Exhausted Capacity of Bicarbonate Buffer in Renal Failure Diagnosed Using Point of Care Analyzer
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Clinical Characteristic
3.2. Comparison of Acide-Base Balance Parameters in Grups A and B
3.3. The Pearson Correlations of Urea, Serum Creatinine (sCr) and Glomerular Filtration Rate (eGFR) with Acide-Base Balance Parameters
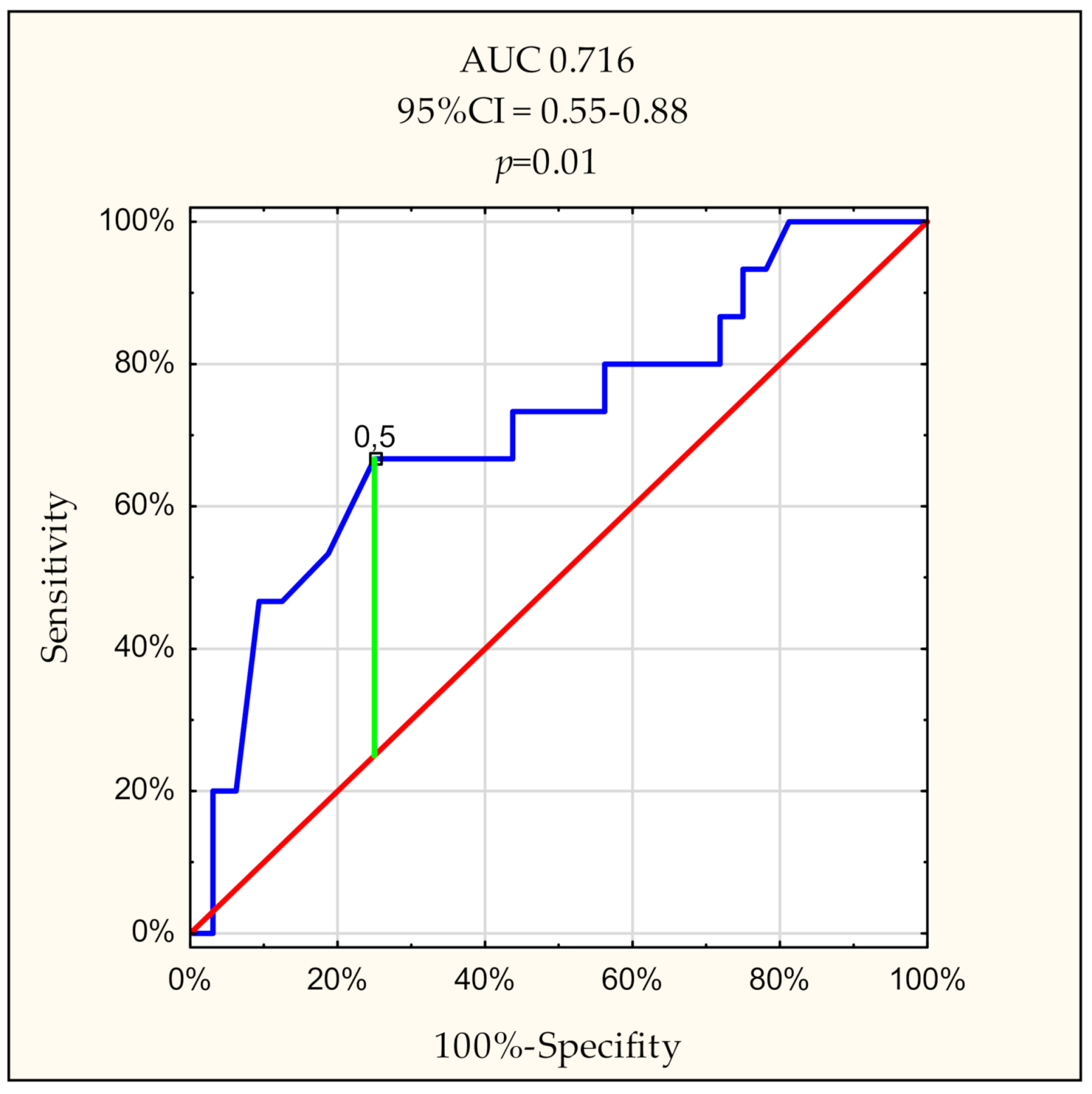
3.4. Receiver Operating Characteristic (ROC) Curves for the Variables with Most Important Discriminative Power for Group B of Patients (eGFR < 10 mL/min/1.73 m2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mak, R.H.; Cheung, W. Energy homeostasis and cachexia in chronic kidney disease. Pediatr. Nephrol. 2006, 21, 1807–1814. [Google Scholar] [CrossRef]
- Ballmer, P.E.; McNurlan, M.A.; Hulter, H.N.; Anderson, S.E.; Garlick, P.J.; Krapf, R. Chronic metabolic acidosis decreases albumin synthesis and induces negative nitrogen balance in humans. J. Clin. Investig. 1995, 95, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Mandel, E.I.; Forman, J.P.; Curhan, G.C.; Taylor, E.N. Plasma bicarbonate and odds of incident hypertension. Am. J. Hypertens. 2013, 26, 1405–1412. [Google Scholar] [CrossRef] [PubMed]
- Kraut, J.A.; Madias, N.E. Consequences and therapy of the metabolic acidosis of chronic kidney disease. Pediatr. Nephrol. 2011, 26, 19–28. [Google Scholar] [CrossRef]
- Shah, S.N.; Abramowitz, M.; Hostetter, T.H.; Melamed, M.L. Serum bicarbonate levels and the progression of kidney disease: A cohort study. Am. J. Kidney Dis. 2009, 54, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Menon, V.; Tighiouart, H.; Vaughn, N.S.; Beck, G.J.; Kusek, J.W.; Collins, A.J.; Greene, T.; Sarnak, M.J. Serum bicarbonate and long-term outcomes in CKD. Am. J. Kidney Dis. 2010, 56, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Abe, M.; Akaishi, T.; Shoji, M.; Yamaguchi, T.; Miki, T.; Satoh, F.; Takayama, S.; Yamasaki, S.; Kawaguchi, K.; Sato, H.; et al. Reno-protective effects of oral alkalizing agents in chronic kidney disease with aciduria: Protocol for a randomized cohort study. BMC Nephrol. 2020, 21, 144. [Google Scholar] [CrossRef] [PubMed]
