Measuring Aqueduct of Sylvius Cerebrospinal Fluid Flow in Multiple Sclerosis Using Different Software
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. MRI Acquisition and Processing
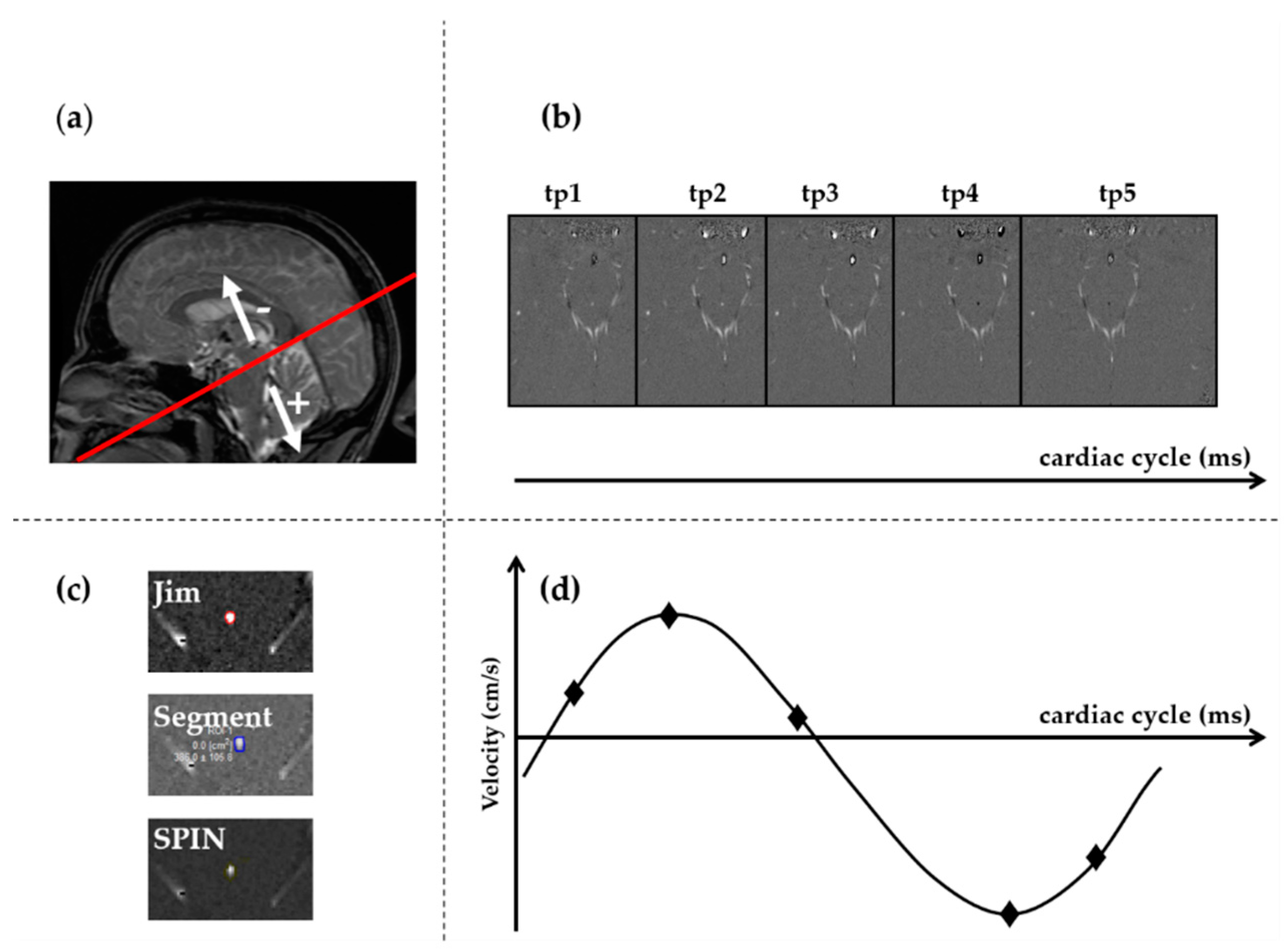
- The time frame with the highest flow, i.e., with the highest contrast of CSF from the surrounding parenchyma, was visually selected (Figure 1B).
- The images were magnified (Figure 1C) so that the AoS was easily visible on the screen, and two kinds of regions of interest (ROIs) were drawn: one corresponding to AoS contour and another one in an area of static tissue (NFA: no-flow area) (Supplementary Figure S1). The latter was used as a reference for correcting the phase background and was manually drawn anteriorly to the AoS [18,21]. The former was drawn semiautomatically or manually in different ways, depending on the software (Figure 1C). In particular, with Jim, we used its semiautomated local thresholding technique, which detects the contours after a pixel of the border is manually identified, as usually done in MS studies for semiautomatic lesion contour drawing [34]. With Segment we manually drew the AoS ROI and then we used the “Refine ROI” tool [33]. With SPIN, we used the region growing approach [20], which requires an initialization with the manual identification of a pixel inside the AoS. All the ROIs were copied to all the time frames. If necessary, a manual adjustment could be performed with all the software packages.
- The velocity, corrected for the phase offset, was computed for each pixel inside the AoS ROI and for each frame of the cardiac cycle (Figure 1D) using each software package. In particular, the velocity was corrected for background velocity by subtracting the average value inside the NFA. The effect of this correction on the mean AoS velocity over the cardiac cycle is shown in Supplementary Figure S2 for one subject, for each software package.
