Reproducibility and Concurrent Validity of Manual Palpation with Rehabilitative Ultrasound Imaging for Assessing Deep Abdominal Muscle Activity: Analysis with Preferential Ratios
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Clinical Data
2.3. Abdominal Drawing-In Maneuver (ADIM)
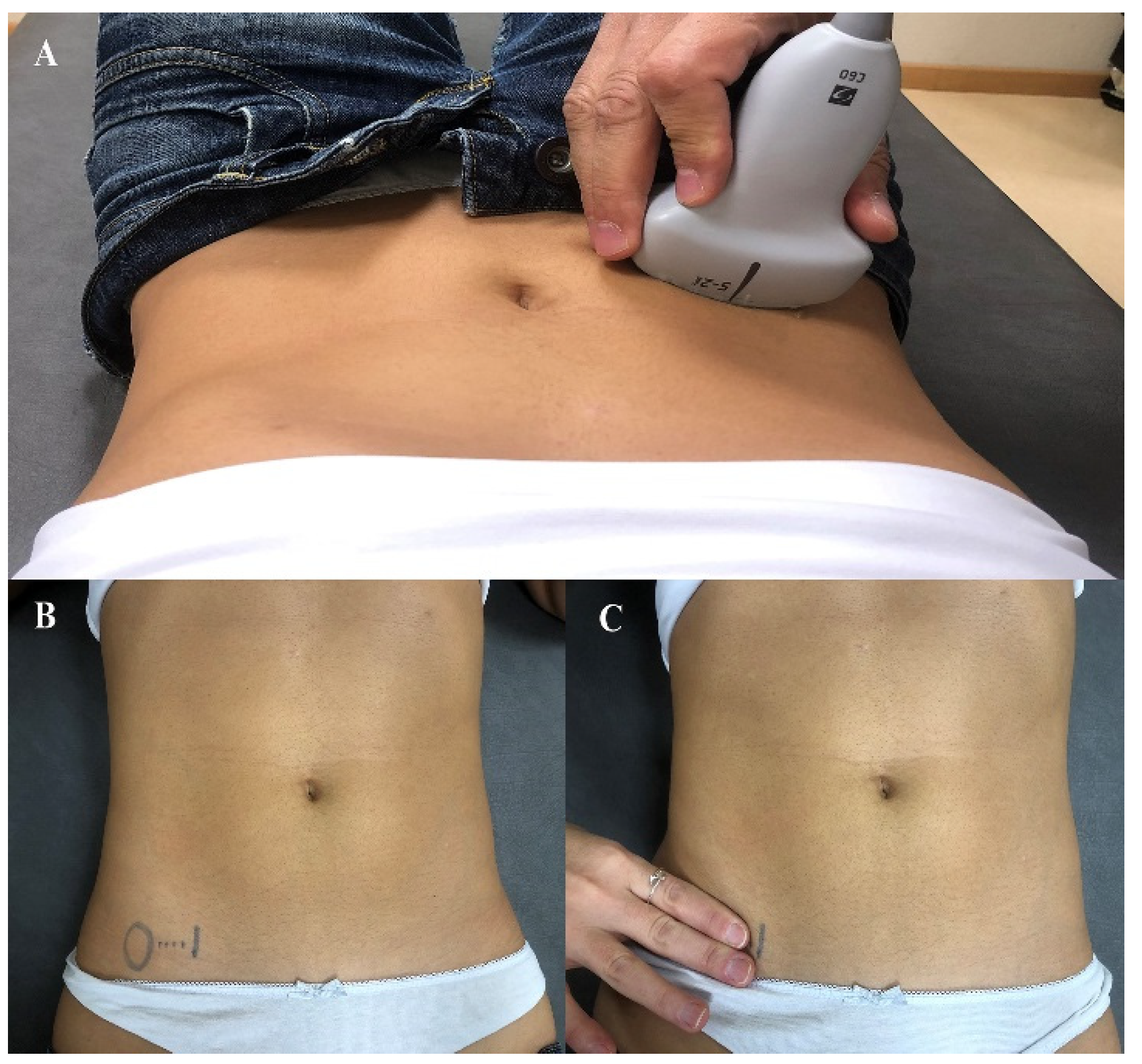
2.4. Rehabilitative Ultrasound Imaging Assessment
2.5. Data Imaging and Management
2.6. Assessors and Reliability Calculation
2.7. Sample Size Calculation
2.8. Statistical Analysis
3. Results
3.1. Participants
3.2. Reliability of US Imaging between Assessors
3.3. Reliability of Manual Palpation during the ADIM
3.4. Concurrent Validity of Manual Palpation
4. Discussion
4.1. Reliability of Manual Palpation during ADIM and RUSI Imaging
4.2. Concurrent Validity of Manual Palpation Compared with RUSI Imaging
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Fatoye, F.; Gebrye, T.; Odeyemi, I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019, 39, 619–626. [Google Scholar] [CrossRef]
- Farahbakhsh, F.; Rostami, M.; Noormohammadpour, P.; Mehraki Zade, A.; Hassanmirazaei, B.; Faghih Jouibari, M.; Kordi, R.; Kennedy, D. Prevalence of low back pain among athletes: A systematic review. J. Back Musculoskelet. Rehabil. 2018, 31, 901–916. [Google Scholar] [CrossRef]
- Beyera, G.K.; O’Brien, J.; Campbell, S. Health-care utilisation for low back pain: A systematic review and meta-analysis of population-based observational studies. Rheumatol. Int. 2019, 39, 1663–1679. [Google Scholar] [CrossRef]
- Dieleman, J.L.; Baral, R.; Birger, M.; Bui, A.L.; Bulchis, A.; Chapin, A.; Hamavid, H.; Horst, C.; Johnson, E.K.; Joseph, J. US spending on personal health care and public health, 1996–2013. JAMA 2016, 316, 2627–2646. [Google Scholar] [CrossRef]
- Hurwitz, E.L.; Randhawa, K.; Yu, H.; Côté, P.; Haldeman, S. The Global Spine Care Initiative: A summary of the global burden of low back and neck pain studies. Eur. Spine J. 2018, 27, S796–S801. [Google Scholar] [CrossRef]
- GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Wong, A.Y.; Parent, E.C.; Funabashi, M.; Kawchuk, G.N. Do changes in transversus abdominis and lumbar multifidus during conservative treatment explain changes in clinical outcomes related to nonspecific low back pain? A systematic review. J. Pain 2014, 15, 377.e1–377.e35. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A. Clinical Guidelines Committee of the American College of Physicians. noninvasive treatments for acute, subacute, and chronic low back pain: A Clinical Practice Guideline from the American College of Physicians. Ann. Intern. Med. 2017, 166, 514–530. [Google Scholar] [CrossRef] [PubMed]