- Eustace, J.A.; Astor, B.; Muntner, P.M.; Ikizler, T.A.; Coresh, J. Prevalence of acidosis and inflammation and their association with low serum albumin in chronic kidney disease. Kidney Int. 2004, 65, 1031–1040. [Google Scholar] [CrossRef]
- Wesson, D.E.; Simoni, J. Acid retention during kidney failure induces endothelin and aldosterone production which lead to progressive GFR decline, a situation ameliorated by alkali diet. Kidney Int. 2010, 78, 1128–1135. [Google Scholar] [CrossRef]
- Scialla, J.J.; Anderson, C.A. Dietary acid load: A novel nutritional target in chronic kidney disease? Adv. Chronic. Kidney Dis. 2013, 20, 141–149. [Google Scholar] [CrossRef]
- May, R.C.; Kelly, R.A.; Mitch, W.E. Metabolic acidosis stimulates protein degradation in rat muscle by a glucocorticoid-dependent mechanism. J. Clin. Investig. 1986, 77, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Abramowitz, M.K.; Melamed, M.L.; Bauer, C.; Raff, A.C.; Hostetter, T.H. Effects of oral sodium bicarbonate in patients with CKD. Clin. J. Am. Soc. Nephrol. 2013, 8, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, A.; Simoni, J.; Sheather, S.J.; Broglio, K.R.; Rajab, M.H.; Wesson, D.E. Daily oral sodium bicarbonate preserves glomerular filtration rate by slowing its decline in early hypertensive nephropathy. Kidney Int. 2010, 78, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Levey, A.S.; Coresh, J.; Greene, T.; Stevens, L.A.; Zhang, Y.L.; Hendriksen, S.; Kusek, J.W.; Van Lente, F.; Chronic Kidney Disease Epidemiology, C. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 2006, 145, 247–254. [Google Scholar] [CrossRef]
- Levin, A.; Stevens, P.E. Summary of KDIGO 2012 CKD Guideline: Behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014, 85, 49–61. [Google Scholar] [CrossRef]
- Gennari, F.J.; Hood, V.L.; Greene, T.; Wang, X.; Levey, A.S. Effect of dietary protein intake on serum total CO2 concentration in chronic kidney disease: Modification of Diet in Renal Disease study findings. Clin. J. Am. Soc. Nephrol. 2006, 1, 52–57. [Google Scholar] [CrossRef]
- Capusa, C.; Stefan, G.; Stancu, S.; Lipan, M.; Tsur, L.D.; Mircescu, G. Metabolic acidosis of chronic kidney disease and subclinical cardiovascular disease markers: Friend or foe? Medicine (Baltimore) 2017, 96, e8802. [Google Scholar] [CrossRef]