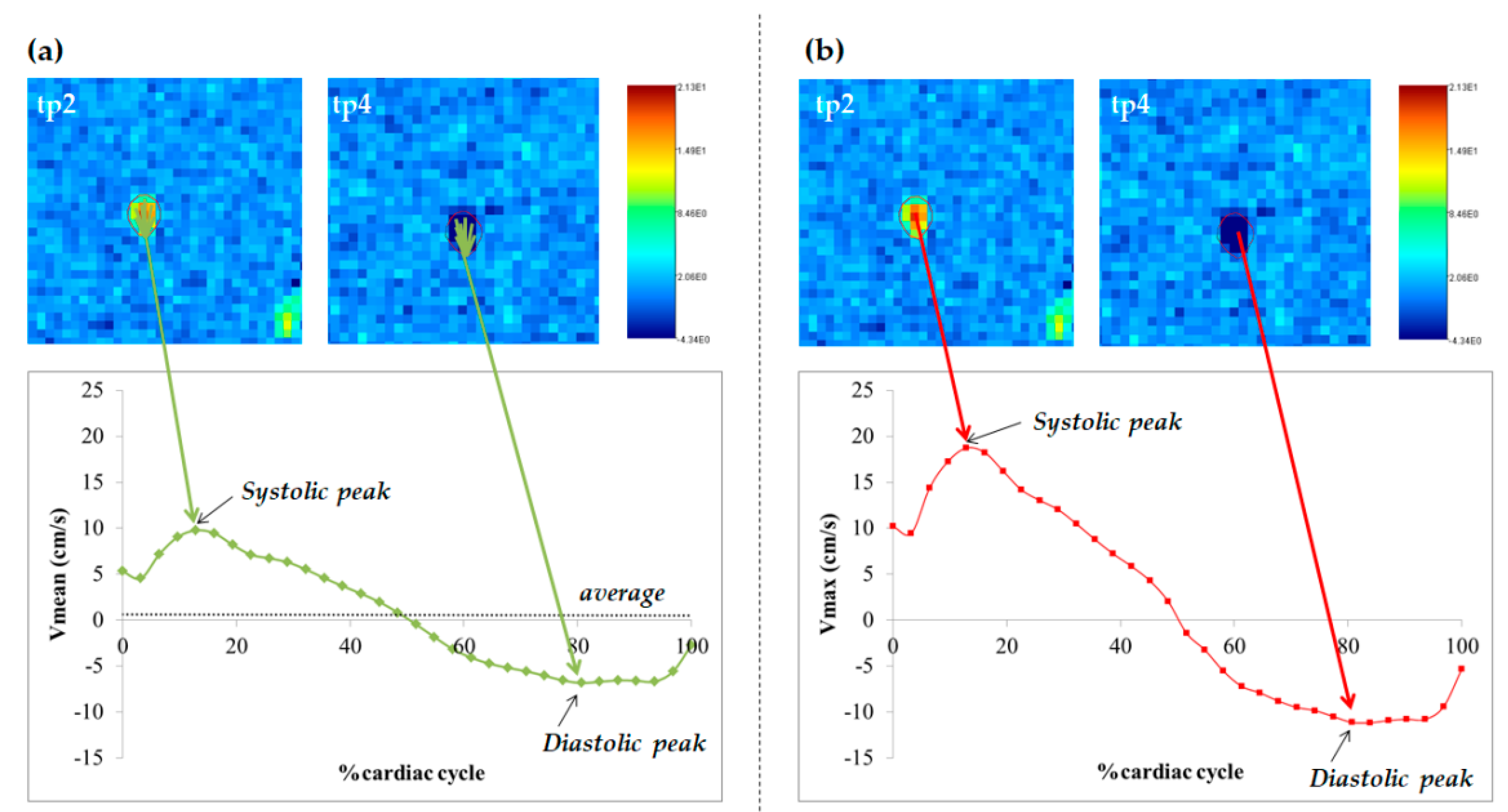
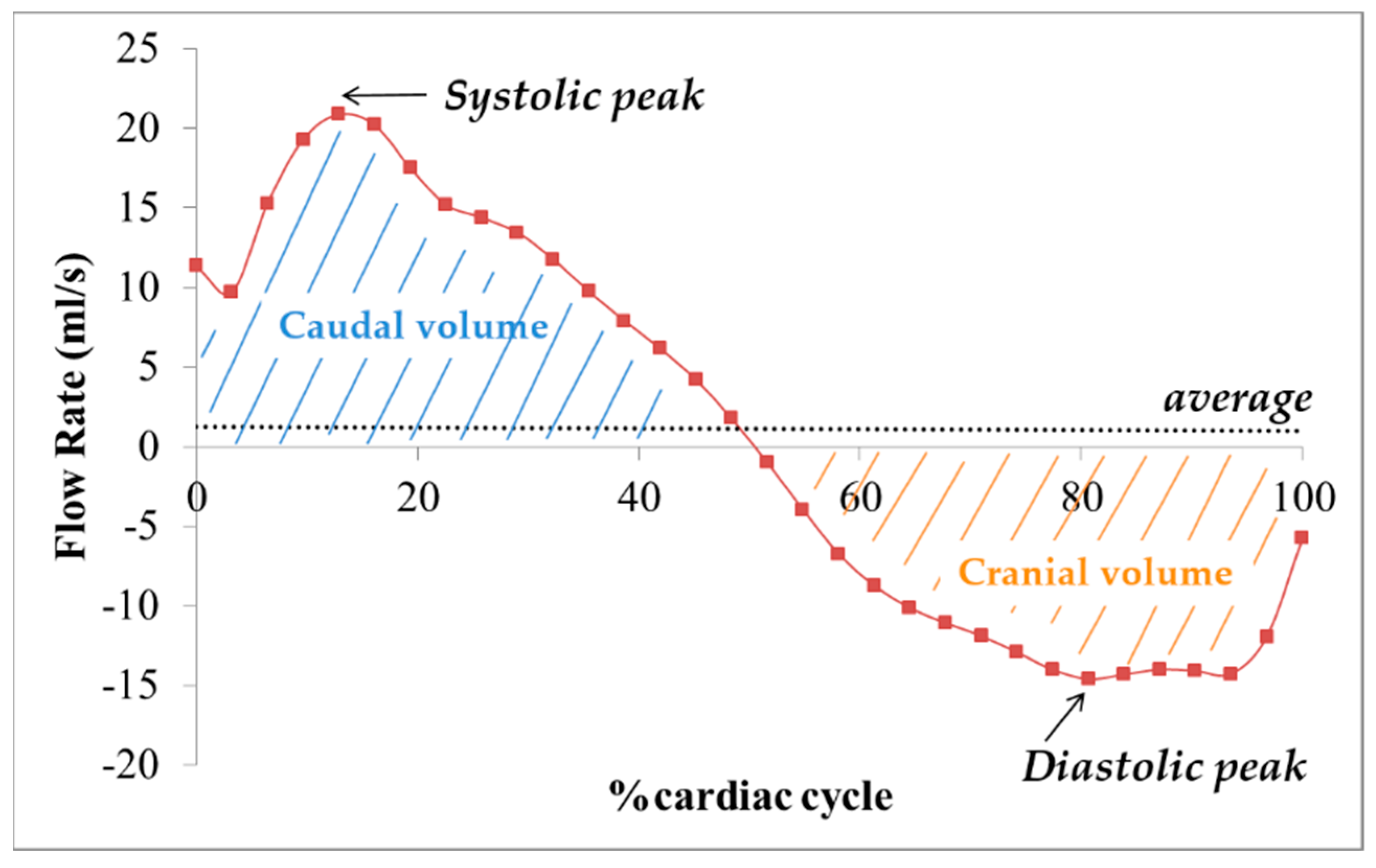
- The following measures were computed for each time frame of the cardiac cycle: (1) the cross-sectional area (CSA, in mm2) of the AoS; (2) mean velocity (Vmean) in cm/s (Figure 2A), as the spatially averaged velocity inside the segmented AoS (sum of all the velocities inside the AoS, divided by the AoS CSA); (3) maximal velocity (Vmax) in cm/s (Figure 2B), as the velocity with the highest value among all the velocities inside the segmented AoS; (4) flow rate (Vmean*AoS CSA) in mL/s (Figure 3). The following measures were computed and retained in the statistical analyses (represented and written in italic in Figure 2 and Figure 3): the average over the cardiac cycle of CSA, Vmean, Vmax, flow rate; the systolic and diastolic peaks of Vmax and Vmean. Moreover, the volumes displaced during the systolic and diastolic phases, i.e., the caudal and cranial volumes, were computed by integrating over time the flow rate to the fourth and third ventricle respectively. The net flow volume was the difference between the two last volumes (considered as absolute measures).
2.3. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics
3.2. Phase Contrast Data Quality
3.3. Repeatability Results
3.4. Reproducibility Results: Differences among Software Packages and between Groups
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Telano, L.N.; Baker, S. Physiology, Cerebral Spinal Fluid; StatPearls: Treasure Island, FL, USA, 2020. [Google Scholar]
- McKnight, C.D.; Rouleau, R.M.; Donahue, M.J.; Claassen, D.O. The Regulation of Cerebral Spinal Fluid Flow and Its Relevance to the Glymphatic System. Curr. Neurol. Neurosci. Rep. 2020, 20, 58. [Google Scholar] [CrossRef] [PubMed]
- Schroth, G.; Klose, U. Cerebrospinal fluid flow. Neuroradiology 1992, 35, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Beggs, C.B.; Shepherd, S.J.; Cecconi, P.; Lagana, M.M. Predicting the aqueductal cerebrospinal fluid pulse: A statistical approach. Appl. Sci. 2019, 9, 2131. [Google Scholar] [CrossRef] [Green Version]
- Korbecki, A.; Zimny, A.; Podgorski, P.; Sasiadek, M.; Bladowska, J. Imaging of cerebrospinal fluid flow: Fundamentals, techniques, and clinical applications of phase-contrast magnetic resonance imaging. Pol. J. Radiol. 2019, 84, e240–e250. [Google Scholar] [CrossRef]
- Bradley, W.G., Jr. Magnetic Resonance Imaging of Normal Pressure Hydrocephalus. Semin. Ultrasound CT MR 2016, 37, 120–128. [Google Scholar] [CrossRef]
- Stoquart-El Sankari, S.; Lehmann, P.; Gondry-Jouet, C.; Fichten, A.; Godefroy, O.; Meyer, M.E.; Baledent, O. Phase-contrast MR imaging support for the diagnosis of aqueductal stenosis. AJNR Am. J. Neuroradiol. 2009, 30, 209–214. [Google Scholar] [CrossRef] [Green Version]
- Long, J.; Lin, H.; Cao, G.; Wang, M.Z.; Huang, X.J.; Xia, J.; Sun, Z. Relationship between intracranial pressure and phase-contrast cine MRI-derived measures of cerebrospinal fluid parameters in communicating hydrocephalus. Quant. Imaging Med. Surg. 2019, 9, 1413–1420. [Google Scholar] [CrossRef]
