A New Anatomical Classification for Tibialis Posterior Tendon Insertion and Its Clinical Implications: A Cadaveric Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Dissection
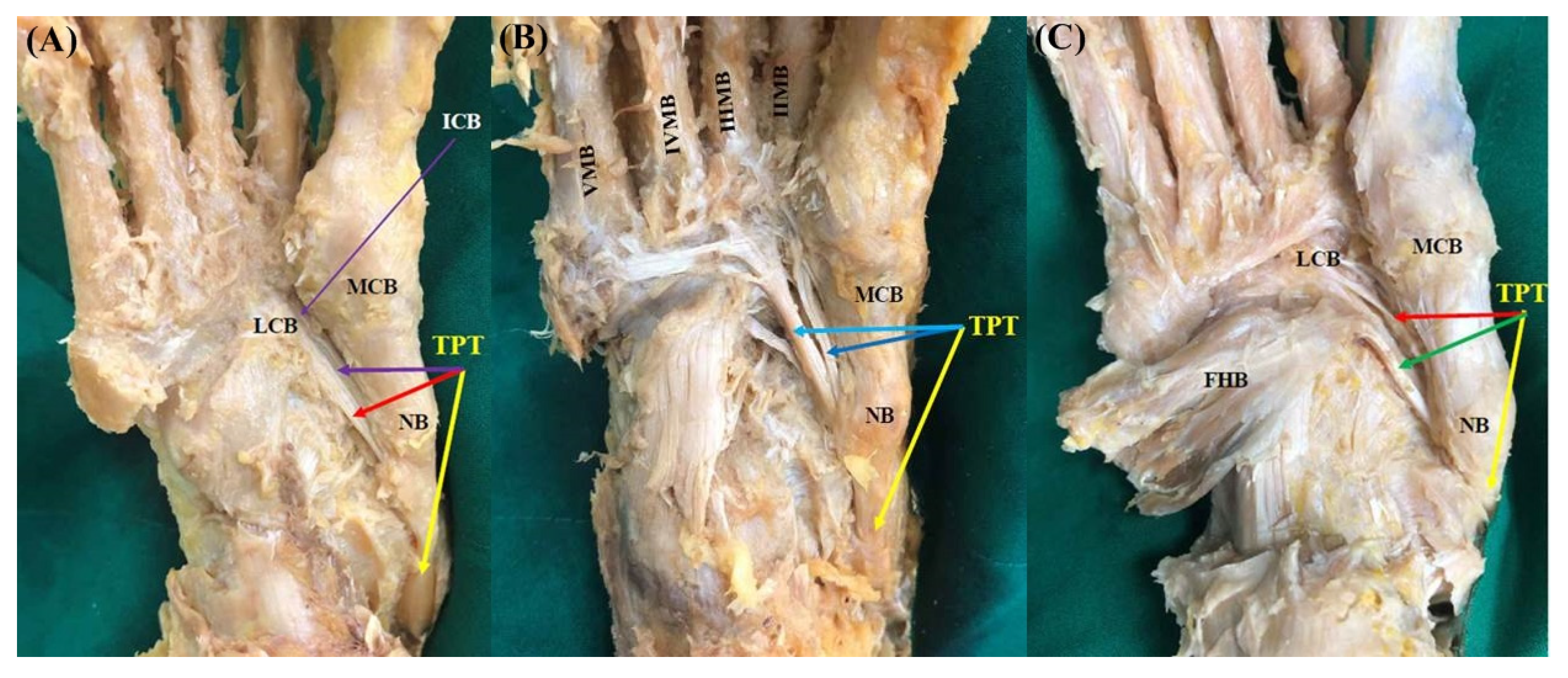
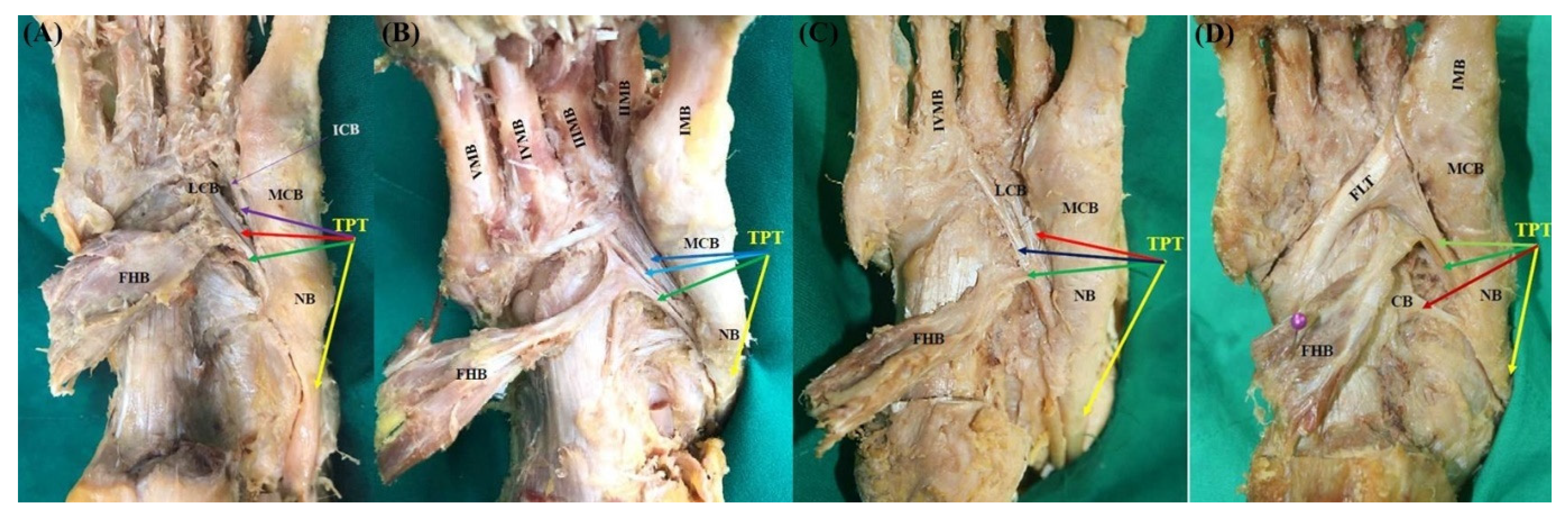
2.2. Assessment of Morphological Characteristics of the TPT Insertion
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johnson, K.A. Tibialis posterior tendon rupture. Clin. Orthop. Relat. Res. 1983, 177, 140–147. [Google Scholar] [CrossRef]
- Johnson, K.A.; Strom, D.E. Tibialis posterior tendon dysfunction. Clin. Orthop. Relat. Res. 1989, 239, 196–206. [Google Scholar] [CrossRef]
- Kohls-Gatzoulis, J.; Angel, J.C.; Singh, D.; Haddad, F.; Livingstone, J.; Berry, G. Tibialis posterior dysfunction: A common and treatable cause of adult acquired flatfoot. BMJ 2004, 329, 1328–1333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mann, R.A. Rupture of the tibialis posterior tendon. Instr. Course Lect. 1984, 33, 302–309. [Google Scholar]
- Mann, R.A. Adult acquired flatfoot deformity. Treatment of dysfunction of the posterior tibial tendon. J. Bone Joint Surg. Am. 1997, 79, 1434. [Google Scholar] [CrossRef]
- Ross, M.H.; Smith, M.; Plinsinga, M.L.; Vicenzino, B. Self-reported social and activity restrictions accompany local impairments in posterior tibial tendon dysfunction: A systematic review. J. Foot Ankle Res. 2018, 11, 49. [Google Scholar] [CrossRef]
- Myerson, M.S.; Badekas, A.; Schon, L.C. Treatment of stage II posterior tibial tendon deficiency with flexor digitorum longus tendon transfer and calcaneal osteotomy. Foot Ankle Int. 2004, 25, 445–450. [Google Scholar] [CrossRef]
- Semple, R.; Murley, G.S.; Woodburn, J.; Turner, D.E. Tibialis posterior in health and disease: A review of structure and function with specific reference to electromyographic studies. J. Foot Ankle Res. 2009, 2, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Basmajian, J.V.; Stecko, G. The Role of Muscles in Arch Support of the Foot. J. Bone Joint Surg. Am. 1963, 45, 1184–1190. [Google Scholar] [CrossRef]
- Mosier, S.M.; Lucas, D.R.; Pomeroy, G.; Manoli, A., 2nd. Pathology of the posterior tibial tendon in posterior tibial tendon insufficiency. Foot Ankle Int. 1998, 19, 520–524. [Google Scholar] [CrossRef]
- Golano, P.; Farinas, O.; Saenz, I. The anatomy of the navicular and periarticular structures. Foot Ankle Clin. 2004, 9, 1–23. [Google Scholar] [CrossRef]
