Comparison between an Emerging Point-of-Care Tool for TSH Evaluation and a Centralized Laboratory-Based Method in a Cohort of Patients from Southern Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Biochemical Measurements
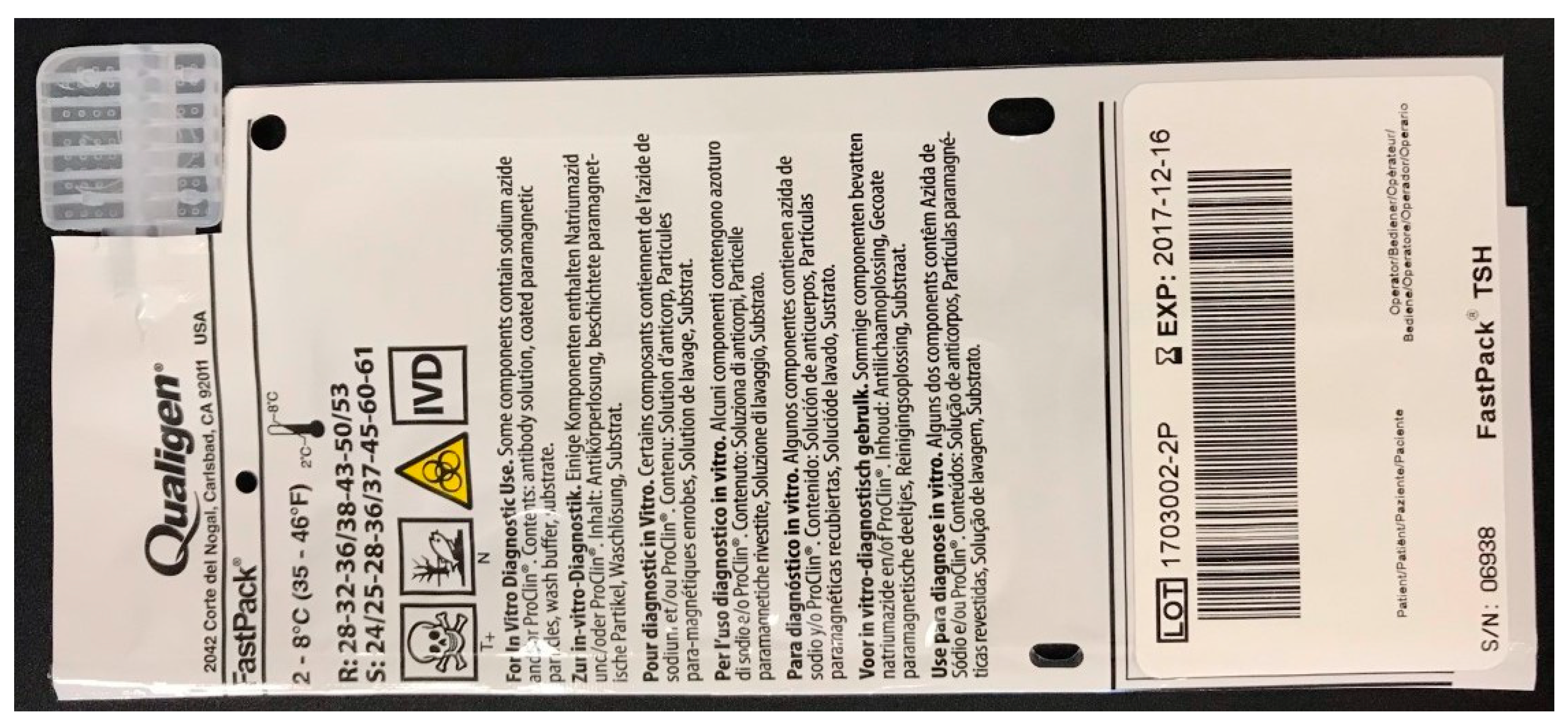
2.2.1. FastPack® IP TSH Immunoassay
2.2.2. Beckman Access 2 TSH Immunoassay
2.3. Instrument Description
2.4. Quality Control
2.5. Study Population
2.6. Questionnaire Data
2.7. Statistical Analysis
3. Results
3.1. Quality Control
3.2. Dilution/Parallelism Assay
3.3. Recovery Test
3.4. Comparison between FastPack® IP and Access 2 TSH Immunoassays
3.5. Study Population
3.6. Prevalence of Goiter
3.7. Questionnaire Data Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Golden, S.H.; Robinson, K.A.; Saldanha, I.; Anton, B.; Ladenson, P.W. Clinical review: Prevalence and incidence of endocrine and metabolic disorders in the United States: A comprehensive review. J. Clin. Endocrinol. Metab. 2009, 94, 1853–1878. [Google Scholar] [CrossRef]
- Garmendia Madariaga, A.; Santos Palacios, S.; Guillen-Grima, F.; Galofre, J.C. The incidence and prevalence of thyroid dysfunction in Europe: A meta-analysis. J. Clin. Endocrinol. Metab. 2014, 99, 923–931. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016, 387, 1513–1530. [Google Scholar] [CrossRef]
- Bolin, K.; Gip, C.; Mork, A.C.; Lindgren, B. Diabetes, healthcare cost and loss of productivity in Sweden 1987 and 2005—A register-based approach. Diabet. Med. 2009, 26, 928–934. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, M.; Arneberg, F.; Line, T.M.; Berg, T.J. Cost of diabetes in Norway 2011. Diabetes Res. Clin. Pract. 2016, 122, 124–132. [Google Scholar] [CrossRef]
- Shrestha, S.S.; Honeycutt, A.A.; Yang, W.; Zhang, P.; Khavjou, O.A.; Poehler, D.C.; Neuwahl, S.J.; Hoerger, T.J. Economic Costs Attributable to Diabetes in Each U.S. State. Diabetes Care 2018, 41, 2526–2534. [Google Scholar] [CrossRef]
- Biener, A.I.; Cawley, J.; Meyerhoefer, C. The medical care costs of obesity and severe obesity in youth: An instrumental variables approach. Health Econ. 2020, 29, 624–639. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.N.; Albrecht, D.; Scholz, A.; Gutierrez-Buey, G.; Lazarus, J.H.; Dayan, C.M.; Okosieme, O.E. Global epidemiology of hyperthyroidism and hypothyroidism. Nat. Rev. Endocrinol. 2018, 14, 301–316. [Google Scholar] [CrossRef] [PubMed]