- Beggs, C.B.; Magnano, C.; Shepherd, S.J.; Belov, P.; Ramasamy, D.P.; Hagemeier, J.; Zivadinov, R. Dirty-appearing white matter in the brain is associated with altered cerebrospinal fluid pulsatility and hypertension in individuals without neurologic disease. J. Neuroimaging 2016, 26, 136–143. [Google Scholar] [CrossRef] [Green Version]
- Öner, S.; Kahraman, A.S.; Özcan, C.; Özdemir, Z.M.; Ünlü, S.; Kamışlı, Ö.; Öner, Z. Cerebrospinal Fluid Dynamics in Patients with Multiple Sclerosis: The Role of Phase-Contrast MRI in the Differential Diagnosis of Active and Chronic Disease. Korean J. Radiol. 2018, 19, 72–78. [Google Scholar] [CrossRef]
- Magnano, C.; Schirda, C.; Weinstock-Guttman, B.; Wack, D.S.; Lindzen, E.; Hojnacki, D.; Bergsland, N.; Kennedy, C.; Belov, P.; Dwyer, M.G.; et al. Cine cerebrospinal fluid imaging in multiple sclerosis. J. Magn. Reson. Imaging 2012, 36, 825–834. [Google Scholar] [CrossRef]
- Gorucu, Y.; Albayram, S.; Balci, B.; Hasiloglu, Z.I.; Yenigul, K.; Yargic, F.; Keser, Z.; Kantarci, F.; Kiris, A. Cerebrospinal fluid flow dynamics in patients with multiple sclerosis: A phase contrast magnetic resonance study. Funct. Neurol. 2011, 26, 215–222. [Google Scholar] [PubMed]
- Jakimovski, D.; Zivadinov, R.; Weinstock-Guttman, B.; Bergsland, N.; Dwyer, M.G.; Lagana, M.M. Longitudinal analysis of cerebral aqueduct flow measures: Multiple sclerosis flow changes driven by brain atrophy. Fluids Barriers CNS 2020, 17, 9. [Google Scholar] [CrossRef] [PubMed]
- Luetmer, P.H.; Huston, J.; Friedman, J.A.; Dixon, G.R.; Petersen, R.C.; Jack, C.R.; McClelland, R.L.; Ebersold, M. Measurement of cerebrospinal fluid flow at the cerebral aqueduct by use of phase-contrast magnetic resonance imaging: Technique validation and utility in diagnosing idiopathic normal pressure hydrocephalus. J. Neurosurg. 2002, 50, 534–543. [Google Scholar]
- El Sankari, S.; Gondry-Jouet, C.; Fichten, A.; Godefroy, O.; Serot, J.M.; Deramond, H.; Meyer, M.E.; Balédent, O. Cerebrospinal fluid and blood flow in mild cognitive impairment and Alzheimer’s disease: A differential diagnosis from idiopathic normal pressure hydrocephalus. J. Fluids Barriers CNS 2011, 8, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zamboni, P.; Menegatti, E.; Weinstock-Guttman, B.; Schirda, C.; Cox, J.L.; Malagoni, A.M.; Hojanacki, D.; Kennedy, C.; Carl, E.; Dwyer, M.G.; et al. The severity of chronic cerebrospinal venous insufficiency in patients with multiple sclerosis is related to altered cerebrospinal fluid dynamics. Funct. Neurol. 2009, 24, 133–138. [Google Scholar] [PubMed]
- Lotz, J.; Döker, R.; Noeske, R.; Schüttert, M.; Felix, R.; Galanski, M.; Gutberlet, M.; Meyer, G.P. In vitro validation of phase-contrast flow measurements at 3 T in comparison to 1.5 T: Precision, accuracy, and signal-to-noise ratios. J. Magn. Reson. Imaging 2005, 21, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Markenroth Bloch, K.; Töger, J.; Ståhlberg, F. Investigation of cerebrospinal fluid flow in the cerebral aqueduct using high-resolution phase contrast measurements at 7T MRI. J. Acta Radiol. 2018, 59, 988–996. [Google Scholar] [CrossRef]