- Lhoste-Trouilloud, A. The tibialis posterior tendon. J. Ultrasound 2012, 15, 2–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bloome, D.M.; Marymont, J.V.; Varner, K.E. Variations on the insertion of the posterior tibialis tendon: A cadaveric study. Foot Ankle Int. 2003, 24, 780–783. [Google Scholar] [CrossRef]
- Kiter, E.; Gunal, I.; Karatosun, V.; Korman, E. The relationship between the tibialis posterior tendon and the accessory navicular. Ann. Anat. 2000, 182, 65–68. [Google Scholar] [CrossRef]
- Olewnik, L. A proposal for a new classification for the tendon of insertion of tibialis posterior. Clin. Anat. 2019, 32, 557–565. [Google Scholar] [CrossRef]
- Swanton, E.; Fisher, L.; Fisher, A.; Molloy, A.; Mason, L. An Anatomic Study of the Naviculocuneiform Ligament and Its Possible Role Maintaining the Medial Longitudinal Arch. Foot Ankle Int. 2019, 40, 352–355. [Google Scholar] [CrossRef]
- Musiał, W. Variations of the terminal insertions of the anterior and posterior tibial muscles in man. Folia Morphol. (Warsaw.) 1963, 22, 294–302. [Google Scholar]
- Willegger, M.; Seyidova, N.; Schuh, R.; Windhager, R.; Hirtler, L. The tibialis posterior tendon footprint: An anatomical dissection study. J. Foot Ankle Res. 2020, 13, 25. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, N.; Jupiter, D.C.; Ciliberti, L.J.; VanBuren, V.; La Fontaine, J. Characteristics of adult flatfoot in the United States. J. Foot Ankle Surg. 2010, 49, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Pita-Fernandez, S.; Gonzalez-Martin, C.; Seoane-Pillado, T.; Lopez-Calvino, B.; Pertega-Diaz, S.; Gil-Guillen, V. Validity of footprint analysis to determine flatfoot using clinical diagnosis as the gold standard in a random sample aged 40 years and older. J. Epidemiol. 2015, 25, 148–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Troiano, G.; Nante, N.; Citarelli, G.L. Pes planus and pes cavus in Southern Italy: A 5 years study. Ann. Ist. Super. Sanita 2017, 53, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Arangio, G.A.; Salathe, E.P. A biomechanical analysis of posterior tibial tendon dysfunction, medial displacement calcaneal osteotomy and flexor digitorum longus transfer in adult acquired flat foot. Clin. Biomech. (Bristol Avon) 2009, 24, 385–390. [Google Scholar] [CrossRef]
- Hui, H.E.; Beals, T.C.; Brown, N.A. Influence of tendon transfer site on moment arms of the flexor digitorum longus muscle. Foot Ankle Int. 2007, 28, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Spratley, E.M.; Arnold, J.M.; Owen, J.R.; Glezos, C.D.; Adelaar, R.S.; Wayne, J.S. Plantar forces in flexor hallucis longus versus flexor digitorum longus transfer in adult acquired flatfoot deformity. Foot Ankle Int. 2013, 34, 1286–1293. [Google Scholar] [CrossRef] [PubMed]
