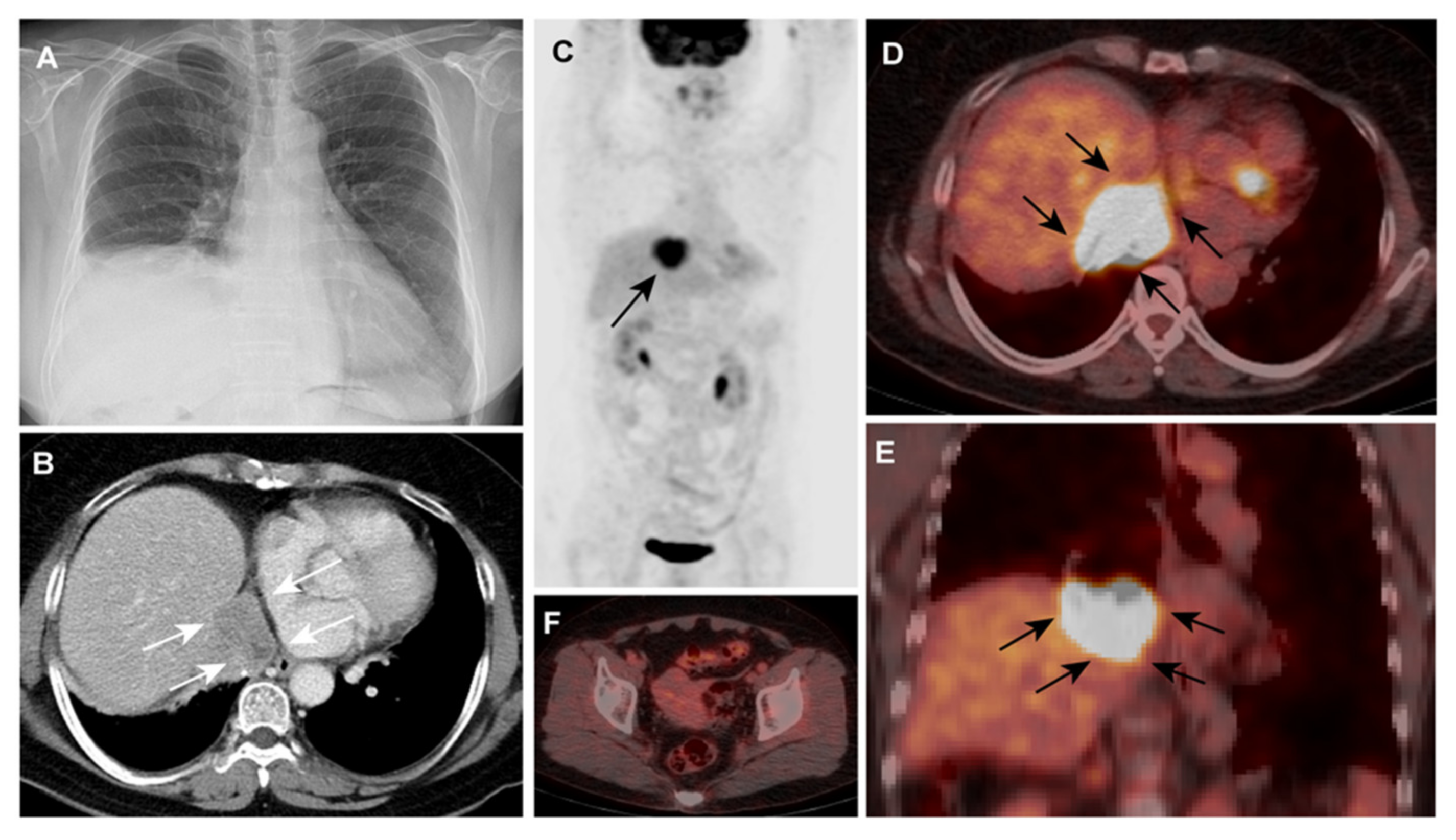
Incidental Detection of Ovarian Cancer as a Solitary Peridiaphragmatic Distant Lymph Node Metastasis without Pelvic Lesions on 18F-FDG PET/CT
Abstract
:Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bast, R.C., Jr.; Klug, T.L.; John, E.S.; Jenison, E.; Niloff, J.M.; Lazarus, H.; Berkowitz, R.S.; Leavitt, T.; Griffiths, C.T.; Parker, L. A radioimmunoassay using a monoclonal antibody to monitor the course of epithelial ovarian cancer. N. Engl. J. Med. 1983, 309, 883–887. [Google Scholar] [CrossRef] [PubMed]
- Xiang, L.; Kong, B. PAX8 is a novel marker for differentiating between various types of tumor, particularly ovarian epithelial carcinomas. Oncol. Lett. 2013, 5, 735–738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, S.; Spencer, J.; Wilkinson, N.; Perren, T. Supradiaphragmatic manifestations of papillary serous adenocarcinoma of the ovary. Clin. Radiol. 1999, 54, 748–754. [Google Scholar] [CrossRef]
- Thomakos, N.; Diakosavvas, M.; Machairiotis, N.; Fasoulakis, Z.; Zarogoulidis, P.; Rodolakis, A. Rare Distant Metastatic Disease of Ovarian and Peritoneal Carcinomatosis: A Review of the Literature. Cancers 2019, 11, 1044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamura, T.; Jeon, J.D. Lymph node metastasis in a gynecologic malignancy. Yonsei Med. J. 2002, 43, 783–791. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.C.; Lee, H.-S.; Jung, D.C.; Choi, J.Y.; Seo, S.-S.; Park, S.-Y. Pathological diagnosis and cytoreduction of cardiophrenic lymph node and pleural metastasis in ovarian cancer patients using video-assisted thoracic surgery. Ann. Surg. Oncol. 2009, 16, 1990–1996. [Google Scholar] [CrossRef] [PubMed]
