Can the MMPI Predict Adult ADHD? An Approach Using Machine Learning Methods
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Experimental Results
3.1.1. General Characteristics
3.1.2. Prediction Accuracy of ML Model
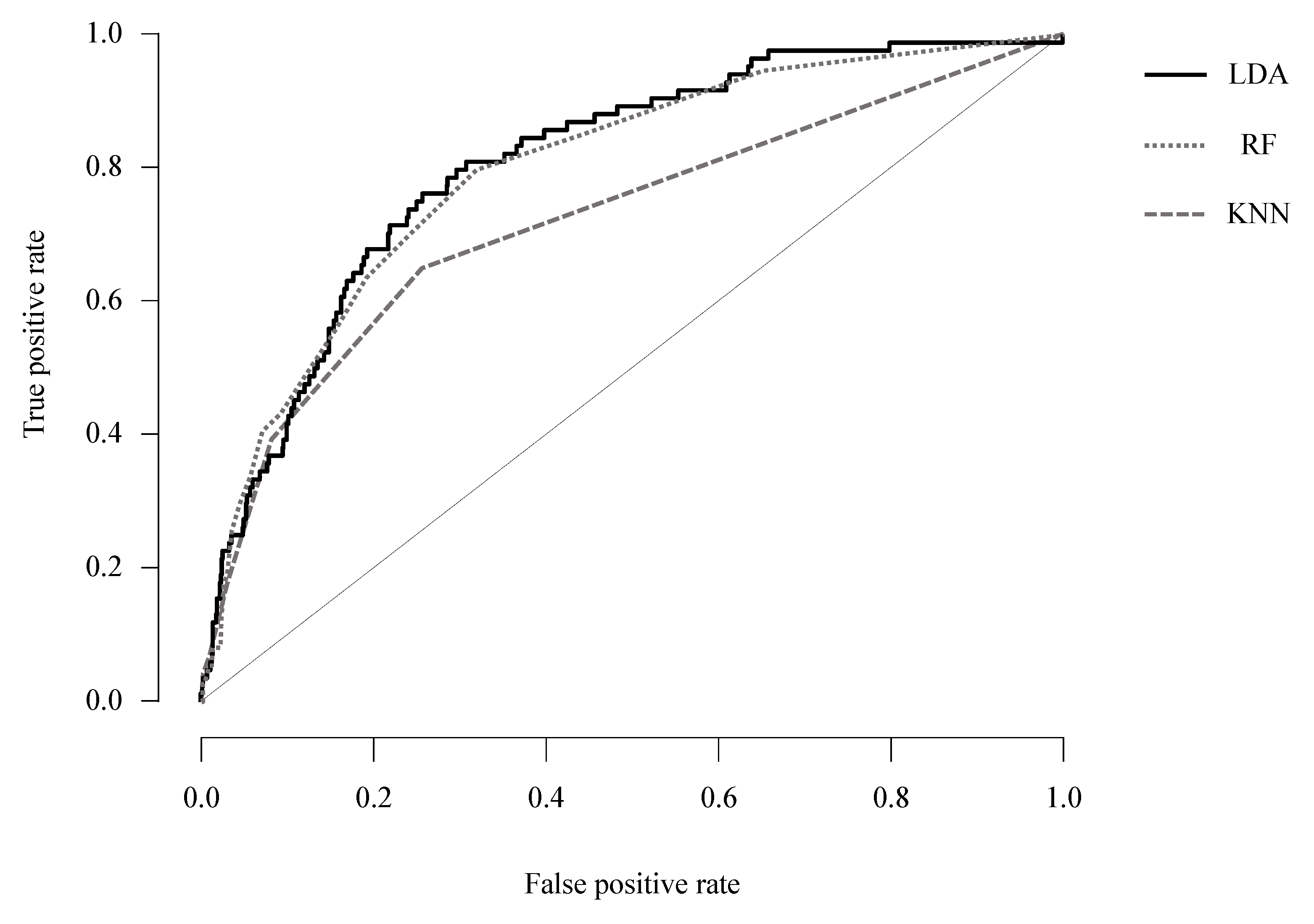
3.1.3. AUC of ML Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub: Washington, DC, USA, 2013. [Google Scholar]
- Barkley, R.A.; Fischer, M.; Smallish, L.; Fletcher, K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J. Abnorm. Psychol. 2002, 111, 279. [Google Scholar] [CrossRef]
- Wender, P.H. Attention-deficit hyperactivity disorder in adults. Psychiatr. Clin. N. Am. 1998, 21, 761–774. [Google Scholar] [CrossRef]
- Kessler, R.C.; Adler, L.A.; Gruber, M.J.; Sarawate, C.A.; Spencer, T.; Van Brunt, D.L. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a representative sample of health plan members. Int. J. Methods Psychiatr. Res. 2007, 16, 52–65. [Google Scholar] [CrossRef] [PubMed]
- De Graaf, R.; Kessler, R.C.; Fayyad, J.; ten Have, M.; Alonso, J.; Angermeyer, M.; Borges, G.; Demyttenaere, K.; Gasquet, I.; de Girolamo, G.; et al. The prevalence and effects of adult attention-deficit/hyperactivity disorder (ADHD) on the performance of workers: Results from the WHO World Mental Health Survey Initiative. Occup. Environ. Med. 2008, 65, 835–842. [Google Scholar] [CrossRef] [Green Version]
- Montejano, L.; Sasane, R.; Hodgkins, P.; Russo, L.; Huse, D. Adult ADHD: Prevalence of diagnosis in a US population with employer health insurance. Curr. Med. Res. Opin. 2011, 27 (Suppl. 2), 5–11. [Google Scholar] [CrossRef]
- Montes, L.G.A.; García, A.O.H.; Ricardo-Garcell, J. ADHD prevalence in adult outpatients with nonpsychotic psychiatric illnesses. J. Atten. Disord. 2007, 11, 150–156. [Google Scholar] [CrossRef]
- Park, S.; Cho, M.J.; Chang, S.M.; Jeon, H.J.; Cho, S.J.; Kim, B.S.; Bae, J.N.; Wang, H.R.; Ahn, J.H.; Hong, J.P. Prevalence, correlates, and comorbidities of adult ADHD symptoms in Korea: Results of the Korean epidemiologic catchment area study. Psychiatry Res. 2011, 186, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Weiss, M.; Murray, C.; Weiss, G. Adults with attention-deficit/hyperactivity disorder: Current concepts. J. Psychiatr. Pract. 2002, 8, 99–111. [Google Scholar] [CrossRef]
- Kessler, R.C.; Green, J.G.; Adler, L.A.; Barkley, R.A.; Chatterji, S.; Faraone, S.V.; Finkelman, M.; Greenhill, L.L.; Gruber, M.J.; Jewell, M.; et al. Structure and diagnosis of adult attention-deficit/hyperactivity disorder: Analysis of expanded symptom criteria from the Adult ADHD Clinical Diagnostic Scale. Arch. Gen. Psychiatry 2010, 67, 1168–1178. [Google Scholar] [CrossRef] [Green Version]
