Nerve Ultrasound as Helpful Tool in Polyneuropathies
Abstract
:1. Introduction
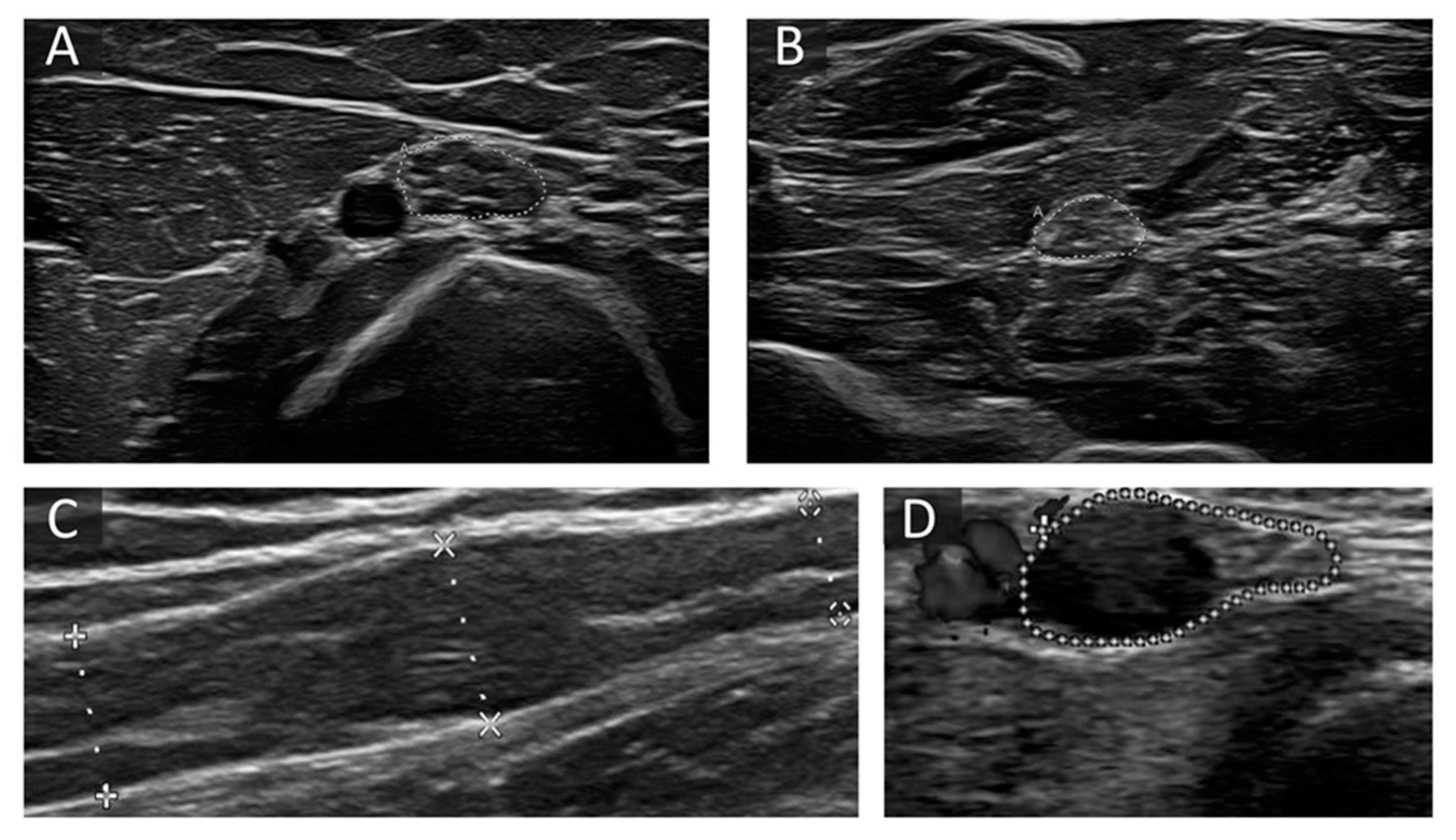
2. Ultrasound Parameters in Neuropathies
3. General Aspects and Examination Protocols
4. Hereditary Neuropathies
5. Hereditary Transthyretin Related and Sporadic Amyloidosis
6. Immune-Mediated Neuropathies
7. Diabetic Neuropathies
8. Other Axonal Neuropathies
9. Neurolymphomatosis and GRAFT Versus Host Diseases
10. Storage Diseases
11. Motor neuron Diseases
12. Scoring Systems
13. Practical Approach Combining Electrophysiology and Nerve Ultrasound
14. Limitations and Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AL | Amyloid light-chain |
| ALS | Amyotrophic lateral sclerosis |
| ATTR | Hereditary transthyretin related amyloidosis |
| BUS | Bochum Ultrasound Score |
| CANVAS | Cerebellar ataxia neuropathy vestibular areflexia syndrome |
| CIDP | Chronic inflammatory demyelinating polyneuropathies |
| CMT | Charcot Marie Tooth |
| CMT1X | X-linked Charcot Marie Tooth type 1 |
| CSA | Cross-sectional area |
| CSF | Cerebrospinal fluid |
| DN | Diabetic neuropathy |
| EFNS | European Federation of Neurological Societies |
| GBS | Guillain-Barre syndrome |
| GvHD | Graft versus host disease |
| HbA1c | Hemoglobin A1c |
| HNPP | Hereditary neuropathy with liability to pressure palsies |
| HRUS | High-resolution nerve ultrasound |
| IgM | Immunoglobulin M |
| IVIG | Intravenous immunoglobulins |
| LSS | Lewis-Sumner Syndrome |
| MADSAM | Multifocal acquired demyelinating sensory and motor neuropathy |
| MAG | Myelin associated glycoprotein |
| MFS | Miller Fisher syndrome |
| MGUS | Monoclonal gammopathy of undetermined significance |
| MMN | Multifocal motor neuropathy |
| MPZ | Myelin protein zero |
| MR | Magnetic Resonance |
| MRI | Magnetic Resonance Imaging |
| NCS | Nerve conduction study |
| NEFL | Neurofilament light polypeptide gene |
| NUP | Neuropathy Ultrasound Protocol |
| PET | Positron emission tomography |
| PLS | Primary lateral sclerosis |
| PMP22 | Peripheral myelin protein 22 |
| PNP | Polyneuropathies |
| PNS | Peripheral nerve system |
| POEMS | polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, skin changes |
| RNA | Ribonucleic acid |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus type 2 |
| SFN | Small fiber neuropathy |
| TTR | Hereditary Transthyretin |
| UPSS | Ultrasound pattern sum score |
References
- Joint Task Force of the EFNS and the PNS European Federation of Neurological Societies/Peripheral Nerve Society guideline on management of multifocal motor neuropathy. Report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society—First revision. J. Peripher. Nerv. Syst. 2010, 15, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Kollmer, J.; Hund, E.; Hornung, B.; Hegenbart, U.; Schonland, S.O.; Kimmich, C.; Kristen, A.V.; Purrucker, J.; Rocken, C.; Heiland, S.; et al. In vivo detection of nerve injury in familial amyloid polyneuropathy by magnetic resonance neurography. Brain 2015, 138, 549–562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Decard, B.F.; Pham, M.; Grimm, A. Ultrasound and MRI of nerves for monitoring disease activity and treatment effects in chronic dysimmune neuropathies-Current concepts and future directions. Clin. Neurophysiol. 2018, 129, 155–167. [Google Scholar] [CrossRef] [PubMed]
- Baute Penry, V.; Cartwright, M.S. Neuromuscular Ultrasound for Peripheral Neuropathies. Semin. Neurol. 2019, 39, 542–548. [Google Scholar] [CrossRef]
- Telleman, J.A.; Grimm, A.; Goedee, S.; Visser, L.H.; Zaidman, C.M. Nerve ultrasound in polyneuropathies. Muscle Nerve 2018, 57, 716–728. [Google Scholar] [CrossRef] [Green Version]
- Walker, F.O.; Cartwright, M.S.; Alter, K.E.; Visser, L.H.; Hobson-Webb, L.D.; Padua, L.; Strakowski, J.A.; Preston, D.C.; Boon, A.J.; Axer, H.; et al. Indications for neuromuscular ultrasound: Expert opinion and review of the literature. Clin. Neurophysiol. 2018, 129, 2658–2679. [Google Scholar] [CrossRef]
- Dengler, R.; De Carvalho, M.; Shahrizaila, N.; Nodera, H.; Vucic, S.; Grimm, A.; Padua, L.; Schreiber, S.; Kneiser, M.K.; Hobson-Webb, L.D.; et al. AANEM-IFCN Glossary of Terms in Neuromuscular Electrodiagnostic Medicine and Ultrasound. Muscle Nerve 2020, 62, 10–12. [Google Scholar] [CrossRef]
- Grimm, A.; Winter, N.; Rattay, T.W.; Hartig, F.; Dammeier, N.M.; Auffenberg, E.; Koch, M.; Axer, H. A look inside the nerve-Morphology of nerve fascicles in healthy controls and patients with polyneuropathy. Clin. Neurophysiol. 2017, 128, 2521–2526. [Google Scholar] [CrossRef]
- Rattay, T.W.; Winter, N.; Décard, B.F.; Dammeier, N.M.; Härtig, F.; Ceanga, M.; Axer, H.; Grimm, A. Nerve ultrasound as follow-up tool in treated multifocal motor neuropathy. Eur. J. Neurol. 2017, 24, 1125–1134. [Google Scholar] [CrossRef]
- Cartwright, M.S.; Baute, V.; Caress, J.B.; Walker, F.O. Ultrahigh-frequency ultrasound of fascicles in the median nerve at the wrist. Muscle Nerve 2017, 56, 819–822. [Google Scholar] [CrossRef]
- Padua, L.; Granata, G.; Sabatelli, M.; Inghilleri, M.; Lucchetta, M.; Luigetti, M.; Coraci, D.; Martinoli, C.; Briani, C. Heterogeneity of root and nerve ultrasound pattern in CIDP patients. Clin. Neurophysiol. 2014, 125, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Hartig, F.; Ross, M.; Dammeier, N.M.; Fedtke, N.; Heiling, B.; Axer, H.; Decard, B.F.; Auffenberg, E.; Koch, M.; Rattay, T.W.; et al. Nerve Ultrasound Predicts Treatment Response in Chronic Inflammatory Demyelinating Polyradiculoneuropathy-a Prospective Follow-Up. Neurotherapeutics 2018, 15, 439–451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisse, A.L.; Pitarokoili, K.; Motte, J.; Gamber, D.; Kerasnoudis, A.; Gold, R.; Yoon, M.S. Nerve echogenicity and intranerve CSA variability in high-resolution nerve ultrasound (HRUS) in chronic inflammatory demyelinating polyneuropathy (CIDP). J. Neurol. 2019, 266, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Gamber, D.; Motte, J.; Kerasnoudis, A.; Yoon, M.S.; Gold, R.; Pitarokoili, K.; Fisse, A.L. High-Resolution Nerve Ultrasound to Assess Nerve Echogenicity, Fascicular Count, and Cross-Sectional Area Using Semiautomated Analysis. J. Neuroimaging 2020, 30, 493–502. [Google Scholar] [CrossRef]