- McGalliard, M.K.; Dedrick, G.S.; Brismée, J.M.; Cook, C.E.; Apte, G.G.; Sizer, P.S., Jr. Changes in transversus abdominis thickness with use of the abdominal drawing-in maneuver during a functional task. PM R 2010, 2, 187–194. [Google Scholar] [CrossRef] [PubMed]
- ShahAli, S.; Shanbehzadeh, S.; ShahAli, S.; Takamjani, I.E. Application of ultrasonography in the assessment of abdominal and lumbar trunk muscle activity in participants with and without low back pain: A systematic review. J. Manip. Physiol. Ther. 2019, 42, 541–550. [Google Scholar] [CrossRef]
- Ellisa, R.; Helsby, J.; Naus, J.; Bassett, S.; Fernández-de-Las-Peñascd, C.; Carneroe, S.F.; Hidesf, J.; O’Sullivan, C.; Teyhen, D.; Stokes, M.; et al. Exploring the use of ultrasound imaging by physiotherapists: An international survey. Musculoskelet. Sci. Pract. 2020, 49, 102213. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, J.L.; Ellis, R.; Hodges, P.W.; OSullivan, C.; Hides, J.; Fernandez-Carnero, S.; Arias-Buria, J.L.; Teyhen, D.S.; Stokes, M.J. Imaging with ultrasound in physical therapy: What is the PT’s scope of practice? A competency-based educational model and training recommendations. Br. J. Sports Med. 2019, 53, 1447–1453. [Google Scholar] [CrossRef]
- Hebert, J.J.; Koppenhaver, S.L.; Parent, E.; Fritz, J.M. A systematic review of the reliability of rehabilitative ultrasound imaging for the quantitative assessment of the abdominal and lumbar trunk muscles. Spine 2009, 34, E848–E856. [Google Scholar] [CrossRef] [PubMed]
- Costa, L.O.; Maher, C.G.; Latimer, J.; Smeets, R.J. Reproducibility of rehabilitative ultrasound imaging for the measurement of abdominal muscle activity: A systematic review. Phys. Ther. 2009, 89, 756–769. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.; Hodges, P.; Hides, J. Therapeutic Exercise for Lumbopelvic Stabilization: A Motor Control Approach for the Treatment and Prevention of Low Back Pain, 2nd ed.; Churchill Livingstone: London, UK, 2004. [Google Scholar]
- Costa, L.O.; Cançado, R.L.; Ferreira, P.H. Short report: Intra-tester reliability of two clinical tests of transversus abdominis muscle recruitment. Physiother. Res. Int. 2006, 11, 48–50. [Google Scholar] [CrossRef] [PubMed]
- Kaping, K.; Äng, B.O.; Rasmussen-Barr, E. The abdominal drawing-in manoeuvre for detecting activity in the deep abdominal muscles: Is this clinical tool reliable and valid? BMJ Open 2015, 5, e008711. [Google Scholar] [CrossRef]
- Jensen, M.P.; Turbner, J.A.; Romano, J.M.; Fisher, L. Comparative reliability and validity of chronic pain intensity measures. Pain 1999, 83, 157–162. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2952. [Google Scholar] [CrossRef]
