Wavy Floating Greater Omentum Findings Are Useful for Differentiating the Etiology of Fetal Ascites
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Summary of Fetal Ascites Cases
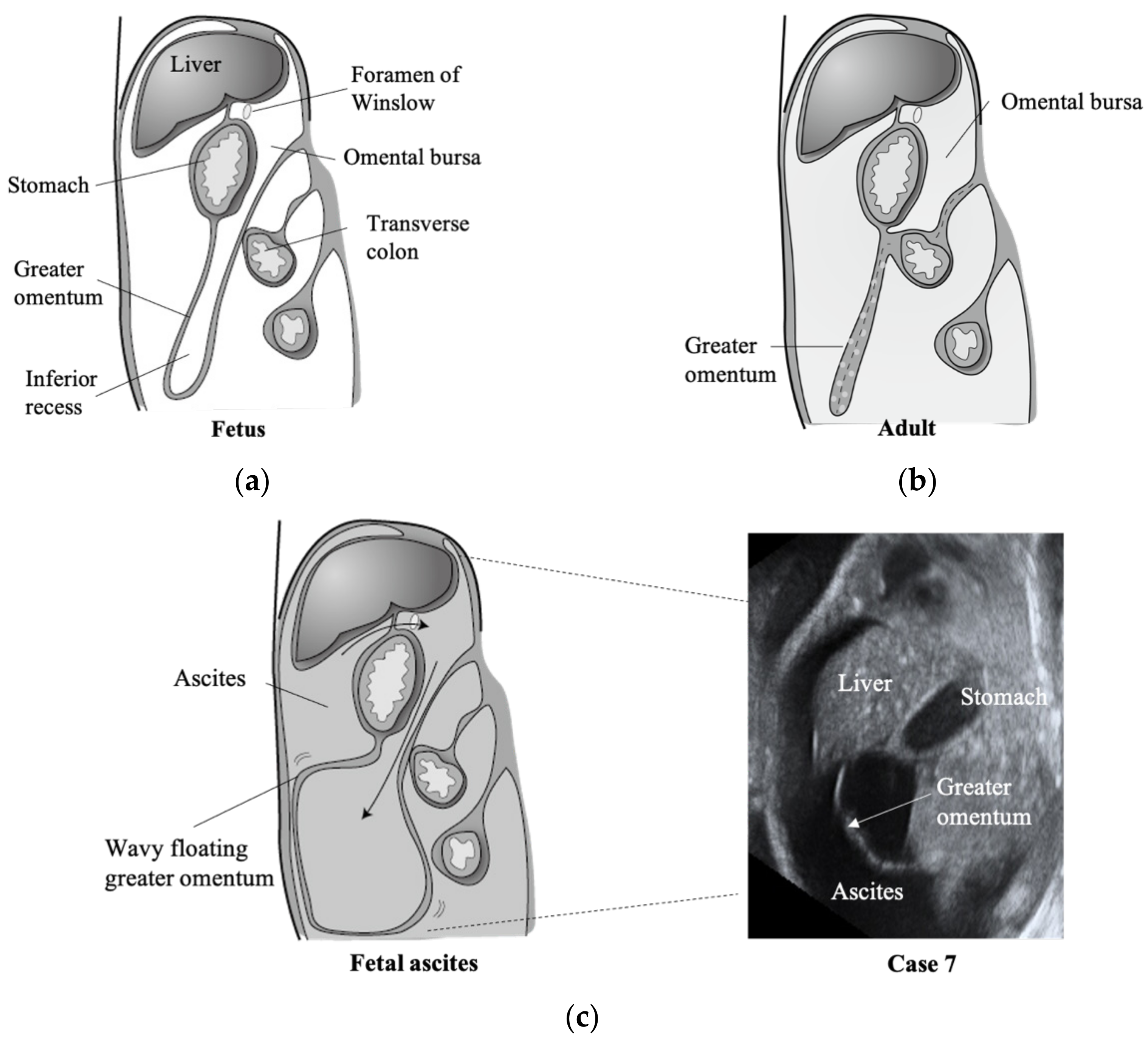
3.2. Fetal Greater Omentum with Ascites
3.3. Fetal Greater Omentum Was Not Observed in Three Cases of Meconium Peritonitis
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Favre, R.; Dreux, S.; Dommergues, M.; Dumez, Y.; Luton, D.; Oury, J.F.; Fiblec, B.L.; Nisand, I.; Muller, F. Nonimmune fetal ascites: A series of 79 cases. Am. J. Obstet. Gynecol. 2004, 190, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Richard, B.; Wolf, D. Abdominal Ascites. In Creasy and Resnik’s Maternal-Fetal Medicine: Principles and Practice, 8th ed.; Resnik, R., Ed.; Elsevier: Philadelphia, MO, USA, 2018; pp. 393–395. [Google Scholar]
- Schmider, A.; Henrich, W.; Reles, A.; Vogel, M.; Dudenhausen, J.W. Isolated fetal ascites caused by primary lymphangiectasia: A case report. Am. J. Obstet. Gynecol. 2001, 184, 227–228. [Google Scholar] [CrossRef] [PubMed]
- Leung, W.C.; Lam, Y.H.; Tang, M.H. Isolated foetal ascites. Hong Kong Med. J. 2001, 7, 432–434. [Google Scholar] [PubMed]
- Piersigilli, F.; Auriti, C.; Marcellini, M.; Marrocco, G.; Soldati, M.; Seganti, G. Isolated fetal ascites due to Budd-Chiari syndrome. Ultrasound Obstet Gynecol. 2008, 31, 222–223. [Google Scholar] [CrossRef] [PubMed]
- Arikan, I.; Barut, A.; Harma, M.; Harma, M.I.; Dogan, S. Isolated Foetal Ascites: A Case Report. J. Med. Cases 2012, 3, 110–112. [Google Scholar] [CrossRef]
- Gross, B.H.; Callen, P.W.; Filly, R.A. Ultrasound appearance of fetal greater omentum. J. Ultrasound Med. 1982, 1, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Platell, C.; Cooper, D.; Papadimitriou, J.M.; Hall, J.C. The omentum. World J. Gastroenterol. 2000, 6, 169–176. [Google Scholar] [CrossRef] [PubMed]
- El Bishry, G. The outcome of isolated fetal ascites. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 137, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Brookes, M.; Zietman, A. Dorsal Mesogastrium. In Clinical Embryology: A Color Atlas and Text; CRC Press: Boca Raton, FL, USA, 1998; pp. 164–167. [Google Scholar]