- Goedee, H.S.; Brekelmans, G.J.; Visser, L.H. Multifocal enlargement and increased vascularization of peripheral nerves detected by sonography in CIDP: A pilot study. Clin. Neurophysiol. 2014, 125, 154–159. [Google Scholar] [CrossRef]
- He, Y.; Xiang, X.; Zhu, B.H.; Qiu, L. Shear wave elastography evaluation of the median and tibial nerve in diabetic peripheral neuropathy. Quant. Imaging Med. Surg. 2019, 9, 273–282. [Google Scholar] [CrossRef]
- Boehm, J.; Scheidl, E.; Bereczki, D.; Schelle, T.; Aranyi, Z. High-resolution ultrasonography of peripheral nerves: Measurements on 14 nerve segments in 56 healthy subjects and reliability assessments. Ultraschall Med. 2014, 35, 459–467. [Google Scholar] [CrossRef] [Green Version]
- Cartwright, M.S.; Passmore, L.V.; Yoon, J.S.; Brown, M.E.; Caress, J.B.; Walker, F.O. Cross-sectional area reference values for nerve ultrasonography. Muscle Nerve 2008, 37, 566–571. [Google Scholar] [CrossRef]
- Grimm, A.; Axer, H.; Heiling, B.; Winter, N. Nerve ultrasound normal values-Readjustment of the ultrasound pattern sum score UPSS. Clin. Neurophysiol. 2018, 129, 1403–1409. [Google Scholar] [CrossRef]
- Tagliafico, A.; Martinoli, C. Reliability of side-to-side sonographic cross-sectional area measurements of upper extremity nerves in healthy volunteers. J. Ultrasound Med. 2013, 32, 457–462. [Google Scholar] [CrossRef]
- Padua, L.; Martinoli, C.; Pazzaglia, C.; Lucchetta, M.; Granata, G.; Erra, C.; Briani, C. Intra- and internerve cross-sectional area variability: New ultrasound measures. Muscle Nerve 2012, 45, 730–733. [Google Scholar] [CrossRef] [PubMed]
- Qrimli, M.; Ebadi, H.; Breiner, A.; Siddiqui, H.; Alabdali, M.; Abraham, A.; Lovblom, L.E.; Perkins, B.A.; Bril, V. Reference values for ultrasonograpy of peripheral nerves. Muscle Nerve 2016, 53, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Kerasnoudis, A.; Pitarokoili, K.; Behrendt, V.; Gold, R.; Yoon, M.S. Cross sectional area reference values for sonography of peripheral nerves and brachial plexus. Clin. Neurophysiol. 2013, 124, 1881–1888. [Google Scholar] [CrossRef] [PubMed]
- Schubert, C.; Grimm, A.S.; Stahl, J.H.; Kupper, H.; Kegele, J.; Wittlinger, J.; Serna-Higuita, L.; Winter, N.; Groeschel, S.; Grimm, A. Nerve ultrasound reference data in children from two to seven years. Clin. Neurophysiol. 2020, 131, 859–865. [Google Scholar] [CrossRef]
- Druzhinin, D.; Naumova capital Ie, C.; Nikitin, S. Nerve ultrasound normal values in children and young adults. Muscle Nerve 2019, 60, 757–761. [Google Scholar] [CrossRef]
- Bathala, L.; Kumar, P.; Kumar, K.; Visser, L.H. Ultrasonographic cross-sectional area normal values of the ulnar nerve along its course in the arm with electrophysiological correlations in 100 Asian subjects. Muscle Nerve 2013, 47, 673–676. [Google Scholar] [CrossRef]
- Grimm, A.S.; Schubert, C.; Grimm, A.; Stahl, J.H.; Küpper, H.; Horber, V.; Kegele, J.; Willikens, S.; Wittlinger, J.; Serna-Higuita, L.; et al. Normative Observational Nerve Ultrasound Values in School-Age Children and Adolescents and Their Application to Hereditary Neuropathies. Front. Neurol. 2020, 11, 303. [Google Scholar] [CrossRef]
- Martinoli, C.; Schenone, A.; Bianchi, S.; Mandich, P.; Caponetto, C.; Abbruzzese, M.; Derchi, L.E. Sonography of the median nerve in Charcot-Marie-Tooth disease. AJR Am. J. Roentgenol. 2002, 178, 1553–1556. [Google Scholar] [CrossRef]
- Pazzaglia, C.; Minciotti, I.; Coraci, D.; Briani, C.; Padua, L. Ultrasound assessment of sural nerve in Charcot-Marie-Tooth 1A neuropathy. Clin. Neurophysiol. 2013, 124, 1695–1699. [Google Scholar] [CrossRef]
- Schreiber, S.; Oldag, A.; Kornblum, C.; Kollewe, K.; Kropf, S.; Schoenfeld, A.; Feistner, H.; Jakubiczka, S.; Kunz, W.S.; Scherlach, C.; et al. Sonography of the median nerve in CMT1A, CMT2A, CMTX, and HNPP. Muscle Nerve 2013, 47, 385–395. [Google Scholar] [CrossRef]
- Goedee, S.H.; Brekelmans, G.J.; van den Berg, L.H.; Visser, L.H. Distinctive patterns of sonographic nerve enlargement in Charcot-Marie-Tooth type 1A and hereditary neuropathy with pressure palsies. Clin. Neurophysiol. 2015, 126, 1413–1420. [Google Scholar] [CrossRef] [PubMed]
- Noto, Y.; Shiga, K.; Tsuji, Y.; Mizuta, I.; Higuchi, Y.; Hashiguchi, A.; Takashima, H.; Nakagawa, M.; Mizuno, T. Nerve ultrasound depicts peripheral nerve enlargement in patients with genetically distinct Charcot-Marie-Tooth disease. J. Neurol. Neurosurg Psychiatry 2015, 86, 378–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yiu, E.M.; Brockley, C.R.; Lee, K.J.; Carroll, K.; de Valle, K.; Kennedy, R.; Rao, P.; Delatycki, M.B.; Ryan, M.M. Peripheral nerve ultrasound in pediatric Charcot-Marie-Tooth disease type 1A. Neurology 2015, 84, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Zaidman, C.M.; Harms, M.B.; Pestronk, A. Ultrasound of inherited vs. acquired demyelinating polyneuropathies. J. Neurol. 2013, 260, 3115–3121. [Google Scholar] [CrossRef] [Green Version]
- Sugimoto, T.; Ochi, K.; Hosomi, N.; Takahashi, T.; Ueno, H.; Nakamura, T.; Nagano, Y.; Maruyama, H.; Kohriyama, T.; Matsumoto, M. Ultrasonographic nerve enlargement of the median and ulnar nerves and the cervical nerve roots in patients with demyelinating Charcot-Marie-Tooth disease: Distinction from patients with chronic inflammatory demyelinating polyneuropathy. J. Neurol. 2013, 260, 2580–2587. [Google Scholar] [CrossRef]
