Occult Disco-Ligamentous Lesions of the Subaxial c-Spine—A Comparison of Preoperative Imaging Findings and Intraoperative Site Inspection
Abstract
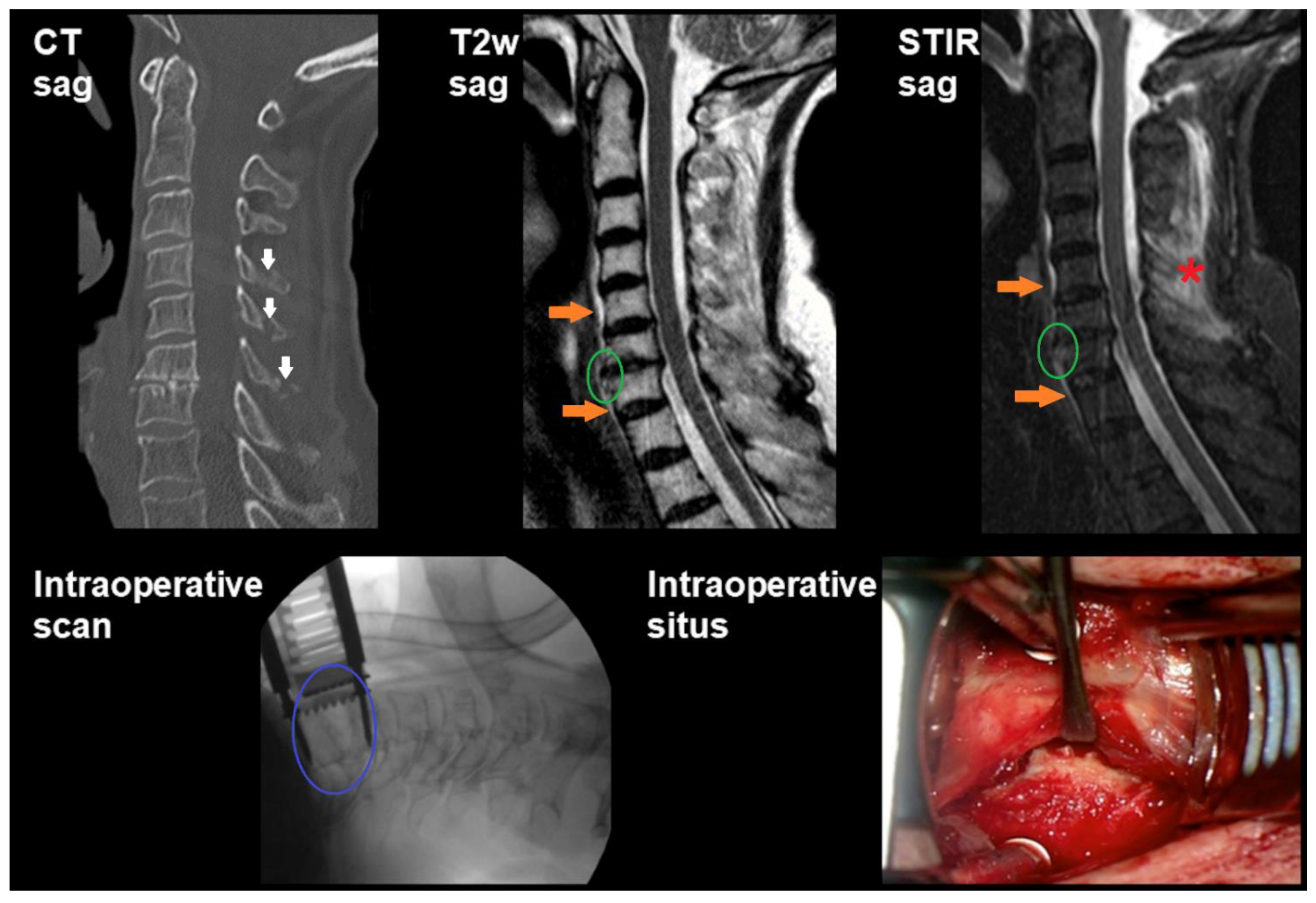
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Inclusion
2.2. Ethical Approval
2.3. Preoperative Imaging
2.3.1. Computed Tomography
2.3.2. Magnetic Resonance Imaging
2.4. Surgery
2.5. Statistical Analyses
3. Results
3.1. Patient Characteristics
3.2. Imaging and Intraoperative Findings
3.3. Sensitivity and Specificity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACDF | Anterior cervical discectomy and fusion |
| ALL | Anterior longitudinal ligament |
| CT | Computed tomography |
| FN | False negative |
| FOV | Field of view |
| FP | False positive |
| MRI | Magnetic resonance imaging |
| PD | Proton density |
| PLL | Posterior longitudinal ligament |
| ROC | Receiver operator characteristics |
| SD | Standard deviation |
| STIR | Short tau inversion recovery |
| TIRM | Turbo inversion recovery magnitude |
| TN | True negative |
| TP | True positive |
References
- Zakrison, T.L.; Williams, B.H. Cervical spine evaluation in the bluntly injured patient. Int. J. Surg. 2016, 33, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Onoue, K.; Farris, C.; Burley, H.; Sung, E.; Clement, M.; Abdalkader, M.; Mian, A. Role of cervical spine MRI in the setting of negative cervical spine CT in blunt trauma: Critical additional information in the setting of clinical findings suggestive of occult injury. J. Neuroradiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Henninger, B.; Kaser, V.; Ostermann, S.; Spicher, A.; Zegg, M.; Schmid, R.; Kremser, C.; Krappinger, D. Cervical Disc and Ligamentous Injury in Hyperextension Trauma: MRI and Intraoperative Correlation. J. Neuroimaging Off. J. Am. Soc. Neuroimaging 2020, 30, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.B.; Dijkers, M.; Devivo, M.J.; Poczatek, R.B. A demographic profile of new traumatic spinal cord injuries: Change and stability over 30 years. Arch. Phys. Med. Rehabil. 2004, 85, 1740–1748. [Google Scholar] [CrossRef]
- Yelamarthy, P.K.K.; Chhabra, H.S.; Vaksha, V.; Agarwal, Y.; Agarwal, A.; Das, K.; Erli, H.J.; Bapat, M.; Singh, R.; Gautam, D.; et al. Radiological protocol in spinal trauma: Literature review and Spinal Cord Society position statement. Eur. Spine J. 2020, 29, 1197–1211. [Google Scholar] [CrossRef]
- Munera, F.; Rivas, L.A.; Nunez, D.B., Jr.; Quencer, R.M. Imaging evaluation of adult spinal injuries: Emphasis on multidetector CT in cervical spine trauma. Radiology 2012, 263, 645–660. [Google Scholar] [CrossRef]
- Holmes, J.F.; Akkinepalli, R. Computed tomography versus plain radiography to screen for cervical spine injury: A meta-analysis. J. Trauma 2005, 58, 902–905. [Google Scholar] [CrossRef] [Green Version]
- Adams, J.M.; Cockburn, M.I.; Difazio, L.T.; Garcia, F.A.; Siegel, B.K.; Bilaniuk, J.W. Spinal clearance in the difficult trauma patient: A role for screening MRI of the spine. Am. Surg. 2006, 72, 101–105. [Google Scholar] [CrossRef]