- Flórez, M.; García, M.A.; García, F. Adaptación transcultural a la población española de la escala de incapacidad por dolor lumbar de Oswestry. Rehabilitación 1995, 29, 138–145. [Google Scholar]
- Ferreira, P.H.; Ferreira, M.L.; Nascimento, D.P.; Pinto, R.Z.; Franco, M.R.; Hodges, P.W. Discriminative and reliability analyses of ultrasound measurement of abdominal muscles recruitment. Man. Ther. 2011, 16, 463–469. [Google Scholar] [CrossRef]
- Henry, S.M.; Westervelt, K.C. The use of real-time ultrasound feedback in teaching abdominal hollowing exercises to healthy subjects. J. Orthop. Sports Phys. Ther. 2005, 35, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Djordjevic, O.; Djordjevic, A.; Konstantinovic, L. Interrater and intrarater reliability of transverse abdominal and lumbar multifidus muscle thickness in subjects with and without low back pain. J. Orthop. Sports Phys. Ther. 2014, 44, 979–988. [Google Scholar] [CrossRef]
- McMeeken, J.M.; Beith, I.D.; Newham, D.J.; Milligan, P.; Critchley, D.J. The relationship between EMG and change in thickness of transversus abdominis. Clin. Biomech. 2004, 19, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.H.; Ferreira, M.L.; Hodges, P.W. Changes in recruitment of the abdominal muscles in people with low back pain: Ultrasound measurement of muscle activity. Spine 2004, 29, 2560–2566. [Google Scholar] [CrossRef] [PubMed]
- Teyhen, D.S.; Miltenberger, C.E.; Deiters, H.M.; Del Toro, Y.M.; Pulliam, J.N.; Childs, J.D.; Boyles, R.E.; Flynn, T.W. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J. Orthop. Sports Phys. Ther. 2005, 35, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Urquhart, D.M.; Hodges, P.W.; Allen, T.J.; Story, I.H. Abdominal muscle recruitment during a range of voluntary exercises. Man. Ther. 2005, 10, 144–153. [Google Scholar] [CrossRef]
- Urquhart, D.M.; Hodges, P.W.; Story, I.H. Postural activity of the abdominal muscles varies between regions of these muscles and between body positions. Gait Posture 2005, 22, 295–301. [Google Scholar] [CrossRef]
- Sim, J.; Wright, C. The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [PubMed]
- Byrt, T.; Bishop, J.; Carlin, J.B. Bias, prevalence and kappa. J. Clin. Epidemiol. 1993, 46, 423–429. [Google Scholar] [CrossRef]