- Grimm, A.; Rasenack, M.; Athanasopoulou, I.M.; Dammeier, N.M.; Lipski, C.; Wolking, S.; Vittore, D.; Décard, B.F.; Axer, H. The modified ultrasound pattern sum score mUPSS as additional diagnostic tool for genetically distinct hereditary neuropathies. J. Neurol. 2016, 263, 221–230. [Google Scholar] [CrossRef]
- Zanette, G.; Fabrizi, G.M.; Taioli, F.; Lauriola, M.F.; Badari, A.; Ferrarini, M.; Cavallaro, T.; Tamburin, S. Nerve ultrasound findings differentiate Charcot-Marie-Tooth disease (CMT) 1A from other demyelinating CMTs. Clin. Neurophysiol. 2018, 129, 2259–2267. [Google Scholar] [CrossRef]
- Zanette, G.; Tamburin, S.; Taioli, F.; Lauriola, M.F.; Badari, A.; Ferrarini, M.; Cavallaro, T.; Fabrizi, G.M. Nerve size correlates with clinical severity in Charcot-Marie-Tooth disease 1A. Muscle Nerve 2019, 60, 744–748. [Google Scholar] [CrossRef]
- Cartwright, M.S.; Brown, M.E.; Eulitt, P.; Walker, F.O.; Lawson, V.H.; Caress, J.B. Diagnostic nerve ultrasound in Charcot-Marie-Tooth disease type 1B. Muscle Nerve 2009, 40, 98–102. [Google Scholar] [CrossRef]
- Luigetti, M.; Sabatelli, M.; Bellone, E.; Fabrizi, G.M.; Padua, L.; Granata, G. Nerve ultrasound in patients with CMT1C: Description of 3 cases. Muscle Nerve 2015, 51, 781–782. [Google Scholar] [CrossRef]
- Castoro, R.; Crisp, J.; Caress, J.B.; Li, J.; Cartwright, M.S. Segmental nerve enlargement in CMT4J. Muscle Nerve 2020, 61, E44–E46. [Google Scholar] [CrossRef] [PubMed]
- Pimentel, N.; Tiongson, E.; Mitchell, W.; Ramos-Platt, L. Case Series: Pediatric Patients with Concomitant Genetic Neuropathy Syndromes and Immune Mediated Polyneuropathy. (1073). Neurology 2020, 94, 1073. [Google Scholar]
- Dyck, P.J.; Swanson, C.J.; Low, P.A.; Bartleson, J.D.; Lambert, E.H. Prednisone-responsive hereditary motor and sensory neuropathy. Mayo Clin. Proc. 1982, 57, 239–246. [Google Scholar] [PubMed]
- Martini, R.; Toyka, K.V. Immune-mediated components of hereditary demyelinating neuropathies: Lessons from animal models and patients. Lancet Neurol. 2004, 3, 457–465. [Google Scholar] [CrossRef]
- Grimm, A.; Winter, N.; Wolking, S.; Vittore, D.; Biskup, S.; Axer, H. Nerve enlargement in an unusual case of inflammatory neuropathy and new gene mutation-morphology is the key. Neurol. Sci. 2017, 38, 1525–1527. [Google Scholar] [CrossRef] [PubMed]
- Hooper, D.R.; Lawson, W.; Smith, L.; Baker, S.K. Sonographic features in hereditary neuropathy with liability to pressure palsies. Muscle Nerve 2011, 44, 862–867. [Google Scholar] [CrossRef]
- Beekman, R.; Visser, L.H. Sonographic detection of diffuse peripheral nerve enlargement in hereditary neuropathy with liability to pressure palsies. J. Clin. Ultrasound 2002, 30, 433–436. [Google Scholar] [CrossRef]
- Kim, S.H.; Yang, S.N.; Yoon, J.S.; Park, B.J. Sonographic evaluation of the peripheral nerves in hereditary neuropathy with liability to pressure palsies: A case report. Ann. Rehabil. Med. 2014, 38, 109–115. [Google Scholar] [CrossRef] [Green Version]
- Bayrak, A.O.; Bayrak, I.K.; Battaloglu, E.; Ozes, B.; Yildiz, O.; Onar, M.K. Ultrasonographic findings in hereditary neuropathy with liability to pressure palsies. Neurol. Res. 2015, 37, 106–111. [Google Scholar] [CrossRef]
- Ginanneschi, F.; Filippou, G.; Giannini, F.; Carluccio, M.A.; Adinolfi, A.; Frediani, B.; Dotti, M.T.; Rossi, A. Sonographic and electrodiagnostic features of hereditary neuropathy with liability to pressure palsies. J. Peripher. Nerv. Syst. 2012, 17, 391–398. [Google Scholar] [CrossRef]
- Dohrn, M.F.; Auer-Grumbach, M.; Baron, R.; Birklein, F.; Escolano-Lozano, F.; Geber, C.; Grether, N.; Hagenacker, T.; Hund, E.; Sachau, J.; et al. Chance or challenge, spoilt for choice? New recommendations on diagnostic and therapeutic considerations in hereditary transthyretin amyloidosis with polyneuropathy: The German/Austrian position and review of the literature. J. Neurol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Gertz, M.A.; Mauermann, M.L.; Grogan, M.; Coelho, T. Advances in the treatment of hereditary transthyretin amyloidosis: A review. Brain. Behav. 2019, 9, e01371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moshe-Lilie, O.; Dimitrova, D.; Heitner, S.B.; Brannagan, T.H., 3rd; Zivkovic, S.; Hanna, M.; Masri, A.; Polydefkis, M.; Berk, J.L.; Gertz, M.A.; et al. TTR gene silencing therapy in post liver transplant hereditary ATTR amyloidosis patients. Amyloid 2020, 27, 250–253. [Google Scholar] [CrossRef] [PubMed]
- Granata, G.; Luigetti, M.; Coraci, D.; Del Grande, A.; Romano, A.; Bisogni, G.; Bramanti, P.; Rossini, P.M.; Sabatelli, M.; Padua, L. Ultrasound evaluation in transthyretin-related amyloid neuropathy. Muscle Nerve 2014, 50, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Podnar, S.; Sarafov, S.; Tournev, I.; Omejec, G.; Zidar, J. Peripheral nerve ultrasonography in patients with transthyretin amyloidosis. Clin. Neurophysiol. 2017, 128, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Salvalaggio, A.; Coraci, D.; Cacciavillani, M.; Obici, L.; Mazzeo, A.; Luigetti, M.; Pastorelli, F.; Grandis, M.; Cavallaro, T.; Bisogni, G.; et al. Nerve ultrasound in hereditary transthyretin amyloidosis: Red flags and possible progression biomarkers. J. Neurol. 2020. [Google Scholar] [CrossRef]
- Rasenack, M.; Proebstel, A.K.; Athanasopoulou, I.M.; Decard, B.F.; Grimm, A. Nerve Hypertrophy in Primary Amyloidosis. Muscle Nerve 2016, 54, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Zaidman, C.M.; Al-Lozi, M.; Pestronk, A. Peripheral nerve size in normals and patients with polyneuropathy: An ultrasound study. Muscle Nerve 2009, 40, 960–966. [Google Scholar] [CrossRef]
- Di Pasquale, A.; Morino, S.; Loreti, S.; Bucci, E.; Vanacore, N.; Antonini, G. Peripheral nerve ultrasound changes in CIDP and correlations with nerve conduction velocity. Neurology 2015, 84, 803–809. [Google Scholar] [CrossRef]