- Sibley, M.H.; Pelham, W.E.; Molina, B.S.G.; Gnagy, E.M.; Waschbusch, D.A.; Garefino, A.C.; Kuriyan, A.B.; Babinski, D.E.; Karch, K.M. Diagnosing ADHD in adolescence. J. Consult. Clin. Psychol. 2012, 80, 139–150. [Google Scholar] [CrossRef] [Green Version]
- Ward, M.F.; Wender, P.H.; Reimherr, F.W. The Wender Utah Rating Scale: An aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am. J. Psychiatry 1993, 150, 885–890. [Google Scholar] [CrossRef]
- Adler, L.A.; Spencer, T.; Faraone, S.V.; Kessler, R.C.; Howes, M.J.; Biederman, J.; Secnik, K. Validity of pilot Adult ADHD Self- Report Scale (ASRS) to Rate Adult ADHD symptoms. Ann. Clin. Psychiatry 2006, 18, 145–148. [Google Scholar] [CrossRef]
- Barkley, R.A. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychol. Bull. 1997, 121, 65–94. [Google Scholar] [CrossRef] [Green Version]
- Canu, W.H.; Carlson, C.L. Rejection sensitivity and social outcomes of young adult men with ADHD. J. Atten. Disord. 2007, 10, 261–275. [Google Scholar] [CrossRef] [Green Version]
- Conners, C.K.; Erhardt, D.; Sparrow, E.P. Conners’ Adult ADHD Rating Scales (CAARS): Technical Manual; Multi-Health Systems: North Tonawanda, NY, USA, 1999. [Google Scholar]
- Corbisiero, S.; Morstedt, B.; Bitto, H.; Stieglitz, R.D. Emotional Dysregulation in Adults with Attention-Deficit/Hyperactivity Disorder-Validity, Predictability, Severity, and Comorbidity. J. Clin. Psychol. 2017, 73, 99–112. [Google Scholar] [CrossRef]
- Faraone, S.; Biederman, J.; Spencer, T. Diagnostic efficiency of symptom items for identifying adult ADHD. J. Adhd. Relat. Disord. 2010, 1, 38–48. [Google Scholar]
- Musser, E.D.; Nigg, J.T. Emotion Dysregulation Across Emotion Systems in Attention Deficit/Hyperactivity Disorder. J. Clin. Child Adolesc. Psychol. 2019, 48, 153–165. [Google Scholar] [CrossRef]
- Safren, S.A.; Sprich, S.E.; Cooper-Vince, C.; Knouse, L.E.; Lerner, J.A. Life impairments in adults with medication-treated ADHD. J. Atten. Disord. 2010, 13, 524–531. [Google Scholar] [CrossRef]
- Shaw-Zirt, B.; Popali-Lehane, L.; Chaplin, W.; Bergman, A. Adjustment, social skills, and self-esteem in college students with symptoms of ADHD. J. Atten. Disord. 2005, 8, 109–120. [Google Scholar] [CrossRef]
- Willcutt, E.G.; Doyle, A.E.; Nigg, J.T.; Faraone, S.V.; Pennington, B.F. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biol. Psychiatry 2005, 57, 1336–1346. [Google Scholar] [CrossRef]
- Yoo, A.K.E.-H.L.; Sang, S.J.S.-T.H.; Kim, H.H.J.-H. Validation of the Korean Version of Barkley Deficits in Executive Functioning Scale Short-Form. Korean J. Clin. Psychol. 2019, 38, 247–256. [Google Scholar]
- McCabe, S.E.; Teter, C.J.; Boyd, C.J. The use, misuse and diversion of prescription stimulants among middle and high school students. Subst. Use Misuse 2004, 39, 1095–1116. [Google Scholar] [CrossRef] [PubMed]