- Landis, J.; Koch, G. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 1977, 33, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Carter, R.; Lubinsky, J.; Domholdt, E. Rehabilitation Research: Prinicipals and Applications, 4th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2011. [Google Scholar]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1988, 240, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Schünemann, H.J.; Griffith, L.E.; Beaton, D.E.; Griffiths, A.F.; Critch, J.N.; Guyattc, G.H. Using the entire cohort in the receiver operating characteristic analysis maximizes precision of the minimal important difference. J. Clin. Epidemiol. 2009, 62, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Eshoj, H.; Ingwersen, K.G.; Larsen, C.M.; Kjaer, B.; Juul-Kristensen, G. Intertester reliability of clinical shoulder instability and laxity tests in subjects with and without self-reported shoulder problems. BMJ Open 2018, 8, e018472. [Google Scholar] [CrossRef]
- Pulkovski, N.; Mannion, A.F.; Caporaso, F.; Toma, V.; Gubler, D.; Helbling, D.; Sprott, H. Ultrasound assessment of transversus abdominis muscle contraction ratio during abdominal hollowing: A useful tool to distinguish between patients with chronic low back pain and healthy controls? Eur. Spine J. 2012, 21, S750–S759. [Google Scholar] [CrossRef]
- Mannion, A.F.; Pulkovski, N.; Toma, V.; Sprott, H. Abdominal muscle size and symmetry at rest and during abdominal hollowing exercises in healthy control subjects. J. Anat. 2008, 213, 173–182. [Google Scholar] [CrossRef]

| Outcome | Asymptomatic Controls (n = 16) | Low Back Pain (n = 16) | p-Value |
|---|---|---|---|
| Mean ± SD/n (%) | Mean ± SD/n (%) | ||
| Age (years) | 29.5 ± 4.5 | 28.5 ± 4.0 | 0.648 |
| Gender (female) | 8 (50%) | 8 (50%) | 1.00 |
| Body mass (kg) | 68.0 ± 9.5 | 67.0 ± 13.0 | 0.854 |
| Height (m) | 1.75 ± 0.1 | 1.70 ± 0.1 | 0.266 |
| BMI (kg/m2) | 22.3 ± 2.0 | 22.9 ± 2.4 | 0.418 |
| VAS (0–100, mm) | – | 39.5 ± 15.9 | – |
| ODI (0–100, %) | – | 24.5 ± 14.5 | – |
| Transversus Abdominis (TrA) | ||||||
|---|---|---|---|---|---|---|
| Outcomes | Mean ± SD | ICC (95 CI) | SEM (mm) | MDC90 (mm; %) | MDC95 (mm; %) | |
| Rater A | Rater B | |||||
| Total Sample (n = 32) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 3.5 ± 0.8 6.2 ± 1.4 2.7 ± 1.4; 77% | 3.4 ± 0.8 6.2 ± 1.5 2.8 ± 1.3; 84% | 0.84 (0.67 to 0.92) 0.86 (0.71 to 0.93) | 0.43 0.72 | 1.01; 29% 1.68; 27% | 1.20; 35% 1.99; 32% |
| Male Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 3.9 ± 0.6 6.4 ± 1.3 2.5 ± 1.5; 64% | 3.8 ± 0.5 6.5 ± 1.4 2.7 ± 1.3; 71% | 0.77 (0.36 to 0.92) 0.89 (0.69 to 0.96) | 0.33 0.61 | 0.76; 20% 1.42; 22% | 0.90; 23% 1.69; 26% |
| Female Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 3.1 ± 0.9 5.9 ± 1.5 2.8 ± 1.3; 90% | 3.0 ± 0.9 5.9 ± 1.5 2.9 ± 1.4; 97% | 0.78 (0.36 to 0.92) 0.83 (0.50 to 0.94) | 0.54 0.83 | 1.26; 41% 1.95; 33% | 1.50; 49% 2.31; 39% |