- Wåhlin, A.; Ambarki, K.; Hauksson, J.; Birgander, R.; Malm, J.; Eklund, A. Phase contrast MRI quantification of pulsatile volumes of brain arteries, veins, and cerebrospinal fluids compartments: Repeatability and physiological interactions. J. Magn. Reson. Imaging 2012, 35, 1055–1062. [Google Scholar] [CrossRef]
- Jiang, J.; Kokeny, P.; Ying, W.; Magnano, C.; Zivadinov, R.; Mark Haacke, E. Quantifying errors in flow measurement using phase contrast magnetic resonance imaging: Comparison of several boundary detection methods. Magn. Reson. Imaging 2015, 33, 185–193. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Lee, H.K.; Kim, J.K.; Kim, H.J.; Park, J.K.; Choi, C.G. CSF flow quantification of the cerebral aqueduct in normal volunteers using phase contrast cine MR imaging. J. Korean J. Radiol. 2004, 5, 81–86. [Google Scholar] [CrossRef] [Green Version]
- Tawfik, A.M.; Elsorogy, L.; Abdelghaffar, R.; Naby, A.A.; Elmenshawi, I. Phase-contrast MRI CSF flow measurements for the diagnosis of normal-pressure hydrocephalus: Observer agreement of velocity versus volume parameters. J. Am. J. Roentgenol. 2017, 208, 838–843. [Google Scholar] [CrossRef] [PubMed]
- Sartoretti, T.; Wyss, M.; Sartoretti, E.; Reischauer, C.; Hainc, N.; Graf, N.; Binkert, C.; Najafi, A.; Sartoretti, S. Sex and age dependencies of aqueductal cerebrospinal fluid dynamics parameters in healthy subjects. J. Front. Aging Neurosci. 2019, 11, 199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindstrøm, E.K.; Ringstad, G.; Mardal, K.-A.; Eide, P.K. Cerebrospinal fluid volumetric net flow rate and direction in idiopathic normal pressure hydrocephalus. J. NeuroImage Clin. 2018, 20, 731–741. [Google Scholar] [CrossRef] [PubMed]
- Flórez, Y.N.; Moratal, D.; Forner, J.; Martí-Bonmatí, L.; Arana, E.; Guajardo-Hernández, U.; Millet-Roig, J. Semiautomatic analysis of phase contrast magnetic resonance imaging of cerebrospinal fluid flow through the aqueduct of Sylvius. Magn. Reson. Mater. Phys. Biol. Med. 2006, 19, 78. [Google Scholar] [CrossRef]
- Alperin, N.; Lee, S.H. PUBS: Pulsatility-based segmentation of lumens conducting non-steady flow. Magn. Reson. Med. 2003, 49, 934–944. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K.; Takahashi, H.; Saijo, M.; Ueguchi, T.; Tanaka, H.; Fujita, N.; Murase, K. Phase-contrast MR studies of CSF flow rate in the cerebral aqueduct and cervical subarachnoid space with correlation-based segmentation. Magn. Reson. Med Sci. 2009, 8, 91–100. [Google Scholar] [CrossRef] [Green Version]
- Balédent, O.; Idy-peretti, I. Cerebrospinal fluid dynamics and relation with blood flow: A magnetic resonance study with semiautomated cerebrospinal fluid segmentation. J. Investig. Radiol. 2001, 36, 368–377. [Google Scholar] [CrossRef]
- Kapsalaki, E.; Svolos, P.; Tsougos, I.; Theodorou, K.; Fezoulidis, I.; Fountas, K.N. Quantification of normal CSF flow through the aqueduct using PC-cine MRI at 3T. In Hydrocephalus; Springer: Berlin/Heidelberg, Germany, 2012; pp. 39–42. [Google Scholar]