- Vanderpump, M.P. The epidemiology of thyroid disease. Br. Med. Bull. 2011, 99, 39–51. [Google Scholar] [CrossRef]
- Bluher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.D.; Silverberg, S.J. Primary hyperparathyroidism. Nat. Rev. Endocrinol. 2018, 14, 115–125. [Google Scholar] [CrossRef]
- McClung, M.R.; Miller, P.D.; Papapoulos, S.E. Osteoporosis. In Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism; Wiley: New York, NY, USA, 2018; pp. 393–397. [Google Scholar] [CrossRef]
- Roth, D.E.; Abrams, S.A.; Aloia, J.; Bergeron, G.; Bourassa, M.W.; Brown, K.H.; Calvo, M.S.; Cashman, K.D.; Combs, G.; De-Regil, L.M.; et al. Global prevalence and disease burden of vitamin D deficiency: A roadmap for action in low- and middle-income countries. Ann. N. Y. Acad. Sci. 2018, 1430, 44–79. [Google Scholar] [CrossRef] [PubMed]
- Delange, F. The disorders induced by iodine deficiency. Thyroid 1994, 4, 107–128. [Google Scholar] [CrossRef]
- Kelly, F.C.; Snedden, W.W. Prevalence and geographical distribution of endemic goitre. Bull. World Health Organ. 1958, 18, 5–173. [Google Scholar] [PubMed]
- Delange, F.; Thilly, C.; Ermans, A.M. Iodine deficiency, a permissive condition in the development of endemic goiter. J. Clin. Endocrinol. Metab. 1968, 28, 114–116. [Google Scholar] [CrossRef]
- Gutekunst, R.; Scriba, P.C. Goitre and iodine deficiency in Europe. Report of the Subcommittee for the Study of Endemic Goitre and Iodine Deficiency of the European Thyroid Association. Lancet 1985, 1, 1289–1293. [Google Scholar]
- Gutekunst, R.; Scriba, P.C. Goiter and iodine deficiency in Europe. The European Thyroid Association report as updated in 1988. J. Endocrinol. Investig. 1989, 12, 209–220. [Google Scholar] [CrossRef][Green Version]
- Delange, F. The role of iodine in brain development. Proc. Nutr. Soc. 2000, 59, 75–79. [Google Scholar] [CrossRef]
- Schaffner, M.; Muhlberger, N.; Conrads-Frank, A.; Qerimi Rushaj, V.; Sroczynski, G.; Koukkou, E.; Heinsbaek Thuesen, B.; Volzke, H.; Oberaigner, W.; Siebert, U.; et al. Benefits and Harms of a Prevention Program for Iodine Deficiency Disorders: Predictions of the Decision-Analytic EUthyroid Model. Thyroid 2021, 31, 494–508. [Google Scholar] [CrossRef]