- Tazawa, K.; Matsuda, M.; Yoshida, T.; Shimojima, Y.; Gono, T.; Morita, H.; Kaneko, T.; Ueda, H.; Ikeda, S. Spinal nerve root hypertrophy on MRI: Clinical significance in the diagnosis of chronic inflammatory demyelinating polyradiculoneuropathy. Intern. Med. 2008, 47, 2019–2024. [Google Scholar] [CrossRef] [Green Version]
- Adachi, Y.; Sato, N.; Okamoto, T.; Sasaki, M.; Komaki, H.; Yamashita, F.; Kida, J.; Takahashi, T.; Matsuda, H. Brachial and lumbar plexuses in chronic inflammatory demyelinating polyradiculoneuropathy: MRI assessment including apparent diffusion coefficient. Neuroradiology 2011, 53, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, C.D.; Miranda, M.A.; Cowley, P.; Morrow, J.M.; Davagnanam, I.; Mehta, H.; Hanna, M.G.; Koltzenburg, M.; Reilly, M.M.; Yousry, T.A.; et al. MRI shows increased sciatic nerve cross sectional area in inherited and inflammatory neuropathies. J. Neurol. Neurosurg. Psychiatry 2011, 82, 1283–1286. [Google Scholar] [CrossRef] [PubMed]
- Lozeron, P.; Lacour, M.C.; Vandendries, C.; Theaudin, M.; Cauquil, C.; Denier, C.; Lacroix, C.; Adams, D. Contribution of plexus MRI in the diagnosis of atypical chronic inflammatory demyelinating polyneuropathies. J. Neurol. Sci. 2016, 360, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Grimm, A.; Vittore, D.; Schubert, V.; Rasenack, M.; Décard, B.F.; Heiling, B.; Hammer, N.; Axer, H. Ultrasound aspects in therapy-naive CIDP compared to long-term treated CIDP. J. Neurol. 2016, 263, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Kerasnoudis, A.; Pitarokoili, K.; Behrendt, V.; Gold, R.; Yoon, M.S. Correlation of nerve ultrasound, electrophysiological and clinical findings in chronic inflammatory demyelinating polyneuropathy. J. Neuroimaging 2015, 25, 207–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imamura, K.; Tajiri, Y.; Kowa, H.; Nakashima, K. Peripheral nerve hypertrophy in chronic inflammatory demyelinating polyradiculoneuropathy detected by ultrasonography. Intern. Med. 2009, 48, 581–582. [Google Scholar] [CrossRef] [Green Version]
- Goedee, H.S.; van der Pol, W.L.; van Asseldonk, J.H.; Franssen, H.; Notermans, N.C.; Vrancken, A.J.; van Es, M.A.; Nikolakopoulos, S.; Visser, L.H.; van den Berg, L.H. Diagnostic value of sonography in treatment-naive chronic inflammatory neuropathies. Neurology 2017, 88, 143–151. [Google Scholar] [CrossRef]
- Herraets, I.J.T.; Goedee, H.S.; Telleman, J.A.; van Eijk, R.P.A.; Verhamme, C.; Saris, C.G.J.; Eftimov, F.; van Alfen, N.; van Asseldonk, J.T.; Visser, L.H.; et al. Nerve ultrasound for diagnosing chronic inflammatory neuropathy: A multicenter validation study. Neurology 2020, 95, e1745–e1753. [Google Scholar] [CrossRef]
- Schreiber, S.; Schreiber, F.; Peter, A.; Isler, E.; Dorner, M.; Heinze, H.J.; Petri, S.; Tempelmann, C.; Nestor, P.J.; Grimm, A.; et al. 7T MR neurography-ultrasound fusion for peripheral nerve imaging. Muscle Nerve 2020, 61, 521–526. [Google Scholar] [CrossRef]
- Oudeman, J.; Eftimov, F.; Strijkers, G.J.; Schneiders, J.J.; Roosendaal, S.D.; Engbersen, M.P.; Froeling, M.; Goedee, H.S.; van Doorn, P.A.; Caan, M.W.A.; et al. Diagnostic accuracy of MRI and ultrasound in chronic immune-mediated neuropathies. Neurology 2020, 94, e62–e74. [Google Scholar] [CrossRef]
- Goedee, H.S.; Herraets, I.J.T.; Visser, L.H.; Franssen, H.; van Asseldonk, J.H.; van der Pol, W.L.; van den Berg, L.H. Nerve ultrasound can identify treatment-responsive chronic neuropathies without electrodiagnostic features of demyelination. Muscle Nerve 2019, 60, 415–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herraets, I.J.T.; Goedee, H.S.; Telleman, J.A.; van Eijk, R.P.A.; van Asseldonk, J.T.; Visser, L.H.; van den Berg, L.H.; van der Pol, W.L. Nerve ultrasound improves detection of treatment-responsive chronic inflammatory neuropathies. Neurology 2020, 94, e1470–e1479. [Google Scholar] [CrossRef] [PubMed]
- Winter, N.; Dammeier, N.; Schäffer, E.; Bornemann, A.; Stahl, J.H.; Herlan, S.; Schuhmann, M.U.; Grimm, A. Nerve Ultrasonography as an Additive Tool to Clinical Examination and Electrodiagnostics in Sporadic Mononeuritis-Imaging is the Key. Ultraschall Med. 2019, 40, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Zaidman, C.M.; Pestronk, A. Nerve size in chronic inflammatory demyelinating neuropathy varies with disease activity and therapy response over time: A retrospective ultrasound study. Muscle Nerve 2014, 50, 733–738. [Google Scholar] [CrossRef] [Green Version]
- Kerasnoudis, A.; Pitarokoili, K.; Gold, R.; Yoon, M.S. Nerve Ultrasound and Electrophysiology for Therapy Monitoring in Chronic Inflammatory Demyelinating Polyneuropathy. J. Neuroimaging 2015, 25, 931–939. [Google Scholar] [CrossRef]
- Hokkoku, K.; Matsukura, K.; Uchida, Y.; Kuwabara, M.; Furukawa, Y.; Tsukamoto, H.; Hatanaka, Y.; Sonoo, M. Quantitative muscle ultrasound is useful for evaluating secondary axonal degeneration in chronic inflammatory demyelinating polyneuropathy. Brain Behav. 2017, 7, e00812. [Google Scholar] [CrossRef] [Green Version]
- Puma, A.; Azulay, N.; Grecu, N.; Suply, C.; Panicucci, E.; Cambieri, C.; Villa, L.; Raffaelli, C.; Sacconi, S. Comparison of high-frequency and ultrahigh-frequency probes in chronic inflammatory demyelinating polyneuropathy. J. Neurol. 2019, 266, 2277–2285. [Google Scholar] [CrossRef]
- Athanasopoulos, D.; Motte, J.; Fisse, A.L.; Grueter, T.; Trampe, N.; Sturm, D.; Tegenthoff, M.; Sgodzai, M.; Klimas, R.; Querol, L.; et al. Longitudinal study on nerve ultrasound and corneal confocal microscopy in NF155 paranodopathy. Ann. Clin. Transl. Neurol. 2020, 7, 1061–1068. [Google Scholar] [CrossRef]