- Kumar, Y.; Hayashi, D. Role of magnetic resonance imaging in acute spinal trauma: A pictorial review. BMC Musculoskelet Disord. 2016, 17, 310. [Google Scholar] [CrossRef] [Green Version]
- Muchow, R.D.; Resnick, D.K.; Abdel, M.P.; Munoz, A.; Anderson, P.A. Magnetic resonance imaging (MRI) in the clearance of the cervical spine in blunt trauma: A meta-analysis. J. Trauma 2008, 64, 179–189. [Google Scholar] [CrossRef]
- Malham, G.M.; Ackland, H.M.; Varma, D.K.; Williamson, O.D. Traumatic cervical discoligamentous injuries: Correlation of magnetic resonance imaging and operative findings. Spine 2009, 34, 2754–2759. [Google Scholar] [CrossRef] [PubMed]
- Demetriades, D.; Charalambides, K.; Chahwan, S.; Hanpeter, D.; Alo, K.; Velmahos, G.; Murray, J.; Asensio, J. Nonskeletal cervical spine injuries: Epidemiology and diagnostic pitfalls. J. Trauma 2000, 48, 724–727. [Google Scholar] [CrossRef] [PubMed]
- Chiu, W.C.; Haan, J.M.; Cushing, B.M.; Kramer, M.E.; Scalea, T.M. Ligamentous injuries of the cervical spine in unreliable blunt trauma patients: Incidence, evaluation, and outcome. J. Trauma 2001, 50, 457–463. [Google Scholar] [CrossRef]
- O’Dowd, J.K. Basic principles of management for cervical spine trauma. Eur. Spine J. 2010, 19, 18–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feuchtbaum, E.; Buchowski, J.; Zebala, L. Subaxial cervical spine trauma. Curr. Rev. Musculoskelet Med. 2016, 9, 496–504. [Google Scholar] [CrossRef] [Green Version]
- Joaquim, A.F.; Patel, A.A. Subaxial cervical spine trauma: Evaluation and surgical decision-making. Glob. Spine J. 2014, 4, 63–70. [Google Scholar] [CrossRef] [Green Version]
- Goradia, D.; Linnau, K.F.; Cohen, W.A.; Mirza, S.; Hallam, D.K.; Blackmore, C.C. Correlation of MR imaging findings with intraoperative findings after cervical spine trauma. Am. J. Neuroradiol. 2007, 28, 209–215. [Google Scholar] [PubMed]
- Zhuge, W.; Ben-Galim, P.; Hipp, J.A.; Reitman, C.A. Efficacy of MRI for assessment of spinal trauma: Correlation with intraoperative findings. J. Spinal Disord. Tech. 2015, 28, 147–151. [Google Scholar] [CrossRef]
- Saifuddin, A.; Green, R.; White, J. Magnetic resonance imaging of the cervical ligaments in the absence of trauma. Spine 2003, 28, 1686–1691. [Google Scholar] [CrossRef] [PubMed]
- Kawakyu-O’Connor, D.; Bordia, R.; Nicola, R. Magnetic Resonance Imaging of Spinal Emergencies. Magn. Reason. Imaging Clin. N. Am. 2016, 24, 325–344. [Google Scholar] [CrossRef]
- Patel, A.; James, S.L.; Davies, A.M.; Botchu, R. Spinal imaging update: An introduction to techniques for advanced MRI. Bone Jt. J. 2015, 97, 1683–1692. [Google Scholar] [CrossRef] [PubMed]
- Ma, J. Dixon techniques for water and fat imaging. J. Int. Soc. Magn. Reson. Med. 2008, 28, 543–558. [Google Scholar] [CrossRef]