- Rushton, J.L.; Whitmire, J.T. Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends: 1992 to 1998. Arch. Pediatr. Adolesc. Med. 2001, 155, 560–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease and Prevention. Attention Deficit/Hyperactivity Disorder (ADHD): Data and Statistics; Centers for Disease and Prevention: Washington, DC, USA, 2013.
- Babcock, Q.; Byrne, T. Student perceptions of methylphenidate abuse at a public liberal arts college. J. Am. Coll. Health 2000, 49, 143–145. [Google Scholar] [CrossRef] [PubMed]
- DeSantis, A.D.; Webb, E.M.; Noar, S.M. Illicit use of prescription ADHD medications on a college campus: A multimethodological approach. J. Am. Coll. Health 2008, 57, 315–324. [Google Scholar] [CrossRef] [PubMed]
- McCabe, S.E.; Teter, C.J.; Boyd, C.J.; Knight, J.R.; Wechsler, H. Nonmedical use of prescription opioids among US college students: Prevalence and correlates from a national survey. Addict. Behav. 2005, 30, 789–805. [Google Scholar] [CrossRef] [PubMed]
- DeSantis, A.D.; Hane, A.C. “Adderall is definitely not a drug”: Justifications for the illegal use of ADHD stimulants. Subst. Use Misuse 2010, 45, 31–46. [Google Scholar] [CrossRef]
- Harp, J.P.; Jasinski, L.J.; Shandera-Ochsner, A.L.; Mason, L.H.; Berry, D.T. Detection of malingered ADHD using the MMPI-2-RF. Psychol. Inj. Law 2011, 4, 32–43. [Google Scholar] [CrossRef]
- Kessler, R.C.; Adler, L.; Ames, M.; Demler, O.; Faraone, S.; Hiripi, E.; Howes, M.J.; Jin, R.; Secnik, K.; Spencer, T. The World Health Organization Adult ADHD Self-Report Scale (ASRS): A short screening scale for use in the general population. Psychol. Med. 2005, 35, 245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, E.V.; Rogers, R. Detection of feigned ADHD across two domains: The MMPI-2-RF and CAARS for faked symptoms and TOVA for simulated attention deficits. J. Psychopathol. Behav. Assess. 2018, 40, 376–385. [Google Scholar] [CrossRef]
- Greene, R.L. The MMPI-2: An Interpretive Manual; Allyn & Bacon: Boston, MA, USA, 2000. [Google Scholar]
- Lubin, B.; Larsen, R.M.; Matarazzo, J.D. Patterns of psychological test usage in the United States: 1935–1982. Am. Psychol. 1984, 39, 451. [Google Scholar] [CrossRef]
- Lubin, B.; Larsen, R.M.; Matarazzo, J.D.; Seever, M. Psychological test usage patterns in five professional settings. Am. Psychol. 1985, 40, 857. [Google Scholar] [CrossRef]
- Tellegen, A.; Ben-Porath, Y.; McNulty, J.; Arbisi, P.; Graham, J.; Kaemmer, B. MMPI-2 Restructured Clinical (RC) Scales: Development, Validation, and Interpretation; University of Minnesota Press: Minneapolis, MN, USA, 2003. [Google Scholar]