| Asymptomatic Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 3.6 ± 0.8 6.3 ± 1.6 2.7 ± 1.5; 77% | 3.4 ± 0.8 6.3 ± 1.6 2.8 ± 1.5; 83% | 0.89 (0.68 to 0.96) 0.89 (0.68 to 0.96) | 0.360.75 | 0.84; 24% 1.75; 28% | 1.00; 29% 2.08; 33% |
| Low Back Pain Patients (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 3.4 ± 0.8 6.0 ± 1.1 2.6 ± 1.3; 76% | 3.3 ± 0.9 6.12± 1.3 2.8 ± 1.2; 85% | 0.79 (0.40 to 0.93) 0.81 (0.47 to 0.94) | 0.51 0.070 | 1.19; 35% 1.64; 27% | 1.41; 42% 1.95; 32% |
| Internal Oblique (IO) | ||||||
| Total Sample (n = 32) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 6.6 ± 1.3 8.0 ± 2.1 1.5 ± 2.0; 22% | 6.6 ± 1.5 8.3 ± 2.2 1.7 ± 1.9; 26% | 0.90 (0.80 to 0.95) 0.85 (0.69 to 0.93) | 0.62 1.10 | 1.44; 22% 2.58; 32% | 1.71; 26% 3.06; 37% |
| Male Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 7.1 ± 1.0 8.2 ± 2.3 1.2 ± 1.4; 15% | 7.1 ± 1.3 8.5 ± 1.9 1.2 ± 1.1; 20% | 0.86 (0.60 to 0.95) 0.83 (0.52 to 0.94) | 0.57 1.15 | 1.34; 19% 2.67; 32% | 1.59;22% 3.17; 38% |
| Female Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 6.0 ± 1.4 7.9 ± 2.1 1.9 ± 1.3; 32% | 6.0± 1.6 8.1 ± 2.4 2.1 ± 1.9; 35% | 0.90 (0.70 to 0.96) 0.87 (0.62 to 0.95) | 0.68 1.10 | 1.58; 26% 2.56; 32% | 1.87; 31% 3.04; 38% |
| Asymptomatic Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 7.0 ± 1.3 8.5 ± 2.2 1.5 ± 2.3; 22% | 7.1 ± 1.5 8.6 ± 2.1 1.5 ± 2.1; 22% | 0.90 (0.70 to 0.96) 0.86 (0.60 to 0.95) | 0.64 1.07 | 1.49; 21% 2.50; 29% | 1.77;25% 2.97; 35% |
| Low Back Pain Patients (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 6.2 ± 1.3 7.6 ± 2.0 1.4 ± 1.7; 23% | 6.1 ± 1.4 7.9 ± 2.3 1.9 ± 1.8; 31% | 0.89 (0.68 to 0.96) 0.83 (0.52 to 0.94) | 0.61 1.16 | 1.42; 23% 2.71; 35% | 1.68; 27% 3.22; 41% |
| External Oblique (EO) | ||||||
| Total Sample (n = 32) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 4.7 ± 1.1 5.6 ± 1.5 0.9 ± 1.4; 19% | 4.6 ± 1.2 5.6 ± 1.6 1.0 ± 1.5; 23% | 0.90 (0.80 to 0.95) 0.84 (0.68 to 0.92) | 0.45 0.83 | 1.06; 23% 1.94; 35% | 1.26; 27% 2.31; 41% |
| Male Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 5.0 ± 1.0 5.6 ± 1.4 0.6 ± 1.4; 12% | 4.8 ± 1.2 5.7 ± 1.8 0.9 ± 1.8; 19% | 0.90 (0.72 to 0.96) 0.89 (0.68 to 0.96) | 0.47 0.73 | 1.09; 22% 1.70; 30% | 1.30; 26% 2.02; 36% |
| Female Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 4.4 ± 1.1 5.6 ± 1.7 1.2 ± 1.4; 27% | 4.3 ± 0.9 5.5 ± 1.6 1.2 ± 1.1; 28% | 0.89 (0.69 to 0.96) 0.81 (0.44 to 0.93) | 0.45 0.94 | 1.05; 24% 2.20; 40% | 1.24; 29% 2.61; 47% |
| Asymptomatic Subjects (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 4.9 ± 1.0 5.9 ± 1.6 1.0 ± 1.6; 20% | 4.6 ± 1.0 5.8 ± 1.8 1.2 ± 1.6; 25% | 0.91 (0.72 to 0.97) 0.88 (0.65 to 0.96) | 0.36 0.80 | 0.84; 18% 1.87; 32% | 1.00; 21% 2.22; 38% |