- Beggs, C.B.; Magnano, C.; Belov, P.; Krawiecki, J.; Ramasamy, D.P.; Hagemeier, J.; Zivadinov, R. Internal Jugular Vein Cross-Sectional Area and Cerebrospinal Fluid Pulsatility in the Aqueduct of Sylvius: A Comparative Study between Healthy Subjects and Multiple Sclerosis Patients. PLoS ONE 2016, 11, e0153960. [Google Scholar] [CrossRef] [Green Version]
- Polman, C.H.; Reingold, S.C.; Banwell, B.; Clanet, M.; Cohen, J.A.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 2011, 69, 292–302. [Google Scholar] [CrossRef] [Green Version]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [Green Version]
- Heiberg, E.; Sjogren, J.; Ugander, M.; Carlsson, M.; Engblom, H.; Arheden, H. Design and validation of Segment--freely available software for cardiovascular image analysis. BMC Med. Imaging 2010, 10, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laganà, M.M.; Mendozzi, L.; Pelizzari, L.; Bergsland, N.P.; Pugnetti, L.; Cecconi, P.; Baselli, G.; Clerici, M.; Nemni, R.; Baglio, F. Are cerebral perfusion and atrophy linked in multiple sclerosis? Evidence for a multifactorial approach to assess neurodegeneration. J. Curr. Neurovascular Res. 2018, 15, 282–291. [Google Scholar] [CrossRef]
- Bartko, J.J. The intraclass correlation coefficient as a measure of reliability. Psychol. Rep. 1966, 19, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Pirastru, A.; Pelizzari, L.; Bergsland, N.; Cazzoli, M.; Cecconi, P.; Baglio, F.; Lagana, M.M. Consistent Cerebral Blood Flow Covariance Networks across Healthy Individuals and Their Similarity with Resting State Networks and Vascular Territories. Diagnostics 2020, 10, 963. [Google Scholar] [CrossRef]
- Huang, T.-Y.; Chung, H.-W.; Chen, M.-Y.; Giiang, L.-H.; Chin, S.-C.; Lee, C.-S.; Chen, C.-Y.; Liu, Y.-J. Supratentorial cerebrospinal fluid production rate in healthy adults: Quantification with two-dimensional cine phase-contrast MR imaging with high temporal and spatial resolution. Radiology 2004, 233, 603–608. [Google Scholar] [CrossRef]
- Bateman, G.A.; Lechner-Scott, J.; Lea, R.A. A comparison between the pathophysiology of multiple sclerosis and normal pressure hydrocephalus: Is pulse wave encephalopathy a component of MS? Fluids Barriers CNS 2016, 13, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Demographic/Clinical Variable | MS | NC | p-Value |
|---|---|---|---|
| N | 30 | 19 | - |
| Age in years, mean ± SD | 51.8 ± 8.8 | 48.4 ± 12.5 | 0.261 § |
| Sex (M/F) | 13/17 | 5/14 | 0.362 # |
| Disease duration in years, mean ± SD | 17.5 ± 11.0 | - | - |
| EDSS, median (IQR) | 2.5 (1.5–6.0) | - | - |
| RRMS/PMS | 17/13 | ||
| DMT, n (%) | - | - | |
| Interferon-β | 9 (30.0) | - | - |
| Glatiramer acetate | 8 (26.7) | - | - |
| Natalizumab | 7 (23.3) | - | - |
| No DMT | 6 (20.0) | - | - |
| Variable of Interest | ICC Values (n = 10) | |||
|---|---|---|---|---|
| Jim | Segment | SPIN | ||
| CSA | average | 0.884 | 0.889 | 0.823 |
| Vmean | systolic peak | 0.699 | 0.985 | 0.948 |
