The Predictive Role of NLR, d-NLR, MLR, and SIRI in COVID-19 Mortality
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Variables, Data Sources, and Measurement
2.4. Statistical Analysis
3. Results
3.1. Participants Characteristics
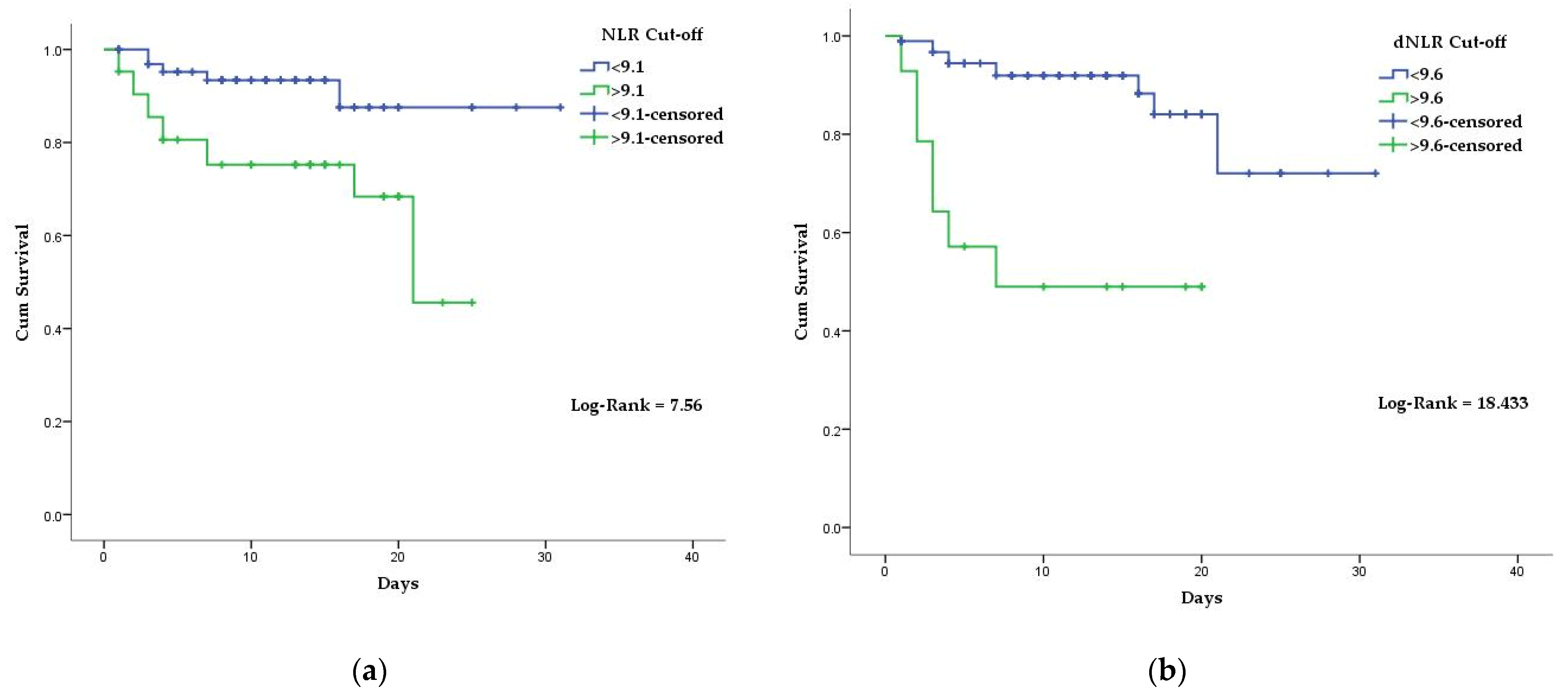
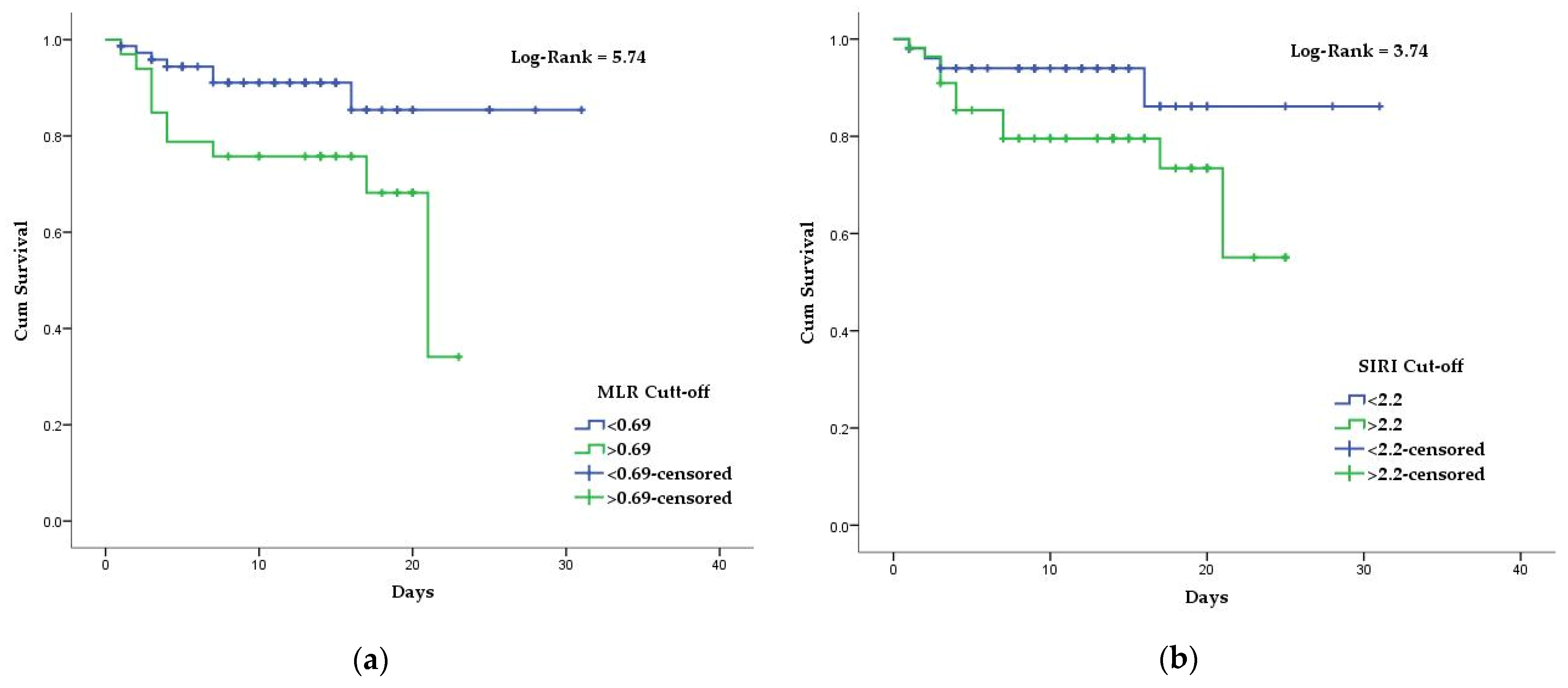
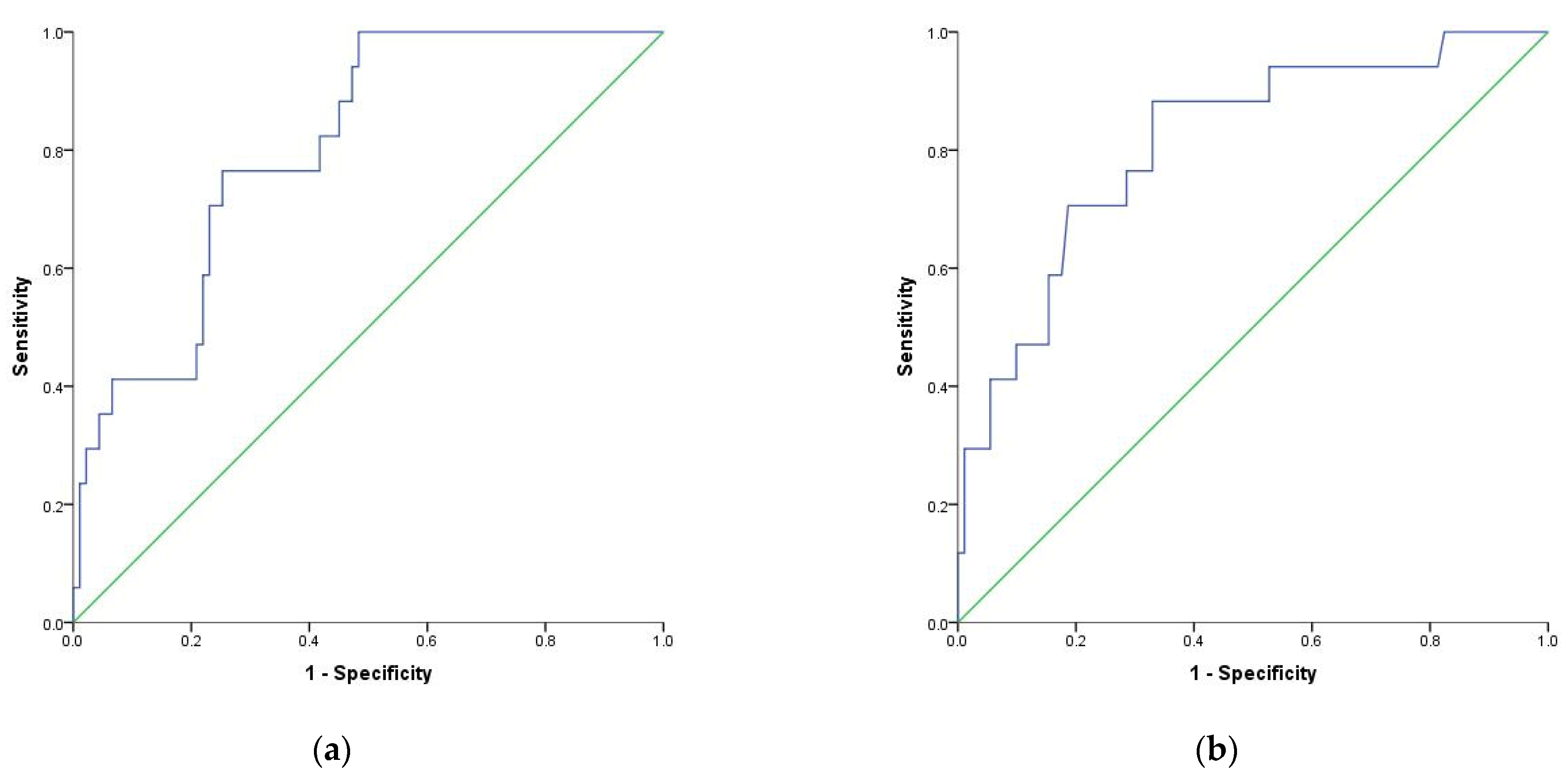
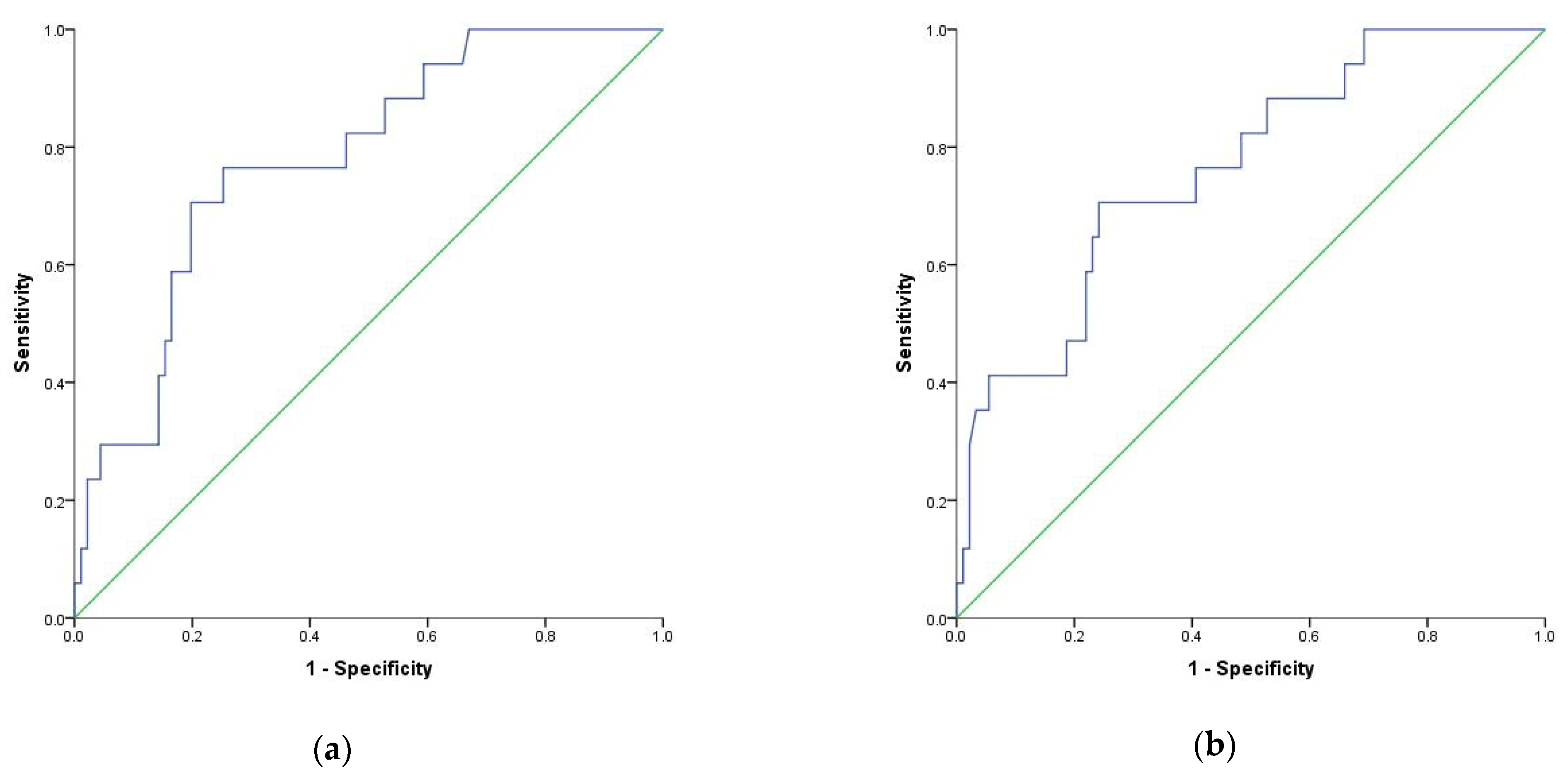
3.2. Using Optimal Cut-Off Values of Inflammatory Markers to Predict Mortality in Patients with COVID-19
3.3. Association of Inflammatory Biomarkers Results with The COVID-19 Mortality
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Naming the Coronavirus Disease (COVID-19) and the Virus That Causes It. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (accessed on 27 November 2021).
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Bio Med. Atenei Parm. 2020, 91, 157–160. [Google Scholar]
