The Relationship between Subjective Symptoms and Quality of Life in Conjunctivochalasis Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Severity of Subjective Symptoms Assessed by Visual Analogue Scale
2.3. Severity of Subjective Symptoms Assessed by the Dry-Eye-Related Quality of Life Score (DEQS) Questionnaire
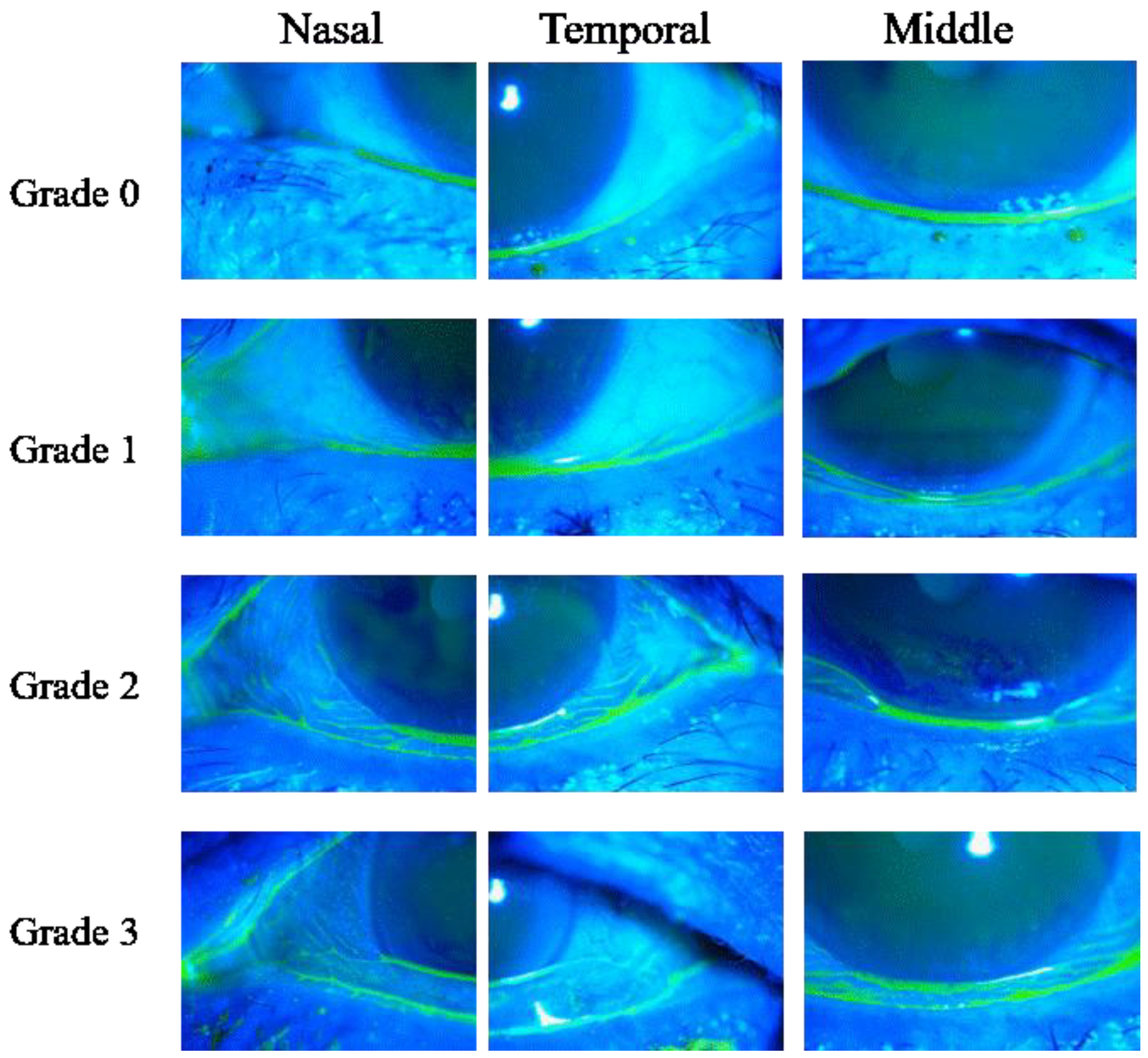
2.4. Ocular Surface Examinations
2.5. Statistical Analysis
3. Results
3.1. Patient Background for CCh and DE
3.2. Subjective Symptoms
3.3. Relationship between Total VAS Score and QOL Score
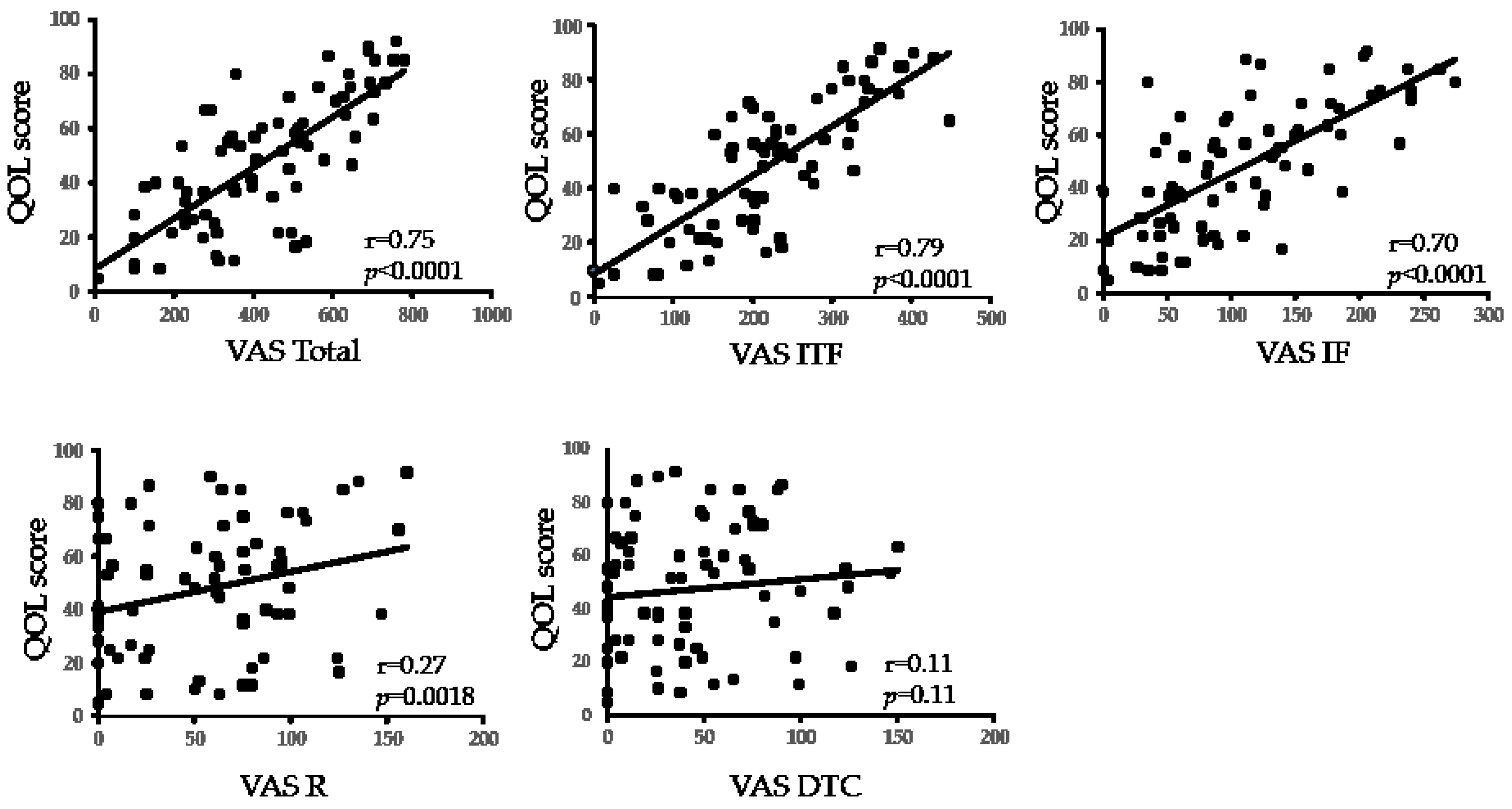
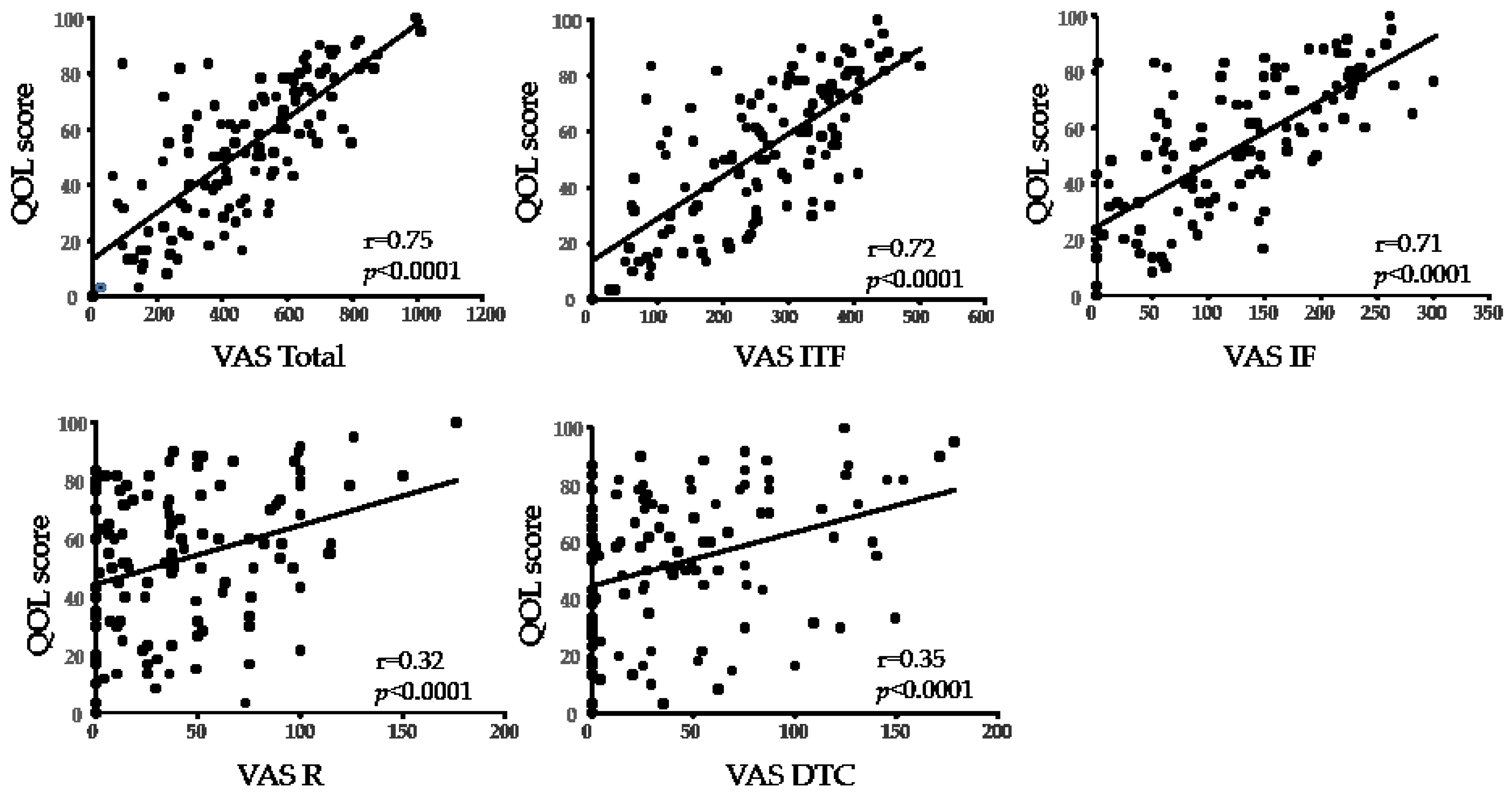
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BEB | benign essential blepharospasm |
| CCh | conjunctivochalasis |
| DE | dry eye |
| DEQS | dry eye-related quality-of-life score |
| DTC | delayed tear clearance |
| FBUT | fluorescein breakup time |
| FRD | friction-related disease |
| ITF | instability of tear film |
| IF | increased friction |
| MGD | meibomian gland dysfunction |
| QOL | quality of life |
| VAS | visual analog scale |
References
- Hughes, W.L. Conjunctivochalasis. Am. J. Ophthalmol. 1942, 25, 48–51. [Google Scholar] [CrossRef]
- Meller, D.; Tseng, S.C. Conjunctivochalasis: Literature review and possible pathophysiology. Surv. Ophthalmol. 1998, 43, 225–232. [Google Scholar] [CrossRef]
- Mimura, T.; Yamagami, S.; Usui, T.; Funatsu, H.; Mimura, Y.; Noma, H.; Honda, N.; Amano, S. Changes of conjunctivochalasis with age in a hospital-based study. Am. J. Ophthalmol. 2009, 147, 171–177.e1. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, N.; Komuro, A.; Nishii, M.; Inagaki, K.; Tanioka, H.; Kawasaki, S.; Kinoshita, S. Clinical impact of conjunctivochalasis on the ocular surface. Cornea 2005, 24, S24–S31. [Google Scholar] [CrossRef]
