Framing Cause-Effect Relationship of Acute Coronary Syndrome in Patients with Chronic Kidney Disease
Abstract
:1. Introduction
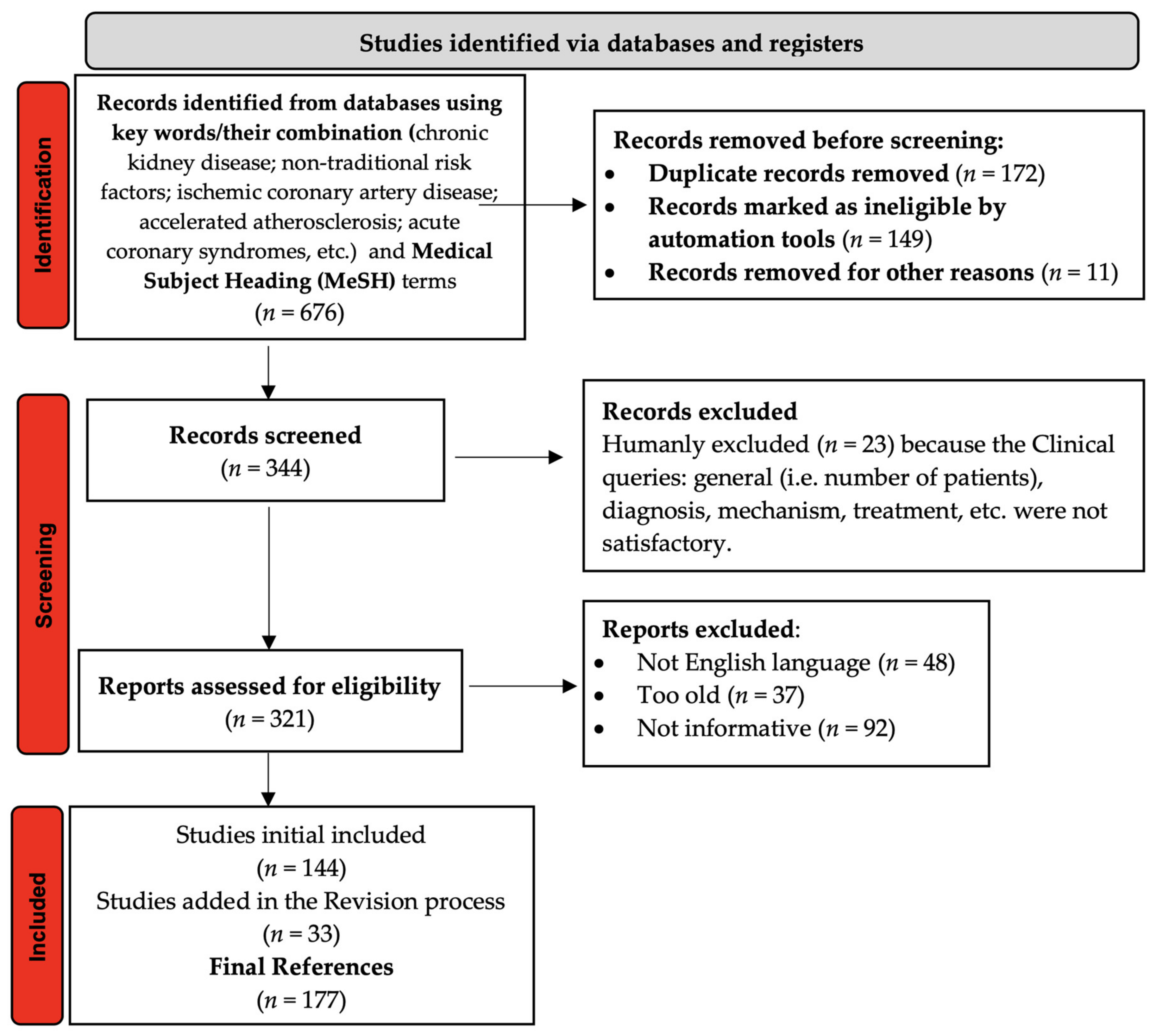
2. Materials and Methods
3. Development and Evolution of Cardiovascular Diseases—The Role of Independent Risk Factors Attributed to CKD
4. CKD—Equivalent to Ischemic Coronary Heart Disease in Terms of Risk of Death
5. The Role of Dyslipidemia in Initiating the Process of Atherosclerosis in Patients with CKD
6. Proteinuria and Microalbuminuria—The Role Played in the Process of Atherosclerosis in CKD
7. The Role of Inflammation in the Initiation of Atherosclerosis and Specific Features in Patients with CKD
8. Oxidative Stress and Endothelial Dysfunction—Aspects Regarding the Pathogenesis of Atherosclerosis in the Context of CKD
9. The Anemia Role in the Pathogenesis of Atherosclerosis in CKD
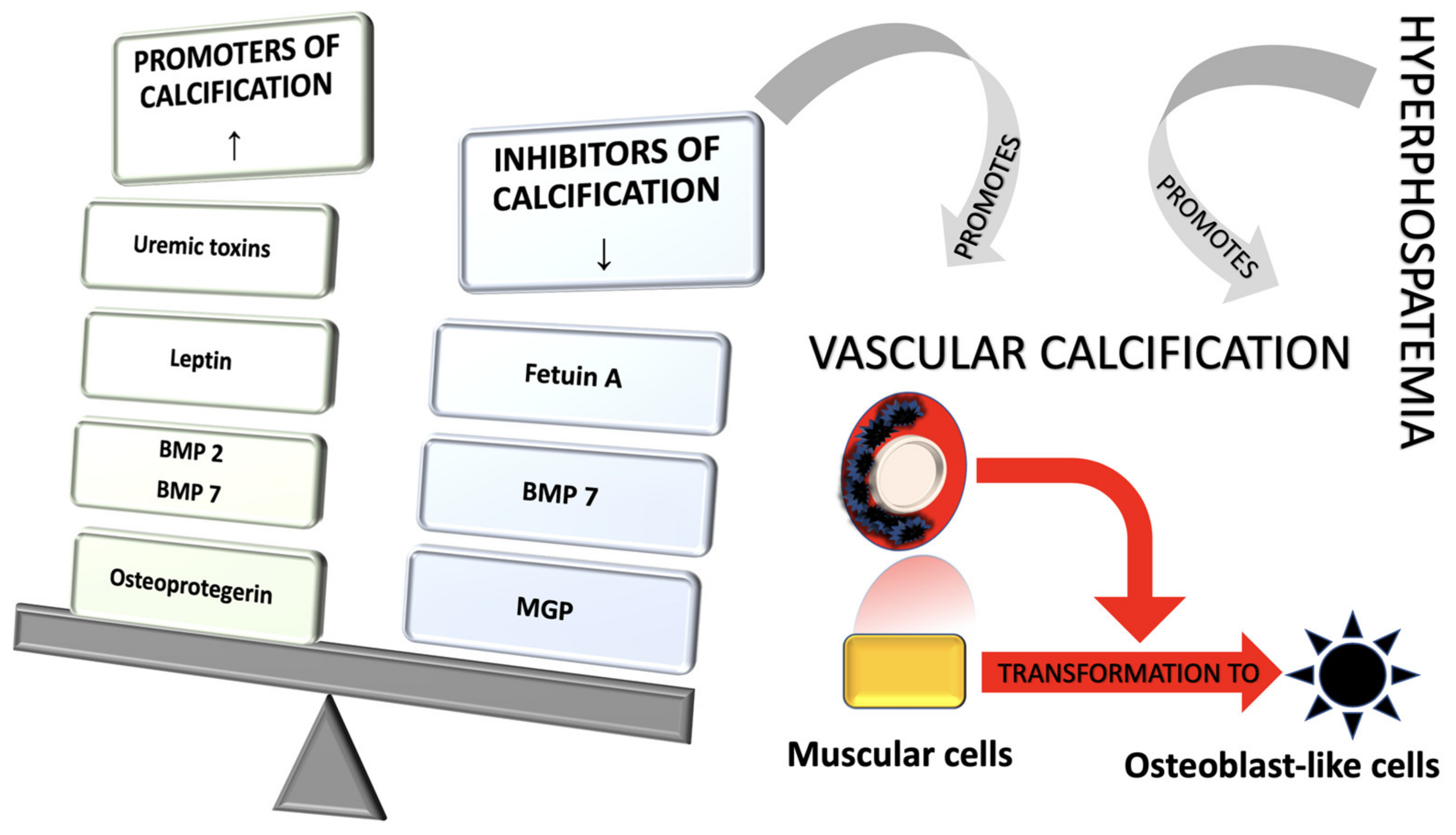
10. Arteriosclerosis and Vascular Calcification—The Role in the Pathogenesis of ACS in Patients with CKD
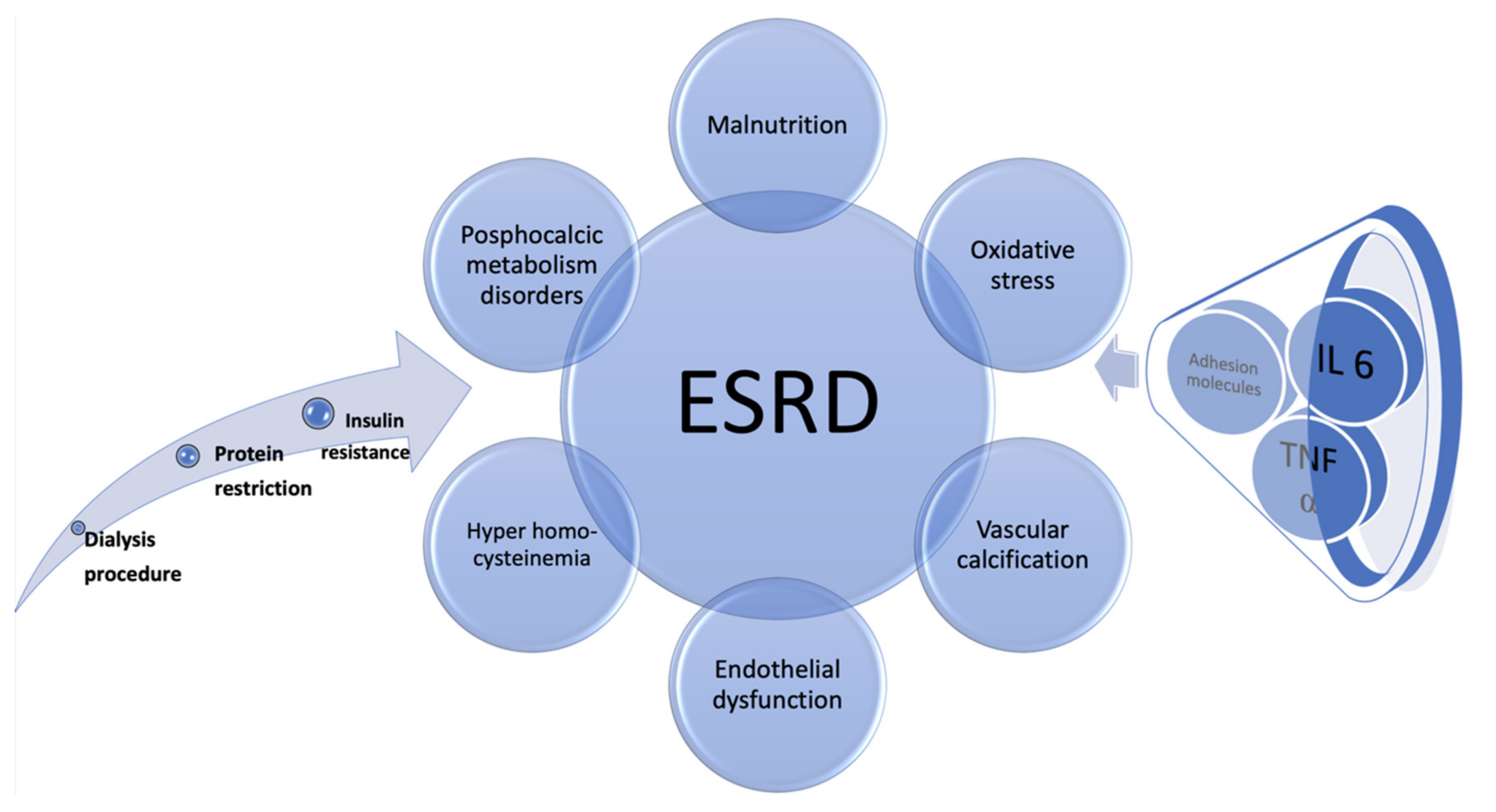
11. Particularities of the Atherosclerotic Process in Patients with End-Stage Renal Disease
12. Treatment Options of ACS in CKD Patients
13. Recent Information on Patients with ACS and CKD
14. Conclusions
15. Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Moisi, M.I.; Rus, M.; Bungau, S.; Zaha, D.C.; Uivarosan, D.; Fratila, O.; Tit, D.M.; Endres, L.; Nistor-Cseppento, D.C.; Popescu, M.I. Acute Coronary Syndromes in Chronic Kidney Disease: Clinical and Therapeutic Characteristics. Med. Lith. 2020, 56, 118. [Google Scholar] [CrossRef] [Green Version]
- Schiffrin, E.L.; Lipman, M.L.; Mann, J.F. Chronic Kidney Disease: Effects on the cardiovascular system. Circulation 2007, 116, 85–97. [Google Scholar] [CrossRef] [Green Version]
- Sarnak, M.J.; Levey, A.S.; Schoolwerth, A.C.; Coresh, J.; Culleton, B.; Hamm, L.L.; McCullough, P.A.; Kasiske, B.L.; Kelepouris, E.; Klag, M.J.; et al. Kidney Disease as a Risk Factor for Development of Cardiovascular Disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Hypertension 2003, 42, 1050–1065. [Google Scholar] [CrossRef]
- Duncker, D.J.; Koller, A.; Merkus, D.; Canty, J.M. Regulation of Coronary Blood Flow in Health and Ischemic Heart Disease. Prog. Cardiovasc. Dis. 2015, 57, 409–422. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J. Clin. Epidemiol. 2021, 134, 178–189. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef]
- Tucker, B.; Fabbian, F.; Giles, M.; Thuraisingham, R.C.; Raine, A.E.; Baker, L.R. Left ventricular hypertrophy and ambulatory blood pressure monitoring in chronic renal failure. Nephrol. Dial. Transplant. 1997, 12, 724–728. [Google Scholar] [CrossRef] [Green Version]
- Culleton, B.F.; Larson, M.; Wilson, P.W.; Evans, J.C.; Parfrey, P.S.; Levy, D. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int. 1999, 56, 2214–2219. [Google Scholar] [CrossRef] [Green Version]
- Teo, K.; Yusuf, S.; Sleight, P.; Anderson, C.; Mookadam, F.; Ramos, B.; Hilbrich, L.; Pogue, J.; Schumacher, H. Rationale, design, and baseline characteristics of 2 large, simple, randomized trials evaluating telmisartan, ramipril, and their combination in high-risk patients: The Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial/Telmisartan Randomized Assessment Study in ACE Intolerant Subjects with Cardiovascular Disease (ONTARGET/TRANSCEND) trials. Am. Heart J. 2004, 148, 52–61. [Google Scholar] [CrossRef]
- Yusuf, S.; Teo, K.; Anderson, C.S.; Pogue, J.; Dyal, L.; Copland, I.; Schumacher, H.; Dagenais, G.; Sleight, P. Effects of the angiotensin-receptor blocker telmisartan on cardiovascular events in high-risk patients intolerant to angiotensin-converting enzyme inhibitors: A randomised controlled trial. Lancet 2008, 372, 1174–1183. [Google Scholar] [CrossRef]
- Clayton, J.A.; Tannenbaum, C. Reporting Sex, Gender, or Both in Clinical Research? JAMA 2016, 316, 1863–1864. [Google Scholar] [CrossRef] [Green Version]
- Tonelli, M.; Wiebe, N.; Culleton, B.; House, A.; Rabbat, C.; Fok, M.; McAlister, F.; Garg, A.X. Chronic Kidney Disease and Mortality Risk: A Systematic Review. J. Am. Soc. Nephrol. 2006, 17, 2034–2047. [Google Scholar] [CrossRef] [Green Version]
- Mahmoodi, B.K.; Matsushita, K.; Woodward, M.; Blankestijn, P.J.; Cirillo, M.; Ohkubo, T.; Rossing, P.; Sarnak, M.J.; Stengel, B.; Yamagishi, K.; et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without hypertension: A meta-analysis. Lancet 2012, 380, 1649–1661. [Google Scholar] [CrossRef] [Green Version]
- Fox, C.S.; Matsushita, K.; Woodward, M.; Bilo, H.J.; Chalmers, J.; Heerspink, H.J.L.; Lee, B.J.; Perkins, R.M.; Rossing, P.; Sairenchi, T.; et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: A meta-analysis. Lancet 2012, 380, 1662–1673. [Google Scholar] [CrossRef] [Green Version]
- Maizel, J.; Six, I.; Slama, M.; Tribouilloy, C.; Sevestre, H.; Poirot, S.; Giummelly, P.; Atkinson, J.; Choukroun, G.; Andrejak, M.; et al. Mechanisms of Aortic and Cardiac Dysfunction in Uremic Mice With Aortic Calcification. Circulation 2009, 119, 306–313. [Google Scholar] [CrossRef] [Green Version]
- Jankowski, J.; Floege, J.; Fliser, D.; Böhm, M.; Marx, N. Cardiovascular Disease in Chronic Kidney Disease: Pathophysiological Insights and Therapeutic Options. Circulation 2021, 143, 1157–1172. [Google Scholar]
- Fujii, H.; Goto, S.; Fukagawa, M. Role of Uremic Toxins for Kidney, Cardiovascular, and Bone Dysfunction. Toxins 2018, 10, 202. [Google Scholar] [CrossRef] [Green Version]
- Vallianou, N.G.; Mitesh, S.; Gkogkou, A.; Geladari, E. Chronic Kidney Disease and Cardiovascular Disease: Is there Any Relationship? Curr. Cardiol. Rev. 2019, 15, 55–63. [Google Scholar] [CrossRef]
- Schulze, F.; Carter, A.M.; Schwedhelm, E.; Ajjan, R.; Maas, R.; von Holten, R.-A.; Atzler, D.; Grant, P.J.; Böger, R.H. Symmetric dimethylarginine predicts all-cause mortality following ischemic stroke. Atherosclerosis 2010, 208, 518–523. [Google Scholar] [CrossRef]
- Levey, A.S.; El-Nahas, M.; de Jong, P.E.; Coresh, J.; Eckhardt, K.-U.; Kasiske, B.L.; Tonelli, M.; Hemmelgarn, M.; Coresh, J.; Astor, B.C.; et al. Chronic Kidney Disease Prognosis Consortium: Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: A collaborative meta-analysis. Lancet 2010, 375, 2073–2081. [Google Scholar]
- Vesa, C.M.; Popa, L.; Popa, A.R.; Rus, M.; Zaha, A.A.; Bungau, S.; Tit, D.M.; Corb Aron, R.A.; Zaha, D.C. Current Data Regarding the Relationship between Type 2 Diabetes Mellitus and Cardiovascular Risk Factors. Diagnostics 2020, 10, 314. [Google Scholar] [CrossRef]
- Stehouwer, C.D.; Smulders, Y.M. Microalbuminuria and Risk for Cardiovascular Disease: Analysis of Potential Mechanisms. J. Am. Soc. Nephrol. 2006, 17, 2106–2111. [Google Scholar] [CrossRef] [Green Version]
- Chade, A.R.; Lerman, A.; Lerman, L.O. Kidney in Early Atherosclerosis. Hypertension 2005, 45, 1042–1049. [Google Scholar] [CrossRef] [Green Version]
- Charytan, D.; Kuntz, R.E.; Mauri, L.; DeFilippi, C. Distribution of Coronary Artery Disease and Relation to Mortality in Asymptomatic Hemodialysis Patients. Am. J. Kidney Dis. 2007, 49, 409–416. [Google Scholar] [CrossRef]
- Shlipak, M.G.; Heidenreich, P.; Noguchi, H.; Chertow, G.M.; Browner, W.S.; McClellan, M.B. Association of Renal Insufficiency with Treatment and Outcomes after Myocardial Infarction in Elderly Patients. Ann. Intern. Med. 2002, 137, 555. [Google Scholar] [CrossRef] [Green Version]
- Al Suwaidi, M.J.; Reddan, D.N.; Williams, K.; Pieper, K.S.; Harrington, R.A.; Califf, R.M.; Granger, C.B.; Ohman, E.M.; Holmes, J.D.R. Prognostic Implications of Abnormalities in Renal Function in Patients With Acute Coronary Syndromes. Circulation 2002, 106, 974–980. [Google Scholar] [CrossRef] [Green Version]
- Pantea-Roșan, L.R.; Pantea, V.A.; Bungau, S.; Tit, D.M.; Behl, T.; Vesa, C.M.; Bustea, C.; Moleriu, R.D.; Rus, M.; Popescu, M.I.; et al. No-Reflow after PPCI—A Predictor of Short-Term Outcomes in STEMI Patients. J. Clin. Med. 2020, 9, 2956. [Google Scholar] [CrossRef]