| Low Back Pain Patients (n = 16) | ||||||
| Rest (mm) ADIM (mm) Change (mm; %) | 4.5 ± 1.2 5.2 ± 1.4 0.8 ± 1.2; 17% | 4.5 ± 1.2 5.4 ± 1.5 0.9 ± 1.4;20% | 0.90 (0.71 to 0.97) 0.79 (0.41 to 0.93) | 0.52 0.88 | 1.21; 27% 2.05; 38% | 1.44; 32% 2.44;46% |
| Interrater Reliability | ||||||
|---|---|---|---|---|---|---|
| Outcome | Observed Agreement | Expected Agreement | Prevalence Index | Bias Index | Kappa (95% CI) | PABAK |
| Day 1 | ||||||
| Total Sample (n = 32) | 0.91 | 0.61 | 0.47 | 0.03 | 0.76 (0.50 to 1.00) | 0.81 |
| Males (n = 16) | 0.94 | 0.59 | 0.44 | 0.06 | 0.85 (0.55 to 1.00) | 0.88 |
| Females (n = 16) | 0.88 | 0.63 | 0.50 | 0.01 | 0.67 (0.23 to 1.00) | 0.75 |
| Asymptomatic (n = 16) | 0.94 | 0.66 | 0.56 | 0.06 | 0.82 (0.47 to 1.00) | 0.88 |
| Low Back Pain (n = 16) | 0.88 | 0.56 | 0.38 | 0.13 | 0.71 (0.34 to 1.00) | 0.75 |
| Day 2 | ||||||
| Total Sample (n = 32) | 0.94 | 0.63 | 0.50 | 0.00 | 0.83 (0.61 to 1.00) | 0.88 |
| Males (n = 16) | 0.94 | 0.59 | 0.44 | 0.06 | 0.85 (0.55 to 1.00) | 0.88 |
| Females (n = 16) | 0.94 | 0.66 | 0.56 | 0.06 | 0.82 (0.47 to 1.00) | 0.88 |
| Asymptomatic (n = 16) | 1.00 | 0.70 | 0.63 | 0.00 | 1.00 (1.00 to 1.00) | 1.00 |
| Low Back Pain (n = 16) | 0.88 | 0.57 | 0.38 | 0.00 | 0.71 (0.33 to 1.00) | 0.75 |
| Intrarater Test-Retest Reliability | ||||||
| Outcome | Observed Agreement | Expected Agreement | Prevalence Index | Bias Index | Kappa (95% CI) | PABAK |
| Rater A | ||||||
| Total Sample (n = 32) | 0.94 | 0.63 | 0.5 | 0 | 0.83 (0.61 to 1.00) | 0.88 |
| Males (n = 16) | 0.94 | 0.59 | 0.44 | 0.06 | 0.85 (0.55 to 1.00) | 0.88 |
| Females (n = 16) | 0.94 | 0.66 | 0.56 | 0.06 | 0.82 (0.47 to 1.00) | 0.88 |
| Asymptomatic (n = 16) | 0.94 | 0.66 | 0.56 | 0.06 | 0.82 (0.47 to 1.00) | 0.88 |
| Low Back Pain (n = 16) | 0.94 | 0.59 | 0.44 | 0.06 | 0.85 (0.55 to 1.00) | 0.88 |
| Rater B | ||||||
| Total Sample (n = 32) | 0.97 | 0.61 | 0.47 | 0.03 | 0.92 (0.77 to 1.00) | 0.94 |
| Males (n = 16) | 0.94 | 0.59 | 0.44 | 0.06 | 0.85 (0.55 to 1.00) | 0.88 |
| Females (n = 16) | 1 | 0.63 | 0.5 | 0 | 1.00 (1.00 to 1.00) | 1 |
| Asymptomatic (n = 16) | 1 | 0.7 | 0.63 | 0 | 1.00 (1.00 to 1.00) | 1. 00 |
| Low Back Pain (n = 16) | 0.94 | 0.55 | 0.31 | 0.06 | 0.86 (0.60 to 1.00) | 0.88 |
| Rater | TrA-CR | TrA-PAR | M-TrA-PAR |
|---|---|---|---|
| Rater A | 0.39 * | 0.48 * | 0.60 ** |
| Rater B | 0.36 * | 0.39 * | 0.51 ** |
| TrA-CR | ||||
| Proposed model for the dichotomous transformation of USI measurements: ROC value (95% CI) = 0.60 (0.39–0.82); p = 0.33 Youden Index = 0.25 TrA-CR Cut-off point = 1.32 | ||||
| TrA-PAR * | ||||