- Dixon, W.T. Simple proton spectroscopic imaging. Radiology 1984, 153, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Glover, G.H.; Schneider, E. Three-point Dixon technique for true water/fat decomposition with B0 inhomogeneity correction. Magn. Reson. Med. 1991, 18, 371–383. [Google Scholar] [CrossRef]
- Guerini, H.; Omoumi, P.; Guichoux, F.; Vuillemin, V.; Morvan, G.; Zins, M.; Thevenin, F.; Drape, J.L. Fat Suppression with Dixon Techniques in Musculoskeletal Magnetic Resonance Imaging: A Pictorial Review. Semin. Musculoskelet Radiol. 2015, 19, 335–347. [Google Scholar] [CrossRef]
- Brandao, S.; Seixas, D.; Ayres-Basto, M.; Castro, S.; Neto, J.; Martins, C.; Ferreira, J.C.; Parada, F. Comparing T1-weighted and T2-weighted three-point Dixon technique with conventional T1-weighted fat-saturation and short-tau inversion recovery (STIR) techniques for the study of the lumbar spine in a short-bore MRI machine. Clin. Radiol. 2013, 68, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Zhadanov, S.I.; Doshi, A.H.; Pawha, P.S.; Corcuera-Solano, I.; Tanenbaum, L.N. Contrast-Enhanced Dixon Fat-Water Separation Imaging of the Spine: Added Value of Fat, In-Phase and Opposed-Phase Imaging in Marrow Lesion Detection. J. Comput. Assist. Tomogr. 2016, 40, 985–990. [Google Scholar] [CrossRef] [PubMed]
- Del Grande, F.; Santini, F.; Herzka, D.A.; Aro, M.R.; Dean, C.W.; Gold, G.E.; Carrino, J.A. Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics 2014, 34, 217–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delfaut, E.M.; Beltran, J.; Johnson, G.; Rousseau, J.; Marchandise, X.; Cotten, A. Fat suppression in MR imaging: Techniques and pitfalls. Radiographics 1999, 19, 373–382. [Google Scholar] [CrossRef]
- Lee, S.; Choi, D.S.; Shin, H.S.; Baek, H.J.; Choi, H.C.; Park, S.E. FSE T2-weighted two-point Dixon technique for fat suppression in the lumbar spine: Comparison with SPAIR technique. Diagn. Interv. Radiol. 2018, 24, 175–180. [Google Scholar] [CrossRef] [Green Version]
- Huijgen, W.H.F.; van Rijswijk, C.S.P.; Bloem, J.L. Is fat suppression in T1 and T2 FSE with mDixon superior to the frequency selection-based SPAIR technique in musculoskeletal tumor imaging? Skelet. Radiol. 2019, 48, 1905–1914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wendl, C.M.; Eiglsperger, J.; Dendl, L.M.; Brodoefel, H.; Schebesch, K.M.; Stroszczynski, C.; Fellner, C. Fat suppression in magnetic resonance imaging of the head and neck region: Is the two-point DIXON technique superior to spectral fat suppression? Br. J. Radiol. 2018, 91, 20170078. [Google Scholar] [CrossRef] [PubMed]
- Sollmann, N.; Monch, S.; Riederer, I.; Zimmer, C.; Baum, T.; Kirschke, J.S. Imaging of the degenerative spine using a sagittal T2-weighted DIXON turbo spin-echo sequence. Eur. J. Radiol. 2020, 131, 109204. [Google Scholar] [CrossRef] [PubMed]
- Padayachee, L.; Cooper, D.J.; Irons, S.; Ackland, H.M.; Thomson, K.; Rosenfeld, J.; Kossmann, T. Cervical spine clearance in unconscious traumatic brain injury patients: Dynamic flexion-extension fluoroscopy versus computed tomography with three-dimensional reconstruction. J. Trauma 2006, 60, 341–345. [Google Scholar] [CrossRef]
