Pancreatic Ductal Adenocarcinoma: Epidemiology and Risk Factors
Abstract
1. Introduction
2. Epidemiology
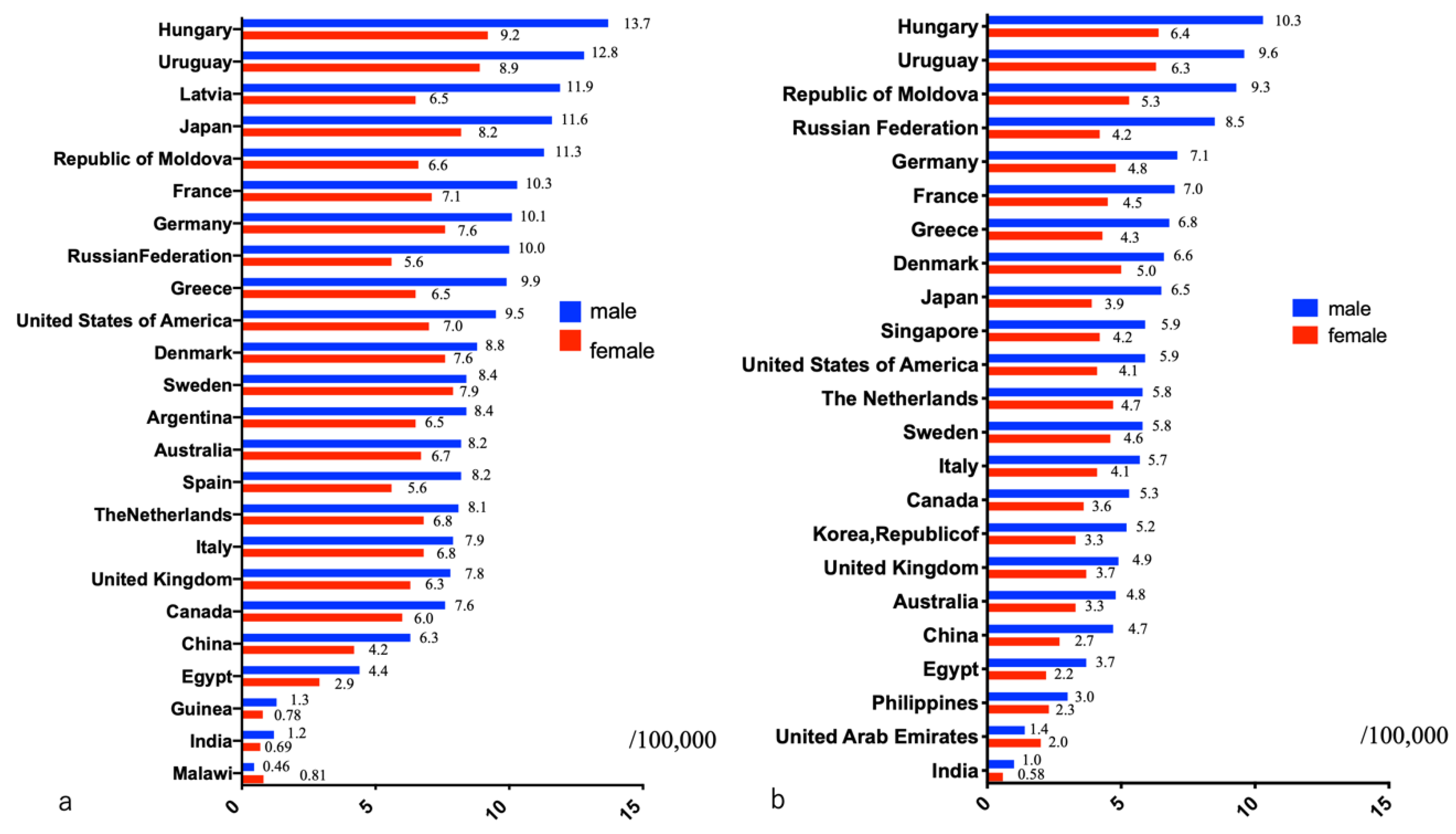
2.1. Status in the World
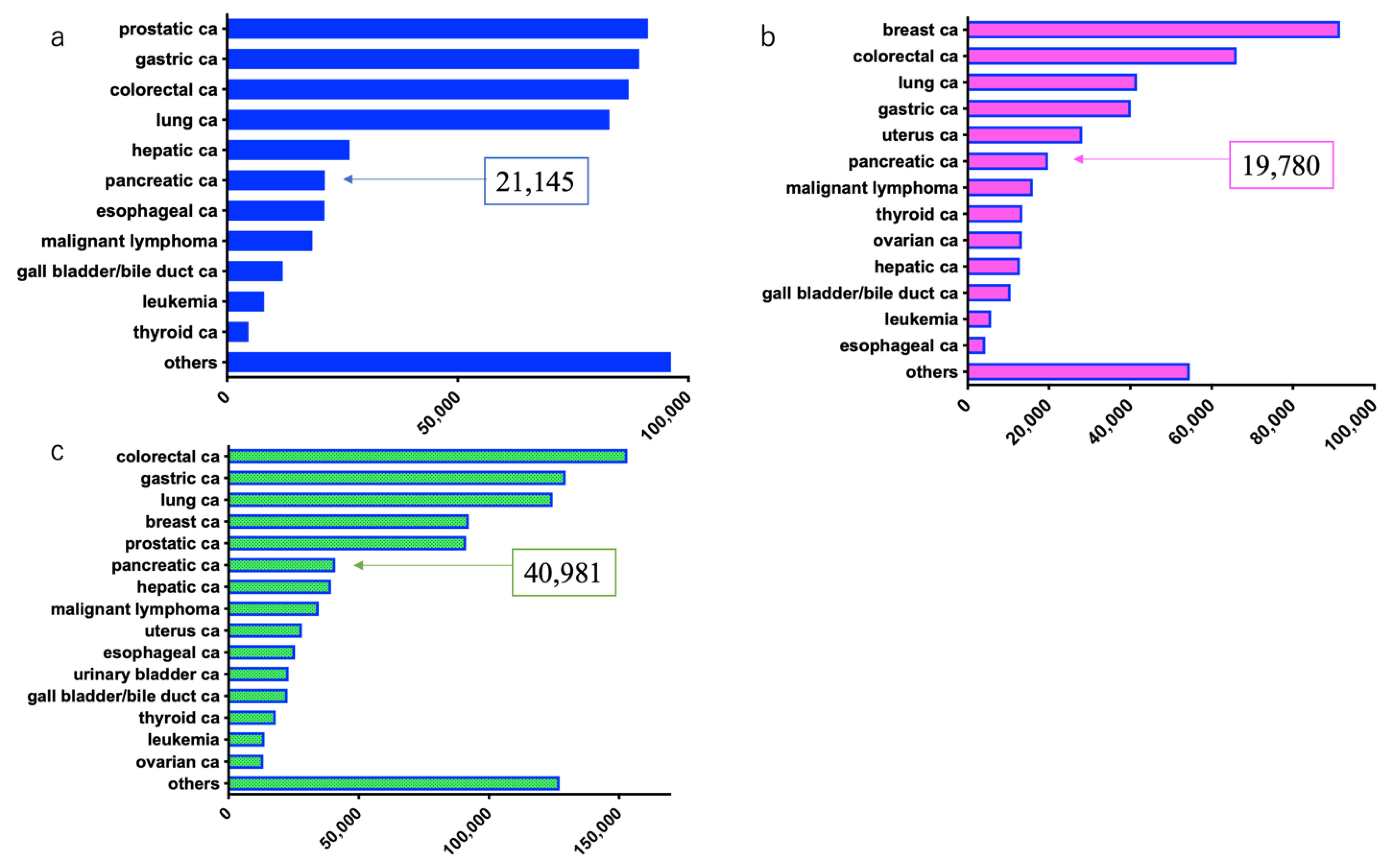
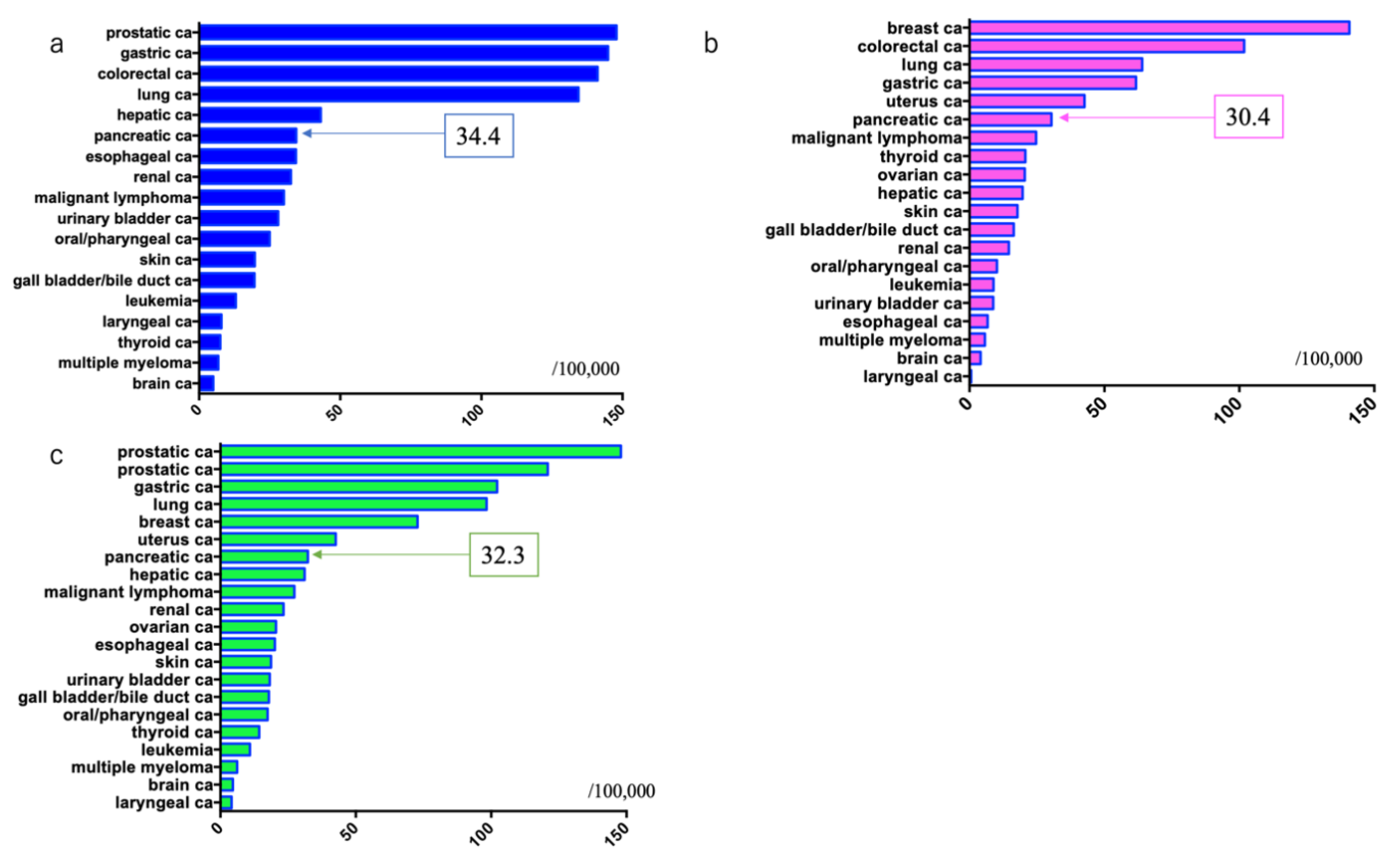
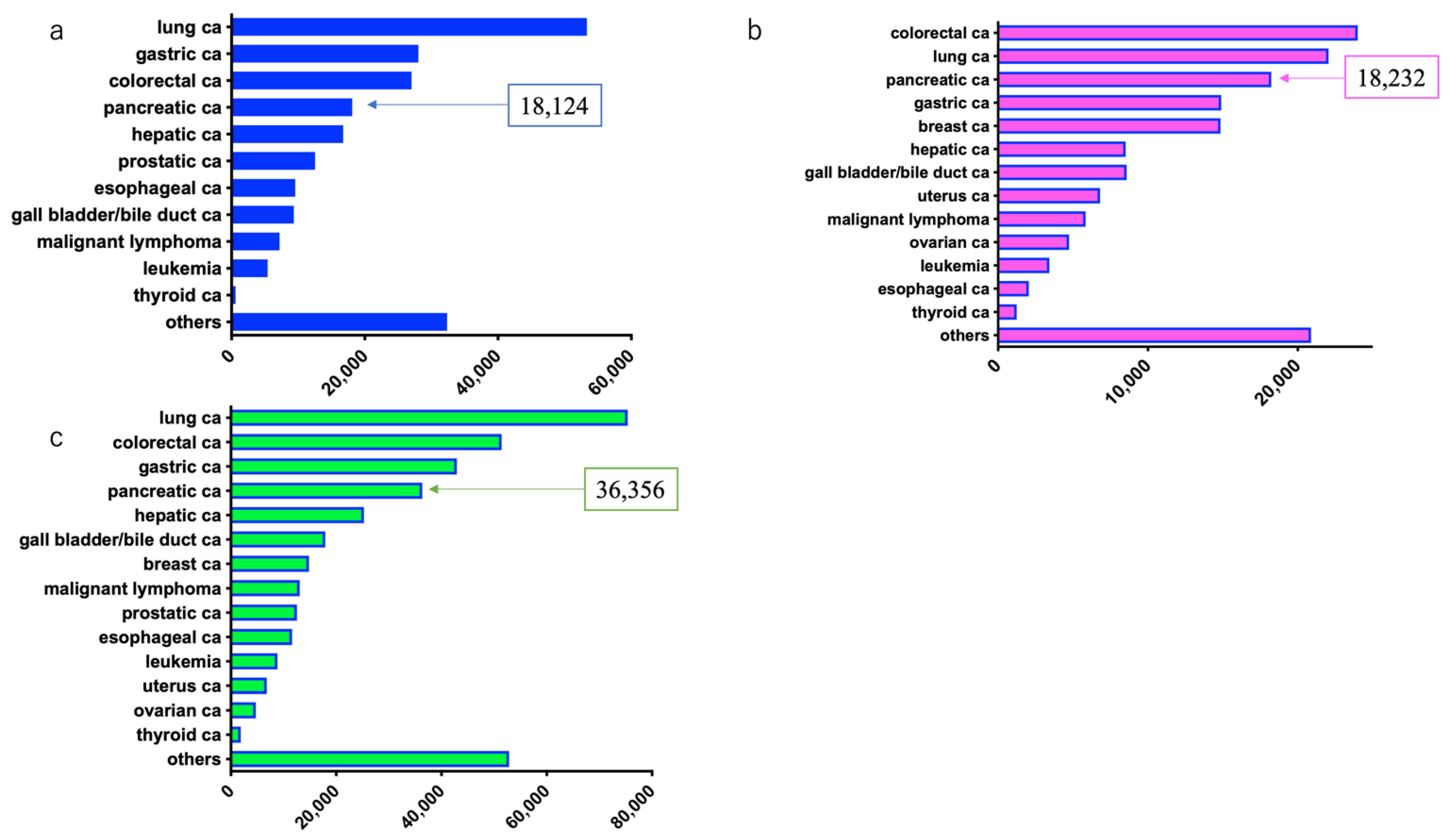
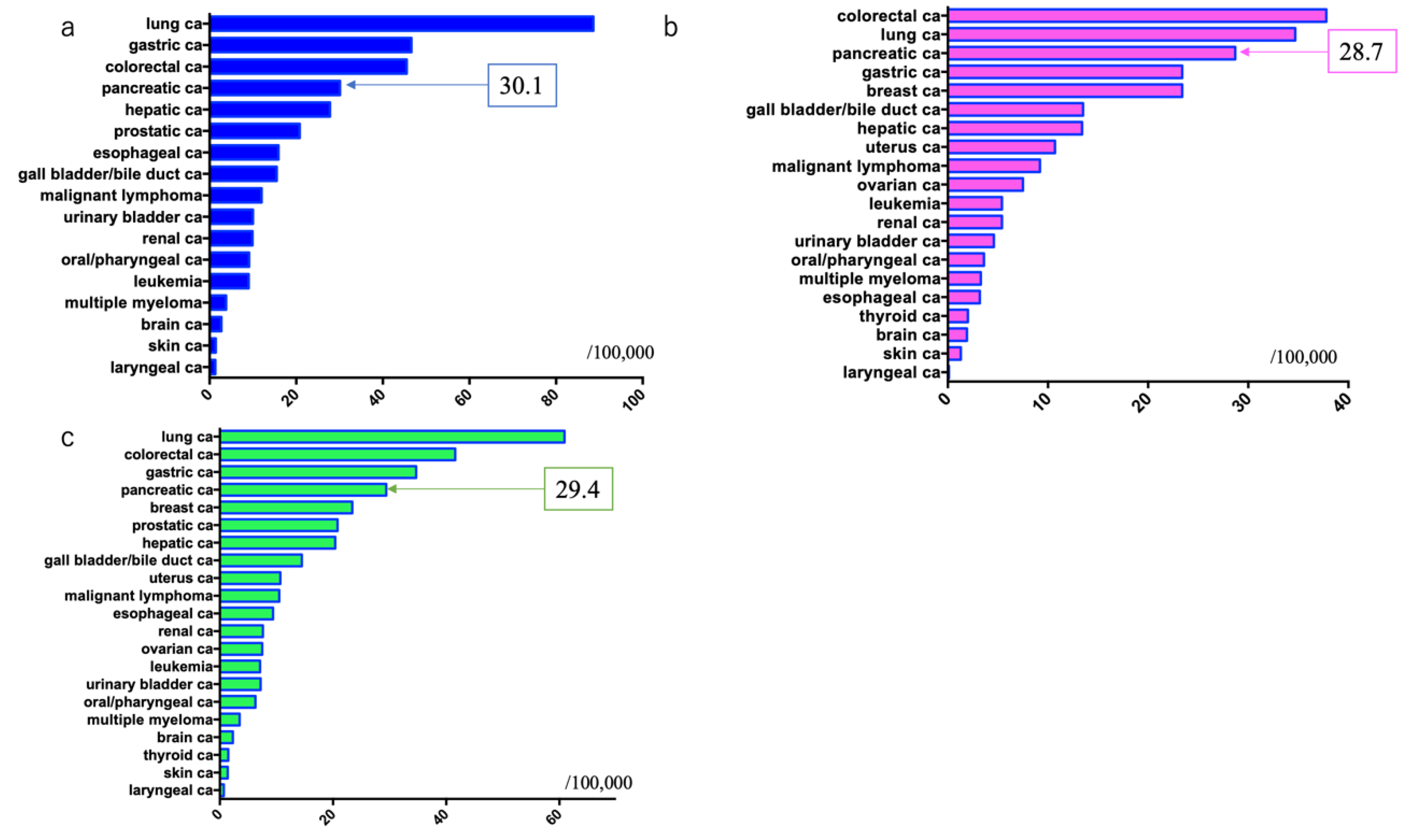
2.2. Current Status in Japan
2.2.1. Number and Incidence of Pancreatic Ductal Adenocarcinoma Cases
2.2.2. Number of Deaths and Mortality Rate of Patients with Pancreatic Ductal Adenocarcinoma
3. Risk Factors