- Jurkovitz, C.T.; Abramson, J.L.; Vaccarino, L.V.; Weintraub, W.S.; McClellan, W.M. Association of High Serum Creatinine and Anemia Increases the Risk of Coronary Events: Results from the Prospective Community-Based Atherosclerosis Risk in Communities (ARIC) Study. J. Am. Soc. Nephrol. 2003, 14, 2919–2925. [Google Scholar] [CrossRef] [Green Version]
- Subbiah, A.K.; Chhabra, Y.K.; Mahajan, S. Cardiovascular disease in patients with chronic kidney disease: A neglected subgroup. Hear. Asia 2016, 8, 56–61. [Google Scholar] [CrossRef] [Green Version]
- Ardhanari, S.; Alpert, M.A.; Aggarwal, K. Cardiovascular disease in chronic kidney disease: Risk factors, pathogenesis, and prevention. Adv. Perit. Dial. Conf. Perit. Dial. 2014, 30, 40–53. [Google Scholar]
- Moisi, M.; Vesa, C.M.; Bungau, S.; Tit, D.M.; Corb Aron, R.A.; Bratu, O.; Diaconu, C.C.; Rus, M.; Popescu, M.I. Acute kidney injury incidence and models for mortality prediction in acute coronary syndromes. Rom J. Mil. Med. 2020, 113, 133–140. [Google Scholar]
- Keane, W.F.; Tomassini, J.E.; Neff, D.R. Lipid Abnormalities in Patients with Chronic Kidney Disease: Implications for the Pathophysiology of Atherosclerosis. J. Atheroscler. Thromb. 2013, 20, 123–133. [Google Scholar] [CrossRef] [Green Version]
- Navab, M.; Reddy, S.T.; Van Lenten, B.J.; Fogelman, A.M. HDL and cardiovascular disease: Atherogenic and atheroprotective mechanisms. Nat. Rev. Cardiol. 2011, 8, 222–232. [Google Scholar] [CrossRef]
- Seliger, S.; Weiss, N.S.; Gillen, D.L.; Kestenbaum, B.; Ball, A.; Sherrard, D.J.; Stehman-Breen, C.O. HMG-CoA reductase inhibitors are associated with reduced mortality in ESRD patients. Kidney Int. 2002, 61, 297–304. [Google Scholar] [CrossRef] [Green Version]
- Gheorghe, G.; Toth, P.P.; Bungau, S.; Behl, T.; Ilie, M.; Stoian, A.P.; Bratu, O.G.; Bacalbasa, N.; Rus, M.; Diaconu, C.C. Cardiovascular Risk and Statin Therapy Considerations in Women. Diagnostics 2020, 10, 483. [Google Scholar] [CrossRef]
- Fellström, B.; Holdaas, H.; Jardine, A.; Holme, I.; Nyberg, G.; Fauchald, P.; Grönhagen-Riska, C.; Madsen, S.; Neumayer, H.-H.; Cole, E.; et al. Effect of fluvastatin on renal end points in the Assessment of Lescol in Renal Transplant (ALERT) trial. Kidney Int. 2004, 66, 1549–1555. [Google Scholar] [CrossRef] [Green Version]
- Popa, A.R.; Pusta, C.T.J.; Vesa, C.M.; Bungau, S.; Buhas, C.L.; Sava, C.; Dimulescu, I.A.; Zaha, D.C.; Bustea, C. Prediction Models of Albumin Renal Excretion in Type 2 Diabetes Mellitus Patients. Rev. De Chim. 2019, 70, 3802–3807. [Google Scholar]
- Tonelli, M.; Pfeffer, M.A. Kidney Disease and Cardiovascular Risk. Annu. Rev. Med. 2007, 58, 123–139. [Google Scholar] [CrossRef]
- Lewis, E.J.; Hunsicker, L.G.; Clarke, W.R.; Berl, T.; Pohl, M.A.; Lewis, J.B.; Ritz, E.; Atkins, R.C.; Rohde, R.; Raz, I.; et al. Renoprotective Effect of the Angiotensin-Receptor Antagonist Irbesartan in Patients with Nephropathy Due to Type 2 Diabetes. N. Engl. J. Med. 2001, 345, 851–860. [Google Scholar] [CrossRef] [Green Version]
- Anavekar, N.S.; Gans, D.J.; Berl, T.; Rohde, R.D.; Cooper, W.; Bhaumik, A.; Hunsicker, L.G.; Rouleau, J.-L.; Lewis, J.B.; Rosendorff, C.; et al. Predictors of cardiovascular events in patients with type 2 diabetic nephropathy and hypertension: A case for albuminuria. Kidney Int. 2004, 66, S50–S55. [Google Scholar] [CrossRef] [Green Version]
- Brenner, B.M.; Cooper, M.E.; De Zeeuw, D.; Keane, W.F.; Mitch, W.E.; Parving, H.-H.; Remuzzi, G.; Snapinn, S.M.; Zhang, Z.; Shahinfar, S. Effects of Losartan on Renal and Cardiovascular Outcomes in Patients with Type 2 Diabetes and Nephropathy. N. Engl. J. Med. 2001, 345, 861–869. [Google Scholar] [CrossRef] [Green Version]
- De Zeeuw, D.; Remuzzi, G.; Parving, H.-H.; Keane, W.F.; Zhang, Z.; Shahinfar, S.; Snapinn, S.; Cooper, M.E.; Mitch, W.E.; Brenner, B.M. Albuminuria, a Therapeutic Target for Cardiovascular Protection in Type 2 Diabetic Patients With Nephropathy. Circulation 2004, 110, 921–927. [Google Scholar] [CrossRef] [Green Version]
- Mattock, M.B.; Barnes, D.J.; Viberti, G.; Keen, H.; Burt, D.; Hughes, J.M.; Fitzgerald, A.P.; Sandhu, B.; Jackson, P.G. Microalbuminuria and coronary heart disease in NIDDM: An incidence study. Diabetes 1998, 47, 1786–1792. [Google Scholar] [CrossRef]
- Mann, J.F.; Yi, Q.-L.; Gerstein, H. Albuminuria as a predictor of cardiovascular and renal outcomes in people with known atherosclerotic cardiovascular disease. Kidney Int. 2004, 66, S59–S62. [Google Scholar] [CrossRef] [Green Version]
- Hillege, H.L.; Fidler, V.; Diercks, G.F.; van Gilst, W.; De Zeeuw, D.; Van Veldhuisen, D.J.; Gans, R.; Janssen, W.M.; Grobbee, D.E.; De Jong, P.E. Urinary Albumin Excretion Predicts Cardiovascular and Noncardiovascular Mortality in General Population. Circulation 2002, 106, 1777–1782. [Google Scholar] [CrossRef]
- Gerstein, H.C.; Mann, J.F.E.; Yi, Q.; Zinman, B.; Dinneen, S.; Hoogwerf, B.; Hallé, J.P.; Young, J.; Rashkow, A.; Joyce, C.; et al. Albuminuria and Risk of Cardiovascular Events, Death, and Heart Failure in Diabetic and Nondiabetic Individuals. JAMA 2001, 286, 421–426. [Google Scholar] [CrossRef] [Green Version]
- Klausen, K.; Borch-Johnsen, K.; Feldt-Rasmussen, B.; Jensen, G.; Clausen, P.; Scharling, H.; Appleyard, M.; Jensen, J.S. Very Low Levels of Microalbuminuria Are Associated With Increased Risk of Coronary Heart Disease and Death Independently of Renal Function, Hypertension, and Diabetes. Circulation 2004, 110, 32–35. [Google Scholar] [CrossRef] [Green Version]
- Alam, S.; Siddiqui, M.R. Accelerated atherosclerosis in patients with Chronic Kidney Disease-the role of traditional and non-traditional risk factors. WebmedCentral Medicine 2014, 5, WMC004759. [Google Scholar]
- Menon, V.; Sarnak, M.J. The epidemiology of chronic kidney disease stages 1 to 4 and cardiovascular disease: A high-risk combination. Am. J. Kidney Dis. 2005, 45, 223–232. [Google Scholar] [CrossRef]
- Stenvinkel, P. Interactions between inflammation, oxidative stress, and endothelial dysfunction in end-stage renal disease. J. Ren. Nutr. 2003, 13, 144–148. [Google Scholar] [CrossRef]
- Ares, M.P.S.; Stollenwerk, M.; Olsson, A.; Kallin, B.; Jovinge, S.; Nilsson, J. Decreased inducibility of TNF expression in lipid-loaded macrophages. BMC Immunol. 2002, 3, 13. [Google Scholar] [CrossRef]
- Varadhachary, A.S.; Monestier, M.; Salgame, P. Reciprocal Induction of IL-10 and IL-12 from Macrophages by Low-Density Lipoprotein and Its Oxidized Forms. Cell. Immunol. 2001, 213, 45–51. [Google Scholar] [CrossRef]
- Motojima, M.; Hosokawa, A.; Yamato, H.; Muraki, T.; Yoshioka, T. Uremic toxins of organic anions up-regulate PAI-1 expression by induction of NF-κB and free radical in proximal tubular cells. Kidney Int. 2003, 63, 1671–1680. [Google Scholar] [CrossRef] [Green Version]
- Menon, V.; Gul, A.; Sarnak, M.J. Cardiovascular risk factors in chronic kidney disease. Kidney Int. 2005, 68, 1413–1418. [Google Scholar] [CrossRef] [Green Version]
- Recio-Mayoral, A.; Banerjee, D.; Streather, C.; Kaski, J.C. Endothelial dysfunction, inflammation and atherosclerosis in chronic kidney disease–a cross-sectional study of predialysis, dialysis and kidney-transplantation patients. Atheroscler. 2011, 216, 446–451. [Google Scholar] [CrossRef]
- Ridker, P.M.; MacFadyen, J.; Cressman, M.; Glynn, R.J. Efficacy of Rosuvastatin Among Men and Women With Moderate Chronic Kidney Disease and Elevated High-Sensitivity C-Reactive Protein: A Secondary Analysis From the JUPITER (Justification for the Use of Statins in Prevention–an Intervention Trial Evaluating Rosuvastatin) Trial. J. Am. Coll. Cardiol. 2010, 55, 1266–1273. [Google Scholar] [CrossRef] [Green Version]
- Himmelfarb, J.; Stenvinkel, P.; Ikizler, T.; Hakim, R.M. The elephant in uremia: Oxidant stress as a unifying concept of cardiovascular disease in uremia. Kidney Int. 2002, 62, 1524–1538. [Google Scholar] [CrossRef] [Green Version]