- Jayson, G.C.; Kohn, E.C.; Kitchener, H.C.; Ledermann, J.A. Ovarian cancer. Lancet 2014, 384, 1376–1388. [Google Scholar] [CrossRef]
- Lengyel, E. Ovarian cancer development and metastasis. Am. J. Pathol. 2010, 177, 1053–1064. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, S.S.; Harris, K.; Pokharel, S.; Yendamuri, S. Calcified Mediastinal Metastasis of Ovarian Cancer Mimicking Broncholithiasis. J. Bronchol. Interv. Pulmonol. 2016, 23, 229–231. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Son, H.J.; Lee, Y.-M.; Lee, J.-H. Incidental Detection of Ovarian Cancer as a Solitary Peridiaphragmatic Distant Lymph Node Metastasis without Pelvic Lesions on 18F-FDG PET/CT. Diagnostics 2021, 11, 422. https://doi.org/10.3390/diagnostics11030422
Son HJ, Lee Y-M, Lee J-H. Incidental Detection of Ovarian Cancer as a Solitary Peridiaphragmatic Distant Lymph Node Metastasis without Pelvic Lesions on 18F-FDG PET/CT. Diagnostics. 2021; 11(3):422. https://doi.org/10.3390/diagnostics11030422
Chicago/Turabian StyleSon, Hye Joo, Yong-Moon Lee, and Jai-Hyuen Lee. 2021. "Incidental Detection of Ovarian Cancer as a Solitary Peridiaphragmatic Distant Lymph Node Metastasis without Pelvic Lesions on 18F-FDG PET/CT" Diagnostics 11, no. 3: 422. https://doi.org/10.3390/diagnostics11030422
APA StyleSon, H. J., Lee, Y. -M., & Lee, J. -H. (2021). Incidental Detection of Ovarian Cancer as a Solitary Peridiaphragmatic Distant Lymph Node Metastasis without Pelvic Lesions on 18F-FDG PET/CT. Diagnostics, 11(3), 422. https://doi.org/10.3390/diagnostics11030422