- Franques, J.; Chapon, F.; Devaux, J.; Mathis, S. Teaching NeuroImages: Cranial nerve hypertrophy in IgG4 anti-neurofascin 155 antibody-positive polyneuropathy. Neurology 2017, 88, e52. [Google Scholar] [CrossRef] [Green Version]
- Simon, N.G.; Kiernan, M.C. Precise correlation between structural and electrophysiological disturbances in MADSAM neuropathy. Neuromuscul. Disord. NMD 2015, 25, 904–907. [Google Scholar] [CrossRef]
- Kerasnoudis, A. Ultrasonography of MADSAM neuropathy: Focal nerve enlargements at sites of existing and resolved conduction blocks. Neuromuscul. Disord. NMD 2012, 22, 1032. [Google Scholar] [CrossRef] [PubMed]
- Scheidl, E.; Böhm, J.; Simó, M.; Rózsa, C.; Bereznai, B.; Kovács, T.; Arányi, Z. Ultrasonography of MADSAM neuropathy: Focal nerve enlargements at sites of existing and resolved conduction blocks. Neuromuscul. Disord. NMD 2012, 22, 627–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neubauer, C.; Gruber, H.; Bauerle, J.; Egger, K. Ultrasonography of Multifocal Acquired Demyelinating Sensory and Motor Neuropathy (MADSAM). Clin. Neuroradiol. 2015, 25, 423–425. [Google Scholar] [CrossRef] [PubMed]
- Grimm, A.; Thomaser, A.L.; Peters, N.; Fuhr, P. Neurological picture. Vagal hypertrophy in immune-mediated neuropathy visualised with high-resolution ultrasound (HR-US). J. Neurol. Neurosurg. Psychiatry 2015, 86, 1277–1278. [Google Scholar] [CrossRef]
- Granata, G.; Pazzaglia, C.; Calandro, P.; Luigetti, M.; Martinoli, C.; Sabatelli, M.; Padua, L. Ultrasound visualization of nerve morphological alteration at the site of conduction block. Muscle Nerve 2009, 40, 1068–1070. [Google Scholar] [CrossRef]
- Dorner, M.; Schreiber, F.; Stephanik, H.; Tempelmann, C.; Winter, N.; Stahl, J.H.; Wittlinger, J.; Willikens, S.; Kramer, M.; Heinze, H.J.; et al. Peripheral Nerve Imaging Aids in the Diagnosis of Immune-Mediated Neuropathies-A Case Series. Diagnostics 2020, 10, 535. [Google Scholar] [CrossRef]
- Grimm, A.; Vittore, D.; Schubert, V.; Lipski, C.; Heiling, B.; Decard, B.F.; Axer, H. Ultrasound pattern sum score, homogeneity score and regional nerve enlargement index for differentiation of demyelinating inflammatory and hereditary neuropathies. Clin. Neurophysiol. 2016, 127, 2618–2624. [Google Scholar] [CrossRef]
- Kerasnoudis, A.; Pitarokoili, K.; Gold, R.; Yoon, M.S. Bochum ultrasound score allows distinction of chronic inflammatory from multifocal acquired demyelinating polyneuropathies. J. Neurol. Sci. 2015, 348, 211–215. [Google Scholar] [CrossRef]
- Tanaka, K.; Ota, N.; Harada, Y.; Wada, I.; Suenaga, T. Normalization of sonographical multifocal nerve enlargements in a MADSAM patient following a good clinical response to intravenous immunoglobulin. Neuromuscul. Disord. NMD 2016, 26, 619–623. [Google Scholar] [CrossRef]
- Grimm, A.; Rasenack, M.; Athanasopoulou, I.; Peters, N.; Fuhr, P. Long-term observations in asymmetric immune-mediated neuropathy with vagus hypertrophy using ultrasound of the nerves. J. Neurol. Sci. 2015, 356, 205–208. [Google Scholar] [CrossRef]
- Mauermann, M.L. Paraproteinemic neuropathies. Continuum 2014, 20, 1307–1322. [Google Scholar] [CrossRef] [PubMed]
- Nobile-Orazio, E.; Bianco, M.; Nozza, A. Advances in the Treatment of Paraproteinemic Neuropathy. Curr. Treat. Options Neurol. 2017, 19, 43. [Google Scholar] [CrossRef] [PubMed]
- Athanasopoulou, I.M.; Rasenack, M.; Grimm, C.; Axer, H.; Sinnreich, M.; Décard, B.F.; Grimm, A. Ultrasound of the nerves-An appropriate addition to nerve conduction studies to differentiate paraproteinemic neuropathies. J. Neurol. Sci. 2016, 362, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Lucchetta, M.; Padua, L.; Granata, G.; Luigetti, M.; Campagnolo, M.; Dalla Torre, C.; Coraci, D.; Sabatelli, M.; Briani, C. Nerve ultrasound findings in neuropathy associated with anti-myelin-associated glycoprotein antibodies. Eur. J. Neurol. 2015, 22, 193–202. [Google Scholar] [CrossRef]
- Vu, Q.D.; Cartwright, M.S. Neuromuscular ultrasound findings in distal acquired demyelinating symmetric variant of chronic inflammatory demyelinating polyneuropathy. Muscle Nerve 2017, 56, E44–E45. [Google Scholar] [CrossRef]
- Lucchetta, M.; Pazzaglia, C.; Granata, G.; Briani, C.; Padua, L. Ultrasound evaluation of peripheral neuropathy in POEMS syndrome. Muscle Nerve 2011, 44, 868–872. [Google Scholar] [CrossRef]
- Mitsuma, S.; Misawa, S.; Shibuya, K.; Isose, S.; Sekiguchi, Y.; Iwai, Y.; Beppu, M.; Watanabe, K.; Amino, H.; Kuwabara, S. Altered axonal excitability properties and nerve edema in POEMS syndrome. Clin. Neurophysiol. 2015, 126, 2014–2018. [Google Scholar] [CrossRef] [Green Version]
- Vlam, L.; Van Der Pol, W.L.; Cats, E.A.; Straver, D.C.; Piepers, S.; Franssen, H.; van den Berg, L.H. Multifocal motor neuropathy: Diagnosis, pathogenesis and treatment strategies. Nat. Rev. Neurol. 2011, 8, 48–58. [Google Scholar] [CrossRef]
- Harschnitz, O.; Jongbloed, B.A.; Franssen, H.; Straver, D.C.; van der Pol, W.L.; van den Berg, L.H. MMN: From immunological cross-talk to conduction block. J. Clin. Immunol. 2014, 34 (Suppl. 1), S112–S119. [Google Scholar] [CrossRef] [Green Version]
- Harschnitz, O.; Van den Berg, L.H.; Johansen, L.E.; Jansen, M.D.; Kling, S.; Vieira de Sa, R.; Vlam, L.; van Rheenen, W.; Karst, H.; Wierenga, C.J.; et al. Autoantibody pathogenicity in a multifocal motor neuropathy induced pluripotent stem cell-derived model. Ann. Neurol. 2016, 80, 71–88. [Google Scholar] [CrossRef]
- Beekman, R.; van den Berg, L.H.; Franssen, H.; Visser, L.H.; van Asseldonk, J.T.; Wokke, J.H. Ultrasonography shows extensive nerve enlargements in multifocal motor neuropathy. Neurology 2005, 65, 305–307. [Google Scholar] [CrossRef] [PubMed]
