.T.; Agnelli, G.; Anderson, F.A.; Arcelus, J.I.; Bergqvist, D.; Brecht, J.G.; Greer, I.A.; Heit, J.A.; Hutchinson, J.L.; Kakkar, A.K.; et al. VTE Impact Assessment Group in Europe (VITAE). Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb. Haemost. 2007, 98, 756–764. [Google Scholar] [PubMed]
- Phillippe, H.M. Overview of venous thromboembolism. Am. J. Manag. Care 2017, 23, S376–S382. [Google Scholar]
- Markel, A.; Gavish, I.; Kfir, H.; Rimbrot, S. Venous thromboembolism: The prevailing approach to diagnosis, prevention and treatment among Internal Medicine practitioners. Int. Angiol. 2017, 36, 42–49. [Google Scholar] [CrossRef]
- Smith, S.B.; Geske, J.B.; Kathuria, P.; Cuttica, M.; Schimmel, D.R.; Courtney, D.M.; Waterer, G.W.; Wunderink, R.G. Analysis of National Trends in Admissions for Pulmonary Embolism. Chest 2016, 150, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Fineschi, V.; Bafunno, V.; Bello, S.; De Stefano, F.; Margaglione, M.; Neri, M.; Riezzo, I.; Turillazzi, E.; Bonsignore, A.; Vecchione, A.; et al. Fatal pulmonary thromboembolism. A retrospective autopsy study: Searching for genetic thrombophilias (Factor V Leiden (G1691A) and FII (G20210A) gene variants) and dating the thrombus. Forensic. Sci. Int. 2012, 214, 152–158. [Google Scholar] [CrossRef]
- Brandimarti, F.; Alessandrini, F.; Pesaresi, M.; Catalani, C.; De Angelis, L.; Galeazzi, R.; Giovagnetti, S.; Gesuita, R.; Righi, E.; Giorgetti, R.; et al. Investigation on genetic thrombophilic factors in FFPE autopsy tissue from subjects who died from pulmonary embolism. Int. J. Leg. Med. 2017, 131, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Soo Hoo, G.W. Overview and assessment of risk factors for pulmonary embolism. Expert Rev. Respir. Med. 2013, 7, 171–191. [Google Scholar] [CrossRef] [PubMed]
- Timp, J.F.; Braekkan, S.K.; Versteeg, H.H.; Cannegieter, S.C. Epidemiology of cancer associated venous thrombosis. Blood 2013, 12210, 1712–1723. [Google Scholar] [CrossRef] [Green Version]
- Lyman, G.H.; Bohlke, K.; Khorana, A.A.; Kuderer, N.M.; Lee, A.Y.; Arcelus, J.I.; Balaban, E.P.; Clarke, J.M.; Flowers, C.R.; Francis, C.W.; et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J. Oncol. Pract. 2015, 11, e442–e444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanco-Molina, A.; Rota, L.L.; Di Micco, P.; Brenner, B.; Trujillo-Santos, J.; Ruiz-Gamietea, A.; Monreal, M.; RIETE Investigators. Venous thromboembolism during pregnancy, postpartum or during contraceptive use. Thromb. Haemost. 2010, 103, 306–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanco-Molina, A.; Trujillo-Santos, J.; Tirado, R.; Cañas, I.; Riera, A.; Valdés, M.; Monreal, M.; RIETE Investigators. Venous thromboembolism in women using hormonal contraceptives. Findings from the RIETE Registry. Thromb. Haemost. 2009, 101, 478–482. [Google Scholar] [CrossRef] [PubMed]