3.1. Family History
3.2. Genetic Disorders
3.3. Diabetes Mellitus
3.4. Intraductal Papillary Mucinous Neoplasms (IPMNs)
3.5. Chronic Pancreatitis
3.6. Obesity
3.7. Smoking
3.8. Alcohol Consumption
3.9. Other
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. CA Global cancer statistics 2020, GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J. Clin. 2021. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. Data Visualization Tools for Exploring the Global Cancer Burden in 2020. Available online: https://gco.iarc.fr/today (accessed on 17 February 2020).
- Wong, M.C.S.; Jiang, J.Y.; Liang, M.; Fang, Y.; Yeung, M.S.; Sung, J.J.Y. Global temporal patterns of pancreatic cancer and association with socioeconomic development. Sci Rep. 2017, 7, 3165. [Google Scholar] [CrossRef] [PubMed]
- Saad, A.M.; Turk, T.; Al-Husseini, M.J.; Abdel-Rahman, O. Trends in pancreatic adenocarcinoma incidence and mortality in the United States in the last four decades; A SEER-based study. BMC Cancer 2018, 18, 688. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics 2017. CA Cancer J. Clin. 2017, 67, 7–30. [Google Scholar] [CrossRef]
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030, the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef]
- Cancer Registry and Statistics. Cancer Information Service, National Cancer Center, Japan (Ministry of Health, Labour and Welfare, National Cancer Registry). Available online: https://ganjoho.jp/reg_stat/statistics/stat/summary.html (accessed on 11 February 2021).
- Available online: http://www.zengankyo.ncc.go.jp/etc/seizonritsu/seizonritsu2012.html (accessed on 11 February 2021).