- Packer, R.K.; Curry, C.A.; Brown, K.M. Urinary organic anion excretion in response to dietary acid and base loading. J. Am. Soc. Nephrol. 1995, 5, 1624–1629. [Google Scholar]
- Vallet, M.; Metzger, M.; Haymann, J.P.; Flamant, M.; Gauci, C.; Thervet, E.; Boffa, J.J.; Vrtovsnik, F.; Froissart, M.; Stengel, B.; et al. Urinary ammonia and long-term outcomes in chronic kidney disease. Kidney Int. 2015, 88, 137–145. [Google Scholar] [CrossRef]
- Kraut, J.A. Disturbances of acid-base balance and bone disease in end-stage renal disease. Semin. Dial. 2000, 13, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Dobre, M.; Yang, W.; Chen, J.; Drawz, P.; Hamm, L.L.; Horwitz, E.; Hostetter, T.; Jaar, B.; Lora, C.M.; Nessel, L.; et al. Association of serum bicarbonate with risk of renal and cardiovascular outcomes in CKD: A report from the Chronic Renal Insufficiency Cohort (CRIC) study. Am. J. Kidney Dis. 2013, 62, 670–678. [Google Scholar] [CrossRef] [PubMed]
- Dobre, M.; Yang, W.; Pan, Q.; Appel, L.; Bellovich, K.; Chen, J.; Feldman, H.; Fischer, M.J.; Ham, L.L.; Hostetter, T.; et al. Persistent high serum bicarbonate and the risk of heart failure in patients with chronic kidney disease (CKD): A report from the Chronic Renal Insufficiency Cohort (CRIC) study. J. Am. Heart Assoc. 2015, 4. [Google Scholar] [CrossRef] [PubMed]

| Variables | Group A GFR ≥ 10 mL/min/1.73 m2 N = 34 | Group B GFR < 10 mL/min/1.73 m2 N = 15 | |||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | p | |
| Age (y.) | 67 | 52–75 | 62 | 42–75 | 0.52 * |
| Causes of CKD | |||||
| No | % | No | % | ||
| DM | 13 | 38 | 8 | 53 | 0.82 |
| Chronic GN | 3 | 9 | 4 | 27 | 0.16 |
| Others | 18 | 53 | 3 | 20 | 0.15 |
| Comorbid conditions | |||||
| CHD | 7 | 21 | 3 | 20 | 0.97 |
| AF | 4 | 12 | 1 | 7 | 0.62 |
| PAD | 6 | 18 | 3 | 20 | 0.87 |
| Stroke | 6 | 18 | 3 | 20 | 0.87 |
| Malignancy | 2 | 6 | 2 | 13 | 0.42 |
| Present and past smoking | 15 | 44 | 3 | 20 | 0.25 |
| Variables | Group A GFR ≥ 10 mL/min/1.73 m2 N = 34 | Group B GFR < 10 mL/min/1.73 m2 N = 15 | |||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | p * | |
| A-pH | 7.36 | 7.32–7.38 | 7.33 | 7.29–7.36 | 0.257 |
| A-pCO2 (mmHg) | 35.40 | 31.5–38 | 33.70 | 29.8–36 | 0.238 |