- Vaudreuil, N.J.; Ledoux, W.R.; Roush, G.C.; Whittaker, E.C.; Sangeorzan, B.J. Comparison of transfer sites for flexor digitorum longus in a cadaveric adult acquired flatfoot model. J. Orthop. Res. 2014, 32, 102–109. [Google Scholar] [CrossRef]
- Conti, M.S.; Garfinkel, J.H.; Ellis, S.J. Outcomes of Reconstruction of the Flexible Adult-acquired Flatfoot Deformity. Orthop. Clin. N. Am. 2020, 51, 109–120. [Google Scholar] [CrossRef]
- Johnson, J.E.; Sangeorzan, B.J.; de Cesar Netto, C.; Deland, J.T.; Ellis, S.J.; Hintermann, B.; Schon, L.C.; Thordarson, D.B.; Myerson, M.S. Consensus on Indications for Medial Cuneiform Opening Wedge (Cotton) Osteotomy in the Treatment of Progressive Collapsing Foot Deformity. Foot Ankle Int. 2020, 41, 1289–1291. [Google Scholar] [CrossRef] [PubMed]
- Lewis, O.J. The Tibialis Posterior Tendon in the Primate Foot. J. Anat. 1964, 98, 209–218. [Google Scholar]
- Martin, B.F. Observations on the Muscles and Tendons of the Medial Aspect of the Sole of the Foot. J. Anat. 1964, 98, 437–453. [Google Scholar]
- Kim, J.; Kim, J.B.; Lee, W.C. Dynamic medial column stabilization using flexor hallucis longus tendon transfer in the surgical reconstruction of flatfoot deformity in adults. Foot Ankle Surg. 2020. [Google Scholar] [CrossRef]
- Deland, J.T. Adult-acquired flatfoot deformity. J. Am. Acad. Orthop. Surg. 2008, 16, 399–406. [Google Scholar] [CrossRef] [Green Version]
- Deland, J.T.; Page, A.; Sung, I.H.; O’Malley, M.J.; Inda, D.; Choung, S. Posterior tibial tendon insufficiency results at different stages. HSS J. 2006, 2, 157–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hiller, L.; Pinney, S.J. Surgical treatment of acquired flatfoot deformity: What is the state of practice among academic foot and ankle surgeons in 2002? Foot Ankle Int. 2003, 24, 701–705. [Google Scholar] [CrossRef]




| Age | Male | Female | Total |
|---|---|---|---|
| 41~50 | 4 | 0 | 4 |
| 51~60 | 8 | 2 | 10 |
| 61~70 | 16 | 9 | 25 |
| 71~80 | 20 | 12 | 32 |
| 81~90 | 20 | 20 | 40 |
| 91~100 | 0 | 7 | 7 |
| Total | 68 | 50 | 118 |
| Classification | Type | Subtype | Main Tendon | Accessory Tendons | n (%) |
|---|---|---|---|---|---|
| Olewnik’s study [15] | 1 | NB, MCB | 13 (16.25) | ||
| 2 | NB, MCB | LCB | 18 (22.5) | ||
| 3 | A | NB, MCB | MCB, LCB | 10 (12.5) | |
| B | NB, MCB | ICB, LCB | 20 (25.0) | ||
| C | NB, MCB | II MB, II~V MB | 5 (6.25) | ||