- Kahaly, G.J.; Dienes, H.P.; Beyer, J.; Hommel, G. Iodide induces thyroid autoimmunity in patients with endemic goitre: A randomised, double-blind, placebo-controlled trial. Eur. J. Endocrinol. 1998, 139, 290–297. [Google Scholar] [CrossRef]
- Zois, C.; Stavrou, I.; Kalogera, C.; Svarna, E.; Dimoliatis, I.; Seferiadis, K.; Tsatsoulis, A. High prevalence of autoimmune thyroiditis in schoolchildren after elimination of iodine deficiency in northwestern Greece. Thyroid 2003, 13, 485–489. [Google Scholar] [CrossRef]
- St John, A.; Price, C.P. Existing and Emerging Technologies for Point-of-Care Testing. Clin. Biochem. Rev. 2014, 35, 155–167. [Google Scholar]
- Pezzuto, F.; Scarano, A.; Marini, C.; Rossi, G.; Stocchi, R.; Di Cerbo, A.; Di Cerbo, A. Assessing the Reliability of Commercially Available Point of Care in Various Clinical Fields. Open Public Health J. 2019, 12, 342–368. [Google Scholar] [CrossRef]
- Park, H.S.; Yoo, J.; Lee, H.; Choi, A.R.; Ryu, J.; Park, K.H.; Oh, E.J. Analytical Evaluation of Portable and Simple FREND Fluorescent Immunoassay for Rapid Quantification of Thyroid-Stimulating Hormone and Free Thyroxine. Clin. Lab. 2016, 62, 2455–2460. [Google Scholar] [CrossRef] [PubMed]
- Jung, W.; Han, J.; Kai, J.; Lim, J.Y.; Sul, D.; Ahn, C.H. An innovative sample-to-answer polymer lab-on-a-chip with on-chip reservoirs for the POCT of thyroid stimulating hormone (TSH). Lab Chip 2013, 13, 4653–4662. [Google Scholar] [CrossRef]
- Znoyko, S.L.; Orlov, A.V.; Bragina, V.A.; Nikitin, M.P.; Nikitin, P.I. Nanomagnetic lateral flow assay for high-precision quantification of diagnostically relevant concentrations of serum TSH. Talanta 2020, 216, 120961. [Google Scholar] [CrossRef] [PubMed]
- Yazawa, Y.; Oonishi, T.; Watanabe, K.; Shiratori, A.; Funaoka, S.; Fukushima, M. System-on-fluidics immunoassay device integrating wireless radio-frequency-identification sensor chips. J. Biosci. Bioeng. 2014, 118, 344–349. [Google Scholar] [CrossRef]
- Ylikotila, J.; Valimaa, L.; Vehniainen, M.; Takalo, H.; Lovgren, T.; Pettersson, K. A sensitive TSH assay in spot-coated microwells utilizing recombinant antibody fragments. J. Immunol. Methods 2005, 306, 104–114. [Google Scholar] [CrossRef]
- Sekisuidiagnostics. 2018. Available online: https://sekisuidiagnostics.com/wp-content/uploads/2018/12/FastPack_TSH-Package-Insert-25000042.pdf (accessed on 26 May 2021).