- Vaziri, N.D.; Dicus, M.; Ho, N.D.; Boroujerdi-Rad, L.; Sindhu, R.K. Oxidative stress and dysregulation of superoxide dismutase and NADPH oxidase in renal insufficiency. Kidney Int. 2003, 63, 179–185. [Google Scholar] [CrossRef] [Green Version]
- Pecoits-Filho, R.; Stenvinkel, P.; Marchlewska, A.; Heimburger, O.; Barany, P.; Hoff, C.M.; Holmes, C.J.; Suliman, M.; Lindholm, B.; Schalling, M.; et al. A functional variant of the myeloperoxidase gene is associated with cardiovascular disease in end-stage renal disease patients. Kidney Int. 2003, 63, S172–S176. [Google Scholar] [CrossRef] [Green Version]
- Vallance, P.; Leiper, J. Cardiovascular Biology of the Asymmetric Dimethylarginine: Dimethylarginine Dimethylaminohydrolase Pathway. Arter. Thromb. Vasc. Biol. 2004, 24, 1023–1030. [Google Scholar] [CrossRef]
- Małyszko, J.; Matuszkiewicz-Rowińska, J. Endothelium, asymmetric dimethylarginine, and atherosclerosis in chronic kidney disease. Pol. Arch. Intern. Med. 2018, 128, 145–147. [Google Scholar] [CrossRef] [Green Version]
- Coen, G.; Mantella, D.; Sardella, D.; Beraldi, M.; Ferrari, I.; Pierantozzi, A.; Lippi, B.; Di Giulio, S. Asymmetric dimethylarginine, vascular calcifi- cations and parathyroid hormone serum levels in hemodialysis patients. J. Nephrol. 2009, 22, 616. [Google Scholar]
- Krzanowski, M.; Krzanowska, K.; Gajda, M.; Dumnicka, P.; Kopeć, G.; Guzik, B.; Woziwodzka, K.; Dziewierz, A.; Litwin, J.A.; Sułowicz, W. Asymmetric dimethylarginine represents a precious risk indicator for radial artery calcification in patients with advanced kidney disease. Pol. Arch. Intern. Med. 2018, 128, 157–165. [Google Scholar] [CrossRef] [Green Version]
- London, G. Pathophysiology of cardiovascular damage in the early renal population. Nephrol. Dial. Transplant. 2001, 16, 3–6. [Google Scholar] [CrossRef] [Green Version]
- Hase, H.; Imamura, Y.; Nakamura, R.; Inishi, Y.; Machii, K.; Maguchi, T. Effects of rHuEPO therapy on exercise capacity in hemodialysis patients with coronary artery disease. Jpn. Circ. J. 1993, 57, 131–137. [Google Scholar] [CrossRef]
- Metivier, F.; Marchais, S.J.; Guerin, A.P.; Pannier, B.; London, G.M. Pathophysiology of anaemia: Focus on the heart and blood vessels. Nephrol. Dial. Transplant. 2000, 15, 14–18. [Google Scholar] [CrossRef] [Green Version]
- Amann, K.; Breitbach, M.; Ritz, E.; Mall, G. Myocyte/capillary mismatch in the heart of uremic patients. J. Am. Soc. Nephrol. 1998, 9, 1018–1022. [Google Scholar] [CrossRef]
- Besarab, A.; Bolton, W.K.; Nissenson, A.R.; Schwab, S.J.; Goodkin, D.A. The Normal Haematocrit Trial in dialysis patients with cardiac disease. Nephrol. Dial. Transplant. 1999, 14, 2043–2044. [Google Scholar] [CrossRef] [Green Version]
- Foley, R.N.; Parfrey, P.S.; Morgan, J.; Barré, P.E.; Campbell, P.; Cartier, P.; Coyle, D.; Fine, A.; Handa, P.; Kingma, I.; et al. Effect of hemoglobin levels in hemodialysis patients with asymptomatic cardiomyopathy. Kidney Int. 2000, 58, 1325–1335. [Google Scholar] [CrossRef] [Green Version]
- Simons, P.; Algra, A.; Van De Laak, M.; Grobbee, D.; Van Der Graaf, Y. Second Manifestations of ARTerial disease (SMART) study: Rationale and design. Eur. J. Epidemiol. 1999, 15, 773–781. [Google Scholar] [CrossRef]
- Marchais, S.J.; Guerin, A.P.; Pannier, B. Arterial Stiffness: Pathophysiology and Clinical Impact. Clin. Exp. Hypertens. 2004, 26, 689–699. [Google Scholar] [CrossRef]
- Kanbay, M.; Afsar, B.; Gusbeth-Tatomir, P.; Covic, A. Arterial stiffness in dialysis patients: Where are we now? Int. Urol. Nephrol. 2009, 42, 741–752. [Google Scholar] [CrossRef]
- Drüeke, T.B.; Massy, Z.A. Atherosclerosis in CKD: Differences from the general population. Nat. Rev. Nephrol. 2010, 6, 723–735. [Google Scholar] [CrossRef]
- Moisi, M.I.; Vesa, C.; Rosan, L.P.; Tica, O.; Ardelean, A.; Zaha, D.; Burta, O.; Popescu, M.I. Atherosclerosis Burden and Therapeutic Challenges Regarding Acute Coronary Syndromes in Chronic Kidney Disease Patients. Maedica 2019, 14, 378–383. [Google Scholar]
- Schwarz, U.; Buzello, M.; Ritz, E.; Stein, G.; Raabe, G.; Wiest, G.; Mall, G.; Amann, K. Morphology of coronary atherosclerotic lesions in patients with end-stage renal failure. Nephrol. Dial. Transplant. 2000, 15, 218–223. [Google Scholar] [CrossRef] [Green Version]
- Budoff, M.J.; Rader, D.J.; Reilly, M.; Mohler, E.R.; Lash, J.; Yang, W.; Rosen, L.; Glenn, M.; Teal, V.; Feldman, H.I. Relationship of Estimated GFR and Coronary Artery Calcification in the CRIC (Chronic Renal Insufficiency Cohort) Study. Am. J. Kidney Dis. 2011, 58, 519–526. [Google Scholar] [CrossRef] [Green Version]
- Qunibi, W.Y. Reducing the Burden of Cardiovascular Calcification in Patients with Chronic Kidney Disease. J. Am. Soc. Nephrol. 2005, 16, S95–S102. [Google Scholar] [CrossRef] [Green Version]
- Ketteler, M.; Schlieper, G.R.; Floege, J. Calcification and Cardiovascular Health: New insights into an old phenomenon. Hypertension 2006, 47, 1027–1034. [Google Scholar] [CrossRef]
- Johnson, R.C.; Leopold, J.A.; Loscalzo, J. Vascular Calcification: Pathobiological mechanisms and clinical implications. Circ. Res. 2006, 99, 1044–1059. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, J.L.; Joannides, A.J.; Skepper, J.N.; McNair, R.; Schurgers, L.J.; Proudfoot, D.; Jahnen-Dechent, W.; Weissberg, P.L.; Shanahan, C.M. Human Vascular Smooth Muscle Cells Undergo Vesicle-Mediated Calcification in Response to Changes in Extracellular Calcium and Phosphate Concentrations: A Potential Mechanism for Accelerated Vascular Calcification in ESRD. J. Am. Soc. Nephrol. 2004, 15, 2857–2867. [Google Scholar] [CrossRef] [Green Version]
- Russo, D.; Palmiero, G.; De Blasio, A.P.; Balletta, M.M.; Andreucci, V.E. Coronary artery calcification in patients with CRF not undergoing dialysis. Am. J. Kidney Dis. 2004, 44, 1024–1030. [Google Scholar] [CrossRef]
- Hruska, K.A.; Mathew, S.; Saab, G. Bone Morphogenetic Proteins in Vascular Calcification. Circ. Res. 2005, 97, 105–114. [Google Scholar] [CrossRef] [Green Version]
- Takeda, S.; Elefteriou, F.; Levasseur, R.; Liu, X.; Zhao, L.; Parker, K.L.; Armstrong, D.; Ducy, P.; Karsenty, G. Leptin Regulates Bone Formation via the Sympathetic Nervous System. Cell 2002, 111, 305–317. [Google Scholar] [CrossRef] [Green Version]
- Vlagopoulos, P.T.; Tighiouart, H.; Weiner, D.E.; Griffith, J.; Pettitt, D.; Salem, D.N.; Levey, A.S.; Sarnak, M.J. Anemia as a Risk Factor for Cardiovascular Disease and All-Cause Mortality in Diabetes: The Impact of Chronic Kidney Disease. J. Am. Soc. Nephrol. 2005, 16, 3403–3410. [Google Scholar] [CrossRef] [Green Version]
- Sarnak, M.J.; Tighiouart, H.; Manjunath, G.; MacLeod, B.; Griffith, J.; Salem, D.; Levey, A.S. Anemia as a risk factor for cardiovascular disease in the atherosclerosis risk in communities (aric) study. J. Am. Coll. Cardiol. 2002, 40, 27–33. [Google Scholar] [CrossRef]
- Collins, A.J.; Li, S.; Peter, W.S.; Ebben, J.; Roberts, T.; Ma, J.Z.; Manning, W. Death, Hospitalization, and Economic Associations among Incident Hemodialysis Patients with Hematocrit Values of 36 to 39%. J. Am. Soc. Nephrol. 2001, 12, 2465–2473. [Google Scholar] [CrossRef]
- Knight, E.L.; Rimm, E.B.; Pai, J.K.; Rexrode, K.M.; Cannuscio, C.C.; Manson, J.E.; Stampfer, M.J.; Curhan, G.C. Kidney dysfunction, inflammation, and coronary events: A prospective study. J. Am. Soc. Nephrol. 2004, 15, 1897–1903. [Google Scholar] [CrossRef] [Green Version]
- Menon, V.; Greene, T.; Wang, X.; Pereira, A.A.; Marcovina, S.M.; Beck, G.J.; Kusek, J.W.; Collins, A.J.; Levey, A.S.; Sarnak, M.J. C-reactive protein and albumin as predictors of all-cause and cardiovascular mortality in chronic kidney disease. Kidney Int. 2005, 68, 766–772. [Google Scholar] [CrossRef] [Green Version]