- Dodds, W.J.; Foley, W.D.; Lawson, T.L.; Stewart, E.T.; Taylor, A. Anatomy and imaging of the lesser peritoneal sac. AJR Am. J. Roentgenol. 1985, 144, 567–575. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shimotsuma, M.; Simpson-Morgan, M.W.; Takahashi, T.; Hagiwara, A. Ontogeny of milky spots in the fetal lamb omentum. Arch. Histol. Cytol. 1994, 57, 291–299. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fukatsu, K.; Saito, H.; Han, I.; Yasuhara, H.; Lin, M.T.; Inoue, T.; Furukawa, S.; Inaba, T.; Hashiguchi, Y.; Matsuda, T.; et al. The greater omentum is the primary site of neutrophil exudation in peritonitis. J. Am. Coll. Surg. 1996, 183, 450–456. [Google Scholar] [PubMed]
- Konturek, S.J.; Brzozowski, T.; Majka, I.; Pawlik, W.; Stachura, J. Omentum and basic fibroblast growth factor in healing of chronic gastric ulcerations in rats. Dig. Dis. Sci. 1994, 39, 1064–1071. [Google Scholar] [CrossRef] [PubMed]
- Jayakumar, S.; Hatsell, L.; Patwardhan, N. Asymptomatic meconium peritonitis presenting as inguinal hernia in a female neonate. J. Neonatal Surg. 2013, 2, 43. [Google Scholar] [CrossRef] [PubMed]

| Case | Gestational Weeks at Diagnosis | Greater Omentum Finding | Associated and Additional Ultrasound Findings | Fetal Hydrops | Outcome (Weeks of Delivery) | Etiology and Associated Disorder of Ascites |
|---|---|---|---|---|---|---|
| 1 | 21w | yes | Omphalocele, Cystic hygroma | yes | IUFD (21w) | Fetal malformations, Non-immune hydrops |
| 2 | 20w | yes | Pleural effusion, Giant placental hematoma | yes | IUFD (23w) | Non-immune hydrops, Chylous ascites |
| 3 | 18w | yes | Laryngeal atresia, PA/VSD, Dilated loops of bowel, Polyhydramnios *Ascites remission (32w) | yes | Stillbirth (35w) | Compression of inferior vena cava by hyperinflated lungs. Meconium peritonitis was not found at autopsy |
| 4 | 18w | yes | CPAM, Polyhydramnios *Ascites remission (30w) | yes | Live birth, NVD (41w) | Compression of inferior vena cava by CPAM |