| A-HCO3−(mmol/L) | 19.90 | 18.3–20.7 | 18.30 | 15.4–21 | 0.201 |
| A-ABE (mmol/L) | −5.40 | −7.7–(−4.5) | −7.60 | −11.3–(−4.1) | 0.197 |
| A-SBE (mmol/L) | −6.20 | −8.50–(−4.9) | −8.40 | −12.4–(−5) | 0.197 |
| A-K+ (mmol/L) | 4.20 | 3.9–4.7 | 4.20 | 3.9–5.1 | 0.624 |
| A-Na+ (mmol/L) | 142.00 | 140–143 | 140.00 | 139–142 | 0.138 |
| A-Ca2+ (mmol/L) | 1.15 | 1.12–1.2 | 1.09 | 0.99–1.13 | 0.008 |
| A-Cl− (mmol/L) | 112.00 | 110–116 | 113.00 | 107–117 | 0.647 |
| A-AG (mmol/L) | 9.50 | 8–10.6 | 10.60 | 10.1–11.9 | 0.023 |
| A-AG (K+) (mmol/L) | 13.80 | 13–14.8 | 15.60 | 13.9–16.4 | 0.020 |
| V-pH | 7.28 | 7.22–7.32 | 7.28 | 7.26–7.36 | 0.405 |
| V-pCO2 (mmHg) | 38.50 | 34.5–41.5 | 35.90 | 33.2–38.6 | 0.182 |
| V-HCO3−(mmol/L) | 17.40 | 14.95–20.1 | 16.80 | 15.5–20 | 0.864 |
| V-ABE (mmol/L) | −8.80 | −11.95–(−5) | −9.60 | −11.1–(−5.1) | 0.936 |
| V-SBE (mmol/L) | −9.50 | −12.75–(−5.3) | −10.50 | −12.1–(−5.6) | 0.991 |
| V-K+ (mmol/L) | 4.30 | 4.05–4.75 | 4.30 | 3.9–5.2 | 0.864 |
| V-Na+ (mmol/L) | 142.00 | 140.5–143 | 141.00 | 138–142 | 0.063 |
| V-Ca2+ (mmol/L) | 1.19 | 1.16–1.26 | 1.12 | 1.02–1.18 | 0.005 |
| V-Cl- (mmol/L) | 114.00 | 109–117 | 110.00 | 107–116 | 0.247 |
| V-AG (mmol/L) | 11.10 | 9.45–12.9 | 11.70 | 10.5–13.2 | 0.288 |
| V-AG (K+) (mmol/L) | 15.75 | 14.25–17.25 | 16.60 | 16–17.5 | 0.222 |
| Δ-pH | 0.04 | 0.02–0.1 | 0.03 | 0.01–0.06 | 0.141 |
| Δ-pCO2 (mmHg) | −1.85 | −4.25–(−0.75) | −2.60 | −3.70–(−1.6) | 0.909 |
| Δ-HCO3−(mmol/L) | 1.30 | 0.55–3.05 | 0.30 | 0–1.4 | 0.019 |
| Δ-ABE (mmol/L) | 1.50 | 0.65–3.85 | 0.40 | −0.3–(1.7) | 0.024 |
| Δ-SBE (mmol/L) | 1.45 | 0.5–3.5 | 0.30 | −0.4–(1.4) | 0.024 |
| Δ-K+ (mmol/L) | 2.60 | 0–6.72 | 1.75 | −2–(7.69) | 0.366 |
| Δ-Na+ (mmol/L) | 0.35 | 0–0.72 | 0.70 | 0–0.71 | 0.653 |
| Δ-Ca2+ (mmol/L) | −0.03 | −0.07–(−0.01) | −0.01 | −0.08–(0) | 0.397 |
| Δ-Cl− (mmol/L) | 0.00 | −1–(1) | 1.00 | 0–1 | 0.100 |
| Δ-AG (mmol/L) | −1.55 | −3.2–(−0.6) | −1.30 | −2.1–(−0.1) | 0.193 |
| Δ-AG (K+) (mmol/L) | −1.85 | −3.35–(−1) | −1.30 | −1.9–(−0.1) | 0.121 |
| urea (mg/dl) | 141.25 | 102.7–150.6 | 167.00 | 143–186.5 | 0.011 |
| sCr (mg/dl) | 4.33 | 4.12–5.15 | 7.47 | 5.05–8.35 | 0.000 |
| eGFR (ml/min/1.73 m2) | 12.00 | 11–15 | 8.00 | 7–9.5 | 0.000 |
