How Should We Measure and Deal with Office Blood Pressure in 2021?
Abstract
:1. Introduction
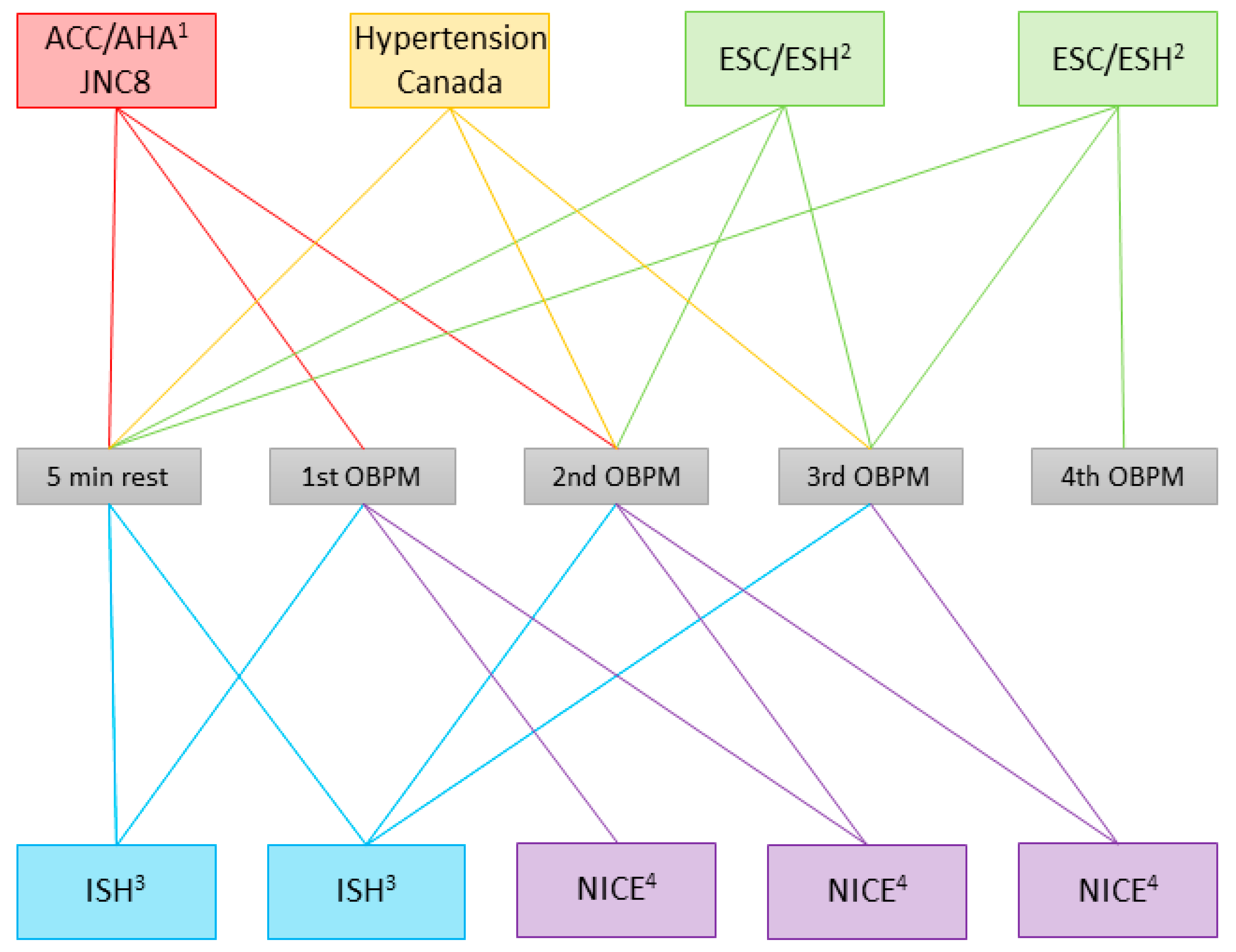
2. Guidelines’ Recommendations for Blood Pressure Measurement
3. Basis for Recommendations
4. What Are the Consequences of the Differences between the Recommended Procedures?
4.1. Single Versus Repeated Measurements
4.2. Difference between the Procedures Recommended by Guidelines
4.3. Adapting the Procedure Based on Arbitrary Threshold Values
4.4. Effect of the Rest Period
4.5. Link from Office Blood Pressure Procedure to Outcome
5. How to Overcome the OBPM Dilemma
5.1. Alternatives to Office Blood Pressure Measurements
5.1.1. Unattended Automated Office Blood Pressure Measurements
5.1.2. Ambulatory Blood Pressure Monitoring
5.1.3. Home Blood Pressure Measurements
5.2. Solution for the Application of Office Blood Pressure Measurements
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Brien, E.; Fitzgerald, D. The history of blood pressure measurement. J. Hum. Hypertens. 1994, 8, 73–84. [Google Scholar]
- Vischer, A.S.; Burkard, T. Principles of blood pressure measurement—Current techniques, office vs. ambulatory blood pressure measurement. Adv. Exp. Med. Biol. 2017, 956, 85–96. [Google Scholar]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Lewington, S.; Clarke, R.; Qizilbash, N.; Peto, R.; Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar] [PubMed]
- Thomopoulos, C.; Parati, G.; Zanchetti, A. Effects of blood pressure lowering on outcome incidence in hypertension: 2. Effects at different baseline and achieved blood pressure levels—Overview and meta-analyses of randomized trials. J. Hypertens. 2014, 32, 2296–2304. [Google Scholar] [CrossRef] [PubMed]
- Böhm, M.; Schumacher, H.; Teo, K.K.; Lonn, E.M.; Mahfoud, F.; Mann, J.F.E.; Mancia, G.; Redon, J.; Schmieder, R.E.; Sliwa, K.; et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: Results from ONTARGET and TRANSCEND trials. Lancet 2017, 389, 2226–2237. [Google Scholar] [CrossRef]
- Clark, C.E.; Warren, F.C.; Boddy, K.; McDonagh, S.T.J.; Moore, S.F.; Goddard, J.; Reed, N.; Turner, M.; Alzamora, M.T.; Blanes, R.R.; et al. Associations between systolic interarm differences in blood pressure and cardiovascular disease outcomes and mortality: Individual participant data meta-analysis, development and validation of a prognostic algorithm: The INTERPRESS-IPD collaboration. Hypertension 2021, 77, 650–661. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergious, G.S.; Tomaszewski, M.; et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rabi, D.M.; McBrien, K.A.; Sapir-Pichhadze, R.; Nakhla, M.; Ahmed, S.B.; Dumanski, S.M.; Butalia, S.; Leung, A.A.; Harris, K.C.; Cloutier, L.; et al. Hypertension Canada’s 2020 comprehensive Guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can. J. Cardiol. 2020, 36, 596–624. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Hypertension in Adults: Diagnosis and Management. NICE Guideline NG136; NICE: London, UK, 2019. [Google Scholar]