- Le, Q.; Cui, X.; Xiang, J.; Ge, L.; Gong, L.; Xu, J. Impact of conjunctivochalasis on visual quality of life: A community population survey. PLoS ONE 2014, 9, e110821. [Google Scholar] [CrossRef]
- Marmalidou, A.; Kheirkhah, A.; Dana, R. Conjunctivochalasis: A systematic review. Surv. Ophthalmol. 2018, 63, 554–564. [Google Scholar] [CrossRef]
- Di Pascuale, M.A.; Espana, E.M.; Kawakita, T.; Tseng, S.C.G. Clinical characteristics of conjunctivochalasis with or without aqueous tear deficiency. Br. J. Ophthalmol. 2004, 88, 388–392. [Google Scholar] [CrossRef] [Green Version]
- Sakane, Y.; Yamaguchi, M.; Yokoi, N.; Uchino, M.; Dogru, M.; Oishi, T.; Ohashi, Y.; Ohashi, Y. Development and Validation of the Dry Eye-Related Quality-of-Life Score Questionnaire. JAMA Ophthalmol. 2013, 131, 1331–1338. [Google Scholar] [CrossRef]
- Ishikawa, S.; Kato, N.; Takeuchi, M. The Efficacy of Strip Meniscometry and DEQS for Dry Eye Screening during Medical Health checkups. Investig. Ophthalmol. Vis. Sci. 2016, 57, 2852. [Google Scholar]
- Shigeyasu, C.; Yamada, M.; Kawashima, M.; Suwaki, K.; Uchino, M.; Hiratsuka, Y.; Yokoi, N.; Tsubota, K.; DECS-J Study Group. Quality of life measures and health utility values among dry eye subgroups. Health Qual. Life Outcomes 2018, 16, 170. [Google Scholar] [CrossRef] [Green Version]
- Sakane, Y.; Yamaguchi, M.; Shiraishi, A. Retrospective Observational Study on Rebamipide Ophthalmic Suspension on Quality of Life of Dry Eye Disease Patients. J. Ophthalmol. 2019, 2019, 8145731. [Google Scholar] [CrossRef] [Green Version]
- Kawashima, M.; Yamada, M.; Shigeyasu, C.; Suwaki, K.; Uchino, M.; Hiratsuka, Y.; Yokoi, N.; Tsubota, K. Association of Systemic Comorbidities with Dry Eye Disease. J. Clin. Med. Res. 2020, 9, 40. [Google Scholar] [CrossRef] [PubMed]