- Ben-Porath, Y.S. Interpreting the MMPI-2-RF; University of Minnesota Press: Minneapolis, MN, USA, 2012. [Google Scholar]
- Ben-Porath, Y.S.; Butcher, J.N. The comparability of MMPI and MMPI-2 scales and profiles. Psychol. Assess. J. Consult. Clin. Psychol. 1989, 1, 345. [Google Scholar] [CrossRef]
- Pope, K.S.; Butcher, J.N.; Seelen, J. The MMPI, MMPI-2, & MMPI-A in Court: A Practical Guide for Expert Witnesses and Attorneys; American Psychological Association: Washington, DC, USA, 2006. [Google Scholar]
- Dwyer, D.B.; Falkai, P.; Koutsouleris, N. Machine Learning Approaches for Clinical Psychology and Psychiatry. Annu. Rev. Clin. Psychol. 2018, 14, 91–118. [Google Scholar] [CrossRef]
- Linthicum, K.P.; Schafer, K.M.; Ribeiro, J.D. Machine learning in suicide science: Applications and ethics. Behav. Sci. Law 2019, 37, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Barry, R.J.; Clarke, A.R.; Johnstone, S.J. A review of electrophysiology in attention-deficit/hyperactivity disorder: I. Qualitative and quantitative electroencephalography. Clin. Neurophysiol. 2003, 114, 171–183. [Google Scholar] [CrossRef]
- Buchsbaum, M.; Wender, P. Average evoked responses in normal and minimally brain dysfunctioned children treated with amphetamine: A preliminary report. Arch. Gen. Psychiatry 1973, 29, 764–770. [Google Scholar] [CrossRef] [PubMed]
- Robaey, P.; Breton, F.; Dugas, M.; Renault, B. An event-related potential study of controlled and automatic processes in 6-8-year-old boys with attention deficit hyperactivity disorder. Electroencephalogr. Clin. Neurophysiol. 1992, 82, 330–340. [Google Scholar] [CrossRef]
- Satterfield, J.H.; Braley, B.W. Evoked potentials and brain maturation in hyperactive and normal children. Electroencephalogr. Clin. Neurophysiol. 1977, 43, 43–51. [Google Scholar] [CrossRef]
- Smith, J.L.; Johnstone, S.J.; Barry, R.J. Aiding diagnosis of attention-deficit/hyperactivity disorder and its subtypes: Discriminant function analysis of event-related potential data. J. Child Psychol. Psychiatry 2003, 44, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, H.-K.; Lee, K. Assessment of suicidal risk using Minnesota multiphasic personality inventory-2 restructured form. BMC Psychiatry 2020, 20, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.; Lee, H.-K.; Lee, K. Which PHQ-9 items can effectively screen for suicide? Machine learning approaches. Int. J. Environ. Res. Public Health 2021, 18, 3339. [Google Scholar] [CrossRef]
- Lee, K.; Lee, H.-K.; Kim, S.; Kim, S.H. The relationship between circadian typology and lifetime experiences of hypomanic symptoms. Psychiatry Res. 2021, 298, 113788. [Google Scholar] [CrossRef]