- McCracken, B.; Klineberg, E.; Pickard, B.; Wisner, D.H. Flexion and extension radiographic evaluation for the clearance of potential cervical spine injures in trauma patients. Eur. Spine J. 2013, 22, 1467–1473. [Google Scholar] [CrossRef] [Green Version]


| Sequence | Number of Patients | ||
|---|---|---|---|
| Non-contrast T1-weighted | Sagittal | 63 | 53 |
| Axial | 3 | ||
| Sagittal & axial | 7 | ||
| T2-weighted | Sagittal | 83 | 3 |
| Axial | 10 | ||
| Sagittal & axial | 56 | ||
| Axial & coronal | 2 | ||
| Sagittal & axial & coronal | 12 | ||
| STIR | Sagittal | 73 | 63 |
| Sagittal & axial | 2 | ||
| Sagittal & coronal | 7 | ||
| Sagittal & axial & coronal | 1 | ||
| PD-weighted | Sagittal | 29 | 3 |
| Coronal | 17 | ||
| Sagittal & coronal | 9 | ||
| Contrast-enhanced T1-weighted | Sagittal | 3 | 2 |
| Sagittal & axial | 1 | ||
| TIRM | Sagittal | 2 | |
| DIXON | Sagittal & coronal | 1 | |
| Item | Value | |
|---|---|---|
| Number of patients | 83 | |
| Age (mean ± SD & range; in years) | 59.4 ± 20.5 (12–94) | |
| Sex (% males/females) | 63.9/36.1 | |
| Trauma mechanism/entity (% of patients) | Traffic accident | 16.9 |
| Polytrauma | 2.4 | |
| Fall | 48.2 | |
| Fall (great height) | 32.5 | |
| Symptoms (% of patients) | None | 0.0 |
| Nuchalgia | 41.0 | |
| Brachialgia | 0.0 | |
| Myelopathy | 3.6 | |
| Monoparesis | 6.0 | |
| Isolated sensory disturbance | 4.8 | |
| Central cord syndrome | 20.5 | |
| Tetraparesis | 8.4 | |
| Nuchalgia & brachialgia | 2.4 | |
| Nuchalgia & monoparesis | 1.2 | |
| Nuchalgia & sensory disturbance | 1.2 | |
| Brachialgia & monoparesis | 1.2 | |
| Nuchalgia & brachialgia & myelopathy | 1.2 | |
| Myelopathy & monoparesis & sensory disturbance | 1.2 | |
| Intubated/not assessible | 7.3 | |
| Surgical procedure (% of patients) | Anterior cervical discectomy and fusion (ACDF) + ventral plate | 75.9 |
| Anterior cervical discectomy or corpectomy and fusion + ventral plate & dorsal stabilization | 19.3 | |
| Anterior cervical corpectomy and fusion + ventral plate | 4.8 | |
| # | Affected Segment(s) | Preoperative Imaging | Intraoperative Situs Inspection | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Disco-Ligamentous Injury | Other Trauma-Related Findings Affecting the Cervical Spine | Other Findings at the Cervical Spine | Acquired Sequences | Disco-Ligamentous Injury | ||||||||
| ALL | Intervertebral Disc | PLL | Interspinous Ligaments | ALL | Intervertebral Disc | PLL | Interspinous Ligaments | |||||
| 1 | C4/5 | - | - | - | - | - | Scoliosis, severe multi-segmental spondylosis, myelomalacia, spinal stenosis | T1w sag/ax, T2w sag/ax, STIR sag | X | X | - | - |
| 2 | C3/4 | - | - | - | - | Prevertebral hematoma | Forestier’s disease, severe multi-segmental spondylosis, myelomalacia, spinal stenosis | T2w sag/ax, STIR sag | X | X | - | - |