| diastolic peak | 0.954 | 0.954 | 0.926 | |
| average | 0.644 # | 0.922 | 0.848 | |
| Vmax | systolic peak | 0.998 | 1.000 | 0.998 |
| diastolic peak | 0.927 | 1.000 | 0.997 | |
| Flow Rate | systolic peak | 0.831 | 0.957 | 0.932 |
| diastolic peak | 0.968 | 0.951 | 0.837 | |
| average | 0.281 n.s. | 0.785 * | 0.866 | |
| Volume | systolic | 0.956 | 0.989 | 0.963 |
| diastolic | 0.958 | 0.972 | 0.923 | |
| Net | 0.293 n.s. | 0.794 * | 0.879 | |
| Model Variables | B | Std. Error | t | 95% Confidence Interval | Partial Eta Squared | Sig. | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| CSA | |||||||
| age | 0.026 | 0.009 | 2.969 | 0.009 | 0.043 | 0.059 | 0.004 * |
| sex | −0.597 | 0.185 | −3.224 | −0.963 | −0.231 | 0.069 | 0.002 * |
| Jim | −0.083 | 0.211 | −0.394 | −0.500 | 0.334 | 0.001 | 0.694 |
| Segment | 0.103 | 0.211 | 0.487 | −0.314 | 0.519 | 0.002 | 0.627 |
| group | 0.607 | 0.181 | 3.359 | 0.250 | 0.964 | 0.074 | 0.001 * |
| Vmean systolic peak | |||||||
| age | 0.028 | 0.017 | 1.590 | −0.007 | 0.062 | 0.018 | 0.114 |
| sex | −1.028 | 0.370 | −2.776 | −1.760 | −0.296 | 0.052 | 0.006 * |
| Jim | 0.032 | 0.421 | 0.077 | −0.800 | 0.865 | 0.000 | 0.939 |
| Segment | −0.044 | 0.421 | −0.105 | −0.877 | 0.788 | 0.000 | 0.916 |
| group | 0.695 | 0.361 | 1.924 | −0.019 | 1.409 | 0.026 | 0.056 |
| Vmean diastolic peak | |||||||
| age | 0.007 | 0.013 | 0.515 | −0.019 | 0.033 | 0.002 | 0.608 |
| sex | 0.471 | 0.284 | 1.655 | −0.091 | 1.033 | 0.019 | 0.100 |
| Jim | −0.246 | 0.324 | −0.759 | −0.886 | 0.394 | 0.004 | 0.449 |
| Segment | −0.100 | 0.324 | −0.307 | −0.739 | 0.540 | 0.001 | 0.759 |
| group | −0.823 | 0.278 | −2.966 | −1.372 | −0.275 | 0.059 | 0.004 * |
| Average Vmean | |||||||
| age | −0.003 | 0.002 | −1.091 | −0.007 | 0.002 | 0.008 | 0.277 |
| sex | −0.102 | 0.052 | −1.976 | −0.205 | 0.000 | 0.027 | 0.050 |
| Jim | −0.044 | 0.059 | −0.752 | −0.161 | 0.072 | 0.004 | 0.453 |
| Segment | −0.029 | 0.059 | −0.491 | −0.145 | 0.087 | 0.002 | 0.624 |
| group | −0.051 | 0.050 | −1.005 | −0.151 | 0.049 | 0.007 | 0.316 |
| Vmax systolic peak | |||||||
| age | 0.138 | 0.029 | 4.842 | 0.082 | 0.195 | 0.143 | 0.000 * |
| sex | −1.279 | 0.611 | −2.095 | −2.486 | −0.072 | 0.030 | 0.038 * |
| Jim | −0.044 | 0.695 | −0.063 | −1.417 | 1.330 | 0.000 | 0.950 |
| Segment | −0.071 | 0.695 | −0.102 | −1.444 | 1.303 | 0.000 | 0.919 |
| group | 0.562 | 0.596 | 0.943 | −0.616 | 1.740 | 0.006 | 0.347 |
| Vmax diastolic peak | |||||||
| age | −0.049 | 0.019 | −2.567 | −0.086 | −0.011 | 0.045 | 0.011 * |
| sex | 0.892 | 0.406 | 2.196 | 0.089 | 1.695 | 0.033 | 0.030 * |
| Jim | 0.003 | 0.462 | 0.006 | −0.911 | 0.916 | 0.000 | 0.995 |
| Segment | −0.030 | 0.462 | −0.064 | −0.943 | 0.884 | 0.000 | 0.949 |
| group | −1.495 | 0.396 | −3.772 | −2.279 | −0.712 | 0.092 | 0.000 * |
| FR systolic peak | |||||||
| age | 0.090 | 0.038 | 2.391 | 0.016 | 0.165 | 0.039 | 0.018 * |
| sex | −3.769 | 0.806 | −4.676 | −5.363 | −2.176 | 0.134 | 0.000 * |
| Jim | −0.050 | 0.917 | −0.055 | −1.863 | 1.763 | 0.000 | 0.956 |