- Shimazaki, J.; Yokoi, N.; Watanabe, H.; Amano, S.; Ohashi, Y.; Kinoshita, S.; Shimomura, Y.; Takamura, E.; Hori, Y.; Nishida, K.; et al. Definition and diagnosis of dry eye in Japan, 2016. Atarashii Ganka 2017, 34, 309–313. (In Japanese) [Google Scholar]
- Amano, S.; Arita, R.; Kinoshita, S.; Yokoi, N.; Sotozono, C.; Komuro, A.; Suzuki, T.; Shimazaki, J.; Den, S.; Maeda, N.; et al. Definition and diagnostic criteria for meibomian gland dysfunction. Atarashii Ganka 2010, 27, 627–631. (In Japanese) [Google Scholar]
- Toda, I.; Fujishima, H.; Tsubota, K. Ocular fatigue is the major symptom of dry eye. Acta Ophthalmol. 1993, 71, 347–352. [Google Scholar] [CrossRef]
- Yokoi, N.; Georgiev, G.A.; Kato, H.; Komuro, A.; Sonomura, Y.; Sotozono, C.; Tsubota, K.; Kinoshita, S. Classification of Fluorescein Breakup Patterns: A Novel Method of Differential Diagnosis for Dry Eye. Am. J. Ophthalmol. 2017, 180, 72–85. [Google Scholar] [CrossRef]
- Yokoi, N. TFOD and TFOT Expert Lecture Paradigm Shift in the Clinical Practice for Dry Eye; Medical Review: Osaka, Japan; Tokyo, Japan, 2020. [Google Scholar]
- Koh, S.; Watanabe, H.; Hosohata, J.; Hori, Y.; Hibino, S.; Nishida, K.; Maeda, N.; Tano, Y. Diagnosing dry eye using a blue-free barrier filter. Am. J. Ophthalmol. 2003, 136, 513–519. [Google Scholar] [CrossRef]
- Van Bijsterveld, O.P. Diagnostic tests in the Sicca syndrome. Arch. Ophthalmol. 1969, 82, 10–14. [Google Scholar] [CrossRef]
- Lemp, M.A. Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes. CLAO J. 1995, 21, 221–232. [Google Scholar]
- McDonald, J.E.; Brubaker, S. Meniscus-induced thinning of tear films. Am. J. Ophthalmol. 1971, 72, 139–146. [Google Scholar] [CrossRef]