- Han, K.H.; Moon, K.J.; Lim, J.Y.; Kim, J.S. MMPI-2-RF: Manual for Korean Version of MMPI-2-RF; Maumsarang Ltd.: Seoul, Korea, 2011. [Google Scholar]
- Kim, J.H.; Lee, E.H.; Joung, Y.S. The WHO Adult ADHD Self-Report Scale: Reliability and Validity of the Korean Version. Psychiatry Investig. 2013, 10, 41–46. [Google Scholar] [CrossRef] [Green Version]
- Instanes, J.T.; Haavik, J.; Halmoy, A. Personality Traits and Comorbidity in Adults with ADHD. J. Atten. Disord. 2016, 20, 845–854. [Google Scholar] [CrossRef]
- Hand, D.J. Principles of data mining. Drug Saf. 2007, 30, 621–622. [Google Scholar] [CrossRef]
- McLachlan, G.J. Discriminant Analysis and Statistical Pattern Recognition; John Wiley & Sons: Hoboken, NJ, USA, 2004; Volume 544. [Google Scholar]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; Volume 398. [Google Scholar]
- Nguyen, Q.H.; Ly, H.-B.; Ho, L.S.; Al-Ansari, N.; Le, H.V.; Tran, V.Q.; Prakash, I.; Pham, B.T. Influence of Data Splitting on Performance of Machine Learning Models in Prediction of Shear Strength of Soil. Math. Probl. Eng. 2021, 2021, 4832864. [Google Scholar] [CrossRef]
- Deo, R.C. Machine Learning in Medicine. Circulation 2015, 132, 1920–1930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Team, J. JASP; 0.14.1; University of Amsterdam: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Faraone, S.V.; Biederman, J.; Mick, E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychol. Med. 2006, 36, 159–165. [Google Scholar] [CrossRef]
- Gizer, I.R.; Ficks, C.; Waldman, I.D. Candidate gene studies of ADHD: A meta-analytic review. Hum. Genet. 2009, 126, 51–90. [Google Scholar] [CrossRef] [PubMed]
- Duda, M.; Haber, N.; Daniels, J.; Wall, D.P. Crowdsourced validation of a machine-learning classification system for autism and ADHD. Transl. Psychiatry 2017, 7, e1133. [Google Scholar] [CrossRef]
- Singh, Y.; Bhatia, P.K.; Sangwan, O. A review of studies on machine learning techniques. Int. J. Comput. Sci. Secur. 2007, 1, 70–84. [Google Scholar]
- Lee, S.; Choi, J.-W.; Kim, K.-M.; Kim, J.W.; Kim, S.; Kang, T.; Kim, J.I.; Lee, Y.S.; Kim, B.; Han, D.H. The guideline of diagnosis and treatment of attention-deficit hyperactivity disorder: Developed by ADHD translational research center. J. Korean Acad. Child Adolesc. Psychiatry 2016, 27, 236–266. [Google Scholar] [CrossRef]
- Davidson, M.A. ADHD in adults: A review of the literature. J. Atten. Disord. 2008, 11, 628–641. [Google Scholar] [CrossRef] [PubMed]
- Lenartowicz, A.; Loo, S.K. Use of EEG to diagnose ADHD. Curr. Psychiatry Rep. 2014, 16, 498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Mahony, N.; Florentino-Liano, B.; Carballo, J.J.; Baca-García, E.; Rodríguez, A.A. Objective diagnosis of ADHD using IMUs. Med. Eng. Phys. 2014, 36, 922–926. [Google Scholar] [CrossRef]