- Kanno, A.; Masamune, A.; Hanada, K.; Maguchi, H.; Shimizu, Y.; Ueki, T.; Hasebe, O.; Ohtsuka, T.; Nakamura, M.; Takenaka, M.; et al. Japan study group on the early detection of pancreatic cancer (JEDPAC). Multicenter study of early pancreatic cancer in Japan. Pancreatology 2018, 18, 61–67. [Google Scholar] [CrossRef]
- Egawa, S.; Toma, H.; Ohigashi, H.; Okusaka, T.; Nakao, A.; Hatori, T.; Maguchi, H.; Yanagisawa, A.; Tanaka, M. Japan pancreatic cancer registry; 30th year anniversary: Japan Pancreas Society. Pancreas 2012, 41, 985–992. [Google Scholar] [CrossRef]
- Kanno, A.; Masamune, A.; Hanada, K.; Kikuyama, M.; Kitano, M. Advances in early detection of pancreatic cancer. Diagnostics 2019, 9, 18. [Google Scholar] [CrossRef]
- Hanada, K.; Amano, H.; Abe, T. Early diagnosis of pancreatic cancer: Current trends and concerns. Ann. Gastroenterol. Surg. 2017, 1, 44–51. [Google Scholar] [CrossRef]
- Hanada, K.; Okazaki, A.; Hirano, N.; Izumi, Y.; Minami, T.; Ikemoto, J.; Kanemitsu, K.; Hino, F. Effective screening for early diagnosis of pancreatic cancer. Best Pract. Res. Clin. Gastroenterol. 2015, 29, 929–939. [Google Scholar] [CrossRef]
- Matsubayashi, H.; Maeda, A.; Kanemoto, H.; Uesaka, K.; Yamazaki, K.; Hironaka, S.; Miyagi, Y.; Ikehara, H.; Ono, H.; Klein, A.; et al. Risk factors of familial pancreatic cancer in Japan: Current smoking and recent onset of diabetes. Pancreas 2011, 40, 974–978. [Google Scholar] [CrossRef]
- Inoue, M.; Tajima, K.; Takezaki, T.; Hamajima, N.; Hirose, K.; Ito, H.; Tominaga, S. Epidemiology of pancreatic cancer in Japan: A nested case-control study from the Hospital-based Epidemiologic Research Program at Aichi Cancer Center (HERPACC). Int. J. Epidemiol. 2003, 32, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Brune, K.A.; Lau, B.; Palmisano, E.; Canto, M.; Goggins, M.G.; Hruban, R.H.; Klein, A.P. Importance of age of onset in pancreatic cancer kindreds. J. Natl. Cancer Inst. 2010, 102, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Couch, F.J.; Johnson, M.R.; Rabe, K.G.; Brune, K.; de Andrade, M.; Goggins, M.; Rothenmund, H.; Gallinger, S.; Klein, A.; Petersen, G.M.; et al. The prevalence of BRCA2 mutations in familial pancreatic cancer. Cancer Epidemiol. Biomark. Prev. 2007, 16, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.; Hruban, R.H.; Kamiyama, M.; Borges, M.; Zhang, X.; Parsons, D.W.; Lin, J.C.; Palmisano, E.; Brune, K.; Jaffee, E.M.; et al. Exomic sequencing identifies PALB2 as a pancreatic cancer susceptibility gene. Science 2009, 324, 217. [Google Scholar] [CrossRef] [PubMed]
- Slater, E.P.; Langer, P.; Niemczyk, E.; Strauch, K.; Butler, J.; Habbe, N.; Neoptolemos, J.P.; Greenhalf, W.; Bartsch, D.K. PALB2 mutations in European familial pancreatic cancer families. Clin. Genet. 2010, 78, 490–494. [Google Scholar] [CrossRef] [PubMed]
- Giardiello, F.M.; Brensinger, J.D.; Tersmette, A.C.; Goodman, S.N.; Petersen, G.M.; Booker, S.V.; Cruz-Corre, M.; Offerhaus, J.A. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology 2000, 119, 1447–1453. [Google Scholar] [CrossRef]
- Goldstein, A.M.; Fraser, M.C.; Struewing, J.P.; Hussussian, C.J.; Ranade, K.; Zametkin, D.P.; Fontaine, L.S.; Organic, S.M.; Dracopoli, N.C.; Clark Jr, W.H.; et al. Increased risk of pancreatic cancer in melanoma-prone kindreds with p16INK4mutations. N. Engl. J. Med. 1995, 333, 970–974. [Google Scholar] [CrossRef]
- Giardiello, F.M.; Offerhaus, G.J.; Lee, D.H.; Krush, A.J.; Tersmette, A.C.; Booker, S.V.; Kelley, N.C.; Hamilton, S.R. Increased risk of thyroid and pancreatic carcinoma in familial adenomatous polyposis. Gut 1993, 34, 1394–1396. [Google Scholar] [CrossRef]
- Kastrinos, F.; Mukherjee, B.; Tayob, N.; Wang, F.; Sparr, J.; Raymond, V.M.; Bandipalliam, P.; Stoffel, E.M.; Gruber, S.B.; Syngal, S. Risk of pancreatic cancer in families with Lynch syndrome. JAMA 2009, 302, 1790–1795. [Google Scholar] [CrossRef]
- Shi, C.; Hruban, R.H.; Klein, A.P. Familial pancreatic cancer. Arch. Pathol. Lab. Med. 2009, 133, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Matsubayashi, H.; Takaori, K.; Morizane, C.; Maguchi, H.; Mizuma, M.; Takahashi, H.; Wada, K.; Hosoi, H.; Yachida, S.; Suzuki, M.; et al. Familial pancreatic cancer: Concept, management and issues. World J. Gastroenterol. 2017, 23, 935–948. [Google Scholar] [CrossRef] [PubMed]
- Rebours, V.; Boutron-Ruault, M.C.; Schnee, M.; Férec, C.; Maire, F.; Hammel, P.; Ruszniewski, P.; Lévy, P. Risk of pancreatic adenocarcinoma in patients with hereditary pancreatitis: A national exhaustive series. Am. J. Gastroenterol. 2008, 103, 111–119. [Google Scholar] [CrossRef]