- Doane, M.G. Blinking and the mechanics of the lacrimal drainage system. Ophthalmology 1981, 88, 844–851. [Google Scholar] [CrossRef]
- Lemp, M.A.; Weiler, H.H. How do tears exit? Invest. Ophthalmol. Vis. Sci. 1983, 24, 619–622. [Google Scholar] [PubMed]
- Liu, D. Conjunctivochalasis. A cause of tearing and its management. Ophthal. Plast. Reconstr. Surg. 1986, 2, 25–28. [Google Scholar] [CrossRef]
- Georgiadis, N.S.; Terzidou, C.D. Epiphora Caused by Conjunctivochalasis. Cornea 2001, 20, 619–621. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, N.; Georgiev, G.A. Tear Film-Oriented Diagnosis and Tear Film-Oriented Therapy for Dry Eye Based on Tear Film Dynamics. Invest. Ophthalmol. Vis. Sci. 2018, 59, DES13–DES22. [Google Scholar] [CrossRef]
- Yokoi, N.; Kato, H.; Kinoshita, S. Facilitation of tear fluid secretion by 3% diquafosol ophthalmic solution in normal human eyes. Am. J. Ophthalmol. 2014, 157, 85–92.e1. [Google Scholar] [CrossRef] [PubMed]
- Takaoka-Shichijo, Y.N.N. Stimulatory effect of diquafosol tetrasodium in the expression of membrane-binding mucin genes in cultured human corneal epithelial cells. Atarasii Gnka 2011, 28, 425–429. (In Japanese) [Google Scholar]
- Shigeyasu, C.; Yamada, M.; Akune, Y. Influence of Ophthalmic Solutions on Tear Components. Cornea 2016, 35 (Suppl. S1), S71–S77. [Google Scholar] [CrossRef] [PubMed]
- Kase, S.; Shinohara, T.; Kase, M. Effect of topical rebamipide on human conjunctival goblet cells. JAMA Ophthalmol. 2014, 132, 1021–1022. [Google Scholar] [CrossRef] [Green Version]
- Itoh, S.; Itoh, K.; Shinohara, H. Regulation of human corneal epithelial mucins by rebamipide. Curr. Eye Res. 2014, 39, 133–141. [Google Scholar] [CrossRef]