- Peng, X.; Lin, P.; Zhang, T.; Wang, J. Extreme learning machine-based classification of ADHD using brain structural MRI data. PLoS ONE 2013, 8, e79476. [Google Scholar] [CrossRef]
| Dimension | Scale | ASRS (−) | ASRS (+) | t | p | Cohen’s d | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Validity Indicators | VRIN_r | 4.19 | ± | 2.37 | 5.27 | ± | 2.69 | −8.51 | <0.001 | −0.45 |
| TRIN_r | 10.37 | ± | 1.97 | 11.25 | ± | 2.27 | −8.28 | <0.001 | −0.44 | |
| F_r | 3.57 | ± | 3.35 | 7.59 | ± | 4.64 | −21.99 | <0.001 | −1.17 | |
| Fp_r | 2.18 | ± | 2.02 | 3.86 | ± | 2.88 | −15.12 | <0.001 | −0.80 | |
| Fs | 2.15 | ± | 1.94 | 4.14 | ± | 2.47 | −18.90 | <0.001 | −1.00 | |
| FBS_r | 9.11 | ± | 3.48 | 12.01 | ± | 4.07 | −15.50 | <0.001 | −0.82 | |
| L_r | 4.46 | ± | 2.24 | 3.25 | ± | 2.09 | 10.24 | <0.001 | 0.54 | |
| K_r | 7.24 | ± | 2.67 | 4.77 | ± | 2.29 | 17.54 | <0.001 | 0.93 | |
| Higher- Order (H-O) | EID | 13.99 | ± | 6.60 | 20.87 | ± | 7.22 | −19.55 | <0.001 | −1.04 |
| THD | 2.55 | ± | 2.70 | 4.86 | ± | 3.95 | −15.61 | <0.001 | −0.83 | |
| BXD | 6.16 | ± | 2.96 | 8.47 | ± | 3.04 | −14.68 | <0.001 | −0.78 | |
| Restructured Clinical (RC) | RCd | 7.38 | ± | 5.17 | 13.54 | ± | 5.40 | −22.41 | <0.001 | −1.19 |
| RC1 | 6.62 | ± | 3.93 | 10.17 | ± | 4.83 | −16.75 | <0.001 | −0.89 | |
| RC2 | 5.53 | ± | 3.11 | 6.57 | ± | 3.20 | −6.32 | <0.001 | −0.34 | |
| RC3 | 4.76 | ± | 2.58 | 6.69 | ± | 2.81 | −13.99 | <0.001 | −0.74 | |
| RC4 | 4.03 | ± | 2.60 | 6.21 | ± | 3.03 | −15.60 | <0.001 | −0.83 | |
| RC6 | 1.46 | ± | 1.83 | 2.99 | ± | 2.78 | −15.07 | <0.001 | −0.80 | |
| RC7 | 7.78 | ± | 4.31 | 12.59 | ± | 4.47 | −20.98 | <0.001 | −1.11 | |
| RC8 | 3.18 | ± | 2.59 | 5.72 | ± | 3.22 | −18.17 | <0.001 | −0.96 | |
| RC9 | 11.28 | ± | 4.61 | 14.71 | ± | 4.01 | −14.19 | <0.001 | −0.75 | |
| Content, Clinical Subscale | MLS | 3.02 | ± | 1.60 | 3.97 | ± | 1.77 | −11.08 | <0.001 | −0.59 |
| GIC | 0.64 | ± | 1.04 | 1.21 | ± | 1.36 | −9.99 | <0.001 | −0.53 | |
| HPC | 1.31 | ± | 1.37 | 2.25 | ± | 1.74 | −12.71 | <0.001 | −0.67 | |
| NUC | 2.99 | ± | 1.69 | 4.02 | ± | 1.74 | −11.56 | <0.001 | −0.61 | |
| COG | 3.06 | ± | 2.13 | 5.68 | ± | 2.16 | −23.18 | <0.001 | −1.23 | |
| SUI | 0.29 | ± | 0.74 | 0.82 | ± | 1.25 | −12.72 | <0.001 | −0.67 | |
| HLP | 1.00 | ± | 1.07 | 1.82 | ± | 1.28 | −14.23 | <0.001 | −0.76 | |
| SFD | 1.41 | ± | 1.26 | 2.45 | ± | 1.28 | −15.54 | <0.001 | −0.82 | |
| NFC | 4.01 | ± | 2.16 | 5.73 | ± | 1.98 | −15.13 | <0.001 | −0.80 | |
| STW | 2.76 | ± | 1.72 | 4.20 | ± | 1.76 | −15.77 | <0.001 | −0.84 | |
| AXY | 0.42 | ± | 0.82 | 1.16 | ± | 1.25 | −16.50 | <0.001 | −0.88 | |
| ANP | 2.37 | ± | 1.64 | 3.78 | ± | 1.75 | −16.07 | <0.001 | −0.85 | |