- Friedenson, B. BRCA1 and BRCA2 pathways and the risk of cancers other than breast or ovarian. Med. Gen. Med. 2005, 7, 60. [Google Scholar]
- Yamauchi, H.; Takei, J. Management of hereditary breast and ovarian cancer. Int. J. Clin. Oncol. 2018, 23, 45–51. [Google Scholar] [CrossRef]
- Iqbal, J.; Ragone, A.; Lubinski, J.; Lynch, H.T.; Moller, P.; Ghadirian, P.; Foulkes, W.D.; Armel, S.; Eisen, A.; Neuhausen, S.L.; et al. The incidence of pancreatic cancer in BRCA1 and BRCA2 mutation carriers. Br. J. Cancer 2012, 107, 2005–2009. [Google Scholar] [CrossRef]
- Golan, T.; Kanji, Z.S.; Epelbaum, R.; Devaud, N.; Dagan, E.; Holter, S.; Aderka, D.; Paluch-Shimon, S.; Kaufman, B.; Hedley, D.; et al. Overall survival and clinical characteristics of pancreatic cancer in BRCA mutation carriers. Br. J. Cancer 2014, 111, 1132–1138. [Google Scholar] [CrossRef]
- Leung, K.; Saif, M.W. BRCA-associated pancreatic cancer: The evolving management. JOP J. Pancreas 2013, 14, 149–151. [Google Scholar]
- Murphy, K.M.; Brune, K.A.; Griffin, C.; Sollenberger, J.E.; Petersen, G.M.; Bansal, R.; Hruban, R.H. Evaluation of candidate genes MAP2K4, MADH4, ACVR1B, and BRCA2 in familial pancreatic cancer: Deleterious BRCA2 mutations in 17%. Cancer Res. 2002, 62, 3789–3793. [Google Scholar] [PubMed]
- Hahn, S.A.; Greenhalf, B.; Ellis, I.; Sina-Frey, M.; Rieder, H.; Korte, B.; Gerdes, B.; Kress, R.; Ziegler, A.; Raeburn, J.A.; et al. BRCA2 germline mutations in familial pancreatic carcinoma. J. Natl. Cancer Inst. 2003, 95, 214–221. [Google Scholar] [CrossRef]
- Leoz, M.L.; Sanchez, A.; Carballal, S.; Ruano, L.; Ocana, T.; Pellise, M.; Castells, A.; Balaguer, F.; Moreira, L. Hereditary gastric and pancreatic cancer predisposition syndromes. Gastroenterol. Hepatol. 2016, 39, 481–793. [Google Scholar] [CrossRef]
- Watson, P.; Vasen, H.F.; Mecklin, J.P.; Bernstein, I.; Aarnio, M.; Jarvinen, H.J.; Myrhoj, T.; Sunde, L.; Wijnen, J.T.; Lynch, H.T. The risk of extra-colonic, extra-endometrial cancer in the Lynch syndrome. Int. J. Cancer 2008, 123, 444–449. [Google Scholar] [CrossRef]
- Becker, A.E.; Hernandez, Y.G.; Frucht, H.; Lucas, A.L. Pancreatic ductal adenocarcinoma: Risk factors, screening, and early detection. World J. Gastroenterol. 2014, 20, 11182–11198. [Google Scholar] [CrossRef] [PubMed]
- Syngal, S.; Brand, R.E.; Church, J.M.; Giardiello, F.M.; Hampel, H.L.; Burt, R.W.; American College of Gastroenterology. ACG clinical guideline: Genetic testing and management of hereditary gastrointestinal cancer syndromes. Am. J. Gastroenterol. 2015, 110, 223–262. [Google Scholar] [CrossRef]
- Greer, J.B.; Lynch, H.T.; Brand, R.E. Hereditary pancreatic cancer: A clinical perspective. Best Pract. Res. Clin. Gastroenterol. 2009, 23, 159–170. [Google Scholar] [CrossRef]
- Ben, Q.; Xu, M.; Ning, X.; Liu, J.; Hong, S.; Huang, W.; Zhang, H.; Li, Z. Diabetes mellitus and risk of pancreatic cancer: A meta-analysis of cohort studies. Eur. J. Cancer 2011, 47, 1928–1937. [Google Scholar] [CrossRef]
- Singh, S.; Singh, P.P.; Singh, A.G.; Murad, M.H.; Sanchez, W. Anti-diabetic medications and the risk of hepatocellular cancer: A systematic review and meta-analysis. Am. J. Gastroenterol. 2013, 108, 881–891. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Kanemitsu, S.; Hatori, T.; Maguchi, H.; Shimizu, Y.; Tada, M.; Nakagohri, T.; Hanada, K.; Osanai, M.; Noda, Y.; et al. Pancreatic ductal adenocarcinoma derived from IPMN and pancreatic ductal adenocarcinoma concomitant with IPMN. Pancreas 2011, 40, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Uehara, H.; Nakaizumi, A.; Ishikawa, O.; Iishi, H.; Tatsumi, K.; Takakura, R.; Ishida, T.; Takano, Y.; Tanaka, S.; Takenaka, A. Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut 2008, 57, 1561–1565. [Google Scholar] [CrossRef]
- Tanno, S.; Nakano, Y.; Koizumi, K.; Sugiyama, Y.; Nakamura, K.; Sasajima, J.; Nishikawa, T.; Mizukami, Y.; Yanagawa, N.; Fujii, T.; et al. Pancreatic ductal adenocarcinomas in long-term follow-up patients with branch duct intraductal papillary mucinous neoplasms. Pancreas 2010, 39, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Pergolini, I.; Sahora, K.; Ferrone, C.R.; Morales-Oyarvide, V.; Wolpin, B.M.; Mucci, L.A.; Brugge, W.R.; Mino-Kenudson, M.; Patino, M.; Sahani, D.V.; et al. Long-term risk of pancreatic malignancy in patients with branch duct intraductal papillary mucinous neoplasm in a referral center. Gastroenterology 2017, 153, 1284–1294. [Google Scholar] [CrossRef]