| 3 | C5/6 | - | - | - | X | Vertebral fracture | - | T1w ax, T2w sag/ax, STIR sag/cor | - | X | - | - |
| 4 | C5/6 | - | - | - | X | Prevertebral hematoma | - | T1w sag, T2w ax, STIR sag/ax/cor, T1w sagittal (CE) | X | X | - | - |
| 5 | C6/7 | - | - | - | - | Vertebral fracture | - | T1w sag, T2w sag/ax, STIR sag, PDW cor | X | X | - | - |
| 6 | C5/6, C6/7 | - | - | - | - | Vertebral fracture | Severe multi-segmental spondylosis | T1w sag, T2w ax/cor, STIR sag | X | X | - | - |
| 7 | C5/6, C6/7 | - | - | - | X | Prevertebral hematoma, vertebral fracture | Severe multi-segmental spondylosis, myelomalacia, spinal stenosis | T1w sag, T2w sag/ax/cor, STIR sag | - | X | - | X |
| 8 | C2/3 | - | - | - | - | Vertebral fracture | Spinal stenosis | T2w ax, STIR sag | X | X | - | - |
| 9 | C6/7 | - | - | - | X | - | Scoliosis, severe multi-segmental spondylosis, myelomalacia, spinal stenosis | T1w sag, T2w sag/ax/cor, STIR sag | X | X | - | - |
| 10 | C4/5, C5/6 | - | - | - | - | Prevertebral hematoma | Forestier’s disease, severe multi-segmental spondylosis, myelomalacia, spinal stenosis | T1w sag, T2w sag/ax, STIR sag | - | X | - | - |
| 11 | C6/7 | - | - | - | - | Vertebral fracture | - | T1w sag, T2w sag/ax, STIR sag | X | X | - | - |
| 12 | C6/7, C7/T1 | - | - | - | - | Vertebral fracture | - | T1w sag, T2w sag/ax, STIR sag | X | X | - | - |
| 13 | C6/7 | - | - | - | X | - | Myelomalacia, spinal stenosis | T1w ax, T2w sag/ax, STIR sag | - | X | - | - |
| 14 | C5/6, C6/7 | - | - | - | X | Vertebral fracture | Scoliosis, severe multi-segmental spondylosis | T1w sag, T2w sag/ax, STIR sag | X | X | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Janssen, I.; Sollmann, N.; Barz, M.; Baum, T.; Schaller, K.; Zimmer, C.; Ryang, Y.-M.; Kirschke, J.S.; Meyer, B. Occult Disco-Ligamentous Lesions of the Subaxial c-Spine—A Comparison of Preoperative Imaging Findings and Intraoperative Site Inspection. Diagnostics 2021, 11, 447. https://doi.org/10.3390/diagnostics11030447
Janssen I, Sollmann N, Barz M, Baum T, Schaller K, Zimmer C, Ryang Y-M, Kirschke JS, Meyer B. Occult Disco-Ligamentous Lesions of the Subaxial c-Spine—A Comparison of Preoperative Imaging Findings and Intraoperative Site Inspection. Diagnostics. 2021; 11(3):447. https://doi.org/10.3390/diagnostics11030447
Chicago/Turabian StyleJanssen, Insa, Nico Sollmann, Melanie Barz, Thomas Baum, Karl Schaller, Claus Zimmer, Yu-Mi Ryang, Jan S. Kirschke, and Bernhard Meyer. 2021. "Occult Disco-Ligamentous Lesions of the Subaxial c-Spine—A Comparison of Preoperative Imaging Findings and Intraoperative Site Inspection" Diagnostics 11, no. 3: 447. https://doi.org/10.3390/diagnostics11030447
APA StyleJanssen, I., Sollmann, N., Barz, M., Baum, T., Schaller, K., Zimmer, C., Ryang, Y.-M., Kirschke, J. S., & Meyer, B. (2021). Occult Disco-Ligamentous Lesions of the Subaxial c-Spine—A Comparison of Preoperative Imaging Findings and Intraoperative Site Inspection. Diagnostics, 11(3), 447. https://doi.org/10.3390/diagnostics11030447