- Grimm, A.; Décard, B.F.; Athanasopoulou, I.; Schweikert, K.; Sinnreich, M.; Axer, H. Nerve ultrasound for differentiation between amyotrophic lateral sclerosis and multifocal motor neuropathy. J. Neurol. 2015, 262, 870–880. [Google Scholar] [CrossRef] [PubMed]
- Loewenbruck, K.F.; Liesenberg, J.; Dittrich, M.; Schafer, J.; Patzner, B.; Trausch, B.; Machetanz, J.; Hermann, A.; Storch, A. Nerve ultrasound in the differentiation of multifocal motor neuropathy (MMN) and amyotrophic lateral sclerosis with predominant lower motor neuron disease (ALS/LMND). J. Neurol. 2016, 263, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Nodera, H.; Izumi, Y.; Takamatsu, N.; Kaji, R. Cervical root sonography to differentiate multifocal motor neuropathy from ALS. J. Med. Investig. 2016, 63, 104–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerasnoudis, A.; Pitarokoili, K.; Behrendt, V.; Gold, R.; Yoon, M.S. Correlation of nerve ultrasound, electrophysiological, and clinical findings in post Guillain-Barre syndrome. J. Peripher. Nerv. Syst. 2013, 18, 232–240. [Google Scholar] [CrossRef]
- Kerasnoudis, A.; Klasing, A.; Behrendt, V.; Gold, R.; Yoon, M.S. Intra- and internerve cross-sectional area variability: New ultrasound measures. Muscle Nerve 2013, 47, 146–147. [Google Scholar] [CrossRef]
- de Leeuw, C.; Wijntjes, J.; Lassche, S.; van Alfen, N. Nerve ultrasound for distinguishing inflammatory neuropathy from amyotrophic lateral sclerosis: Not black and white. Muscle Nerve 2020, 61, E33–e37. [Google Scholar] [CrossRef]
- Schreiber, S.; Vielhaber, S.; Schreiber, F.; Cartwright, M.S. Peripheral nerve imaging in amyotrophic lateral sclerosis. Clin. Neurophysiol. 2020, 131, 2315–2326. [Google Scholar] [CrossRef]
- Wakerley, B.R.; Uncini, A.; Yuki, N. Guillain-Barré and Miller Fisher syndromes--new diagnostic classification. Nat. Rev. Neurol. 2014, 10, 537–544. [Google Scholar] [CrossRef]
- De Sanctis, P.; Doneddu, P.E.; Vigano, L.; Selmi, C.; Nobile-Orazio, E. Guillain-Barre syndrome associated with SARS-CoV-2 infection. A systematic review. Eur. J. Neurol. 2020, 27, 2361–2370. [Google Scholar] [CrossRef]
- Mohite, D.; Omole, J.A.; Bhatti, K.S.; Kaleru, T.; Khan, S. The Association of Anti-Ganglioside Antibodies in the Pathogenesis and Development of Zika-Associated Guillain-Barre Syndrome. Cureus 2020, 12, e8983. [Google Scholar] [CrossRef] [PubMed]
- Grimm, A.; Decard, B.F.; Axer, H. Ultrasonography of the peripheral nervous system in the early stage of Guillain-Barre syndrome. J. Peripher. Nerv. Syst. 2014, 19, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Gallardo, E.; Sedano, M.J.; Orizaola, P.; Sanchez-Juan, P.; Gonzalez-Suarez, A.; Garcia, A.; Teran-Villagra, N.; Ruiz-Soto, M.; Alvaro, R.L.; Berciano, M.T.; et al. Spinal nerve involvement in early Guillain-Barre syndrome: A clinico-electrophysiological, ultrasonographic and pathological study. Clin. Neurophysiol. 2015, 126, 810–819. [Google Scholar] [CrossRef] [PubMed]
- Razali, S.N.O.; Arumugam, T.; Yuki, N.; Rozalli, F.I.; Goh, K.J.; Shahrizaila, N. Serial peripheral nerve ultrasound in Guillain-Barre syndrome. Clin. Neurophysiol. 2016, 127, 1652–1656. [Google Scholar] [CrossRef] [PubMed]
- Mori, A.; Nodera, H.; Takamatsu, N.; Maruyama-Saladini, K.; Osaki, Y.; Shimatani, Y.; Kaji, R. Sonographic evaluation of peripheral nerves in subtypes of Guillain-Barre syndrome. J. Neurol. Sci. 2016, 364, 154–159. [Google Scholar] [CrossRef]
- Decard, B.F.; Fladt, J.; Axer, H.; Fischer, D.; Grimm, A. Nerve ultrasound in Miller Fisher variant of Guillain-Barre syndrome. Muscle Nerve 2015, 52, 1106–1110. [Google Scholar] [CrossRef]
- Berciano, J.; Gallardo, E. Spinal nerve pathology in Guillain-Barre syndrome associated with COVID-19 infection. Muscle Nerve 2020, 62, E74–E75. [Google Scholar] [CrossRef]
- Grimm, A.; Décard, B.F.; Schramm, A.; Pröbstel, A.K.; Rasenack, M.; Axer, H.; Fuhr, P. Ultrasound and electrophysiologic findings in patients with Guillain-Barré syndrome at disease onset and over a period of six months. Clin. Neurophysiol. 2016, 127, 1657–1663. [Google Scholar] [CrossRef]
- Almeida, V.; Mariotti, P.; Veltri, S.; Erra, C.; Padua, L. Nerve ultrasound follow-up in a child with Guillain-Barre syndrome. Muscle Nerve 2012, 46, 270–275. [Google Scholar] [CrossRef]
- Grimm, A.; Oertl, H.; Auffenberg, E.; Schubert, V.; Ruschil, C.; Axer, H.; Winter, N. Differentiation Between Guillain-Barré Syndrome and Acute-Onset Chronic Inflammatory Demyelinating Polyradiculoneuritis-a Prospective Follow-up Study Using Ultrasound and Neurophysiological Measurements. Neurotherapeutics 2019, 16, 838–847. [Google Scholar] [CrossRef] [Green Version]
- Hobson-Webb, L.D.; Massey, J.M.; Juel, V.C. Nerve ultrasound in diabetic polyneuropathy: Correlation with clinical characteristics and electrodiagnostic testing. Muscle Nerve 2013, 47, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Pitarokoili, K.; Kerasnoudis, A.; Behrendt, V.; Labedi, A.; Ayzenberg, I.; Gold, R.; Yoon, M.S. Facing the diagnostic challenge: Nerve ultrasound in diabetic patients with neuropathic symptoms. Muscle Nerve 2016, 54, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Gupta, K.; Kaur, S. High resolution ultrasonography of the tibial nerve in diabetic peripheral neuropathy. J. Ultrason 2017, 17, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Ito, H.; Morita, A.; Uno, Y.; Nishimura, T.; Kawase, H.; Kato, Y.; Matsuoka, T.; Takeda, J.; Seishima, M. Sonographic evaluation of the median nerve in diabetic patients: Comparison with nerve conduction studies. J. Ultrasound Med. 2009, 28, 727–734. [Google Scholar] [CrossRef]
- Breiner, A.; Qrimli, M.; Ebadi, H.; Alabdali, M.; Lovblom, L.E.; Abraham, A.; Albulahi, H.; Perkins, B.A.; Bril, V. Peripheral nerve high-resolution ultrasound in diabetes. Muscle Nerve 2017, 55, 171–178. [Google Scholar] [CrossRef]