- Tholen, D.W.; Kroll, M.; Astles, J.R.; Caffo, A.L.; Happe, T.M.; Krouwer, J.; Lasky, F. Evaluation of the Linearity of Quantitative Measurement Procedures: A Statistical Approach; Approved Guideline; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2003; Volume 23. [Google Scholar]
- Rodbard, D. Statistical quality control and routine data processing for radioimmunoassays and immunoradiometric assays. Clin. Chem. 1974, 20, 1255–1270. [Google Scholar]
- Harris, E.K. Distinguishing Physiologic Variation from Analytic Variation. J. Chronic Dis. 1970, 23, 469–480. [Google Scholar] [CrossRef]
- Brunn, J.; Block, U.; Ruf, G.; Bos, I.; Kunze, W.P.; Scriba, P.C. [Volumetric analysis of thyroid lobes by real-time ultrasound (author’s transl)]. Dtsch. Med. Wochenschr. 1981, 106, 1338–1340. [Google Scholar] [CrossRef] [PubMed]
- Andreasson, U.; Perret-Liaudet, A.; van Waalwijk van Doorn, L.J.; Blennow, K.; Chiasserini, D.; Engelborghs, S.; Fladby, T.; Genc, S.; Kruse, N.; Kuiperij, H.B.; et al. A Practical Guide to Immunoassay Method Validation. Front. Neurol. 2015, 6, 179. [Google Scholar] [CrossRef] [PubMed]
- Sulejmanovic, M.; Cickusic, A.J.; Salkic, S.; Bousbija, F.M. Annual Incidence of Thyroid Disease in Patients Who First Time Visit Department for Thyroid Diseases in Tuzla Canton. Mater. Socio-Med. 2019, 31, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Hollowell, J.G.; Staehling, N.W.; Flanders, W.D.; Hannon, W.H.; Gunter, E.W.; Spencer, C.A.; Braverman, L.E. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J. Clin. Endocrinol. Metab. 2002, 87, 489–499. [Google Scholar] [CrossRef]
- Helfand, M.; U.S. Preventive Services Task Force. Screening for subclinical thyroid dysfunction in nonpregnant adults: A summary of the evidence for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2004, 140, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.L.; Mandel, S.J.; Weetman, A.P. Disorders of the thyroid gland. In Harrison’s Principles of Internal Medicine, 17th ed.; Fauci, A.S., Kasper, D.L., Longo, D.L., Braunwald, E., Hauser, S.L., Jameson, J.L., Loscalzo, J., Eds.; McGraw-Hill, Medical Pub. Division: New York, NY, USA, 2008. [Google Scholar]
- Surks, M.I.; Ortiz, E.; Daniels, G.H.; Sawin, C.T.; Col, N.F.; Cobin, R.H.; Franklyn, J.A.; Hershman, J.M.; Burman, K.D.; Denke, M.A.; et al. Subclinical thyroid disease: Scientific review and guidelines for diagnosis and management. JAMA 2004, 291, 228–238. [Google Scholar] [CrossRef]
- Rugge, J.B.; Bougatsos, C.; Chou, R. Screening and treatment of thyroid dysfunction: An evidence review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2015, 162, 35–45. [Google Scholar] [CrossRef]
