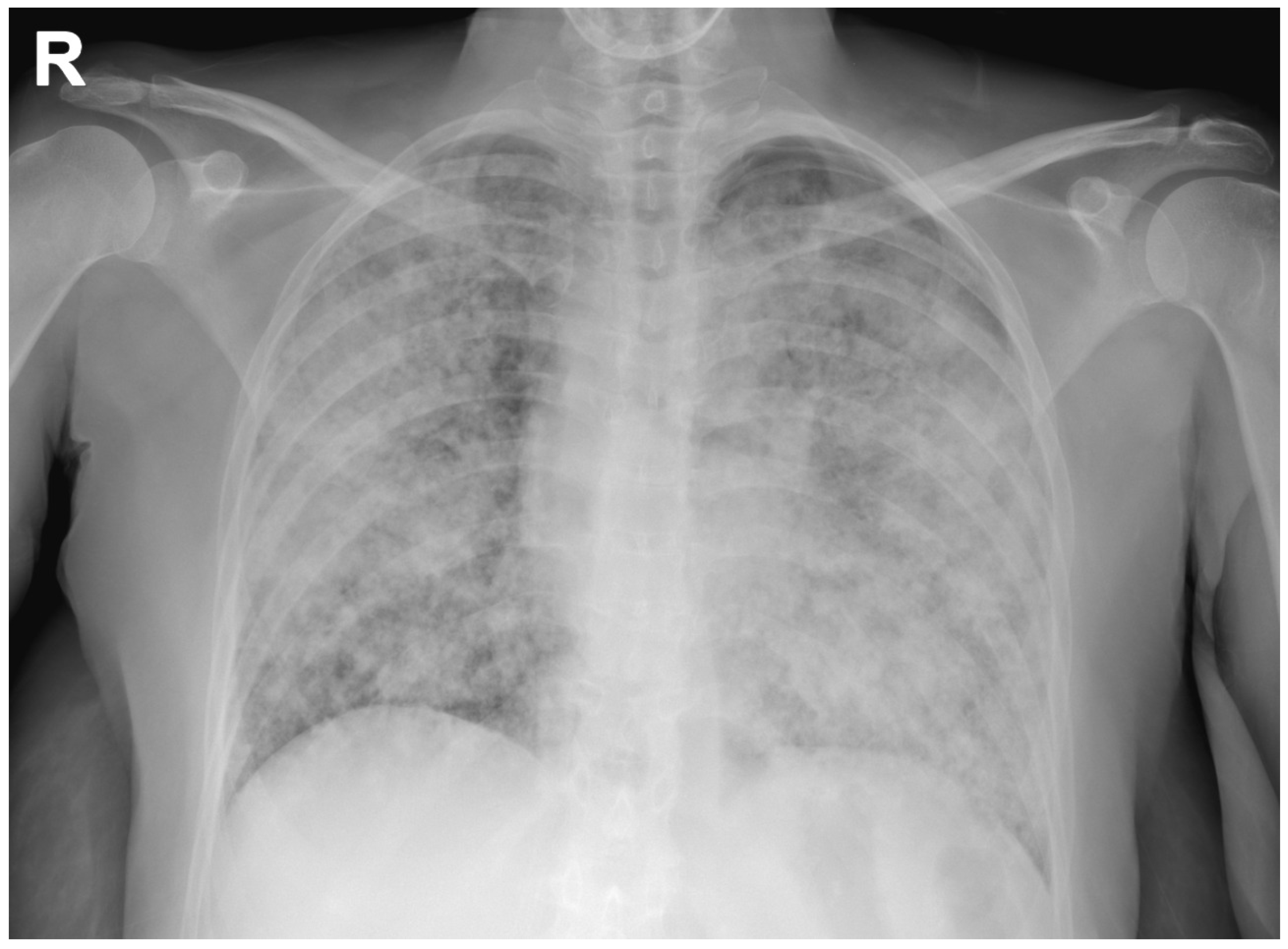
A “Galactic” Chest X-ray
Abstract
:- What Would Be Your Next Diagnostic Examination?
- Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Aikins, A.; Kanne, J.P.; Chung, J.H. Galaxy sign. J. Thorac. Imaging 2012, 27, W164. [Google Scholar] [CrossRef] [PubMed]
- Chiarenza, A.; Esposto Ultimo, L.; Falsaperla, D.; Travali, M.; Foti, P.V.; Torrisi, S.E.; Palmucci, S. Chest imaging using signs, symbols, and naturalistic images: A practical guide for radiologists and non-radiologists. Insights Imaging 2019, 10, 114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andreu, J.; Mauleón, S.; Pallisa, E.; Majó, J.; Martinez-Rodriguez, M.; Cáceres, J. Miliary lung disease revisited. Curr. Probl. Diagn. Radiol. 2002, 31, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Togashi, Y.; Masago, K.; Kubo, T.; Sakamori, Y.; Kim, Y.H.; Hatachi, Y.; Mishima, M. Association of diffuse, random pulmonary metastases, including miliary metastases, with epidermal growth factor receptor mutations in lung adenocarcinoma. Cancer 2011, 117, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Mirijello, A.; Zarrelli, M.; Miscio, G.; de Matthaeis, A.; Piscitelli, P.; Carbonelli, C.M.; De Cosmo, S. Diagnosis of COVID-19 in Patients with Negative Nasopharyngeal Swabs: Reliability of Radiological and Clinical Diagnosis and Accuracy Versus Serology. Diagnostics 2021, 11, 386. [Google Scholar] [CrossRef] [PubMed]
- Linder, J. Lung cancer cytology. Something old, something new. Am. J. Clin. Pathol. 2000, 114, 169–171. [Google Scholar] [CrossRef] [PubMed]

| Laboratory Tests | Results | Reference Range |
|---|---|---|
| ALT (U/L) | 20.00 | 10–42 |
| AST (U/L) | 24.00 | 8–30 |
| Total bilirubin (mg/dL) | 0.40 | 0.2–1.0 |
| Sodium (mmol/L) | 159.0 | 136–145 |
| Potassium (mmol/L) | 4.9 | 3.5–5.0 |
| Clorum (mmol/L) | 125.0 | 98–107 |
| Creatinine (mg/dL) | 0.50 | 0.55–1.02 |
| Urea (mg/dL) | 30.0 | 15–38 |
| Glycemia (mg/dL) | 92.0 | 70–100 |
| Total protein (g/dL) | 6.30 | 6.4–8.2 |
| C-reactive protein (mg/dL) | <0.290 | <0.30 |
| Erythrocyte sedimentation rate (mm) | 45 | 2–15 |
| Procalcitonin (µ/L) | 0.09 | <0.50 |
| Hemoglobin (g/dL) | 14.1 | 12–16 |
| Mean corpuscular volume (FL) | 87 | 77–98 |
| Red blood cells (103/mm3) | 5080 | 4200–5400 |
| White blood cells (/mm3) | 20,650 | 4300–10,800 |
| Neutrophilis (%) | 94.6 | 40–80 |
| Lymphocytes (%) | 3.5 | 10–45 |
| Monocytes (%) | 1.3 | 2.0–10.0 |
| Basophils (%) | 0.00 | <1.50 |
| Eosinophils (%) | 0.4 | 0.3–7.0 |
| Platelets (103/mm3) | 481 | 130–400 |
| Fibrinogen (mg/dL) | 669 | 150–400 |
| INR (Ratio) | 1.03 | 0.80–1.20 |
| pH | 7.44 | 7.35–7.45 |
| PCO2 (mmHg) | 31.5 | 35.0–45.0 |
| PO2 (mmHg) | 52.9 | 80.0–100.0 |
| HCO3 (mmol/L) | 21.9 | 22.0–26.0 |
| Lactate (mmol/L) | 0.9 | 0.5–1.6 |
| SpO2 (%) | 91.2 | 90–99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carbonelli, C.; de Matthaeis, A.; Mirijello, A.; Di Micco, C.; Maiello, E.; De Cosmo, S.; Graziano, P. A “Galactic” Chest X-ray. Diagnostics 2021, 11, 899. https://doi.org/10.3390/diagnostics11050899
Carbonelli C, de Matthaeis A, Mirijello A, Di Micco C, Maiello E, De Cosmo S, Graziano P. A “Galactic” Chest X-ray. Diagnostics. 2021; 11(5):899. https://doi.org/10.3390/diagnostics11050899
Chicago/Turabian StyleCarbonelli, Cristiano, Angela de Matthaeis, Antonio Mirijello, Concetta Di Micco, Evaristo Maiello, Salvatore De Cosmo, and Paolo Graziano. 2021. "A “Galactic” Chest X-ray" Diagnostics 11, no. 5: 899. https://doi.org/10.3390/diagnostics11050899
APA StyleCarbonelli, C., de Matthaeis, A., Mirijello, A., Di Micco, C., Maiello, E., De Cosmo, S., & Graziano, P. (2021). A “Galactic” Chest X-ray. Diagnostics, 11(5), 899. https://doi.org/10.3390/diagnostics11050899