- Weekly Epidemiological Update on COVID-19—23 November 2021. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---23-november-2021 (accessed on 30 November 2021).
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus (accessed on 27 November 2021).
- Dascalu, S. The Successes and Failures of the Initial COVID-19 Pandemic Response in Romania. Front. Public Health 2020, 8, 344. [Google Scholar] [CrossRef] [PubMed]
- Alsharif, W.; Qurashi, A. Effectiveness of COVID-19 Diagnosis and Management Tools: A Review. Radiography 2021, 27, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Seyit, M.; Avci, E.; Nar, R.; Senol, H.; Yilmaz, A.; Ozen, M.; Oskay, A.; Aybek, H. Neutrophil to Lymphocyte Ratio, Lymphocyte to Monocyte Ratio and Platelet to Lymphocyte Ratio to Predict the Severity of COVID-19. Am. J. Emerg. Med. 2021, 40, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, T.S.; de Sá, K.S.G.; Ishimoto, A.Y.; Becerra, A.; Oliveira, S.; Almeida, L.; Gonçalves, A.V.; Perucello, D.B.; Andrade, W.A.; Castro, R.; et al. Inflammasomes Are Activated in Response to SARS-CoV-2 Infection and Are Associated with COVID-19 Severity in Patients. J. Exp. Med. 2021, 218, e20201707. [Google Scholar] [CrossRef]
- Koupenova, M.; Freedman, J.E. Platelets and COVID-19: Inflammation, Hyperactivation and Additional Questions. Circ. Res. 2020, 127, 1419–1421. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.-P.; Liu, J.; Tao, W.; Li, H. The Diagnostic and Predictive Role of NLR, d-NLR and PLR in COVID-19 Patients. Int. Immunopharmacol. 2020, 84, 106504. [Google Scholar] [CrossRef]
- Karimi, A.; Shobeiri, P.; Kulasinghe, A.; Rezaei, N. Novel Systemic Inflammation Markers to Predict COVID-19 Prognosis. Front. Immunol. 2021, 12, 741061. [Google Scholar] [CrossRef]
- Hirahara, T.; Arigami, T.; Yanagita, S.; Matsushita, D.; Uchikado, Y.; Kita, Y.; Mori, S.; Sasaki, K.; Omoto, I.; Kurahara, H.; et al. Combined Neutrophil-Lymphocyte Ratio and Platelet-Lymphocyte Ratio Predicts Chemotherapy Response and Prognosis in Patients with Advanced Gastric Cancer. BMC Cancer 2019, 19, 672. [Google Scholar] [CrossRef]
- Zhang, Y.; Lu, J.-J.; Du, Y.-P.; Feng, C.-X.; Wang, L.-Q.; Chen, M.-B. Prognostic Value of Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Gastric Cancer. Medicine 2018, 97, e0144. [Google Scholar] [CrossRef] [PubMed]
- Krečak, I.; Holik, H.; Morić Perić, M.; Zekanović, I.; Coha, B.; Valovičić Krečak, M.; Gverić-Krečak, V.; Lucijanić, M. Neutrophil-to-lymphocyte and Platelet-to-lymphocyte Ratios as Prognostic Biomarkers in Polycythemia Vera [Online early access]. Int. J. Lab. Hematol. 2021. Available online: https://onlinelibrary.wiley.com (accessed on 31 December 2021).