- Kang, S.; Kim, S.H.; Yang, S.N.; Yoon, J.S. Sonographic features of peripheral nerves at multiple sites in patients with diabetic polyneuropathy. J. Diabetes Complicat. 2016, 30, 518–523. [Google Scholar] [CrossRef]
- Arumugam, T.; Razali, S.N.; Vethakkan, S.R.; Rozalli, F.I.; Shahrizaila, N. Relationship between ultrasonographic nerve morphology and severity of diabetic sensorimotor polyneuropathy. Eur. J. Neurol. 2016, 23, 354–360. [Google Scholar] [CrossRef]
- Tawfik, E.A.; Walker, F.O.; Cartwright, M.S.; El-Hilaly, R.A. Diagnostic Ultrasound of the Vagus Nerve in Patients with Diabetes. J. Neuroimaging 2017, 27, 589–593. [Google Scholar] [CrossRef]
- Kerasnoudis, A.; Woitalla, D.; Gold, R.; Pitarokoili, K.; Yoon, M.S. Sarcoid neuropathy: Correlation of nerve ultrasound, electrophysiological and clinical findings. J. Neurol. Sci. 2014, 347, 129–136. [Google Scholar] [CrossRef]
- Ito, T.; Kijima, M.; Watanabe, T.; Sakuta, M.; Nishiyama, K. Ultrasonography of the tibial nerve in vasculitic neuropathy. Muscle Nerve 2007, 35, 379–382. [Google Scholar] [CrossRef]
- Grimm, A.; Decard, B.F.; Bischof, A.; Axer, H. Ultrasound of the peripheral nerves in systemic vasculitic neuropathies. J. Neurol. Sci. 2014, 347, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Üçeyler, N.; Schäfer, K.A.; Mackenrodt, D.; Sommer, C.; Müllges, W. High-Resolution Ultrasonography of the Superficial Peroneal Motor and Sural Sensory Nerves May Be a Non-invasive Approach to the Diagnosis of Vasculitic Neuropathy. Front. Neurol. 2016, 7, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goedee, H.S.; van der Pol, W.L.; van Asseldonk, J.H.; Vrancken, A.; Notermans, N.C.; Visser, L.H.; van den Berg, L.H. Nerve sonography to detect peripheral nerve involvement in vasculitis syndromes. Neurol. Clin. Pract. 2016, 6, 293–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Decard, B.F.; Grimm, A.; Andelova, M.; Deman, A.; Banderet, B.; Garcia, M.; Fuhr, P. Hepatitis-E virus associated neuralgic amyotrophy with sustained plexus brachialis swelling visualized by high-resolution ultrasound. J. Neurol. Sci. 2015, 351, 208–210. [Google Scholar] [CrossRef]
- Dabir, A.; Pawar, G. Teaching NeuroImages: Lyme disease presenting as Bannwarth syndrome. Neurology 2018, 91, e1459–e1460. [Google Scholar] [CrossRef] [Green Version]
- Grimm, A.; Décard, B.F.; Axer, H.; Fuhr, P. The Ultrasound pattern sum score-UPSS. A new method to differentiate acute and subacute neuropathies using ultrasound of the peripheral nerves. Clin. Neurophysiol. 2015, 126, 2216–2225. [Google Scholar] [CrossRef]
- Lycan, T.W.; Hsu, F.C.; Ahn, C.S.; Thomas, A.; Walker, F.O.; Sangueza, O.P.; Shiozawa, Y.; Park, S.H.; Peters, C.M.; Romero-Sandoval, E.A.; et al. Neuromuscular ultrasound for taxane peripheral neuropathy in breast cancer. Muscle Nerve 2020, 61, 587–594. [Google Scholar] [CrossRef]
- Pitarokoili, K.; Hoffken, N.; Lonneker, N.; Fisse, A.L.; Trampe, N.; Gold, R.; Reinacher-Schick, A.; Yoon, M.S. Prospective Study of the Clinical, Electrophysiologic, and Sonographic Characteristics of Oxaliplatin-Induced Neuropathy. J. Neuroimaging 2019, 29, 133–139. [Google Scholar] [CrossRef] [Green Version]
- Leadbetter, R.; Weatherall, M.; Pelosi, L. Nerve ultrasound as a diagnostic tool for sensory neuronopathy in spinocerebellar ataxia syndrome. Clin. Neurophysiol. 2019, 130, 568–572. [Google Scholar] [CrossRef]
- Grisold, W.; Grisold, A.; Marosi, C.; Meng, S.; Briani, C. Neuropathies associated with lymphoma. Neurooncol. Pract. 2015, 2, 167–178. [Google Scholar] [CrossRef]
- Campagnolo, M.; Cacciavillani, M.; Cavallaro, T.; Ferrari, S.; Gasparotti, R.; Zambello, R.; Briani, C. Neurolymphomatosis, a rare manifestation of peripheral nerve involvement in lymphomas: Suggestive features and diagnostic challenges. J. Peripher. Nerv. Syst. 2020, 25, 312–315. [Google Scholar] [CrossRef] [PubMed]
- Ruzhansky, K.M.; Brannagan, T.H., 3rd. Neuromuscular complications of hematopoietic stem cell transplantation. Muscle Nerve 2015, 52, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Cocito, D.; Romagnolo, A.; Rosso, M.; Peci, E.; Lopiano, L.; Merola, A. CIDP-like neuropathies in graft versus host disease. J. Peripher. Nerv. Syst. 2015, 20, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Karam, C.; Mauermann, M.L.; Johnston, P.B.; Lahoria, R.; Engelstad, J.K.; Dyck, P.J. Immune-mediated neuropathies following stem cell transplantation. J. Neurol. Neurosurg. Psychiatry 2014, 85, 638–642. [Google Scholar] [CrossRef]
- Kupper, H.; Kaiser, N.; Winter, N.; Kehrer, C.; Groeschel, S.; Bevot, A.; Nagele, T.; Krageloh-Mann, I.; Grimm, A. Enlargement of peripheral nerves in Krabbe disease: The diagnostic value of nerve ultrasound. Muscle Nerve 2020, 61, E24–E27. [Google Scholar] [CrossRef]
- Grimm, A.; Schaffer, E.; Just, J.; Schols, L.; Kehrer, C.; Bevot, A.; Ziemann, U.; Krageloh-Mann, I. Thickening of the peripheral nerves in metachromatic leukodystrophy. J. Neurol. Sci. 2016, 368, 399–401. [Google Scholar] [CrossRef]
- Rattay, T.W.; Just, J.; Röben, B.; Hengel, H.; Schüle, R.; Synofzik, M.; Söhn, A.S.; Winter, N.; Dammeier, N.; Schöls, L.; et al. Nerve ultrasound characterizes AMN polyneuropathy as inhomogeneous and focal hypertrophic. Orphanet J. Rare Dis. 2018, 13, 194. [Google Scholar] [CrossRef]
- Mori, A.; Nodera, H.; Takamatsu, N.; Maruyama-Saladini, K.; Osaki, Y.; Shimatani, Y.; Oda, M.; Izumi, Y.; Kaji, R. Sonographic evaluation of cervical nerve roots in ALS and its clinical subtypes. J. Med. Investig. 2016, 63, 54–57. [Google Scholar] [CrossRef] [Green Version]
- Grimm, A.; Rattay, T.W.; Winter, N.; Axer, H. Peripheral nerve ultrasound scoring systems: Benchmarking and comparative analysis. J. Neurol. 2017, 264, 243–253. [Google Scholar] [CrossRef]