- Sacks, F.M.; Obarzanek, E.; Windhauser, M.M.; Svetkey, L.P.; Vollmer, W.M.; McCullough, M.; Karanja, N.; Lin, P.-H.; Steele, P.; Proschan, M.A.; et al. Rationale and design of the dietary approaches to stop hypertension trial (DASH). A multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann. Epidemiol. 1995, 5, 108–118. [Google Scholar] [CrossRef]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amery, A.; Birkenhäger, W.; Bulpitt, C.J.; Clément, D.; De Leeuw, P.; Dollery, C.T.; Fagard, R.; Fletcher, A.; Forette, F.; Leonetti, G.; et al. Syst-Eur. A multicentre trial on the treatment of isolated systolic hypertension in the elderly: Objectives, protocol, and organization. Aging Clin. Exp. Res. 1991, 3, 287–302. [Google Scholar] [CrossRef] [PubMed]
- Staessen, J.A.; Fagard, R.; Thijs, L.; Celis, H.; Arabidze, G.G.; Birkenhäger, W.H.; Bulpitt, C.J.; de Leeuw, P.W.; Dollery, C.T.; Fletcher, A.E.; et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet 1997, 350, 757–764. [Google Scholar] [CrossRef]
- Lonn, E.M.; Bosch, J.; Lopez-Jaramillo, P.; Zhu, J.; Liu, L.; Pais, P.; Diaz, R.; Xavier, D.; Sliwa, K.; Dans, A.; et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N. Engl. J. Med. 2016, 374, 2009–2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansson, L.; Zanchetti, A.; Carruthers, S.G.; Dahlöf, B.; Elmfeldt, D.; Julius, S.; Menard, J.; Rahn, K.H.; Wedel, H.; Westerling, S.; et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: Principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet 1998, 351, 1755–1762. [Google Scholar] [CrossRef]
- Jamerson, K.; Weber, M.A.; Bakris, G.L.; Dahlöf, B.; Pitt, B.; Shi, V.; Hester, A.; Gupte, J.; Gatlin, M.; Velazquez, E.J. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N. Engl. J. Med. 2008, 359, 2417–2428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cushman, W.C.; Evans, G.W.; Byington, R.P.; Goff, D.C., Jr.; Grimm, R.H., Jr.; Cutler, J.A.; Simons-Morton, D.G.; Basile, J.N.; Corson, M.A.; Probstfield, J.L.; et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N. Engl. J. Med. 2010, 362, 1575–1585. [Google Scholar]
- Wright, J.T., Jr.; Williamson, J.D.; Whelton, P.K.; Snyder, J.K.; Sink, K.M.; Rocco, M.V.; Reboussin, D.M.; Rahman, M.; Oparil, S.; Lewis, C.E.; et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 2015, 373, 2103–2116. [Google Scholar] [PubMed]
- Johnson, K.C.; Whelton, P.K.; Cushman, W.C.; Cutler, J.A.; Evans, G.W.; Snyder, J.K.; Ambrosius, W.T.; Beddhu, S.; Cheung, A.K.; Fine, L.J.; et al. Blood Pressure measurement in SPRINT (Systolic Blood Pressure Intervention Trial). Hypertension 2018, 71, 848–857. [Google Scholar] [CrossRef]