- Tripepi, G.; Raso, F.M.; Sijbrands, E.; Seck, M.S.; Maas, R.; Boger, R.; Witteman, J.; Rapisarda, F.A.; Malatino, L.; Mallamaci, F.; et al. Inflammation and Asymmetric Dimethylarginine for Predicting Death and Cardiovascular Events in ESRD Patients. Clin. J. Am. Soc. Nephrol. 2011, 6, 1714–1721. [Google Scholar] [CrossRef] [Green Version]
- Jalal, D.; Chonchol, M.; Etgen, T.; Sander, D. C-reactive protein as a predictor of cardiovascular events in elderly patients with chronic kidney disease. J. Nephrol. 2012, 25, 719–725. [Google Scholar] [CrossRef] [Green Version]
- Amdur, R.L.; Feldman, H.I.; Dominic, E.A.; Anderson, A.H.; Beddhu, S.; Rahman, M.; Wolf, M.; Reilly, M.; Ojo, A.; Townsend, R.R.; et al. Use of Measures of Inflammation and Kidney Function for Prediction of Atherosclerotic Vascular Disease Events and Death in Patients With CKD: Findings From the CRIC Study. Am. J. Kidney Dis. 2019, 73, 344–353. [Google Scholar] [CrossRef] [Green Version]
- Ridker, P.M.; MacFadyen, J.G.; Glynn, R.J.; Koenig, W.; Libby, P.; Everett, B.M.; Lefkowitz, M.; Thuren, T.; Cornel, J. Inhibition of Interleukin-1β by Canakinumab and Cardiovascular Outcomes in Patients with Chronic Kidney Disease. J. Am. Coll. Cardiol. 2018, 71, 2405–2414. [Google Scholar] [CrossRef]
- Wang, Z.; Hoy, W.E. Albuminuria and incident coronary heart disease in Australian Aboriginal people. Kidney Int. 2005, 68, 1289–1293. [Google Scholar] [CrossRef] [Green Version]
- Culleton, B.; Hemmelgarn, B.R.; Manns, B.J.; Taub, K.J.; Tonelli, M.; Klarenbach, S.; Jindal, K.K.; Douglas, S.; McLaughlin, K.; Ahmed, S.B.; et al. Relation between kidney function, proteinuria, and adverse outcomes. JAMA 2010, 303, 423–429. [Google Scholar]
- Yuyun, M.F.; Khaw, K.T.; Luben, R.; Welch, A.; Bingham, S.; Day, N.E.; Wareham, N.J. European Prospective Investigation into Cancer in Norfolk (EPIC-Norfolk) population study: Microalbuminuria independently predicts all-cause and cardiovascular mortality in a British population: The European Prospective Investigation into Cancer in Norfolk (EPIC-Norfolk) population study. Int. J. Epidemiol. 2004, 33, 189–198. [Google Scholar]
- Ahmad, Z.; Arab, S.; Khazaai, H.; Hambali, Z. Oxidative stress and its association with cardiovascular disease in chronic renal failure patients. Indian J. Nephrol. 2011, 21, 21–25. [Google Scholar] [CrossRef]
- Meuwese, M.C.; Stroes, E.S.; Hazen, S.L.; van Miert, J.N.; Kuivenhoven, J.A.; Schaub, R.G.; Wareham, N.J.; Luben, R.; Kastelein, J.J.; Khaw, K.-T.; et al. Serum Myeloperoxidase Levels Are Associated With the Future Risk of Coronary Artery Disease in Apparently Healthy Individuals: The EPIC-Norfolk Prospective Population Study. J. Am. Coll. Cardiol. 2007, 50, 159–165. [Google Scholar] [CrossRef] [Green Version]
- London, G.M.; Guérin, A.P.; Marchais, S.J.; Métivier, F.; Pannier, B.; Adda, H. Arterial media calcification in end-stage renal disease: Impact on all-cause and cardiovascular mortality. Nephrol. Dial. Transplant. 2003, 18, 1731–1740. [Google Scholar] [CrossRef]
- Chen, J.; Budoff, M.J.; Reilly, M.; Yang, W.; Rosas, S.E.; Rahman, M.; Zhang, X.; Roy, J.A.; Lustigova, E.; Nessel, L.; et al. Coronary Artery Calcification and Risk of Cardiovascular Disease and Death Among Patients With Chronic Kidney Disease. JAMA Cardiol. 2017, 2, 635–643. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, S.; Ishibashi-Ueda, H.; Niizuma, S.; Yoshihara, F.; Horio, T.; Kawano, Y. Coronary Calcification in Patients with Chronic Kidney Disease and Coronary Artery Disease. Clin. J. Am. Soc. Nephrol. 2009, 4, 1892–1900. [Google Scholar] [CrossRef]
- Wang, X.-R.; Zhang, J.-J.; Xu, X.-X.; Wu, Y.-G. Prevalence of coronary artery calcification and its association with mortality, cardiovascular events in patients with chronic kidney disease: A systematic review and meta-analysis. Ren. Fail. 2019, 41, 244–256. [Google Scholar] [CrossRef]
- As’ habi, A.; Tabibi, H.; Hedayati, M.; Mahdavi-Mazdeh, M.; Nozary-Heshmati, B. Association of malnutrition-inflammation score, dialysis-malnutrition score and serum albumin with novel risk factors for cardiovascular diseases in hemodialysis patients. Ren. Fail. 2015, 37, 113–116. [Google Scholar]
- Pisetkul, C.; Chanchairujira, K.; Chotipanvittayakul, N.; Ong-Ajyooth, L.; Chanchairujira, T. Malnutrition-inflammation score associated with atherosclerosis, inflammation and short-term outcome in hemodialysis patients. J. Med Assoc. Thail. 2010, 93, 147. [Google Scholar]
- Oh, Y.J.; Kim, A.J.; Ro, H.; Chang, J.H.; Lee, H.H.; Chung, W.; Hyun, Y.Y.; Lee, J.; Kim, Y.H.; Han, S.H.; et al. Low-dose aspirin was associated with an increased risk of cardiovascular events in patients with chronic kidney disease patients and low bodyweight: Results from KNOW-CKD study. Sci. Rep. 2021, 11, 1–10. [Google Scholar] [CrossRef]
- Ethier, J.; Bragg-Gresham, J.L.; Piera, L.; Akizawa, T.; Asano, Y.; Mason, N.; Gillespie, B.W.; Young, E.W. Aspirin Prescription and Outcomes in Hemodialysis Patients: The Dialysis Outcomes and Practice Patterns Study (DOPPS). Am. J. Kidney Dis. 2007, 50, 602–611. [Google Scholar] [CrossRef]
- James, S.; Budaj, A.; Aylward, P.; Buck, K.K.; Cannon, C.P.; Cornel, J.; Harrington, R.A.; Horrow, J.; Katus, H.; Keltai, M.; et al. Ticagrelor Versus Clopidogrel in Acute Coronary Syndromes in Relation to Renal Function: Results from the Platelet Inhibition and Patient Outcomes (PLATO) trial. Circulation 2010, 122, 1056–1067. [Google Scholar] [CrossRef] [Green Version]
- Sciahbasi, A.; Rizzello, V.; Gonzini, L.; Giampaoli, S.; Greco, C.; Di Pasquale, G.; Mureddu, G.F.; Di Chiara, A.; Lioy, E.; Boccanelli, A. Chronic aspirin and statin therapy in patients with impaired renal function and acute coronary syndromes: Results from the IN-ACS Outcome Registry. Eur. J. Prev. Cardiol. 2014, 21, 214–221. [Google Scholar] [CrossRef]
- De Filippo, O.; D’Ascenzo, F.; Raposeiras-Roubin, S.; Abu-Assi, E.; Peyracchia, M.; Bocchino, P.P.; Kinnaird, T.; Ariza-Solé, A.; Liebetrau, C.; Manzano-Fernández, S. P2Y12 inhibitors in acute coronary syndrome patients with renal dysfunction: An analysis from the RENAMI and BleeMACS projects. Eur. Heart J. Cardiovasc. Pharmacother. 2020, 6, 31–42. [Google Scholar]
- Bonello, L.; Laine, M.; Lemesle, G.; Puymirat, E.; Dabry, T.; Thuny, F.; Paganelli, F.; Aradi, D.; Frere, C.; Burtey, S.; et al. Meta-Analysis of Potent P2Y12-ADP Receptor Antagonist Therapy Compared to Clopidogrel Therapy in Acute Coronary Syndrome Patients with Chronic Kidney Disease. Thromb. Haemost. 2018, 118, 1839–1846. [Google Scholar] [CrossRef]
- Wang, H.; Qi, J.; Li, Y.; Tang, Y.; Li, C.; Li, J.; Han, Y. Pharmacodynamics and pharmacokinetics of ticagrelor vs. clopidogrel in patients with acute coronary syndromes and chronic kidney disease. Br. J. Clin. Pharmacol. 2017, 84, 88–96. [Google Scholar] [CrossRef] [Green Version]
- Mavrakanas, T.A.; Kamal, O.; Charytan, D.M. Prasugrel and Ticagrelor in Patients with Drug-Eluting Stents and Kidney Failure. Clin. J. Am. Soc. Nephrol. 2021, 16, 757–764. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar]
- Stub, D.; Smith, K.; Bernard, S.; Nehme, Z.; Stephenson, M.; Bray, J.; Cameron, P.; Barger, B.; Ellims, A.H.; Taylor, A.; et al. Air Versus Oxygen in ST-Segment–Elevation Myocardial Infarction. Circulation 2015, 131, 2143–2150. [Google Scholar] [CrossRef] [Green Version]
- Babes, E.; Zaha, D.; Tit, D.; Nechifor, A.; Bungau, S.; Andronie-Cioara, F.; Behl, T.; Stoicescu, M.; Munteanu, M.; Rus, M.; et al. Value of Hematological and Coagulation Parameters as Prognostic Factors in Acute Coronary Syndromes. Diagnostics 2021, 11, 850. [Google Scholar] [CrossRef]
- Zeymer, U.; Hohlfeld, T.; Vom Dahl, J.; Erbel, R.; Münzel, T.; Zahn, R.; Roitenberg, A.; Breitenstein, S.; Pap, Á.F.; Trenk, D. Prospective, randomised trial of the time dependent antiplatelet effects of 500 mg and 250 mg acetylsalicylic acid iv and 300 mg po in ACS (ACUTE). Thromb. Haemost. 2017, 117, 625–635. [Google Scholar]