- Gong, D.Y.; Liu, X.F.; Huang, F.J. Clinical feature analysis of fatal pulmonary thromboembolism: Experiences from 41 autopsy-confirmed cases. Eur. Rev. Med. Pharm. Sci. 2013, 17, 701–706. [Google Scholar]
- Sweet, P.H., 3rd; Armstrong, T.; Chen, J.; Masliah, E.; Witucki, P. Fatal pulmonary embolism update: 10 years of autopsy experience at an academic medical center. JRSM Short Rep. 2013, 4, 2042533313489824. [Google Scholar] [CrossRef]
- Cordasco, F.; Sicilia, F.; Sacco, M.A.; Ricci, P.; Savastano, S.; Iezzi, I.; Aquila, I. A forensic case of erosive cystitis and septic pulmonary embolism: Is there a correlation? Clin. Ter. 2020, 171, e192–e196. [Google Scholar] [PubMed]
- Yamashita, Y.; Morimoto, T.; Kimura, T. Venous thromboembolism: Recent advancement and future perspective. J. Cardiol. 2022, 79, 79–89. [Google Scholar] [CrossRef]
- Manzoni, M.; Reggiani, M.; GrAM. A simplified diagnostic algorithm for the management of suspected pulmonary embolism: The YEARS study. Int. Emerg. Med. 2018, 13, 429–431. [Google Scholar] [CrossRef]
- Henriksson, P.; Westerlund, E.; Wallén, H.; Brandt, L.; Hovatta, O.; Ekbom, A. Incidence of pulmonary and venous thromboembolism in pregnancies after in vitro fertilisation: Cross sectional study. BMJ 2013, 346, e8632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sweetland, S.; Beral, V.; Balkwill, A.; Liu, B.; Benson, V.S.; Canonico, M.; Green, J.; Reeves, G.K.; Million Women Study Collaborators. Venous thromboembolism risk in relation to use of different types of postmenopausal hormone therapy in a large prospective study. J. Thromb. Haemost. 2012, 10, 2277–2286. [Google Scholar] [CrossRef] [PubMed]
- Turillazzi, E.; Riezzo, I.; Neri, M.; Pomara, C.; Cecchi, R.; Fineschi, V. The diagnosis of fatal pulmonary fat embolism using quantitative morphometry and confocal laser scanning microscopy. Pathol. Res. Pract. 2008, 204, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Ro, A.; Kageyama, N.; Mukai, T. Pathophysiology of Venous Thromboembolism with Respect to the Anatomical Features of the Deep Veins of Lower Limbs: A Review. Ann. Vasc. Dis. 2017, 10, 99–106. [Google Scholar] [CrossRef] [Green Version]
- Margiotta, G.; Coletti, A.; Severini, S.; Tommolini, F.; Lancia, M. Medico-Legal Aspects of Pulmonary Thromboembolism. Adv. Exp. Med. Biol. 2017, 906, 407–418. [Google Scholar]
- Albolino, S.; Bellandi, T.; Cappelletti, S.; Di Paolo, M.; Fineschi, V.; Frati, P.; Offidani, C.; Tanzini, M.; Tartaglia, R.; Turillazzi, E. New rules on patient’s safety and professional liability for the Italian health service. Curr. Pharm. Biotechnol. 2019, 20, 615–624. [Google Scholar] [CrossRef]
- Mobilia, F.; Casali, M.B.; Gallieni, M.; Genovese, U.R. Lethal pulmonary thromboembolism: An autopsy-based study on a rare but legally relevant event. Med. Sci. Law. 2014, 54, 78–83. [Google Scholar] [CrossRef]