- Agodoa, L.Y.; Appel, L.; Bakris, G.L.; Beck, G.; Bourgoignie, J.; Briggs, J.P.; Charleston, J.; Cheek, D.; Cleveland, W.; Douglas, J.G.; et al. Effect of ramipril vs. amlodipine on renal outcomes in hypertensive nephrosclerosis: A randomized controlled trial. JAMA 2001, 285, 2719–2728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appel, L.J.; Wright, J.T., Jr.; Greene, T.; Agodoa, L.Y.; Astor, B.C.; Bakris, G.L.; Cleveland, W.H.; Charleston, J.; Contreras, G.; Faulkner, M.L.; et al. Intensive blood-pressure control in hypertensive chronic kidney disease. N. Engl. J. Med. 2010, 363, 918–929. [Google Scholar] [CrossRef] [Green Version]
- Williams, B.; MacDonald, T.M.; Morant, S.; Webb, D.J.; Sever, P.; McInnes, G.; Ford, I.; Cruickshank, J.K.; Caulfield, M.J.; Salsbury, J.; et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): A randomised, double-blind, crossover trial. Lancet 2015, 386, 2059–2068. [Google Scholar] [CrossRef] [Green Version]
- Williams, B.; MacDonald, T.M.; Caulfield, M.; Cruickshank, J.K.; McInnes, G.; Sever, P.; Webb, D.J.; Salsbury, J.; Morant, S.; Ford, I.; et al. Prevention and treatment of hypertension with algorithm-based therapy (PATHWAY) number 2: Protocol for a randomised crossover trial to determine optimal treatment for drug-resistant hypertension. BMJ Open 2015, 5, e008951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998, 317, 703–713. [Google Scholar] [CrossRef] [Green Version]
- Sever, P.S.; Dahlöf, B.; Poulter, N.R.; Wedel, H.; Beevers, G.; Caulfield, M.; Collins, R.; Kjeldsen, S.E.; McInnes, G.T.; Mehlsen, J.; et al. Rationale, design, methods and baseline demography of participants of the Anglo-Scandinavian Cardiac Outcomes Trial. ASCOT investigators. J. Hypertens. 2001, 19, 1139–1147. [Google Scholar] [CrossRef] [Green Version]
- Dahlöf, B.; Sever, P.S.; Poulter, N.R.; Wedel, H.; Beevers, D.G.; Caulfield, M.; Collins, R.; Kjeldsen, S.E.; Kristinsson, A.; McInnes, G.T.; et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): A multicentre randomised controlled trial. Lancet 2005, 366, 895–906. [Google Scholar]
- Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA 1967, 202, 1028–1034. [Google Scholar] [CrossRef]
- Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA 1970, 213, 1143–1152. [Google Scholar] [CrossRef]
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: The antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA 2002, 288, 2981–2997. [Google Scholar] [CrossRef]
- SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991, 265, 3255–3264. [Google Scholar] [CrossRef]
- Beaney, T.; Schutte, A.E.; Tomaszewski, M.; Ariti, C.; Burrell, L.M.; Castillo, R.R.; Charchar, F.J.; Damasceno, A.; Kruger, R.; Lackland, D.T.; et al. May measurement month 2017: An analysis of blood pressure screening results worldwide. Lancet Glob. Health 2018, 6, e736–e743. [Google Scholar] [CrossRef] [Green Version]
- Beaney, T.; Burrell, L.M.; Castillo, R.R.; Charchar, F.J.; Cro, S.; Damasceno, A.; Kruger, R.; Nilsson, P.M.; Prabhakaran, D.; Ramirez, A.J.; et al. May measurement month 2018: A pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. Eur. Heart J. 2019, 40, 2006–2017. [Google Scholar] [CrossRef] [Green Version]
- Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA 1979, 242, 2562–2571. [Google Scholar] [CrossRef]
- Sebo, P.; Pechère-Bertschi, A.; Herrmann, F.R.; Haller, D.M.; Bovier, P. Blood pressure measurements are unreliable to diagnose hypertension in primary care. J. Hypertens. 2014, 32, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Burkard, T.; Mayr, M.; Winterhalder, C.; Leonardi, L.; Eckstein, J.; Vischer, A.S. Reliability of single office blood pressure measurements. Heart 2018, 104, 1173–1179. [Google Scholar] [CrossRef]
- Morton, V.; Torgerson, D.J. Effect of regression to the mean on decision making in health care. BMJ 2003, 326, 1083–1084. [Google Scholar] [CrossRef] [Green Version]
- Galton, F. Regression towards mediocrity in hereditary stature. J. Anthropol. Inst. Great Br. Irel. 1886, 15, 246–263. [Google Scholar] [CrossRef]
- Messerli, F.H.; Rexhaj, E. Of headwind and tailwind, regression to the mean and Wilder’s principle. J. Hypertens. 2019, 37, 4–5. [Google Scholar] [CrossRef] [PubMed]
- Vischer, A.S.; Mayr, M.; Socrates, T.; Winterhalder, C.; Leonardi, L.; Eckstein, J.; Burkard, T. Impact of single-occasion American vs. Canadian office blood pressure measurement recommendations on blood pressure classification. Am. J. Hypertens. 2019, 32, 143–145. [Google Scholar] [CrossRef]
- Vischer, A.S.; Socrates, T.; Winterhalder, C.; Eckstein, J.; Mayr, M.; Burkard, T. Impact of single-visit American versus European office blood pressure measurement procedure on individual blood pressure classification: A cross-sectional study. Clin. Res. Cardiol. 2019, 108, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Batty, G.D.; Stamatakis, E.; Kivimaki, M. Hypertension awareness and psychological distress. Hypertension 2010, 56, 547–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pickering, T.G. Now we are sick: Labeling and hypertension. J. Clin. Hypertens. 2006, 8, 57–60. [Google Scholar] [CrossRef]
- Haynes, R.B.; Sackett, D.L.; Taylor, D.W.; Gibson, E.S.; Johnson, A.L. Increased absenteeism from work after detection and labeling of hypertensive patients. N. Engl. J. Med. 1978, 299, 741–744. [Google Scholar] [CrossRef]
- Vischer, A.S.; Socrates, T.; Winterhalder, C.; Eckstein, J.; Mayr, M.; Burkard, T. How should we measure blood pressure? Implications of the fourth blood pressure measurement in office blood pressure. J. Clin. Hypertens. 2020. [Google Scholar] [CrossRef]
- Qi, W.; Wu, Q.; Wu, Y.; Peng, Q.; Li, P.; Cheng, X.; Su, H. Talking with a doctor during a visit elicits increases in systolic and diastolic blood pressure. Blood Press. Monit. 2017, 22, 265–267. [Google Scholar] [CrossRef]
- Andreadis, E.A.; Agaliotis, G.D.; Angelopoulos, E.T.; Tsakanikas, A.P.; Chaveles, I.A.; Mousoulis, G.P. Automated office blood pressure and 24-h ambulatory measurements are equally associated with left ventricular mass index. Am. J. Hypertens. 2011, 24, 661–666. [Google Scholar] [CrossRef] [Green Version]