- Tomaniak, M.; Chichareon, P.; Klimczak-Tomaniak, D.; Takahashi, K.; Kogame, N.; Modolo, R.; Wang, R.; Ono, M.; Hara, H.; Gao, C.; et al. Impact of renal function on clinical outcomes after PCI in ACS and stable CAD patients treated with ticagrelor: A prespecified analysis of the GLOBAL LEADERS randomized clinical trial. Clin. Res. Cardiol. 2020, 109, 930–943. [Google Scholar] [CrossRef]
- Tonelli, M.; Isles, C.; Curhan, G.C.; Tonkin, A.; Pfeffer, M.A.; Shepherd, J.; Sacks, F.M.; Furberg, C.; Cobbe, S.M.; Simes, J.; et al. Effect of Pravastatin on Cardiovascular Events in People With Chronic Kidney Disease. Circulation 2004, 110, 1557–1563. [Google Scholar] [CrossRef]
- Rysz, J.; Aronow, W.S.; Stolarek, R.S.; Hannam, S.; Mikhailidis, D.P.; Banach, M. Nephroprotective and clinical potential of statins in dialyzed patients. Expert Opin. Ther. Targets 2009, 13, 541–550. [Google Scholar] [CrossRef]
- Nikolic, D.; Nikfar, S.; Salari, P.; Rizzo, M.; Ray, K.K.; Pencina, M.J.; Mikhailidis, D.P.; Toth, P.P.; Nicholls, S.J.; Rysz, J.; et al. Effects of statins on lipid profile in chronic kidney disease patients: A meta-analysis of randomized controlled trials. Curr. Med. Res. Opin. 2013, 29, 435–451. [Google Scholar] [CrossRef]
- Shibui, T.; Nakagomi, A.; Kusama, Y.; Atarashi, H.; Mizuno, K. Impact of Statin Therapy on Renal Function and Long-Term Prognosis in Acute Coronary Syndrome Patients With Chronic Kidney Disease. Int. Hear. J. 2010, 51, 312–318. [Google Scholar] [CrossRef] [Green Version]
- Natanzon, S.S.; Matetzky, S.; Beigel, R.; Iakobishvili, Z.; Goldenberg, I.; Shechter, M. Statin therapy among chronic kidney disease patients presenting with acute coronary syndrome. Atherosclerosis 2019, 286, 14–19. [Google Scholar] [CrossRef]
- McCullough, P.A.; Sandberg, K.R.; Borzak, S.; Hudson, M.P.; Garg, M.; Manley, H.J. Benefits of aspirin and beta-blockade after myocardial infarction in patients with chronic kidney disease. Am. Heart J. 2002, 144, 226–232. [Google Scholar] [CrossRef]
- Yan, A.T.; Yan, R.T.; Tan, M.; Constance, C.; Lauzon, C.; Zaltzman, J.; Wald, R.; Fitchett, D.; Langer, A.; Goodman, S.G. Treatment and one-year outcome of patients with renal dysfunction across the broad spectrum of acute coronary syndromes. Can. J. Cardiol. 2006, 22, 115–120. [Google Scholar] [CrossRef]
- Chonchol, M.; Benderly, M.; Goldbourt, U. Beta-blockers for coronary heart disease in chronic kidney disease. Nephrol. Dial. Transplant. 2008, 23, 2274–2279. [Google Scholar] [CrossRef] [Green Version]
- Berger, A.K.; Duval, S.; Krumholz, H.M. Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. J. Am. Coll. Cardiol. 2003, 42, 201–208. [Google Scholar] [CrossRef] [Green Version]
- Evans, M.; Carrero, J.-J.; Szummer, K.; Åkerblom, A.; Edfors, R.; Spaak, J.; Jacobson, S.H.; Andell, P.; Lindhagen, L.; Jernberg, T. Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers in Myocardial Infarction Patients With Renal Dysfunction. J. Am. Coll. Cardiol. 2016, 67, 1687–1697. [Google Scholar] [CrossRef]
- Cheng, J.; Zhang, W.; Zhang, X.; Han, F.; Li, X.; He, X.; Li, Q.; Chen, J. Effect of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers on All-Cause Mortality, Cardiovascular Deaths, and Cardiovascular Events in Patients With Diabetes Mellitus. JAMA Intern. Med. 2014, 174, 773–785. [Google Scholar] [CrossRef] [Green Version]
- McCullough, P.A.; Sandberg, K.R.; Yee, J.; Hudson, M.P. Mortality benefit of angiotensin-converting enzyme inhibitors after cardiac events in patients with end-stage renal disease. J. Renin-Angiotensin-Aldosterone Syst. 2002, 3, 188–191. [Google Scholar] [CrossRef]
- Qin, Y.; Chen, T.; Chen, Q.; Lv, J.Y.; Qi, N.; Wu, C.; He, J. The effect of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker use on mortality in patients with chronic kidney disease: A meta-analysis of observational studies. Pharmacoepidemiol. Drug Saf. 2016, 25, 503–511. [Google Scholar] [CrossRef]
- Danchin, N.; Cucherat, M.; Thuillez, C.; Durand, E.; Kadri, Z.; Steg, P.G. Angiotensin-Converting Enzyme Inhibitors in Patients With Coronary Artery Disease and Absence of Heart Failure or Left Ventricular Systolic Dysfunction: An overview of long-term randomized controlled trials. Arch. Intern. Med. 2006, 166, 787–796. [Google Scholar] [CrossRef] [Green Version]
- Fox, K.A.A.; Antman, E.M.; Montalescot, G.; Agewall, S.; SomaRaju, B.; Verheugt, F.W.A.; Lopez-Sendon, J.; Hod, H.; Murphy, S.A.; Braunwald, E. The impact of renal dysfunction on outcomes in the ExTRACT-TIMI 25 trial. J. Am. Coll. Cardiol. 2007, 49, 2249–2255. [Google Scholar]
- Januzzi, J.L., Jr.; Snapinn, S.M.; DiBattiste, P.M.; Jang, I.-K.; Theroux, P. Benefits and safety of tirofiban among acute coronary syndrome patients with mild to moderate renal insufficiency: Results from the Platelet Receptor Inhibition in Ischemic Syndrome Management in Patients Limited by Unstable Signs and Symptoms (PRISM-PLUS) trial. Circulation 2002, 105, 2361–2366. [Google Scholar]
- Chew, D.P.; Bhatt, D.L.; Kimball, W.; Henry, T.D.; Berger, P.; McCullough, P.A.; Feit, F.; Bittl, J.A.; Lincoff, A. Bivalirudin provides increasing benefit with decreasing renal function: A meta-analysis of randomized trials. Am. J. Cardiol. 2003, 92, 919–923. [Google Scholar] [CrossRef]
- Mehran, R.; Nikolsky, E.; Lansky, A.J.; Kirtane, A.J.; Kim, Y.-H.; Feit, F.; Manoukian, S.; Moses, J.W.; Ebrahimi, R.; Ohman, E.M.; et al. Impact of Chronic Kidney Disease on Early (30-Day) and Late (1-Year) Outcomes of Patients With Acute Coronary Syndromes Treated With Alternative Antithrombotic Treatment Strategies: An ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) Substudy. JACC Cardiovasc. Interv. 2009, 2, 748–757. [Google Scholar] [CrossRef] [Green Version]
- Capricorn, I. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: The CAPRICORN randomised trial. Lancet 2001, 357, 1385–1390. [Google Scholar]
- Washam, J.B.; Herzog, C.A.; Beitelshees, A.L.; Cohen, M.G.; Henry, T.D.; Kapur, N.K.; Mega, J.L.; Menon, V.; Page, R.L.; Newby, L.K. Pharmacotherapy in Chronic Kidney Disease Patients Presenting With Acute Coronary Syndrome: A Scientific Statement From the American Heart Association. Circulation 2015, 131, 1123–1149. [Google Scholar] [CrossRef] [Green Version]
- Wali, R.K.; Iyengar, M.; Beck, G.J.; Chartyan, D.M.; Chonchol, M.; Lukas, M.A.; Cooper, C.; Himmelfarb, J.; Weir, M.R.; Berl, T. Efficacy and safety of carvedilol in treatment of heart failure with chronic kidney disease: A meta-analysis of randomized trials. Circ. Heart Fail. 2011, 4, 18–26. [Google Scholar]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Russ. J. Cardiol. 2021, 26, 4418. [Google Scholar] [CrossRef]
- Ponikowski, P.; Ronco, C.; Anker, S.D. Cardiorenal syndromes–recommendations from clinical practice guidelines: The cardiologist’s view. In Cardiorenal Syndromes in Critical Care; Karger Publishers: London, UK, 2010; Volume 165, pp. 145–152. [Google Scholar]
- Garthwaite, E.; Bhandari, S. The Effects of Angiotensin Converting Enzyme Inhibitors on Potassium Homeostasis in Dialysis Patients with and Without Residual Renal Function. Artif. Organs 2009, 33, 641–647. [Google Scholar] [CrossRef]
- Joy, E.R.; Kurian, J.; Gale, C.P. Comparative effectiveness of primary PCI versus fibrinolytic therapy for ST elevation myocardial infarction: A review of the literature. J. Comp. Eff. Res. 2016, 5, 217–226. [Google Scholar] [CrossRef]
- Zhang, X.; Hu, L.; Zheng, W. Percutaneous Coronary Intervention versus Coronary Artery Bypass Graft in Acute Coronary Syndrome patients with Renal Dysfunction. Sci. Rep. 2018, 8, 2283. [Google Scholar] [CrossRef]
- Chan, W.; Ivanov, J.; Ko, D.; Fremes, S.; Rao, V.; Jolly, S.; Cantor, W.J.; Lavi, S.; Overgaard, C.B.; Ruel, M. Clinical outcomes of treatment by percutaneous coronary intervention versus coronary artery bypass graft surgery in patients with chronic kidney disease undergoing index revascularization in Ontario. Circulation 2015, 8, e001973. [Google Scholar]