- Odell, W.D.; Wilber, J.F.; Paul, W.E. Radioimmunoassay of thyrotropin in human serum. J. Clin. Endocrinol. Metab. 1965, 25, 1179–1188. [Google Scholar] [CrossRef]
- Jonklaas, J.; Kahric-Janicic, N.; Soldin, O.P.; Soldin, S.J. Correlations of free thyroid hormones measured by tandem mass spectrometry and immunoassay with thyroid-stimulating hormone across 4 patient populations. Clin. Chem. 2009, 55, 1380–1388. [Google Scholar] [CrossRef]
- Ostrowska, M.; Bartoszewicz, Z.; Bednarczuk, T.; Walczak, K.; Zgliczynski, W.; Glinicki, P. The effect of biotin interference on the results of blood hormone assays. Endokrynol. Pol. 2019, 70, 102–121. [Google Scholar] [CrossRef]
- Wang, T.; Sheng, S.; Ruan, M.; Yan, J.; Gu, J.; Jiang, Y.; Gao, Y.; Lu, H. Clinical Evaluation of the Immune Colloidal Gold Method for Rapid Qualitative and Quantitative Measurement of Thyroid-Stimulating Hormone as an Assay for Hypothyroidism. Adv. Ther. 2016, 33, 2001–2011. [Google Scholar] [CrossRef] [PubMed]






| Within-Run Assay | ||||
|---|---|---|---|---|
| Low–Normal TSH Level | Intermediate TSH Level | High TSH Level | High TSH Level | |
| Samples | N = 10 | N = 10 | N = 10 | N = 10 |
| Mean ± SD | 0.70 ± 0.06 | 9.51 ± 0.71 | 39.49 ± 1.59 | 52.59 ± 3.53 |
| CV (%) | 8.57 | 7.47 | 4.03 | 6.71 |
| RSD (%) | 0.70 ± 8.57 | 9.51 ± 7.47 | 39.49 ± 4.03 | 52.59 ± 6.71 |
| Between-Run Assay | ||||
| Control Sample 1 | Control Sample 2 | |||
| Lot# | 2001037 | 2001038 | ||
| Mean * | 0.89 | 23.80 | ||
| Range * | 0.39–1.40 | 15.8–31.8 | ||
| Samples | N = 14 | N = 14 | ||
| Mean ± SD | 0.87 ± 0.09 | 26.55 ± 1.68 | ||
| CV (%) | 10.34 | 6.33 | ||
| RSD (%) | 0.87 ± 10.84 | 26.55 ± 6.33 | ||
| Sample | TSH Added (mIU/L) | TSH Recovered (mIU/L) | Recovery (%) |
|---|---|---|---|
| #1 | 1.09 | 0.97 | 89.0 |
| #2 | 3.26 | 3.07 | 94.2 |
| #3 | 9.77 | 9.67 | 99.0 |
| #4 | 21.1 | 20.4 | 96.7 |
| #5 | 29.3 | 29.8 | 101.7 |
| #6 | 39.4 | 40.2 | 102.0 |
| #7 | 41.2 | 39.6 | 96.1 |
| Patients’ Features | Mean ± SD | Median | Range |
|---|---|---|---|
| Age (yr) | |||
| -All subjects (100) | 52.2 ± 17.3 | 51.5 | 19–90 |
| -Control subjects (25) | 47.8 ± 18.3 | 44 | 19–79 |
| -Hashimoto’s thyroiditis (45) | 51.2 ± 16.7 | 51 | 21–86 |
| -Graves’ disease (6) | 48.3 ± 11.8 | 52.5 | 30–89 |
| -Nodular non-toxic goiter (6) | 56.2 ± 20.3 | 54 | 28–90 |
| -Multinodular non-toxic goiter (15) | 59.1 ± 16.9 | 52 | 23–89 |
| -Papillary thyroid carcinoma (3) | 69.3 ± 11.9 | 73 | 56–79 |
| Sex (F/M) | 68/32 | ||
| Family history of thyroid disease (Y/N) | 41/59 | ||
| Smoker (Y/N) | 22/78 | ||
| Use of iodized salt (Y/N) | 61/39 | ||
| Radiation treatment to head, neck, or chest (Y/N) | 0/100 | ||