- Itakura, H.; Kashima, T.; Itakura, M.; Akiyama, H.; Kishi, S. Topical rebamipide improves lid wiper epitheliopathy. Clin. Ophthalmol. 2013, 7, 2137–2141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aoki, T.; Yokoi, N.; Kato, H.; Komuro, A.; Sonomura, Y.; Sotozono, C. Shigeru Kinoshita Mechanism and Current State of Treatment for Filamentary Keratitis with Dry Eye. Nihon Ganka Gakkai Zasshi. 2019, 123, 1065–1070. [Google Scholar]
- Takahashi, Y.; Ichinose, A.; Kakizaki, H. Topical rebamipide treatment for superior limbic keratoconjunctivitis in patients with thyroid eye disease. Am. J. Ophthalmol. 2014, 157, 807–812.e2. [Google Scholar] [CrossRef] [PubMed]
- Vu, C.H.V.; Kawashima, M.; Yamada, M.; Suwaki, K.; Uchino, M.; Shigeyasu, C.; Hiratsuka, Y.; Yokoi, N.; Tsubota, K. Dry Eye Cross-Sectional Study in Japan Study Group Influence of Meibomian Gland Dysfunction and Friction-Related Disease on the Severity of Dry Eye. Ophthalmology 2018, 125, 1181–1188. [Google Scholar] [CrossRef] [PubMed]
- Hosotani, Y.; Yokoi, N.; Okamoto, M.; Ishikawa, H.; Komuro, A.; Kato, H.; Mimura, O.; Gomi, F. Characteristics of tear abnormalities associated with benign essential blepharospasm and amelioration by means of botulinum toxin type A treatment. Jpn. J. Ophthalmol. 2020, 64, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Prabhasawat, P.; Tseng, S.C. Frequent association of delayed tear clearance in ocular irritation. Br. J. Ophthalmol. 1998, 82, 666–675. [Google Scholar] [CrossRef]
- Fodor, E.; Barabino, S.; Montaldo, E.; Mingari, M.C.; Rolando, M. Quantitative evaluation of ocular surface inflammation in patients with different grade of conjunctivochalasis. Curr. Eye Res. 2010, 35, 665–669. [Google Scholar] [CrossRef]

| CCh (n = 75) | DE (n = 122) | |