- Bangalore, S.; Guo, Y.; Samadashvili, Z.; Blecker, S.; Xu, J.; Hannan, E.L. Revascularization in patients with multivessel coronary artery disease and chronic kidney disease: Everolimus-eluting stents versus coronary artery bypass graft surgery. J. Am. Coll. Cardiol. 2015, 66, 1209–1220. [Google Scholar]
- Milojevic, M.; Head, S.J.; Mack, M.J.; Mohr, F.W.; Morice, M.C.; Dawkins, K.D.; Holmes, D.R., Jr.; Serruys, P.W.; Kappetein, A.P. The impact of chronic kidney disease on outcomes following percutaneous coronary interventions versus coronary artery bypass grafting in patients with complex coronary artery disease: Five-year follow-up of SYNTAX trial. EuroIntervention 2018, 14, 102–111. [Google Scholar]
- Giustino, G.; Mehran, R.; Serruys, P.W.; Sabik, J.F.; Milojevic, M.; Simonton, C.A.; Puskas, J.D.; Kandzari, D.E.; Morice, M.-C.; Taggart, D.P. Left main revascularization with PCI or CABG in patients with chronic kidney disease: EXCEL trial. J. Am. Coll. Cardiol. 2018, 72, 754–765. [Google Scholar]
- Chertow, G.M.; Normand, S.-L.T.; McNeil, B.J. “Renalism”: Inappropriately Low Rates of Coronary Angiography in Elderly Individuals with Renal Insufficiency. J. Am. Soc. Nephrol. 2004, 15, 2462–2468. [Google Scholar] [CrossRef] [Green Version]
- Szummer, K.; Lundman, P.; Jacobson, S.H.; Schön, S.; Lindbäck, J.; Stenestrand, U.; Wallentin, L.; Jernberg, T.; Swedeheart, F. Relation between renal function, presentation, use of therapies and in-hospital complications in acute coronary syndrome: Data from the SWEDEHEART register. J. Intern. Med. 2010, 268, 40–49. [Google Scholar] [CrossRef]
- McCullough, P.A. Contrast-Induced Acute Kidney Injury. J. Am. Coll. Cardiol. 2008, 51, 1419–1428. [Google Scholar] [CrossRef] [Green Version]
- Everson, M.; Sukcharoen, K.; Milner, Q. Contrast-associated acute kidney injury. BJA Educ. 2020, 20, 417–423. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron 2012, 120, c179–c184. [Google Scholar] [CrossRef]
- Helgason, D.; Long, T.E.; Helgadottir, S.; Palsson, R.; Sigurdsson, G.H.; Gudbjartsson, T.; Indridason, O.S.; Gudmundsdottir, I.J.; Sigurdsson, M.I. Acute kidney injury following coronary angiography: A nationwide study of incidence, risk factors and long-term outcomes. J. Nephrol. 2018, 31, 721–730. [Google Scholar] [CrossRef]
- Shacham, Y.; Steinvil, A.; Arbel, Y. Acute kidney injury among ST elevation myocardial infarction patients treated by primary percutaneous coronary intervention: A multifactorial entity. J. Nephrol. 2016, 29, 169–174. [Google Scholar] [CrossRef]
- Bagshaw, S.M.; George, C.; Bellomo, R. Early acute kidney injury and sepsis: A multicentre evaluation. Crit. Care 2008, 12, R47. [Google Scholar] [CrossRef] [Green Version]
- Chaumont, M.; Pourcelet, A.; Nuffelen, M.; Racapé, J.; Leeman, M.; Hougardy, J. Acute Kidney Injury in Elderly Patients With Chronic Kidney Disease: Do Angiotensin-Converting Enzyme Inhibitors Carry a Risk? J. Clin. Hypertens. 2016, 18, 514–521. [Google Scholar] [CrossRef] [Green Version]
- Brown, J.R.; Robb, J.F.; Block, C.A.; Schoolwerth, A.C.; Kaplan, A.V.; O’Connor, G.T.; Solomon, R.J.; Malenka, D.J. Does Safe Dosing of Iodinated Contrast Prevent Contrast-Induced Acute Kidney Injury? Circ. Cardiovasc. Interv. 2010, 3, 346–350. [Google Scholar] [CrossRef] [Green Version]
- Keaney, J.J.; Hannon, C.M.; Murray, P.T. Contrast-induced acute kidney injury: How much contrast is safe? Nephrol. Dial. Transplant. 2013, 28, 1376–1383. [Google Scholar] [CrossRef] [Green Version]
- Andreucci, M.; Faga, T.; Pisani, A.; Sabbatini, M.; Michael, A. Acute Kidney Injury by Radiographic Contrast Media: Pathogenesis and Prevention. BioMed Res. Int. 2014, 2014, 362725. [Google Scholar] [CrossRef]
- Kuźma, Ł.; Małyszko, J.; Kurasz, A.; Niwińska, M.M.; Zalewska-Adamiec, M.; Bachórzewska-Gajewska, H.; Dobrzycki, S. Impact of renal function on patients with acute coronary syndromes: 15,593 patient-years study. Ren. Fail. 2020, 42, 881–889. [Google Scholar] [CrossRef]
- Cheng, W.; Wu, X.; Liu, Q.; Wang, H.-S.; Zhang, N.-Y.; Xiao, Y.-Q.; Yan, P.; Li, X.-W.; Duan, X.-J.; Peng, J.-C.; et al. Post-contrast acute kidney injury in a hospitalized population: Short-, mid-, and long-term outcome and risk factors for adverse events. Eur. Radiol. 2020, 30, 3516–3527. [Google Scholar] [CrossRef] [Green Version]
- Weisbord, S.D.; Gallagher, M.; Jneid, H.; Garcia, S.; Cass, A.; Thwin, S.-S.; Conner, T.A.; Chertow, G.M.; Bhatt, D.L.; Shunk, K.; et al. Outcomes after Angiography with Sodium Bicarbonate and Acetylcysteine. N. Engl. J. Med. 2018, 378, 603–614. [Google Scholar] [CrossRef]
- National Clinical Guideline Centre. National Clinical Guideline Centre. National Institute for Health and Clinical Excellence: Guidance. In Acute Kidney Injury: Prevention, Detection and Management up to the Point of Renal Replacement Therapy, Royal College of Physicians (UK) Copyright © 2013; National Clinical Guideline Centre: London, UK, 2013. [Google Scholar]
- Abdel-Daim, M.M.; Abo-El-Sooud, K.; Aleya, L.; Bungǎu, S.G.; Najda, A.; Saluja, R. Alleviation of Drugs and Chemicals Toxicity: Biomedical Value of Antioxidants. Oxidative Med. Cell. Longev. 2018, 2018, 1–2. [Google Scholar] [CrossRef]
- Bangalore, S.; Maron, D.J.; O’Brien, S.M.; Fleg, J.L.; Kretov, E.I.; Briguori, C.; Kaul, U.; Reynolds, H.; Mazurek, T.; Sidhu, M.S.; et al. Management of Coronary Disease in Patients with Advanced Kidney Disease. New Engl. J. Med. 2020, 382, 1608–1618. [Google Scholar] [CrossRef]
- Liu, K.; Li, M.; Li, L.; Wu, B.; Xu, X.; Ge, Y.; Mao, H.; Xing, C. The Effect of Coronary Angiography Timing on Cardiac Surgery Associated Acute Kidney Injury Incidence and Prognosis. Front. Med. 2021, 8. [Google Scholar] [CrossRef]
- Mavrakanas, T.A.; Chatzizisis, Y.S.; Gariani, K.; Kereiakes, D.J.; Gargiulo, G.; Helft, G.; Gilard, M.; Feres, F.; Costa, R.A.; Morice, M.-C.; et al. Duration of Dual Antiplatelet Therapy in Patients with CKD and Drug-Eluting Stents. Clin. J. Am. Soc. Nephrol. 2019, 14, 810–822. [Google Scholar] [CrossRef]
- Rymer, J.A.; Kaltenbach, L.A.; Doll, J.A.; Messenger, J.C.; Peterson, E.D.; Wang, T.Y. Safety of Dual-Antiplatelet Therapy After Myocardial Infarction Among Patients With Chronic Kidney Disease. J. Am. Heart Assoc. 2019, 8, e012236. [Google Scholar] [CrossRef]
- Park, S.; Choi, Y.; Kang, J.; Kim, M.; Geum, M.J.; Kim, S.; Rhie, S. P2Y12 Antiplatelet Choice for Patients with Chronic Kidney Disease and Acute Coronary Syndrome: A Systematic Review and Meta-Analysis. J. Pers. Med. 2021, 11, 222. [Google Scholar] [CrossRef]
- Burlacu, A.; Covic, A. Longer or shorter dual antiplatelet therapy in dialysis patients receiving a coronary drug-eluting stent? A rope game still ongoing. Clin. Kidney J. 2020, 13, 749–752. [Google Scholar] [CrossRef]
- Aiyegbusi, O.L.; Kyte, D.; Cockwell, P.; Anderson, N.; Calvert, M. A patient-centred approach to measuring quality in kidney care: Patient-reported outcome measures and patient-reported experience measures: Patient-reported outcome measures and patient-reported experience measures. Curr. Opin. Nephrol. Hypertens. 2017, 26, 442–449. [Google Scholar] [CrossRef]
- Ohtake, T.; Kobayashi, S. Impact of vascular calcification on cardiovascular mortality in hemodialysis patients: Clinical significance, mechanisms and possible strategies for treatment. Ren. Replace. Ther. 2017, 3, 13. [Google Scholar] [CrossRef] [Green Version]
- Franchi, F.; Rollini, F.; Been, L.; Maaliki, N.; Jaoude, P.A.; Rivas, A.; Zhou, X.; Jia, S.; Briceno, M.; Lee, C.H.; et al. Impact of Chronic Kidney Disease on the Pharmacodynamic and Pharmacokinetic Effects of Ticagrelor in Patients with Diabetes Mellitus and Coronary Artery Disease. Eur. Heart J. Cardiovasc. Pharm. 2021, pvab042. [Google Scholar] [CrossRef]
- Chronic Kidney Disease (CKD) Platelet Study. Available online: https://clinicaltrials.gov/ct2/keydates/NCT03649711 (accessed on 15 July 2021).