| Segment | 0.341 | 0.917 | 0.372 | −1.472 | 2.154 | 0.001 | 0.711 |
| group | 2.341 | 0.787 | 2.976 | 0.786 | 3.896 | 0.059 | 0.003 * |
| FR diastolic peak | |||||||
| age | −0.026 | 0.029 | −0.874 | −0.084 | 0.032 | 0.005 | 0.383 |
| sex | 2.087 | 0.629 | 3.318 | 0.844 | 3.331 | 0.072 | 0.001 * |
| Jim | 0.041 | 0.716 | 0.057 | −1.374 | 1.456 | 0.000 | 0.954 |
| Segment | −0.366 | 0.716 | −0.511 | −1.781 | 1.049 | 0.002 | 0.610 |
| group | −2.137 | 0.614 | −3.481 | −3.351 | −0.923 | 0.079 | 0.001 * |
| Average FR | |||||||
| age | −0.001 | 0.005 | −0.263 | −0.010 | 0.008 | 0.000 | 0.793 |
| sex | −0.302 | 0.099 | −3.047 | −0.498 | −0.106 | 0.062 | 0.003 * |
| Jim | 0.052 | 0.113 | 0.458 | −0.171 | 0.274 | 0.001 | 0.648 |
| Segment | −0.002 | 0.113 | −0.020 | −0.225 | 0.221 | 0.000 | 0.984 |
| group | 0.151 | 0.097 | 1.558 | −0.040 | 0.342 | 0.017 | 0.121 |
| Caudal volume | |||||||
| age | 0.445 | 0.183 | 2.429 | 0.083 | 0.808 | 0.040 | 0.016 * |
| sex | −18.134 | 3.922 | −4.623 | −25.888 | −10.379 | 0.132 | 0.000 * |
| Jim | 0.509 | 4.462 | 0.114 | −8.313 | 9.331 | 0.000 | 0.909 |
| Segment | 1.895 | 4.462 | 0.425 | −6.927 | 10.716 | 0.001 | 0.672 |
| group | 10.495 | 3.828 | 2.742 | 2.927 | 18.062 | 0.051 | 0.007 * |
| Cranial volume | |||||||
| age | −0.447 | 0.181 | −2.467 | −0.805 | −0.089 | 0.041 | 0.015 * |
| sex | 12.802 | 3.876 | 3.303 | 5.140 | 20.464 | 0.072 | 0.001 * |
| Jim | 0.371 | 4.409 | 0.084 | −8.346 | 9.088 | 0.000 | 0.933 |
| Segment | −2.094 | 4.409 | −0.475 | −10.811 | 6.623 | 0.002 | 0.636 |
| group | −7.856 | 3.782 | −2.077 | −15.334 | −0.379 | 0.030 | 0.040 * |
| Net volume | |||||||
| age | −0.002 | 0.076 | −0.021 | −0.151 | 0.148 | 0.000 | 0.984 |
| sex | −5.332 | 1.619 | −3.294 | −8.532 | −2.131 | 0.071 | 0.001 * |
| Jim | 0.880 | 1.842 | 0.478 | −2.761 | 4.520 | 0.002 | 0.634 |
| Segment | −0.199 | 1.842 | −0.108 | −3.840 | 3.441 | 0.000 | 0.914 |
| group | 2.638 | 1.580 | 1.670 | −0.485 | 5.761 | 0.019 | 0.097 |
| PC-Derived Variable | Software | GLM Analysis p-Value | RM-ANOVA Analysis p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Jim | Segment | SPIN | Jim vs. Segment | Jim vs. SPIN | Segment vs. SPIN | Jim vs. Segment | Jim vs. SPIN | Segment vs. SPIN | ||
| CSA (mm2) | average | 2.59 ± 1.09 | 2.78 ± 1.22 | 2.68 ± 1.23 | 1 | 1 | 1 | 0.033 * | 1.000 | 0.421 |
| Vmean (cm/s) | systolic peak | 5.64 ± 2.20 | 5.56 ± 2.23 | 5.6 ± 2.19 | 1 | 1 | 1 | 0.798 | 1.000 | 1.000 |
| diastolic peak | −4.43 ± 1.8 | −4.28 ± 1.62 | −4.18 ± 1.54 | 1 | 1 | 1 | 0.235 | 0.044 * | 0.352 | |
| average | 0.19 ± 0.3 | 0.21 ± 0.29 | 0.23 ± 0.28 | 1 | 1 | 1 | 1.000 | 0.577 | 0.931 | |
| Vmax (cm/s) | systolic peak | 9.65 ± 3.88 | 9.62 ± 3.84 | 9.70 ± 3.90 | 1 | 1 | 1 | 0.982 | 0.496 | 0.101 |
| diastolic peak | −7.01 ± 2.49 | −7.04 ± 2.5 | −7.02 ± 2.50 | 1 | 1 | 1 | 1.000 | 1.000 | 1.000 | |
| Flow rate (mL/min) | systolic peak | 9.21 ± 5.22 | 9.60 ± 5.29 | 9.26 ± 5.26 | 1 | 1 | 1 | 0.149 | 1.000 | 0.089 |
| diastolic peak | −6.92 ± 3.67 | −7.32 ± 4.1 | −6.96 ± 3.87 | 1 | 1 | 1 | 0.064 | 1.000 | 0.082 | |