- Furukoji, E.; Gi, T.; Yamashita, A.; Moriguchi-Goto, S.; Kojima, M.; Sugita, C.; Sakae, T.; Sato, T.; Hirai, T.; Asada, Y. CD163 macrophage and erythrocyte contents in aspirated deep vein thrombus are associated with the time after onset: A pilot study. Thromb. J. 2016, 14, 46. [Google Scholar] [CrossRef] [Green Version]
- Saukko, P.; Knight, B. Knight’s Forensic Pathology, 4th ed.; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar]
- Fineschi, V.; Turillazzi, E.; Neri, M.; Pomara, C.; Riezzo, I. Histological age determination of venous thrombosis: A neglected forensic task in fatal pulmonary thrombo-embolism. Forensic. Sci. Int. 2009, 186, 22–28. [Google Scholar] [CrossRef]
- Irniger, W. Histologische altersbestimmung von thrombosen und embolien. Virchows Arch. Pathol. Anat. Physiol. Klin. Med. 1963, 336, 220–237. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [Green Version]
- Nosaka, M.; Ishida, Y.; Kimura, A.; Kondo, T. Time-dependent appearance of intrathrombus neutrophils and macrophages in a stasis-induced deep vein thrombosis model and its application to thrombus age determination. Int. J. Leg. Med. 2009, 123, 235–240. [Google Scholar] [CrossRef]
- Nosaka, M.; Ishida, Y.; Kimura, A.; Kondo, T. Immunohistochemical detection of MMP-2 and MMP-9 in a stasis-induced deep vein thrombosis model and its application to thrombus age estimation. Int. J. Leg. Med. 2010, 124, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Nosaka, M.; Ishida, Y.; Kimura, A.; Kondo, T. Time-dependent organic changes of intravenous thrombi in stasis-induced deep vein thrombosis model and its application to thrombus age determination. Forensic. Sci. Int. 2010, 195, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Nosaka, M.; Ishida, Y.; Kuninaka, Y.; Kimura, A.; Kondo, T. Immunohistochemical detection of uPA, tPA, and PAI-1 in a stasis-induced deep vein thrombosis model and its application to thrombus age estimation. Int. J. Leg. Med. 2012, 126, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Nosaka, M.; Ishida, Y.; Kimura, A.; Kondo, T. Immunohistochemical detection of intrathrombotic macrophage-derived cytokines and its application to thrombus age estimation in murine deep vein thrombosis model. Int. J. Leg. Med. 2013, 129, 1021–1025. [Google Scholar] [CrossRef] [PubMed]
- Nosaka, M.; Ishida, Y.; Kimura, A.; Hama, M.; Kawaguchi, T.; Yamamoto, H.; Kuninaka, Y.; Kondo, T. Immunohistochemical detection of intrathrombotic IL-6 and its application to thrombus age estimation. Int. J. Leg. Med. 2015, 129, 1021–1025. [Google Scholar] [CrossRef]
- Nosaka, M.; Ishida, Y.; Kimura, A.; Kawaguchi, T.; Yamamoto, H.; Kuninaka, Y.; Kondo, T. Immunohistochemical detection of intrathrombotic fibrocytes and its application to thrombus age estimation in murine deep vein thrombosis model. Int. J. Leg. Med. 2017, 131, 179–183. [Google Scholar] [CrossRef]
- Nosaka, M.; Ishida, Y.; Kimura, A.; Yamamoto, H.; Kato, T.; Kuninaka, Y.; Shimada, E.; Kondo, T. Detection of intrathrombotic endothelial progenitor cells and its application to thrombus age estimation in a murine deep vein thrombosis model. Int. J. Leg. Med. 2017, 131, 1633–1638. [Google Scholar] [CrossRef]