| Variables | Urea (mg/dL) | sCr (mg/dL) | eGFR (mL/min/1.73 m2) | |||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| A-pH | −0.1238 | 0.412 | 0.0094 | 0.951 | 0.1588 | 0.292 |
| A-pCO2 (mmHg) | −0.1119 | 0.459 | −0.0876 | 0.562 | 0.0803 | 0.596 |
| A-HCO3− (mmol/L) | −0.1336 | 0.376 | −0.0171 | 0.910 | 0.1481 | 0.326 |
| A-ABE (mmol/L) | −0.1432 | 0.342 | −0.0270 | 0.859 | 0.1557 | 0.301 |
| A-SBE (mmol/L) | −0.1268 | 0.401 | −0.0196 | 0.897 | 0.1406 | 0.351 |
| A-K+ (mmol/L) | 0.2930 | 0.048 | 0.0894 | 0.555 | −0.0117 | 0.939 |
| A-Na+ (mmol/L) | 0.0359 | 0.813 | −0.0642 | 0.672 | −0.3073 | 0.038 |
| A-Ca2+ (mmol/L) | −0.1347 | 0.372 | −0.3166 | 0.032 | 0.3234 | 0.028 |
| A-Cl− (mmol/L) | −0.1134 | 0.453 | −0.1680 | 0.264 | −0.0704 | 0.642 |
| A-AG (mmol/L) | 0.4532 | 0.002 | 0.3506 | 0.017 | −0.4357 | 0.002 |
| A-AG (K+) (mmol/L) | 0.5443 | 0.000 | 0.3811 | 0.009 | −0.4444 | 0.002 |
| V-pH | 0.0388 | 0.798 | 0.2905 | 0.050 | −0.1978 | 0.188 |
| V-pCO2 (mmHg) | −0.0138 | 0.928 | −0.1660 | 0.270 | 0.1527 | 0.311 |
| V-HCO3− (mmol/L) | 0.0607 | 0.689 | 0.2171 | 0.147 | −0.1385 | 0.359 |
| V-ABE (mmol/L) | 0.0515 | 0.734 | 0.2099 | 0.162 | −0.1339 | 0.375 |
| V-SBE (mmol/L) | 0.0530 | 0.726 | 0.1954 | 0.193 | −0.1183 | 0.434 |
| V-K+ (mmol/L) | 0.2137 | 0.154 | 0.0624 | 0.680 | 0.0013 | 0.993 |
| V-Na+ (mmol/L) | 0.0333 | 0.826 | −0.1699 | 0.259 | −0.1896 | 0.207 |
| V-Ca2+ (mmol/L) | −0.2164 | 0.149 | −0.3889 | 0.008 | 0.3820 | 0.009 |
| V-Cl− (mmol/L) | −0.1840 | 0.221 | −0.2605 | 0.080 | 0.0289 | 0.849 |
| V-AG (mmol/L) | 0.3001 | 0.043 | 0.0951 | 0.530 | −0.1513 | 0.315 |
| V-AG (K+) (mmol/L) | 0.3845 | 0.008 | 0.1184 | 0.433 | −0.1610 | 0.285 |
| Δ-pH | −0.1642 | 0.276 | −0.3683 | 0.012 | 0.4028 | 0.006 |
| Δ-pCO2 (mmHg) | −0.1426 | 0.344 | 0.1299 | 0.389 | −0.1200 | 0.427 |
| Δ-HCO3− (mmol/L) | −0.3105 | 0.036 | −0.3943 | 0.007 | 0.4647 | 0.001 |
| Δ-ABE (mmol/L) | −0.3012 | 0.042 | −0.3980 | 0.006 | 0.4604 | 0.001 |
| Δ-SBE (mmol/L) | −0.3016 | 0.042 | −0.3873 | 0.008 | 0.4426 | 0.002 |
| Δ-K+ (mmol/L) | 0.2021 | 0.178 | 0.0684 | 0.652 | −0.0320 | 0.833 |
| Δ-Na+ (mmol/L) | 0.0129 | 0.932 | 0.1889 | 0.209 | −0.2924 | 0.049 |
| Δ-Ca2+ (mmol/L) | 0.1862 | 0.215 | 0.1735 | 0.249 | −0.1436 | 0.341 |
| Δ-Cl− (mmol/L) | 0.1650 | 0.273 | 0.2059 | 0.170 | −0.2620 | 0.079 |