- Raimondi, S.; Lowenfels, A.B.; Morselli-Labate, A.M.; Maisonneuve, P.; Pezzilli, R. Pancreatic cancer in chronic pancreatitis; Aetiology, incidence, and early detection. Best Pract. Res. Clin. Gastroenterol. 2010, 24, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Bang, U.C.; Benfield, T.; Hyldstrup, L.; Bendtsen, F.; Beck Jensen, J.E. Mortality, cancer, and comorbidities associated with chronic pancreatitis: A Danish nationwide matched-cohort study. Gastroenterology 2014, 146, 989–994. [Google Scholar] [CrossRef]
- Ueda, J.; Tanaka, M.; Ohtsuka, T.; Tokunaga, S.; Shimosegawa, T. Research Committee of Intractable Diseases of the Pancreas. Surgery for chronic pancreatitis decreases the risk for pancreatic cancer: A multicenter retrospective analysis. Surgery 2013, 153, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Whitcomb, D.C.; Frulloni, L.; Garg, P.; Greer, J.B.; Schneider, A.; Yadav, D.; Shimosegawa, T. Chronic pancreatitis: An international draft consensus proposal for a new mechanistic definition. Pancreatology 2016, 16, 218–224. [Google Scholar] [CrossRef]
- Liu, J.; Wang, Y.; Yu, Y. Meta-analysis reveals an association between acute pancreatitis and the risk of pancreatic cancer. World J. Clin. Cases 2020, 8, 4416–4430. [Google Scholar] [CrossRef]
- Aune, D.; Greenwood, D.C.; Chan, D.S.; Vieira, R.; Vieira, A.R.; Navarro Rosenblatt, D.A.; Cade, J.E.; Burley, V.J.; Norat, T. Body mass index, abdominal fatness and pancreatic cancer risk: A systematic review and non-linear dose-response meta-analysis of prospective studies. Ann Oncol. 2012, 23, 843–852. [Google Scholar] [CrossRef]
- Stolzenberg-Solomon, R.Z.; Adams, K.; Leitzmann, M.; Schairer, C.; Michaud, D.S.; Hollenbeck, A.; Schatzkin, A.; Silverman, D.T. Adiposity, physical activity, and pancreatic cancer in the National Institutes of Health-AARP Diet and Health Cohort. Am. J. Epidemiol. 2008, 167, 586–597. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Kikuchi, S.; Tamakoshi, A.; Yagyu, K.; Obata, Y.; Inaba, Y.; Kurosawa, M.; Kawamura, T.; Motohashi, Y.; Ishibashi, T.; et al. Obesity, physical activity and the risk of pancreatic cancer in a large Japanese cohort. Int. J. Cancer. 2007, 120, 2665–2671. [Google Scholar] [CrossRef]
- Koyanagi, Y.N.; Matsuo, K.; Ito, H.; Tamakoshi, A.; Sugawara, Y.; Hidaka, A.; Wada, K.; Oze, I.; Kitamura, Y.; Liu, R.; et al. Body-mass index and pancreatic cancer incidence: A pooled analysis of nine population-based cohort studies with more than 340,000 Japanese subjects. J. Epidemiol. 2018, 28, 245–252. [Google Scholar] [CrossRef]
- Matsuo, K.; Ito, H.; Wakai, K.; Nagata, C.; Mizoue, T.; Tanaka, K.; Tsuji, I.; Tamakoshi, A.; Sasazuki, S.; Inoue, M.; et al. Cigarette smoking and pancreas cancer risk: An evaluation based on a systematic review of epidemiologic evidence in the Japanese population. Jpn. J. Clin. Oncol. 2011, 41, 1292–1302. [Google Scholar] [CrossRef]
- Luo, J.; Iwasaki, M.; Inoue, M.; Sasazuki, S.; Otani, T.; Ye, W.; Tsugane, S.; JPHC Study Group. Body mass index, physical activity and the risk of pancreatic cancer in relation to smoking status and history of diabetes: A large-scale population-based cohort study in Japan—The JPHC study. Cancer Causes Control. 2007, 18, 603–612. [Google Scholar] [CrossRef]
- Lynch, S.M.; Vrieling, A.; Lubin, J.H.; Kraft, P.; Mendelsohn, J.B.; Hartge, P.; Canzian, F.; Steplowski, E.; Arslan, A.A.; Gross, M.; et al. Cigarette smoking and pancreatic cancer: A pooled analysis from the pancreatic cancer cohort consortium. Am. J. Epidemiol. 2009, 170, 403–413. [Google Scholar] [CrossRef]
- Tramacere, I.; Scotti, L.; Jenab, M.; Bagnardi, V.; Bellocco, R.; Rota, M.; Corrao, G.; Bravi, F.; Boffetta, P.; La Vecchia, C. Alcohol drinking and pancreatic cancer risk: A meta-analysis of the dose-risk relation. Int. J. Cancer. 2010, 126, 1474–1486. [Google Scholar] [CrossRef]
- Ojajärvi, A.; Partanen, T.; Ahlbom, A.; Hakulinen, T.; Kauppinen, T.; Weiderpass, E.; Wesseling, C. Estimating the relative risk of pancreatic cancer associated with exposure agents in job title data in a hierarchical Bayesian meta-analysis. Scand. J. Work Environ. Health 2007, 33, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Iodice, S.; Maisonneuve, P.; Botteri, E.; Sandri, M.T.; Lowenfels, A.B. ABO blood group and cancer. Eur. J. Cancer 2010, 46, 3345–3350. [Google Scholar] [CrossRef]
- Wolpin, B.M.; Chan, A.T.; Hartge, P.; Chanock, S.J.; Kraft, P.; Hunter, D.J.; Giovannucci, E.L.; Fuchs, C.S. ABO blood group and the risk of pancreatic cancer. J. Natl. Cancer Inst. 2009, 101, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Wolpin, B.M.; Kraft, P.; Gross, M.; Helzlsouer, K.; Bueno-de-Mesquita, H.B.; Steplowski, E.; Stolzenberg-Solomon, R.Z.; Arslan, A.A.; Jacobs, E.J.; Lacroix, A.; et al. Pancreatic cancer risk and ABO blood group alleles: Results from the pancreatic cancer cohort consortium. Cancer Res. 2010, 70, 1015–1023. [Google Scholar] [CrossRef]