| Other autoimmune diseases (Y/N) | 4/96 | ||
| Thyroid volume (mL) | |||
| -All subjects (97) | 16.6 ± 9.1 | 14.0 | 2.4–56.0 |
| -Control subjects (25) | 11.1 ± 3.1 | 11.4 | 5.8–16.2 |
| -Hashimoto’s thyroiditis (45) | 16.3 ± 7.0 | 14.1 | 2.4–35.2 |
| -Graves’ disease (6) | 15.9 ± 8.2 | 18.3 | 4.3–25.7 |
| -Nodular non-toxic goiter (6) | 15.5 ± 9.5 | 10.7 | 8.1–30.4 |
| -Multinodular non-toxic goiter (15) | 27.7 ± 12.4 | 24.8 | 9.9–56.0 |
| -Papillary thyroid carcinoma (3) | NA | NA | NA |
| TSH (mIU/L) | |||
| -All subjects (100) | 3.00 ± 4.29 | 1.85 | 0.22–34.50 |
| -Control subjects (25) | 1.37 ± 0.81 | 1.20 | 0.42–4.20 |
| -Hashimoto’s thyroiditis (45) | 3.72 ± 3.00 | 2.80 | 0.52–34.50 |
| -Graves’ disease (6) | 2.16 ± 1.83 | 3.50 | 0.34–4.60 |
| -Nodular non-toxic goiter (6) | 1.05 ± 0.61 | 1.12 | 0.22–1.70 |
| -Multinodular non-toxic goiter (15) | 1.64 ± 1.13 | 1.60 | 0.30–4.60 |
| -Papillary thyroid carcinoma (3) | 1.80 ± 0.53 | 1.60 | 1.40–2.40 |
| Previous steroid treatment for active Graves’ orbitopathy (Y/N) | 0/6 | ||
| TRAb-positive Graves’ patients (Y/N) | 0/6 | ||
| Recent exposure to iodinated contrast media (Y/N) | 0/100 | ||
| Methimazole-treated Graves’ patients (Y/N) | 6/0 | ||
| LT4-treated Hashimoto’s patients (Y/N) | 17/28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Cerbo, A.; Quagliano, N.; Napolitano, A.; Pezzuto, F.; Iannitti, T.; Di Cerbo, A. Comparison between an Emerging Point-of-Care Tool for TSH Evaluation and a Centralized Laboratory-Based Method in a Cohort of Patients from Southern Italy. Diagnostics 2021, 11, 1590. https://doi.org/10.3390/diagnostics11091590
Di Cerbo A, Quagliano N, Napolitano A, Pezzuto F, Iannitti T, Di Cerbo A. Comparison between an Emerging Point-of-Care Tool for TSH Evaluation and a Centralized Laboratory-Based Method in a Cohort of Patients from Southern Italy. Diagnostics. 2021; 11(9):1590. https://doi.org/10.3390/diagnostics11091590
Chicago/Turabian StyleDi Cerbo, Alfredo, Nazario Quagliano, Antonella Napolitano, Federica Pezzuto, Tommaso Iannitti, and Alessandro Di Cerbo. 2021. "Comparison between an Emerging Point-of-Care Tool for TSH Evaluation and a Centralized Laboratory-Based Method in a Cohort of Patients from Southern Italy" Diagnostics 11, no. 9: 1590. https://doi.org/10.3390/diagnostics11091590
APA StyleDi Cerbo, A., Quagliano, N., Napolitano, A., Pezzuto, F., Iannitti, T., & Di Cerbo, A. (2021). Comparison between an Emerging Point-of-Care Tool for TSH Evaluation and a Centralized Laboratory-Based Method in a Cohort of Patients from Southern Italy. Diagnostics, 11(9), 1590. https://doi.org/10.3390/diagnostics11091590