- Lucijanic, M.; Cicic, D.; Stoos-Veic, T.; Pejsa, V.; Lucijanic, J.; Fazlic Dzankic, A.; Vlasac Glasnovic, J.; Soric, E.; Skelin, M.; Kusec, R. Elevated Neutrophil-to-Lymphocyte-Ratio and Platelet-to-Lymphocyte Ratio in Myelofibrosis: Inflammatory Biomarkers or Representatives of Myeloproliferation Itself? Anticancer Res. 2018, 38, 3157–3163. [Google Scholar]
- Proctor, M.J.; McMillan, D.C.; Morrison, D.S.; Fletcher, C.D.; Horgan, P.G.; Clarke, S.J. A Derived Neutrophil to Lymphocyte Ratio Predicts Survival in Patients with Cancer. Br. J. Cancer 2012, 107, 695–699. [Google Scholar] [CrossRef] [Green Version]
- Grenader, T.; Nash, S.; Adams, R.; Kaplan, R.; Fisher, D.; Maughan, T.; Bridgewater, J. Derived Neutrophil Lymphocyte Ratio Is Predictive of Survival from Intermittent Therapy in Advanced Colorectal Cancer: A Post Hoc Analysis of the MRC COIN Study. Br. J. Cancer 2016, 114, 612–615. [Google Scholar] [CrossRef]
- Yang, T.; Hao, L.; Yang, X.; Luo, C.; Wang, G.; Cai, C.L.; Qi, S.; Li, Z. Prognostic Value of Derived Neutrophil-to-lymphocyte Ratio (DNLR) in Patients with Non-small Cell Lung Cancer Receiving Immune Checkpoint Inhibitors: A Meta-analysis. BMJ Open 2021, 11, e049123. [Google Scholar]
- Jiang, S.; Wang, S.; Wang, Q.; Deng, C.; Feng, Y.; Ma, F.; Ma, J.; Liu, X.; Hu, C.; Hou, T. Systemic Inflammation Response Index (SIRI) Independently Predicts Survival in Advanced Lung Adenocarcinoma Patients Treated with First-Generation EGFR-TKIs. Cancer Manag. Res. 2021, 13, 1315–1322. [Google Scholar] [CrossRef]
- Citu, C.; Neamtu, R.; Sorop, V.-B.; Horhat, D.I.; Gorun, F.; Tudorache, E.; Gorun, O.M.; Boarta, A.; Tuta-Sas, I.; Citu, I.M. Assessing SARS-CoV-2 Vertical Transmission and Neonatal Complications. J. Clin. Med. 2021, 10, 5253. [Google Scholar] [CrossRef]
- Macedo, A.; Gonçalves, N.; Febra, C. COVID-19 Fatality Rates in Hospitalized Patients: Systematic Review and Meta-Analysis. Ann. Epidemiol. 2021, 57, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China: A Retrospective Cohort Study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Chen, L.; Yu, J.; He, W.; Chen, L.; Yuan, G.; Dong, F.; Chen, W.; Cao, Y.; Yang, J.; Cai, L.; et al. Risk Factors for Death in 1859 Subjects with COVID-19. Leukemia 2020, 34, 2173–2183. [Google Scholar] [CrossRef] [PubMed]
- Fois, A.G.; Paliogiannis, P.; Scano, V.; Cau, S.; Babudieri, S.; Perra, R.; Ruzzittu, G.; Zinellu, E.; Pirina, P.; Carru, C.; et al. The Systemic Inflammation Index on Admission Predicts In-Hospital Mortality in COVID-19 Patients. Molecules 2020, 25, 5725. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of Comorbidities and Its Effects in Patients Infected with SARS-CoV-2: A Systematic Review and Meta-Analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Gong, J.; Ou, J.; Qiu, X.; Jie, Y.; Chen, Y.; Yuan, L.; Cao, J.; Tan, M.; Xu, W.; Zheng, F.; et al. A Tool for Early Prediction of Severe Coronavirus Disease 2019 (COVID-19): A Multicenter Study Using the Risk Nomogram in Wuhan and Guangdong, China. Clin. Infect. Dis. 2020, 71, 833–840. [Google Scholar] [CrossRef] [Green Version]