|---|---|---|
| Age, years | 67.8 ± 8.5 | 66.2 ± 9.9 |
| Male:Female | 16:59 | 14:108 |
| FBUT, sec | 2.1 ± 1.5 | 2.1 ± 1.4 |
| van Bijsterveld score | 1.3 ± 1.9 | 1.4 ± 1.5 |
| NIH score | 1.5 ± 2.7 | 1.8 ± 2.5 |
| CCh grade | 4.6 ± 1.7 | 1.5 ± 0.7 * |
| Schirmer 1, mm | 11.2 ± 9.0 | 12.9 ± 10.6 |
| Versus | r | p | |
|---|---|---|---|
| QOL score of CCH | Total | 0.75 | p < 0.0001 |
| ITF | 0.79 | p < 0.0001 | |
| IF | 0.70 | p < 0.0001 | |
| R | 0.27 | p = 0.018 | |
| DTC | 0.11 | p = 0.11 | |
| QOL score of DE | Total | 0.75 | p < 0.0001 |
| ITF | 0.72 | p < 0.0001 | |
| IF | 0.71 | p < 0.0001 | |
| R | 0.32 | p < 0.0001 | |
| DTC | 0.35 | p < 0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Komuro, A.; Yokoi, N.; Kato, H.; Sonomura, Y.; Sotozono, C.; Kinoshita, S. The Relationship between Subjective Symptoms and Quality of Life in Conjunctivochalasis Patients. Diagnostics 2021, 11, 179. https://doi.org/10.3390/diagnostics11020179
Komuro A, Yokoi N, Kato H, Sonomura Y, Sotozono C, Kinoshita S. The Relationship between Subjective Symptoms and Quality of Life in Conjunctivochalasis Patients. Diagnostics. 2021; 11(2):179. https://doi.org/10.3390/diagnostics11020179
Chicago/Turabian StyleKomuro, Aoi, Norihiko Yokoi, Hiroaki Kato, Yukiko Sonomura, Chie Sotozono, and Shigeru Kinoshita. 2021. "The Relationship between Subjective Symptoms and Quality of Life in Conjunctivochalasis Patients" Diagnostics 11, no. 2: 179. https://doi.org/10.3390/diagnostics11020179
APA StyleKomuro, A., Yokoi, N., Kato, H., Sonomura, Y., Sotozono, C., & Kinoshita, S. (2021). The Relationship between Subjective Symptoms and Quality of Life in Conjunctivochalasis Patients. Diagnostics, 11(2), 179. https://doi.org/10.3390/diagnostics11020179