| average | 0.36 ± 0.59 | 0.3 ± 0.66 | 0.31 ± 0.47 | 1 | 1 | 1 | 1.000 | 1.000 | 1.000 | |
| volume (µL/cc) | caudal volume | 31.89 ± 22.65 | 33.26 ± 23.51 | 32.04 ± 24.55 | 1 | 1 | 1 | 0.244 | 1.000 | 0.068 |
| cranial volume | −27.39 ± 24.61 | −31.76 ± 32.71 | −29.50 ± 27.37 | 1 | 1 | 1 | 0.103 | 1.000 | 0.106 | |
| net | 4.50 ± 5.46 | 1.50 ± 14.7 | 2.54 ± 3.88 | 1 | 1 | 1 | 1.000 | 1.000 | 1.000 | |
| Jim | Segment | SPIN | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NC | MS | p-Value | NC | MS | p-Value | NC | MS | p-Value | ||
| CSA (mm2) | 2.07 ± 0.87 | 2.93 ± 1.09 | 0.020 * | 2.29 ± 1.15 | 3.09 ± 1.19 | 0.084 | 2.22 ± 1.24 | 2.96 ± 1.16 | 0.120 | |
| Vmean (cm/s) | systolic peak | 5.11 ± 2.19 | 5.97 ± 2.18 | 0.377 | 4.96 ± 2.09 | 5.94 ± 2.26 | 0.277 | 4.96 ± 1.96 | 6.01 ± 2.26 | 0.211 |
| diastolic peak | −3.81 ± 2.19 | −4.82 ± 1.42 | 0.082 | −3.76 ± 2.06 | −4.61 ± 1.18 | 0.11 | −3.70 ± 1.98 | −4.48 ± 1.12 | 0.113 | |
| average | 0.26 ± 0.27 | 0.15 ± 0.32 | 0.169 | 0.22 ± 0.34 | 0.19 ± 0.26 | 0.637 | 0.23 ± 0.23 | 0.24 ± 0.31 | 0.853 | |
| Vmax (cm/s) | systolic peak | 8.90 ± 4.30 | 10.12 ± 3.58 | 0.614 | 8.83 ± 4.22 | 10.13 ± 3.56 | 0.567 | 8.91 ± 4.30 | 10.20 ± 3.61 | 0.610 |
| diastolic peak | −6.08 ± 2.85 | −7.59 ± 2.06 | 0.036 * | −6.14 ± 2.91 | −7.61 ± 2.06 | 0.045 * | −6.05 ± 2.92 | −7.64 ± 2.01 | 0.035 * | |
| Flow Rate (mL/min) | systolic peak | 7.56 ± 6.37 | 9.83 ± 4.13 | 0.078 | 7.75 ± 6.38 | 10.26 ± 4.23 | 0.101 | 7.51 ± 6.62 | 9.93 ± 3.98 | 0.124 |
| diastolic peak | −5.54 ± 4.46 | −7.49 ± 2.80 | 0.019 * | −5.68 ± 4.85 | −8.12 ± 3.28 | 0.095 | −5.18 ± 4.17 | −7.73 ± 3.26 | 0.075 | |
| average | 0.30 ± 0.34 | 0.40 ± 0.71 | 0.811 | 0.12 ± 0.87 | 0.42 ± 0.47 | 0.214 | 0.18 ± 0.24 | 0.39 ± 0.55 | 0.209 | |
| Volume (µL/cc) | caudal | 31.89 ± 22.65 | 47.37 ± 26.05 | 0.117 | 33.26 ± 23.51 | 48.76 ± 24.65 | 0.113 | 32.04 ± 24.55 | 46.44 ± 24.74 | 0.158 |
| cranial | −27.39 ± 24.61 | −40.96 ± 19.17 | 0.105 | −31.76 ± 32.71 | −42.21 ± 19.77 | 0.375 | −29.50 ± 27.37 | −40.22 ± 20.01 | 0.301 | |
| net | 4.50 ± 5.46 | 6.41 ± 11.6 | 0.738 | 1.50 ± 14.7 | 6.54 ± 7.66 | 0.219 | 2.54 ± 3.88 | 6.21 ± 8.86 | 0.182 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laganà, M.M.; Jakimovski, D.; Bergsland, N.; Dwyer, M.G.; Baglio, F.; Zivadinov, R. Measuring Aqueduct of Sylvius Cerebrospinal Fluid Flow in Multiple Sclerosis Using Different Software. Diagnostics 2021, 11, 325. https://doi.org/10.3390/diagnostics11020325
Laganà MM, Jakimovski D, Bergsland N, Dwyer MG, Baglio F, Zivadinov R. Measuring Aqueduct of Sylvius Cerebrospinal Fluid Flow in Multiple Sclerosis Using Different Software. Diagnostics. 2021; 11(2):325. https://doi.org/10.3390/diagnostics11020325
Chicago/Turabian StyleLaganà, Maria Marcella, Dejan Jakimovski, Niels Bergsland, Michael G. Dwyer, Francesca Baglio, and Robert Zivadinov. 2021. "Measuring Aqueduct of Sylvius Cerebrospinal Fluid Flow in Multiple Sclerosis Using Different Software" Diagnostics 11, no. 2: 325. https://doi.org/10.3390/diagnostics11020325