- Campbell, N.R.; McKay, D.W.; Conradson, H.; Lonn, E.; Title, L.M.; Anderson, T. Automated oscillometric blood pressure versus auscultatory blood pressure as a predictor of carotid intima-medial thickness in male firefighters. J. Hum. Hypertens. 2007, 21, 588–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dolan, E.; Stanton, A.; Thijs, L.; Hinedi, K.; Atkins, N.; McClory, S.; Hond, E.D.; McCormack, P.; Staessen, J.A.; O’Brien, E. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: The Dublin outcome study. Hypertension 2005, 46, 156–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, W.Y.; Melgarejo, J.D.; Thijs, L.; Zhang, Z.Y.; Boggia, J.; Wei, F.F.; Hansen, T.W.; Asayama, K.; Ohkubo, T.; Jeppesen, J.; et al. Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA 2019, 322, 409–420. [Google Scholar] [CrossRef]
- Shimbo, D.; Abdalla, M.; Falzon, L.; Townsend, R.R.; Muntner, P. Studies comparing ambulatory blood pressure and home blood pressure on cardiovascular disease and mortality outcomes: A systematic review. J. Am. Soc. Hypertens. 2016, 10, 224–234.e17. [Google Scholar] [CrossRef] [Green Version]
- Choi, E.J.; Jeong, D.W.; Lee, J.G.; Lee, S.; Kim, Y.J.; Yi, Y.H.; Cho, Y.H.; Im, S.J.; Bae, M.J. The impact of bladder distension on blood pressure in middle aged women. Korean J. Fam. Med. 2011, 32, 306–310. [Google Scholar] [CrossRef]
- Salvetti, M.; Paini, A.; Aggiusti, C.; Bertacchini, F.; Stassaldi, D.; Capellini, S.; De Ciuceis, C.; Rizzoni, D.; Gatta, R.; Rosei, E.A.; et al. Unattended versus attended blood pressure measurement. Hypertension 2019, 73, 736–742. [Google Scholar] [CrossRef]
- Pappaccogli, M.; Di Monaco, S.; Perlo, E.; Burrello, J.; D’Ascenzo, F.; Veglio, F.; Monticone, S.; Rabbia, F. Comparison of automated office blood pressure with office and out-off-office measurement techniques. Hypertension 2019, 73, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Roerecke, M.; Kaczorowski, J.; Myers, M.G. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: A systematic review and meta-ANALYSIS. JAMA Intern. Med. 2019, 179, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Myers, M.G. Eliminating the human factor in office blood pressure measurement. J. Clin. Hypertens. 2014, 16, 83–86. [Google Scholar] [CrossRef] [Green Version]
- Wohlfahrt, P.; Cífková, R.; Krajčoviechová, A.; Šulc, P.; Bruthans, J.; Linhart, A.; Filipovsky, J.; Mayer, O.; Widimsky, J., Jr. Comparison of three office blood pressure measurement techniques and their effect on hypertension prevalence in the general population. J. Hypertens. 2019, 38, 656–662. [Google Scholar] [CrossRef]
- Andreadis, E.A.; Geladari, C.V.; Angelopoulos, E.T.; Kolyvas, G.N.; Papademetriou, V. Morning surge and peak morning ambulatory blood pressure versus automated office blood pressure in predicting cardiovascular disease. High Blood Press. Cardiovasc. Prev. 2019, 26, 209–215. [Google Scholar] [CrossRef]