- Risch, H.A.; Yu, H.; Lu, L.; Kidd, M.S. ABO blood group, Helicobacter pylori seropositivity, and risk of pancreatic cancer: A case-control study. J. Natl. Cancer Inst. 2010, 102, 502–505. [Google Scholar] [CrossRef] [PubMed]
- Risch, H.A.; Lu, L.; Kidd, M.S.; Wang, J.; Zhang, W.; Ni, Q.; Gao, Y.T.; Yu, H. Helicobacter pylori seropositivities and risk of pancreatic carcinoma. Cancer Epidemiol. Biomark. Prev. 2014, 23, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Bao, Y.; Spiegelman, D.; Li, R.; Giovannucci, E.; Fuchs, C.S.; Michaud, D.S. History of peptic ulcer disease and pancreatic cancer risk in men. Gastroenterology 2010, 138, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Iloeje, U.H.; Yang, H.I.; Jen, C.L.; Su, J.; Wang, L.Y.; You, S.L.; Lu, S.N.; Chen, C.J. Risk of pancreatic cancer in chronic hepatitis B virus infection: Data from the REVEAL-HBV cohort study. Liver Int. 2010, 30, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Beaney, A.J.; Banim, P.J.R.; Luben, R.; Lentjes, M.A.H.; Khaw, K.T.; Hart, A.R. Higher meat intake is positively associated with higher risk of developing pancreatic cancer in an age-dependent manner and are modified by plasma antioxidants: A prospective cohort study (EPIC-Norfolk) using data from food diaries. Pancreas 2017, 46, 672–678. [Google Scholar] [CrossRef]
- Rossi, M.; Lipworth, L.; Polesel, J.; Negri, E.; Bosetti, C.; Talamini, R.; McLaughlin, J.K.; La Vecchia, C. Dietary glycemic index and glycemic load and risk of pancreatic cancer: A case-control study. Ann. Epidemiol. 2010, 20, 460–465. [Google Scholar] [CrossRef]
- Polesel, J.; Talamini, R.; Negri, E.; Bosetti, C.; Boz, G.; Lucenteforte, E.; Franceschi, S.; Serraino, D.; La Vecchia, C. Dietary habits and risk of pancreatic cancer: An Italian case-control study. Cancer Causes Control. 2010, 21, 493–500. [Google Scholar] [CrossRef] [PubMed]
| Disease | Disease Gene | Hereditary Form | The Risk of PDAC |
|---|---|---|---|
| Hereditary pancreatitis | PRSS1 | Autosomal dominant | 60–87 |
| Hereditary breast and ovarian cancer syndrome | BRCA1/2 | Autosomal dominant | 4.1–5.8 |
| Peutz–Jeghers syndrome | STK11/LKB1 | Autosomal dominant | 132 |
| Familial atypical multiple mole melanoma syndrome | CDKN2A/p16 | Autosomal dominant | 13–22 |
| Hereditary colorectal adenomatous polyposis | APC | Autosomal dominant | 4.4 |
| Hereditary nonpolyposis colorectal cancer | hMSH2, hMLH1 | Autosomal dominant | 8.6 |
| Risk Factors | The Risk of PDAC | |
|---|---|---|
| Family history | Patients with PDAC in the family | 6.79-fold |
| Patients with family members with PDAC < 50 years old | 9.31-fold | |
| Genetic disorders | Hereditary pancreatitis | 67–87-fold |
| Hereditary pancreatic cancer syndrome | Refer to Table 1 | |
| Complications | Diabetes mellitus | <1 year 5.38-fold, 1–4 years 1.95-fold, 5–9 years 1.49-fold, ≥10 years 1.47-fold |
| Obesity | Risk of PDAC onset in males in their 20 s with body mass index ≥ 30 kg/m2: 3.5-fold | |
| Chronic pancreatitis | Within 4 years of diagnosis: 14.6-fold | |
| ≥5 years after diagnosis: 4.8-fold | ||
| Intraductal Papillary Mucinous Neoplasms (IPMNs) | Branch-type IPMN: 15.8–26-fold | |
| Preferences | Smoking | 1.68-fold |
| Alcohol | 1.22-fold | |
| Occupation | Chlorinated hydrocarbon exposure | 2.21-fold |
| Food | Red meat | 1.25–1.76-fold |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ushio, J.; Kanno, A.; Ikeda, E.; Ando, K.; Nagai, H.; Miwata, T.; Kawasaki, Y.; Tada, Y.; Yokoyama, K.; Numao, N.; et al. Pancreatic Ductal Adenocarcinoma: Epidemiology and Risk Factors. Diagnostics 2021, 11, 562. https://doi.org/10.3390/diagnostics11030562
Ushio J, Kanno A, Ikeda E, Ando K, Nagai H, Miwata T, Kawasaki Y, Tada Y, Yokoyama K, Numao N, et al. Pancreatic Ductal Adenocarcinoma: Epidemiology and Risk Factors. Diagnostics. 2021; 11(3):562. https://doi.org/10.3390/diagnostics11030562
Chicago/Turabian StyleUshio, Jun, Atsushi Kanno, Eriko Ikeda, Kozue Ando, Hiroki Nagai, Tetsurou Miwata, Yuki Kawasaki, Yamato Tada, Kensuke Yokoyama, Norikatsu Numao, and et al. 2021. "Pancreatic Ductal Adenocarcinoma: Epidemiology and Risk Factors" Diagnostics 11, no. 3: 562. https://doi.org/10.3390/diagnostics11030562
APA StyleUshio, J., Kanno, A., Ikeda, E., Ando, K., Nagai, H., Miwata, T., Kawasaki, Y., Tada, Y., Yokoyama, K., Numao, N., Tamada, K., Lefor, A. K., & Yamamoto, H. (2021). Pancreatic Ductal Adenocarcinoma: Epidemiology and Risk Factors. Diagnostics, 11(3), 562. https://doi.org/10.3390/diagnostics11030562