- Nosaka, M.; Ishida, Y.; Kuninaka, Y.; Taruya, A.; Kimura, A.; Shimada, E.; Yamamoto, H.; Michiue, T.; Furukawa, F.; Kondo, T. The application of autophagy to thrombus age estimation in murine deep vein thrombosis model. Int. J. Leg. Med. 2020, 134, 1061–1066. [Google Scholar] [CrossRef]
- Nosaka, M.; Ishida, Y.; Kuninaka, Y.; Ishigami, A.; Taruya, A.; Shimada, E.; Hashizume, Y.; Yamamoto, H.; Kimura, A.; Furukawa, F.; et al. Intrathrombotic appearances of AQP-1 and AQP-3 in relation to thrombus age in murine deep vein thrombosis model. Int. J. Leg. Med. 2021, 135, 547–553. [Google Scholar] [CrossRef]
- Maffeis, V.; Nicolè, L.; Rago, C.; Fassina, A. Histological criteria for age determination of fatal venous thromboembolism. Int. J. Leg. Med. 2018, 132, 775–780. [Google Scholar] [CrossRef]
- Mansueto, G.; Costa, D.; Capasso, E.; Varavallo, F.; Brunitto, G.; Caserta, R.; Esposito, S.; Niola, M.; Sardu, C.; Marfella, R.; et al. The dating of thrombus organization in cases of pulmonary embolism: An autopsy study. BMC Cardiovasc. Disord. 2019, 19, 250. [Google Scholar] [CrossRef]
- Moller, P. Studien uber die embolische und autochtone thrombose in der Arteria Pulmonalis. Beiträge Pathol. Anat. 1923, 71, 27. [Google Scholar]
- Sevitt, S. Organic fragmentation in pulmonary thrombo-emboli. J. Pathol 1977, 122, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Olsen, E.G.J. The Pathology of the Heart, 2nd ed.; Mac Millan: London, UK, 1980. [Google Scholar]
- Leu, A.J.; Leu, H.J. Spezielle Probleme bei der histologischen Altersbestimmung von Thromben und Emboli. Pathologe 1989, 10, 87–92. [Google Scholar]
- Janssen, W. Forensic Histopathology, 1st ed.; Springer: Berlin/Heidelberg, Germany, 1984. [Google Scholar]
- Quarmby, J.; Smith, A.; Collins, M.; Cederlholm-Williams, S.; Burnand, K. A model of in vivo human venous thrombosis that confirms changes in the release of specific soluble cell adhesion molecules in experimental venous thrombogenesis. J. Vasc. Surg. 1999, 30, 139–147. [Google Scholar] [CrossRef] [Green Version]
- Modarai, B.; Burnand, K.G.; Humphries, J.; Waltham, M.; Smith, A. The role of neovascularization in the resolution of venous thrombus. Thromb. Haemost. 2005, 93, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Freytes, D.O.; Kang, J.W.; Marcos-Campos, I.; Vunjak-Novakovic, G. Macrophages modulate the viability and growth of human mesenchymal stem cells. J. Cell Biochem. 2013, 114, 220–229. [Google Scholar] [CrossRef]