| 5 | 23w | yes | Umbilical cord cysts | no | Live birth, Emergency C/S due to CAM (28w) | Congenital CMV infection (maternal CMV–IgM-negative), Chylous ascites |
| 6 | 26w | yes | Neck and abdominal cysts, Polyhydramnios *Ascites remission (30w) | no | Live birth, Emergency C/S due to NRFS (37w) | Congenital CMV infection (maternal CMV–IgM-positive) |
| 7 | 28w | yes | Polyhydramnios | no | IUFD (32w) | Idiopathic (chylous ascites) |
| 8 | 18w | yes | Omphalocele, Cleft lip, and palate | no | TOP (19w) | Fetal malformations |
| 9 | 31w | no | Polyhydramnios | no | Live birth, Emergency C/S due to NRFS (32w) | Meconium peritonitis, Small bowel atresia |
| 10 | 39w | no | Dilated loops of bowel | no | Live birth, Emergency C/S due to NRFS (39w) | Meconium peritonitis, Midgut volvulus with intestinal malrotation and atresia |
| 11 | 28w | no | Abdominal calcification, Dilated loops of bowel, Polyhydramnios *Ascites remission (33w) | no | Live birth, NVD (38w) | Meconium peritonitis, Intussusception |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iizuka, T.; Ono, M.; Yamazaki, R.; Kagami, K.; Mitani, Y.; Sakai, S.; Fujiwara, H. Wavy Floating Greater Omentum Findings Are Useful for Differentiating the Etiology of Fetal Ascites. Diagnostics 2021, 11, 326. https://doi.org/10.3390/diagnostics11020326
Iizuka T, Ono M, Yamazaki R, Kagami K, Mitani Y, Sakai S, Fujiwara H. Wavy Floating Greater Omentum Findings Are Useful for Differentiating the Etiology of Fetal Ascites. Diagnostics. 2021; 11(2):326. https://doi.org/10.3390/diagnostics11020326
Chicago/Turabian StyleIizuka, Takashi, Masanori Ono, Rena Yamazaki, Kyosuke Kagami, Yusuke Mitani, Seisho Sakai, and Hiroshi Fujiwara. 2021. "Wavy Floating Greater Omentum Findings Are Useful for Differentiating the Etiology of Fetal Ascites" Diagnostics 11, no. 2: 326. https://doi.org/10.3390/diagnostics11020326
APA StyleIizuka, T., Ono, M., Yamazaki, R., Kagami, K., Mitani, Y., Sakai, S., & Fujiwara, H. (2021). Wavy Floating Greater Omentum Findings Are Useful for Differentiating the Etiology of Fetal Ascites. Diagnostics, 11(2), 326. https://doi.org/10.3390/diagnostics11020326