| BRF | 2.00 | ± | 1.55 | 2.73 | ± | 1.77 | −8.75 | <0.001 | −0.46 | |
| MSF | 3.97 | ± | 2.31 | 4.03 | ± | 2.32 | −0.45 | 0.66 | −0.02 | |
| JCP | 0.83 | ± | 1.07 | 1.48 | ± | 1.39 | −11.35 | <0.001 | −0.60 | |
| SUB | 0.70 | ± | 0.95 | 1.16 | ± | 1.32 | −8.79 | <0.001 | −0.47 | |
| AGG | 2.51 | ± | 1.85 | 3.90 | ± | 1.99 | −14.19 | <0.001 | −0.75 | |
| ACT | 2.36 | ± | 1.74 | 3.61 | ± | 1.73 | −13.57 | <0.001 | −0.72 | |
| FML | 2.07 | ± | 1.85 | 3.73 | ± | 2.22 | −16.72 | <0.001 | −0.89 | |
| IPP | 4.37 | ± | 2.18 | 4.50 | ± | 2.16 | −1.12 | 0.26 | −0.06 | |
| SAV | 4.16 | ± | 2.58 | 4.54 | ± | 2.67 | −2.73 | 0.01 | −0.15 | |
| SHY | 3.33 | ± | 2.01 | 4.27 | ± | 1.92 | −8.91 | <0.001 | −0.47 | |
| DSF | 0.78 | ± | 1.12 | 1.37 | ± | 1.46 | −9.61 | <0.001 | −0.51 | |
| AES | 2.94 | ± | 1.69 | 3.12 | ± | 1.76 | −2.04 | 0.04 | −0.11 | |
| MEC | 2.22 | ± | 1.81 | 2.41 | ± | 1.88 | −1.95 | 0.05 | −0.10 | |
| Personality Psychopathology Five (PSY-5) | AGGR_r | 7.85 | ± | 3.23 | 8.56 | ± | 3.14 | −4.16 | <0.001 | −0.22 |
| PSYC_r | 3.07 | ± | 2.79 | 5.60 | ± | 3.89 | −16.58 | <0.001 | −0.88 | |
| DISC_r | 5.73 | ± | 2.54 | 7.16 | ± | 2.67 | −10.61 | <0.001 | −0.56 | |
| NEGE_r | 7.88 | ± | 3.87 | 11.43 | ± | 3.72 | −17.36 | <0.001 | −0.92 | |
| INTR_r | 8.06 | ± | 3.82 | 8.26 | ± | 3.74 | −1.01 | 0.31 | −0.05 | |
| Trees or Nearest Neighbors | Validation Accuracy | Test Accuracy | OOB Accuracy | |
|---|---|---|---|---|
| K-Nearest Neighbors Classification | 7 | 0.927 | 0.931 | |
| Linear Discriminant Analysis | 0.912 | |||
| Random Forest Classification | 40 | 0.944 | 0.936 | 0.078 |
| Precision | Recall | F1 Score | AUC | |
|---|---|---|---|---|
| K-Nearest Neighbors Classification | 0.900 | 0.931 | 0.909 | 0.722 |
| Linear Discriminant Analysis | 0.899 | 0.912 | 0.905 | 0.806 |
| Random Forest Classification | 0.916 | 0.936 | 0.909 | 0.790 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Lee, H.-K.; Lee, K. Can the MMPI Predict Adult ADHD? An Approach Using Machine Learning Methods. Diagnostics 2021, 11, 976. https://doi.org/10.3390/diagnostics11060976
Kim S, Lee H-K, Lee K. Can the MMPI Predict Adult ADHD? An Approach Using Machine Learning Methods. Diagnostics. 2021; 11(6):976. https://doi.org/10.3390/diagnostics11060976
Chicago/Turabian StyleKim, Sunhae, Hye-Kyung Lee, and Kounseok Lee. 2021. "Can the MMPI Predict Adult ADHD? An Approach Using Machine Learning Methods" Diagnostics 11, no. 6: 976. https://doi.org/10.3390/diagnostics11060976
APA StyleKim, S., Lee, H.-K., & Lee, K. (2021). Can the MMPI Predict Adult ADHD? An Approach Using Machine Learning Methods. Diagnostics, 11(6), 976. https://doi.org/10.3390/diagnostics11060976