- Laine, M.; Lemesle, G.; Burtey, S.; Cayla, G.; Range, G.; Quaino, G.; Canault, M.; Pankert, M.; Paganelli, F.; Puymirat, E.; et al. TicagRelor Or Clopidogrel in severe or terminal chronic kidney patients Undergoing PERcutaneous coronary intervention for acute coronary syndrome: The TROUPER trial. Am. Heart J. 2020, 225, 19–26. [Google Scholar] [CrossRef]
- Improving Cardiovascular Health of Patients with Chronic Kidney Disease. Available online: https://www.tracktrial.org/ (accessed on 16 July 2021).
- Garg, A.X.; Suri, R.S.; Eggers, P.; Finkelstein, F.O.; Greene, T.; Kimmel, P.L.; Kliger, A.S.; Larive, B.; Lindsay, R.M.; Pierratos, A.; et al. Patients receiving frequent hemodialysis have better health-related quality of life compared to patients receiving conventional hemodialysis. Kidney Int. 2017, 91, 746–754. [Google Scholar] [CrossRef] [Green Version]

| Number of Patients | Mechanisms Incriminated in Cardiovascular Disease Development | Study Outcome | Findings | Ref. |
|---|---|---|---|---|
| Anemia | ||||
| 3015 | Increased preload Reduced afterload Increased cardiac output | MI; Fatal CHD; Stroke; Death | Interaction between anemia and CKD was statistically significant for all outcomes. | [84] |
| 14,410 | CV disease | Anemia is associated with CV disease and represents an independent predictor for their outcome. | [85] | |
| 67,000 | CV mortality | Decreased levels of hematocrit were associated with high CV mortality | [86] | |
| Inflammation | ||||
| 244 | Decline of the cytokines’ clearance Inflammatory cells recruitment Vascular calcification by transforming endothelial cells into osteoblasts-like cells Acceleration of atherosclerosis | Coronary events | Inflammatory markers predict coronary events in women with CKD | [87] |
| 585 | CV death | Inflammation is an independent predictor of CV mortality in CKD | [88] | |
| 225 | CV events; Death | High ADMA levels are correlated with CV events and death in ESRD | [89] | |
| 3905 | Development of vascular events: MI, stroke | High levels of hs-CRP predict vascular events in CKD patients | [90] | |
| 2399 | Prediction of CV disease occurrence; Death | Inflammation is an independent predictor of CV disease development and death in CKD | [91] | |
| 10,000 | Major CV events; CV death; All-cause mortality | Improved outcome in CKD patients using an inhibitor of interleukin-1β | [92] | |
| Proteinuria and Microalbuminuria | ||||
| 870 | Association with increased production of adhesion molecules Promotes endothelial dysfunction | CAD | Micro and macroalbuminuria represents independent predictors for CAD development | [93] |
| 920,985 | All-cause mortality; MI; Progression of kidney function decline | High values of proteinuria are independently associated with the mentioned outcomes | [94] | |
| 25,112 | Fatal and stable CAD | Microalbuminuria is useful in detecting subjects with high risk of CAD development | [95] | |
| 9043 | CV events (MI, stroke, CV death) | All the degrees of albuminuria predict CV events occurrence in subjects with or without DM | [46] | |
| Oxidative Stress and Endothelial Disfunction | ||||
| 173 | Reactive oxygen species reduces the available nitric oxide There is an enhancement of phagocytic cells infiltration in the vascular wall | Correlation between oxidative stress markers and CV disorders in subject with and without CKD | Markers of oxidative stress influence CV disease appearance in CKD | [96] |
| 3375 | Correlation between myeloperoxidase and CAD development | The mentioned oxidative stress marker predicts CAD appearance in health subjects | [97] | |
| Vascular Calcification | ||||
| 202 | Vascular calcification expresses similar characteristic with osteogenesis Disbalance between promoters and inhibitors of vascular calcification, favorizing the promoters Increased arterial stiffness Impaired coronary artery perfusion | CV and all-cause mortality | Arterial calcification represents an independent predictor of CV mortality | [98] |
| 2069 | CV disease development All-cause mortality | Coronary artery calcification is strongly related with CV disorders, especially MI and all-cause mortality in CKD | [99] | |
| 117 | Coronary artery calcification burden in CAD using autopsy cases | Different types of coronary artery calcification are correlated with the uremic RF, especially medial calcification | [100] | |
| 17,222 | CV mortality CV events | Coronary artery calcification is an independent predictor of CV events and mortality in CKD patients | [101] | |
| Malnutrition | ||||
| 291 | Association with an important inflammatory status The most important consequences are hypoalbuminemia and dyslipidemia | CV disease risk | Strong correlation between malnutrition and CV disease occurrence | [102] |
| 100 | Atherosclerosis and mortality | Inflammation-malnutrition score is useful for atherosclerosis and negative outcome prediction | [103] | |
| Design/No. of Subjects | CKD Stage | Type of ACS | Treatment Group/Control Group | Efficacy | Ref. |
|---|---|---|---|---|---|
| Antiplatelets | |||||
| Prospective *, **/2070 | CKD stages 1 to 5 | With or without CAD | Low-dose aspirin users/Aspirin non-users | Beneficial effect in reducing CV events /mortality; no significant increasing of bleeding risk in subjects with previous cardiac disorders; recommended for secondary prevention. | [104] |
| Sub analysis **/28,320 | ESRD | With or without CAD | Aspirin users/Aspirin non-users | No improvements in prevention of CV mortality/cardiac events, potential benefits in strokes prevention; no increase of bleeding risk. | [105] |
| Sub analysis **/3237 | CKD stages 1 to 5 | STEMINSTEMI | Ticagrelor/Clopidogrel | In patients with both ACS and CKD, ticagrelor (vs. clopidogrel) significantly decreases ischemic endpoints, respectively mortality, without a major bleeding risk, but involving much more minor bleedings events. | [106] |
| Sub analysis **/1484 | Moderate GFR | AMI | Statins + aspirin/Aspirin alone or no treatment | Chronic treatment with statin or the combination of aspirin + statin was associated with reduced in-hospital mortality and better results, both in the short and long term. | [107] |
| Sub analysis **/2490 | CKD stages 1 to 5 | All typed of ACS | Potent P2Y12 inhibitor (Prasugrel or ticagrelor) /Clopidogrel | Ticagrelor vs. clopidogrel or prasugrel decreases the recurrence of MI as well as mortality (occurring from any cause) in subjects with ACS + CKD undergoing PCI. The therapy has been shown to be safe, ensuring the long-term maintenance of the low risk of bleeding. | [108] |
| Meta-analysis **/31,234 | CKD stages 1 to 5 | All typed of ACS | Potent P2Y12 inhibitor (Prasugrel or ticagrelor) /Clopidogrel | In patients suffering of both ACS + CKD, PPAs (vs. clopidogrel) are considered to have a significantly lower incidence of MACE, without increasing the risk of bleeding events. In contrast, in PCI subjects, the beneficial effect of PPAs on MACE has been associated with decreased mortality. | [109] |
| Prospective study **/60 | ≥3 b CKD | NSTE-ACS | Ticagrelor/Clopidogrel | In patients with CKD and NSTE—ACS, ticagrelor proved an increased potent platelet inhibition vs. clopidogrel | [110] |
| Sub analysis **/2171 | CKD stages 1 to 5 | ACS and stable CAD | 1-month DAPTTicagrelor monotherapy (23 months)/12 months DAPT12 months aspirin | In patients with CKD treated with ticagrelor monotherapy, no differential therapeutical side effects were found related to all-cause death/new Q-wave AMI after PCI | [116] |
| Retrospective study/7718 | ESRD | ACS and stable CAD | Prasugrel or ticagrelor/Clopidogrel | In patients with ESRD managed with drug-eluting stents, it was observed that ticagrelor or prasugrel (vs. clopidogrel) cannot be associated with relevant benefits | [111] |
| Statins | |||||
| Sub analysis**/4491 | Moderate CKD | With or without CAD | Pravastatin/Placebo | In patients with/at risk for coronary disease + moderate CKD, pravastatin decreases CV event rates | [117] |