- Carter, E.J.; Moise, N.; Alcántara, C.; Sullivan, A.M.; Kronish, I.M. Patient barriers and facilitators to ambulatory and home blood pressure monitoring: A qualitative study. Am. J. Hypertens. 2018, 31, 919–927. [Google Scholar] [CrossRef]
- Krisai, P.; Vischer, A.S.; Kilian, L.; Meienberg, A.; Mayr, M.; Burkard, T. Accuracy of 24-hour ambulatory blood pressure monitoring by a novel cuffless device in clinical practice. Heart 2019, 105, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Kilian, L.; Krisai, P.; Socrates, T.; Arranto, C.; Pfister, O.; Meienberg, A.; Mayr, M.; Vischer, A.S.; Burkard, T. Analyzing 24-Hour blood pressure measurements with a novel cuffless pulse transit time device in clinical practice―Does the software for heartbeat detection matter? Diagnostics 2020, 10, 361. [Google Scholar] [CrossRef] [PubMed]
- Socrates, T.; Krisai, P.; Vischer, A.S.; Meienberg, A.; Mayr, M.; Burkard, T. Improved agreement and diagnostic accuracy of a cuffless 24-hour blood pressure measurement device in clinical practice. Sci. Rep. 2020, 11, 1143. [Google Scholar] [CrossRef] [PubMed]
- Ward, A.M.; Takahashi, O.; Stevens, R.; Heneghan, C. Home measurement of blood pressure and cardiovascular disease: Systematic review and meta-analysis of prospective studies. J. Hypertens. 2012, 30, 449–456. [Google Scholar] [CrossRef]
- Schwartz, C.L.; Seyed-Safi, A.; Haque, S.; Bray, E.P.; Greenfield, S.; Hobbs, F.D.R.; Little, P.; Mant, J.; Williams, B.; Mcmanus, R.J. Do patients actually do what we ask: Patient fidelity and persistence to the targets and self-management for the control of blood pressure in stroke and at risk groups blood pressure self-management intervention. J. Hypertens. 2018, 36, 1753–1761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, M.H.; Kim, G.H.; Kim, J.H.; Moon, K.W.; Yoo, K.D.; Rho, T.H.; Chul-Min, K. Reliability of home blood pressure monitoring: In the context of validation and accuracy. Blood Press. Monit. 2015, 20, 215–220. [Google Scholar] [CrossRef]


| Guidelines | AHT Threshold | Reference |
|---|---|---|
| ACC/AHA | 130/80 mmHg 1 | [11] |
| JNC8 | 150/90 mmHg/140/90 mmHg 2 | [12] |
| Hypertension Canada | 140/90 mmHg 3 | [13] |
| ESC/ESH | 140/90 mmHg | [9] |
| ISH | 140/90 mmHg | [10] |
| NICE | 140/90 mmHg 4 | [14] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vischer, A.S.; Burkard, T. How Should We Measure and Deal with Office Blood Pressure in 2021? Diagnostics 2021, 11, 235. https://doi.org/10.3390/diagnostics11020235
Vischer AS, Burkard T. How Should We Measure and Deal with Office Blood Pressure in 2021? Diagnostics. 2021; 11(2):235. https://doi.org/10.3390/diagnostics11020235
Chicago/Turabian StyleVischer, Annina S., and Thilo Burkard. 2021. "How Should We Measure and Deal with Office Blood Pressure in 2021?" Diagnostics 11, no. 2: 235. https://doi.org/10.3390/diagnostics11020235
APA StyleVischer, A. S., & Burkard, T. (2021). How Should We Measure and Deal with Office Blood Pressure in 2021? Diagnostics, 11(2), 235. https://doi.org/10.3390/diagnostics11020235