| Proposed model for the dichotomous transformation of USI measurements: ROC value (95% CI) = 0.86 (0.71–1.00); p = 0.001 Youden Index = 0.73 TrA-PAR Cut-off point = 0.06 | ||||
| Rater | Sensitivity (95% CI) | Specificity (95% CI) | LR + (95% CI) | LR-(95% CI) |
| ADIM | ||||
| Rater A | 0.90 (0.77–1.00) | 0.33 (0.12–0.55) | 1.35 (1.00–1.93) | 0.30 (0.07–1.00) |
| Rater B | 0.85 (0.69–1.00) | 0.50 (0.22–0.78) | 1.70 (1.00–3.08) | 0.30 (0.09–0.98) |
| M-TrA-PAR * | ||||
| Proposed model for the dichotomous transformation of USI measurements: ROC value (95% CI) = 0.89 (0.74–1.00); p < 0.001 Youden Index = 0.78 M-TrA-PAR Cut-off point = 0.08 | ||||
| Rater | Sensitivity (95% CI) | Specificity (95% CI) | LR + (95% CI) | LR-(95% CI) |
| ADIM | ||||
| Rater A | 1.00 (1.00–1.00) | 0.62 (0.35–0.88) | 2.60 (1.31–5.17) | 0.00 (0.00–0.00) |
| Rater B | 0.95 (0.85–1.00) | 0.62 (0.35–0.88) | 2.46 (1.23–4.94) | 0.09 (0.01–0.60) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valentín-Mazarracin, I.; Nogaledo-Martín, M.; López-de-Uralde-Villanueva, I.; Fernández-de-las-Peñas, C.; Stokes, M.; Arias-Buría, J.L.; Díaz-Arribas, M.J.; Plaza-Manzano, G. Reproducibility and Concurrent Validity of Manual Palpation with Rehabilitative Ultrasound Imaging for Assessing Deep Abdominal Muscle Activity: Analysis with Preferential Ratios. Diagnostics 2021, 11, 298. https://doi.org/10.3390/diagnostics11020298
Valentín-Mazarracin I, Nogaledo-Martín M, López-de-Uralde-Villanueva I, Fernández-de-las-Peñas C, Stokes M, Arias-Buría JL, Díaz-Arribas MJ, Plaza-Manzano G. Reproducibility and Concurrent Validity of Manual Palpation with Rehabilitative Ultrasound Imaging for Assessing Deep Abdominal Muscle Activity: Analysis with Preferential Ratios. Diagnostics. 2021; 11(2):298. https://doi.org/10.3390/diagnostics11020298
Chicago/Turabian StyleValentín-Mazarracin, Irene, Miriam Nogaledo-Martín, Ibai López-de-Uralde-Villanueva, César Fernández-de-las-Peñas, María Stokes, José L. Arias-Buría, María J. Díaz-Arribas, and Gustavo Plaza-Manzano. 2021. "Reproducibility and Concurrent Validity of Manual Palpation with Rehabilitative Ultrasound Imaging for Assessing Deep Abdominal Muscle Activity: Analysis with Preferential Ratios" Diagnostics 11, no. 2: 298. https://doi.org/10.3390/diagnostics11020298
APA StyleValentín-Mazarracin, I., Nogaledo-Martín, M., López-de-Uralde-Villanueva, I., Fernández-de-las-Peñas, C., Stokes, M., Arias-Buría, J. L., Díaz-Arribas, M. J., & Plaza-Manzano, G. (2021). Reproducibility and Concurrent Validity of Manual Palpation with Rehabilitative Ultrasound Imaging for Assessing Deep Abdominal Muscle Activity: Analysis with Preferential Ratios. Diagnostics, 11(2), 298. https://doi.org/10.3390/diagnostics11020298