- Kerasnoudis, A.; Pitarokoili, K.; Behrendt, V.; Gold, R.; Yoon, M.S. Nerve ultrasound score in distinguishing chronic from acute inflammatory demyelinating polyneuropathy. Clin. Neurophysiol. 2014, 125, 635–641. [Google Scholar] [CrossRef]
- Schreiber, S.; Dannhardt-Stieger, V.; Henkel, D.; Debska-Vielhaber, G.; Machts, J.; Abdulla, S.; Kropf, S.; Kollewe, K.; Petri, S.; Heinze, H.J.; et al. Quantifying disease progression in amyotrophic lateral sclerosis using peripheral nerve sonography. Muscle Nerve 2016, 54, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, S.; Abdulla, S.; Debska-Vielhaber, G.; Machts, J.; Dannhardt-Stieger, V.; Feistner, H.; Oldag, A.; Goertler, M.; Petri, S.; Kollewe, K.; et al. Peripheral nerve ultrasound in amyotrophic lateral sclerosis phenotypes. Muscle Nerve 2015, 51, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Kerasnoudis, A.; Pitarokoili, K.; Haghikia, A.; Gold, R.; Yoon, M.S. Nerve ultrasound protocol in differentiating chronic immune-mediated neuropathies. Muscle Nerve 2016, 54, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Tawfik, E.A.; Cartwright, M.S.; Grimm, A.; Boon, A.J.; Kerasnoudis, A.; Preston, D.C.; Wilder-Smith, E.; Axer, H.; Hobson-Webb, L.D.; van Alfen, N.; et al. Guidelines for neuromuscular ultrasound training. Muscle Nerve 2019, 60, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Walker, F.O.; Alter, K.E.; Boon, A.J.; Cartwright, M.S.; Flores, V.H.; Hobson-Webb, L.D.; Hunt, C.H.; Primack, S.J.; Shook, S.J. Qualifications for practitioners of neuromuscular ultrasound: Position statement of the American Association of Neuromuscular and Electrodiagnostic Medicine. Muscle Nerve 2010, 42, 442–444. [Google Scholar] [CrossRef]
- Simon, N.G. Clinical and economic arguments to support a neuromuscular ultrasound service. Clin. Neurophysiol. Pract. 2019, 4, 168–169. [Google Scholar] [CrossRef]





| Diagnosis | Predominant Nerve Conduction Findings | Common Ultrasound Findings | Echointensity | Scores/Cut-Offs |
|---|---|---|---|---|
| Hereditary Neuropathies | ||||
| CMT1a | Demyelinating | Homogeneous nerve enlargement | Reduced | UPSS > 8 HS ≥ 4 |
| CMT1b | Demyelinating | Homogeneous nerve enlargement (smaller than CMT1a) | Reduced | UPSS > 8 HS > 3 |
| Other CMT1/4 | Demyelinating | Regional nerve enlargement (heterogeneous) | Insufficient data | Insufficient data |
| CMT2 | Axonal | No significant nerve enlargement | Insufficient data | UPSS < 3 |
| HNPP | Nerve entrapment | Enlargement at entrapment sites | Reduced at entrapment sites | UPSS < 3 Entrapment ratios > 1,5 |
| ATTR | Axonal and nerve entrapment | Proximal nerve enlargement and at entrapment sites | Reduced | UPSS > 3, entrapment |
| SCA neuropathy/ CANVAS | Axonal (sensory dominant) | No nerve enlargement (upper limb nerves <5mm2 in CANVAS patients) | Increased | Upper limb nerves <5mm2 |
| Storage diseases | ||||
| Metachromatic and Adrenoleucodystrophies/ Cerebrotendinous Xanthochromatosis | Demyelinating, homogeneous | Diffuse nerve enlargement | Reduced | UPSS > 3 (AMN) |
| Acquired neuropathies | ||||
| GBS | Axonal (AMAN/AMSAN), demyelinating (AIDP/MFS) | Nerve root and vagus nerve enlargement | Reduced | UPSS < 5 UPSB ≥ 1 UPSC < 1 BUS < 2 |
| CIDP | Demyelinating EFNS criteria (symmetric) | Heterogeneous enlargement of all nerves (proximal predominant, median nerve, ulnar nerve, nerve roots and plexus) | Heterogeneous (Class 1 reduced, Class 2 increased, Class 3 mixed/ not enlarged) | UPSS > 5 BUS > 1 |
| MADSAM | Demyelinating with temporal dispersion and conduction block (asymmetric) | Fascicular and regionally restricted nerve enlargement, also resembling CIDP pattern | Similar to CIDP | UPSS > 3 UPSC > 0 |
| Multifocal Motor Neuropathy | Conduction block, only motor nerves affected | Fascicular and regionally restricted nerve enlargement, correlating with conduction block in up to 75% | Reduced> increased | UPSS > 3 UPSC < 1 (no sensory nerves affected) |
| Anti-MAG PNP | Demyelinating | Similar to CIDP | Similar to CIDP | Similar to CIDP |
| MGUS-CIDP | Similar to CIDP | Similar to CIDP | Similar to CIDP | Similar to CIDP |
| Other PNP associated with MGUS | Axonal | No enlargement | Insufficient data | UPSS < 3 |
| Multiple Myeloma associated PNP | Axonal | No enlargement | Insufficient data | UPSS < 3 |
| POEMS | Demyelinating (homogeneous) | Heterogeneous nerve enlargement, entrapment sites | Insufficient data | UPSS > 3 |
| Vasculitis | Axonal (asymmetric) | Focal nerve enlargement in symptomatic nerves | Increased | UPSS 3–9 Multifocal nerve enlargement of ≥1 nerve |
| Diabetic PNP | Axonal > >demyelinating | Slight nerve enlargement (e.g., entrapment sites) | Inconsistent data | UPSS < 3 |
| ChTx induced neuropathies | Axonal | No significant nerve enlargement | Increased | UPSS < 3 |
| Other axonal neuropathies (e.g., vitamin deficiency) | Axonal | No nerve enlargement | Insufficient data | UPSS < 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kramer, M.; Grimm, A.; Winter, N.; Dörner, M.; Grundmann-Hauser, K.; Stahl, J.-H.; Wittlinger, J.; Kegele, J.; Kronlage, C.; Willikens, S. Nerve Ultrasound as Helpful Tool in Polyneuropathies. Diagnostics 2021, 11, 211. https://doi.org/10.3390/diagnostics11020211
Kramer M, Grimm A, Winter N, Dörner M, Grundmann-Hauser K, Stahl J-H, Wittlinger J, Kegele J, Kronlage C, Willikens S. Nerve Ultrasound as Helpful Tool in Polyneuropathies. Diagnostics. 2021; 11(2):211. https://doi.org/10.3390/diagnostics11020211
Chicago/Turabian StyleKramer, Magdalena, Alexander Grimm, Natalie Winter, Marc Dörner, Kathrin Grundmann-Hauser, Jan-Hendrik Stahl, Julia Wittlinger, Josua Kegele, Cornelius Kronlage, and Sophia Willikens. 2021. "Nerve Ultrasound as Helpful Tool in Polyneuropathies" Diagnostics 11, no. 2: 211. https://doi.org/10.3390/diagnostics11020211