| Prospective study *, **/1255 | ESRD | With or without CAD | Atorvastatin/Placebo | No significant difference in the CV events rate/total mortality in the therapy group | [118] |
| Meta-analysis *, **/3594 | CKD 1 to 5 | With or without CAD | Statins/Placebo | In patients with non-dialysis CKD, statin treatment significantly alters the lipid profile; also, a less beneficial effect was observed in dialysis patients, the long-term therapy being less effective. | [119] |
| Retrospective study **/510 | CKD 1 to 4 | ACS | Statins/Placebo | In patients with ACS + CKD, statin therapy significantly reduced CV events. | [120] |
| Sub analysis **/8945 | CKD 1 to 4 | ACS | Statins/Placebo | In patients with ACS + CKD, it was observed that the beneficial effect of statins was maintained. | [121] |
| β-Blockers | |||||
| Prospective study **/1724 | CKD 1 to 4 | ACS | β-Blockers/Placebo | Decreased CV mortality in subjects receiving both β-Blockers. | [122] |
| Prospective study **/3510 | CKD 1 to 4 | ACS | β-Blockers/Placebo | Improving of 1 year survival rate was noticed in subjects receiving β-Blockers regardless of the kidney function status. | [123] |
| Sub analysis **/3075 | CKD 1 to 4 | ACS and stable CAD | β-Blockers/Placebo | AMI rate and sudden cardiac death were reduced due to β-Blockers regardless of the kidney function. | [124] |
| Retrospective study **/146765 | ESRD | ACS | β-Blockers/Placebo | In subjects with ESRD + ACS, β-Blockers reduced the mortality with 22%. | [125] |
| ACE inhibitors/ARB | |||||
| Sub analysis **/64,442 | CKD 1 to 5 | ACS | ACE inhibitors or ARB/Placebo | Reduced mortality and improved outcome in subjects treated with ACE inhibitors or ARB. | [126] |
| Meta-analysis *, **/56,694 | CKD 1 to 4 | With or without CAD | ACE inhibitors or ARB/Placebo | ACE inhibitors had a major contribution in improving CV mortality and CV events, but ARB did not influence those outcomes. | [127] |
| Retrospective study **/527 | ESRD | With or without CAD | ACE inhibitors/Placebo | Reduced mortality in ESRD subjects treated with ACE inhibitors. | [128] |
| Meta-analysis **/81,541 | CKD 1 to 4 | With or without CAD | ACE inhibitors/Placebo | Better survival rate and reduced mortality in subjects using ACE inhibitors. | [129] |
| Meta-analysis **/33,960 | CKD 1 to 4 | CAD | ACE inhibitors/Placebo | ACE inhibitors reduced the mortality and CV events rate in subjects with stable CAD without LV dysfunction. | [130] |
| Anticoagulants | |||||
| Prospective study **/1724 | CKD 1 to 4 | STEMI | UFH/Enoxaparine | Enoxaparine was superior to UFH, but in subjects with severe CKD this effect disappeared, and adverse effects rate was high. | [131] |
| Sub analysis **/1915 | CKD 1 to 4 | NSTEMI | Tirofiban + UFH/Tirofiban Placebo + UFH/UFH Placebo + Tirofiban | Reduced complications of ACS in subjects treated with mild or moderate CKD treated with Tirofiban. | [132] |
| Meta-analysis **/5035 | CKD 1 to 5 | CAD | Bivalirudin/Heparin | Benefits in reducing ischemic and bleeding events in subjects using Bivalirudin. | [133] |
| Sub analysis **/12,939 | CKD 1 to 4 | ACS | Bivalirudin/Heparin + glycoprotein IIb/IIIa inhibitor/Bivalirudin + glycoprotein IIb/IIIa inhibitor | Monotherapy with bivalirudin therapy did not influence the ischemic outcomes, but the bleeding events were lower. | [134] |
| Design/Origin of the Study Population/No. of Subjects/Type of Stent Used/Type of CAD | Patients with | Short/Long Term MACE | Findings | Ref. | |||
|---|---|---|---|---|---|---|---|
| Left Main Disease | 3 Vessels Involvement | ||||||
| PCI; CABG | PCI% | CABG% | p Value | ||||
| Retrospective cohort study/The Second Drug-Eluting Stent Impact on Revascularization Registry/2923/Second generation DES/ACS | 79 (4.2%); 185 (18.1%) | 501 (26.3%); 707 (69.3%) | 1.5/12.2 | 4.4/10.0 | <0.0001/ 0.1124 | The revascularization technique was recognized to be a time sensitive covariate for MACE. In the short term, when compared to CABG, PCI is likely to present a decreased risk for MACE. Risk ratio for PCI compared to CABG grows with time. | [142] |
| Observational study/Cardiac Care Network of Ontario Cardiac Registry/1786/Second generation DES/Stable CAD and ACS | 132 (13.3%); 1108 (36.8%) | 292 (29.3%); 1679 (55.8%) | 13.8/40.3 | 4.0/18,6 | <0.001/ <0.001 | CABG was linked with enhanced early and late clinical results in contrast with PCI using DES in subjects who present CKD subjected to index revascularization. | [143] |
| Observational study/New York State Percutaneous Coronary Intervention Reporting System and the Cardiac Surgery Reporting System registries/5920/Second generation DES/Stable CAD and ACS | 1269 (42.9%); 1367 (46.2%) | - | 29/458 death events | 51/469 death events | 0.01/ 0.40 | PCI was linked to an increased long-term risk of recurrent revascularization and maybe AMI, while CABG was linked with an increased short-term risk of stroke, repeated revascularization or death. | [144] |
| 11/90 stroke events | 50/143 stroke events | <0.0001/ 0.0002 | |||||
| 20/233 AMI events | 15/153 AMI events | 0.40/ <0.0001 | |||||
| Retrospective sub-analysis/Syntax/1638/First generation DES/Stable CAD and ACS | 19 (18.5); 13 (11.7) | 31 (34.4%); 20 (24.5%) | 6.3/37.3 | 4.0/25.1 | 0.34/ <0.001 | After PCI, the negative influence of CKD on long-term results seems to be enhanced in contrast with CABG, particularly in CKD subjects with extensive CAD and diabetes. | [145] |
| Retrospective sub-analysis/Excel/361/Second generation DES/Stable CAD and ACS | 177; 184 | 64 | 19/40 | 54/33 | <0.0001/ <0.001 | No differences between the PCI or CABG for the components of death or primary composite endpoint, stroke, or AMI at 3 years even though PCI was linked with considerably decreased short-term MACE in contrast to CABG. PCI and CABG are both indicated in elected high-risk patients with CKD and LMCAD. | [146] |
| Criteria | Ref. | ||
|---|---|---|---|
| Definition | The condition can be linked causally to giving contrast media | Serum creatinine increases by ≥26.5 μmol/L within 48 h; Serum creatinine increases by ≥1.5-fold from baseline within 1 week.Urine output <0.5 mL/kg/h of body weight for >6 consecutive hours. | [151] |
| Risk Factors | Individual factors | Age | [152] |
| Diabetes mellitus | |||
| Myocardial infarction | |||
| Chronic kidney disease | |||
| Cardiogenic shock | |||
| Hyponatremia | |||
| Anemia | [153] | ||
| Leukocytosis | [154] | ||
| Previous treatment with renin-angiotensin-blockers | [155] | ||
| Characteristics of the contrast agent | Contrast dose/100 mL | [156,157] | |
| High-osmolality contrast | [158] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moisi, M.I.; Bungau, S.G.; Vesa, C.M.; Diaconu, C.C.; Behl, T.; Stoicescu, M.; Toma, M.M.; Bustea, C.; Sava, C.; Popescu, M.I. Framing Cause-Effect Relationship of Acute Coronary Syndrome in Patients with Chronic Kidney Disease. Diagnostics 2021, 11, 1518. https://doi.org/10.3390/diagnostics11081518
Moisi MI, Bungau SG, Vesa CM, Diaconu CC, Behl T, Stoicescu M, Toma MM, Bustea C, Sava C, Popescu MI. Framing Cause-Effect Relationship of Acute Coronary Syndrome in Patients with Chronic Kidney Disease. Diagnostics. 2021; 11(8):1518. https://doi.org/10.3390/diagnostics11081518
Chicago/Turabian StyleMoisi, Mădălina Ioana, Simona Gabriela Bungau, Cosmin Mihai Vesa, Camelia Cristina Diaconu, Tapan Behl, Manuela Stoicescu, Mirela Mărioara Toma, Cristiana Bustea, Cristian Sava, and Mircea Ioachim Popescu. 2021. "Framing Cause-Effect Relationship of Acute Coronary Syndrome in Patients with Chronic Kidney Disease" Diagnostics 11, no. 8: 1518. https://doi.org/10.3390/diagnostics11081518
APA StyleMoisi, M. I., Bungau, S. G., Vesa, C. M., Diaconu, C. C., Behl, T., Stoicescu, M., Toma, M. M., Bustea, C., Sava, C., & Popescu, M. I. (2021). Framing Cause-Effect Relationship of Acute Coronary Syndrome in Patients with Chronic Kidney Disease. Diagnostics, 11(8), 1518. https://doi.org/10.3390/diagnostics11081518