- Finn, A.V.; Nakano, M.; Polavarapu, R.; Karmali, V.; Saeed, O.; Zhao, X.; Yazdani, S.; Otsuka, F.; Davis, T.; Habib, A.; et al. Hemoglobin directs macrophage differentiation and prevents foam cell formation in human atherosclerotic plaques. J. Am. Coll. Cardiol. 2012, 59, 166–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turillazzi, E.; Karch, S.B.; Neri, M.; Pomara, C.; Riezzo, I.; Fineschi, V. Confocal laser scanning microscopy. Using new technology to answer old questions in forensic investigations. Int. J. Leg. Med. 2008, 122, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Turillazzi, E.; Baroldi, G.; Silver, M.D.; Parolini, M.; Pomara, C.; Fineschi, V. A systematic study of a myocardial lesion: Colliquative myocytolysis. Int. J. Cardiol. 2005, 104, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Dettmeyer, R.B. Forensic Histopathology: Fundamentals and Perspectives, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]

| Used Antibodies | Studies Included in Systematic Review | |||
|---|---|---|---|---|
| Fineschi et al. 2009 [30] | Furukoji et al. 2016 [28] | Maffeis et al. 2017 [43] | Mansueto et al. 2019 [44] | |
| Fibrin | 16 (DVT) | |||
| Fibrinogen | 140 (DVT + PTE) | 30 (PTE) | ||
| MPO | 1 (DVT + PTE) | |||
| Integrin α2bβ3 | 16 (DVT) | 1 (DVT + PTE) | ||
| SMA | 16 (DVT) | |||
| Glycophorin A | 16 (DVT) | |||
| CD3 | 30 (PTE) | |||
| CD15 | 140 (DVT + PTE) | |||
| CD34 | 16 (DVT) | 1 (DVT + PTE) | ||
| CD45 | 140 (DVT + PTE) | 30 (PTE) | ||
| CD61 | 140 (DVT + PTE) | |||
| CD68 | 140 (DVT + PTE) | 16 (DVT) | 1 (DVT + PTE) | 30 (PTE) |
| CD163 | 16 (DVT) | |||
| CD206 | 16 (DVT) | |||
| Factor VIII | 30 (PTE) | |||
| Heterogeneities | Studies Included in Systematic Review | |||
|---|---|---|---|---|
| Fineschi et al. [30] | Furukoji et al. [28] | Maffeis et al. [43] | Mansueto et al. [44] | |
| Year | 2009 | 2016 | 2017 | 2019 |
| Country | Italy | Japan | Italy | Italy |
| Type of Study | Retrospective Study | Retrospective Study | Case Report | Retrospective Study |
| Patient Selection | Post-Mortem Examination of Fatal PTE Cases | Alive Clinical-Diagnosed DVT Patients | Fatal PTE Case | Post-Mortem Examination of Fatal PTE Cases |
| Number of Patients | 140 | 16 | 1 | 30 |
| Patients Sex | 63 Males 77 Females | 8 Males 8 Females | 1 Female | 19 Males 11 Females |
| Age Range | 37–73 Years | 35–78 Years | 46 Years | 38–87 Years |
| Specimen Typology | DVT and PTE | DVT | DVT and PTE | PTE |
| Vessel Wall Collection | Yes | No | Yes | Yes |
| Histological Comparison | Yes | Yes | Yes | Yes |
| Histological Techniques | H&E, Masson, Azan, Mallory, PTAH, Van Gieson, Perls, von Kossa | H&E | H&E, Van Gieson, Perls | H&E, Picro Sirius Red/Fast Green |
| Other Employed Techniques | Confocal Laser Scanning Microscope (CLSM) | - | - | Immunofluorescence |
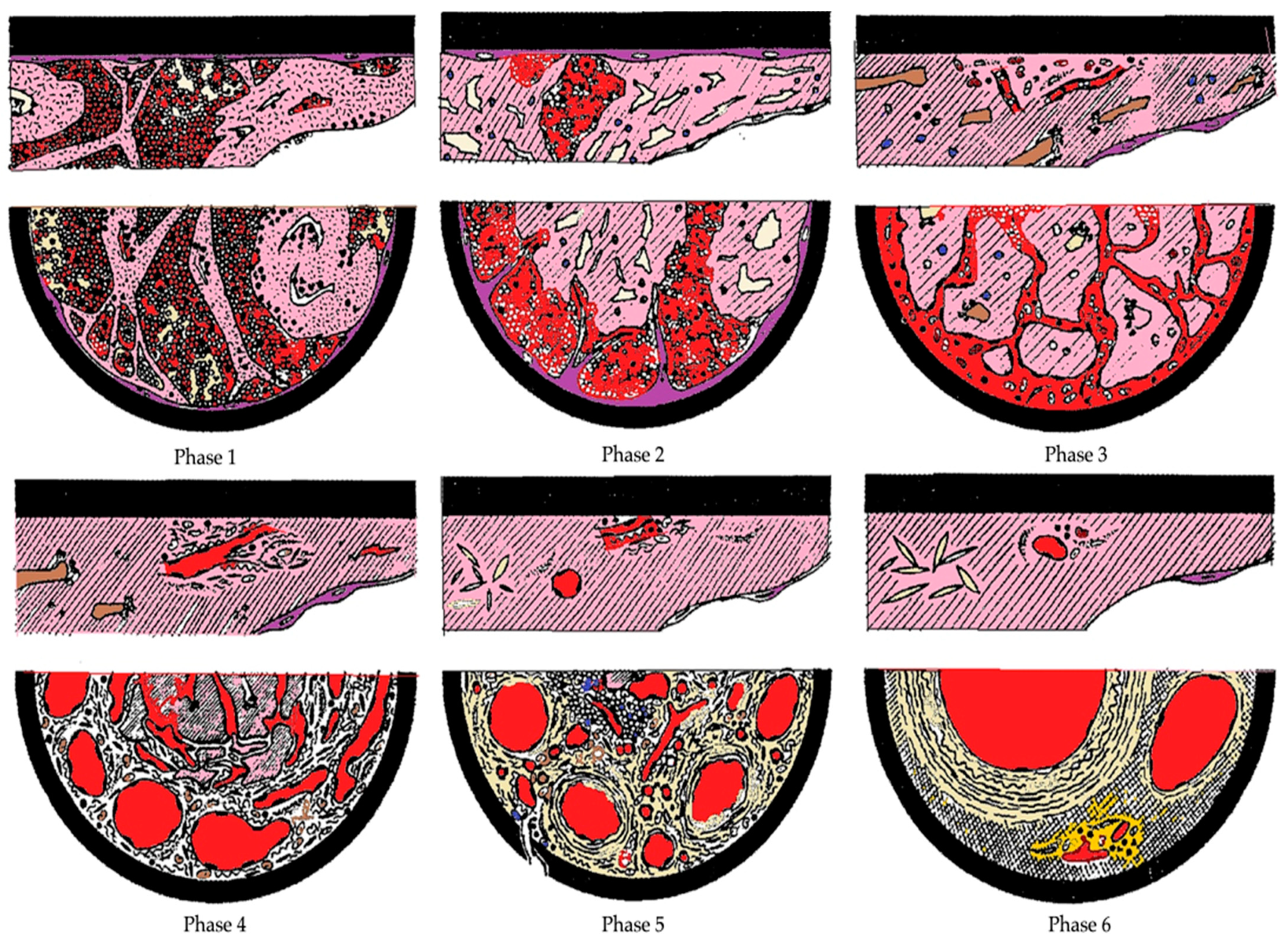
| Phase | Histological Modification |
|---|---|