| 4 | A | NB, MCB | PCCL, CB, FHB | 7 (8.8) | |
| B | NB, MCB | LCB, II MB, FHB | 3 (3.7) | ||
| C | NB, MCB | LCB, ICB, I MB + FLT | 4 (5.0) | ||
| Sum | 80 (100) | ||||
| Current study | 1 | NB, MCB | 2 (1.7) | ||
| 2 | NB, MCB | LCB | 13 (11.0) | ||
| 3 | B | NB, MCB | ICB, LCB | 5 (4.3) | |
| C | NB, MCB | II MB, II~V MB | 9 (7.6) | ||
| K | NB, MCB | LCB, FHB | 11 (9.3) | ||
| 4 | K-1 | NB, MCB | ICB, LCB, FHB | 25 (21.2) | |
| K-2 | NB, MCB | II MB, II~V MB, FHB | 38 (32.2) | ||
| K-3 | NB, MCB | LCB, IV MB, FHB | 13 (11.0) | ||
| K-4 | NB, MCB | FLT+ I MB, CB, FHB | 2 (1.7) | ||
| Sum | 118 (100) |
| Olewnik’s Study [15] | Current Study | p Value | ||
|---|---|---|---|---|
| Type | 1 | 13 (16.25) | 2 (1.7) | <0.001 |
| 2 | 18 (22.5) | 13 (11.0) | ||
| 3 | 35 (43.75) | 25 (21.2) | ||
| 4 | 14 (17.5) | 78 (66.1) | ||
| Sum | 80 (100) | 118 (100) |
| Gender | p Value | |||
|---|---|---|---|---|
| Male | Female | |||
| Type | 1 | 0 (0.0) | 2 (4.0) | 0.006 |
| 2 | 11 (16.2) | 2 (4.0) | ||
| 3 | 9 (13.2) | 16 (32.0) | ||
| 4 | 48 (70.6) | 30 (60.0) | ||
| Sum | 68 (100.0) | 50 (100.0) | ||
| Width | Male | Female | p Value |
|---|---|---|---|
| Insertion to navicular bone | 11.60 ± 1.74 | 10.82 ± 1.20 | 0.007 |
| Insertion to medial cuneiform bone | 12.47 ± 2.47 | 11.60 ± 2.16 | 0.057 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-H.; Kim, D.; Kwon, H.-W.; Lee, M.; Choi, Y.-J.; Park, K.-R.; Youn, K.H.; Cho, J. A New Anatomical Classification for Tibialis Posterior Tendon Insertion and Its Clinical Implications: A Cadaveric Study. Diagnostics 2021, 11, 1619. https://doi.org/10.3390/diagnostics11091619
Park J-H, Kim D, Kwon H-W, Lee M, Choi Y-J, Park K-R, Youn KH, Cho J. A New Anatomical Classification for Tibialis Posterior Tendon Insertion and Its Clinical Implications: A Cadaveric Study. Diagnostics. 2021; 11(9):1619. https://doi.org/10.3390/diagnostics11091619
Chicago/Turabian StylePark, Jeong-Hyun, Digud Kim, Hyung-Wook Kwon, Mijeong Lee, Yu-Jin Choi, Kwang-Rak Park, Kwan Hyun Youn, and Jaeho Cho. 2021. "A New Anatomical Classification for Tibialis Posterior Tendon Insertion and Its Clinical Implications: A Cadaveric Study" Diagnostics 11, no. 9: 1619. https://doi.org/10.3390/diagnostics11091619
APA StylePark, J.-H., Kim, D., Kwon, H.-W., Lee, M., Choi, Y.-J., Park, K.-R., Youn, K. H., & Cho, J. (2021). A New Anatomical Classification for Tibialis Posterior Tendon Insertion and Its Clinical Implications: A Cadaveric Study. Diagnostics, 11(9), 1619. https://doi.org/10.3390/diagnostics11091619