| Δ-AG (mmol/L) | 0.1655 | 0.272 | 0.2933 | 0.048 | −0.3246 | 0.028 |
| Δ-AG (K+) (mmol/L) | 0.1860 | 0.216 | 0.2958 | 0.046 | −0.3198 | 0.030 |
| AUC | 95% CI | p | Proposed Cut-Off Point | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | |
|---|---|---|---|---|---|---|---|---|
| A-AG | 0.707 | 0.54–0.87 | 0.013 | 9.9 mmol/L | 86.7 | 66.7 | 54.2 | 91.7 |
| A-AG (K+) | 0.712 | 0.55–0.88 | 0.012 | 14.3 mmol/L | 73.3 | 66.7 | 50.0 | 84.6 |
| Δ-pH | 0.634 | 0.47–0.80 | 0.119 | 0.065 | 86.7 | 43.8 | 41.9 | 87.5 |
| Δ-HCO3− | 0.716 | 0.55–0.88 | 0.010 | 0.5 mmol/L | 66.7 | 75.0 | 55.5 | 82.7 |
| Δ-ABE | 0.707 | 0.54–0.87 | 0.013 | 0.6 mmol/L | 60.0 | 75.0 | 53.9 | 80.0 |
| Δ-SBE | 0.708 | 0.55–0.87 | 0.012 | 0.9 mmol/L | 73.3 | 62.5 | 47.8 | 83.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gołębiowski, T.; Kusztal, M.; Konieczny, A.; Kuriata-Kordek, M.; Gawryś, A.; Augustyniak-Bartosik, H.; Letachowicz, K.; Zielińska, D.; Wiśniewska, M.; Krajewska, M. Exhausted Capacity of Bicarbonate Buffer in Renal Failure Diagnosed Using Point of Care Analyzer. Diagnostics 2021, 11, 226. https://doi.org/10.3390/diagnostics11020226
Gołębiowski T, Kusztal M, Konieczny A, Kuriata-Kordek M, Gawryś A, Augustyniak-Bartosik H, Letachowicz K, Zielińska D, Wiśniewska M, Krajewska M. Exhausted Capacity of Bicarbonate Buffer in Renal Failure Diagnosed Using Point of Care Analyzer. Diagnostics. 2021; 11(2):226. https://doi.org/10.3390/diagnostics11020226
Chicago/Turabian StyleGołębiowski, Tomasz, Mariusz Kusztal, Andrzej Konieczny, Magdalena Kuriata-Kordek, Ada Gawryś, Hanna Augustyniak-Bartosik, Krzysztof Letachowicz, Dorota Zielińska, Magdalena Wiśniewska, and Magdalena Krajewska. 2021. "Exhausted Capacity of Bicarbonate Buffer in Renal Failure Diagnosed Using Point of Care Analyzer" Diagnostics 11, no. 2: 226. https://doi.org/10.3390/diagnostics11020226
APA StyleGołębiowski, T., Kusztal, M., Konieczny, A., Kuriata-Kordek, M., Gawryś, A., Augustyniak-Bartosik, H., Letachowicz, K., Zielińska, D., Wiśniewska, M., & Krajewska, M. (2021). Exhausted Capacity of Bicarbonate Buffer in Renal Failure Diagnosed Using Point of Care Analyzer. Diagnostics, 11(2), 226. https://doi.org/10.3390/diagnostics11020226