| 1st Phase (1–7 Days) | Flowing blood on an eroded endothelium, eliciting a platelet plug and fibrin deposition with a layered growth (Zahn’s lines). No reaction between endothelium and thrombus is visible. Erythrocytes are preserved and agglomerated. Initial white blood cells pyknosis. Monocytes cells with enlarged nuclei. Calcium is observed as precipitates with von Kossa stain. The thrombus at its initiation is firmly attached to a small portion of the vessel wall and is not easily removed to leave fragments in situ. On the contrary, a coagulum maintains the usual blood composition (i.e., prevailing red cells plus leukocytes and platelets and a fine network of fibrin), is not attached to the endothelium, and can be easily removed. |
| 2nd Phase (2–8 Weeks) | Endothelial budding and proliferative changes of the medial ring are represented by the penetration of fibroblasts. Macrophages containing hemosiderin predominate, red blood cells ghosts and fibrinous transformation. The ribbons of fibrin changing to coalescences, trapping white cells. The free surface of thrombus is covered by the endothelium. Scattered nuclear debris of white blood cells |
| 3rd Phase (More than 2 Months) | Completely hyalinized thrombus with central sinuous cavities and more advanced recanalizing neo-formed larger vessels with fresh flowing blood. Few white cells are visible between compact, fiber-rich and cell-deficient connective tissue. |
| Time Elapsed since the Formation of Thrombus (Days) | |||
|---|---|---|---|
| 1 Day | 1–3 Days | 5 Days or More | |
| N/M Ratio * | >5 (6.8 ± 1.1) | >2 (2.5 ± 0.4) | > or = 1 (1.1 ± 0.1) |
| Histological Findings | 3-Point Inflammatory Cellular Infiltration and Fibrosis Semi-Quantitative Score | |||
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |
| Cellular Infiltration | Absent | Little | Moderate | High |
| Fibrosis | Absent | 10–40% | 40–80% | >80% |
| Early (1 h) | Recent (1 h–24 h) | Recent-Medium (24 h–48 h) | Medium (48 h–72 h) | Old (>72 h) | |
|---|---|---|---|---|---|
| Inflammatory Cells | 0 | 1 | 1/2 | 2/3 | 0/1 |
| Fibrosis | 0 | 0 | 1 | 2 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Fazio, N.; Delogu, G.; Ciallella, C.; Padovano, M.; Spadazzi, F.; Frati, P.; Fineschi, V. State-of-Art in the Age Determination of Venous Thromboembolism: A Systematic Review. Diagnostics 2021, 11, 2397. https://doi.org/10.3390/diagnostics11122397
Di Fazio N, Delogu G, Ciallella C, Padovano M, Spadazzi F, Frati P, Fineschi V. State-of-Art in the Age Determination of Venous Thromboembolism: A Systematic Review. Diagnostics. 2021; 11(12):2397. https://doi.org/10.3390/diagnostics11122397
Chicago/Turabian StyleDi Fazio, Nicola, Giuseppe Delogu, Costantino Ciallella, Martina Padovano, Federica Spadazzi, Paola Frati, and Vittorio Fineschi. 2021. "State-of-Art in the Age Determination of Venous Thromboembolism: A Systematic Review" Diagnostics 11, no. 12: 2397. https://doi.org/10.3390/diagnostics11122397
APA StyleDi Fazio, N., Delogu, G., Ciallella, C., Padovano, M., Spadazzi, F., Frati, P., & Fineschi, V. (2021). State-of-Art in the Age Determination of Venous Thromboembolism: A Systematic Review. Diagnostics, 11(12), 2397. https://doi.org/10.3390/diagnostics11122397