- Itelman, E.; Wasserstrum, Y.; Segev, A.; Avaky, C.; Negru, L.; Cohen, D.; Turpashvili, N.; Anani, S.; Zilber, E.; Lasman, N.; et al. Clinical Characterization of 162 COVID-19 Patients in Israel: Preliminary Report from a Large Tertiary Center. Isr. Med. Assoc. J. 2020, 22, 271–274. [Google Scholar]
- Tatum, D.; Taghavi, S.; Houghton, A.; Stover, J.; Toraih, E.; Duchesne, J. Neutrophil-to-Lymphocyte Ratio and Outcomes in Louisiana COVID-19 Patients. Shock Augusta Ga 2020, 54, 652–658. [Google Scholar] [CrossRef]
- Prozan, L.; Shusterman, E.; Ablin, J.; Mitelpunkt, A.; Weiss-Meilik, A.; Adler, A.; Choshen, G.; Kehat, O. Prognostic Value of Neutrophil-to-Lymphocyte Ratio in COVID-19 Compared with Influenza and Respiratory Syncytial Virus Infection. Sci. Rep. 2021, 11, 21519. [Google Scholar] [CrossRef]
- Huguet, E.; Maccallini, G.; Pardini, P.; Hidalgo, M.; Obregon, S.; Botto, F.; Koretzky, M.; Nilsson, P.M.; Ferdinand, K.; Kotliar, C. Reference Values for Neutrophil to Lymphocyte Ratio (NLR), a Biomarker of Cardiovascular Risk, According to Age and Sex in a Latin American Population. Curr. Probl. Cardiol. 2021, 46, 100422. [Google Scholar] [CrossRef]
- Wang, X.; Qiu, L.; Li, Z.; Wang, X.-Y.; Yi, H. Understanding the Multifaceted Role of Neutrophils in Cancer and Autoimmune Diseases. Front. Immunol. 2018, 9, 2456. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.-Y.; Feng, S.-D.; Chen, G.-P.; Wu, J.-N. Predictive Value of the Neutrophil to Lymphocyte Ratio for Disease Deterioration and Serious Adverse Outcomes in Patients with COVID-19: A Prospective Cohort Study. BMC Infect. Dis. 2021, 21, 80. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Liang, H.; Ou, L.; Chen, B.; Chen, A.; Li, C.; Li, Y.; Guan, W.; Sang, L.; Lu, J.; et al. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Intern. Med. 2020, 180, 1081. [Google Scholar] [CrossRef]
- Liu, Y.; Du, X.; Chen, J.; Jin, Y.; Peng, L.; Wang, H.H.X.; Luo, M.; Chen, L.; Zhao, Y. Neutrophil-to-Lymphocyte Ratio as an Independent Risk Factor for Mortality in Hospitalized Patients with COVID-19. J. Infect. 2020, 81, e6–e12. [Google Scholar] [CrossRef]
- Wang, C.; Deng, R.; Gou, L.; Fu, Z.; Zhang, X.; Shao, F.; Wang, G.; Fu, W.; Xiao, J.; Ding, X.; et al. Preliminary Study to Identify Severe from Moderate Cases of COVID-19 Using Combined Hematology Parameters. Ann. Transl. Med. 2020, 8, 593. [Google Scholar] [CrossRef]
- Simadibrata, D.M.; Pandhita, B.A.W.; Ananta, M.E.; Tango, T. Platelet-to-Lymphocyte Ratio, a Novel Biomarker to Predict the Severity of COVID-19 Patients: A Systematic Review and Meta-Analysis. J. Intensive Care Soc. 2020, 175114372096958. [Google Scholar] [CrossRef]
- Doganci, S.; Ince, M.E.; Ors, N.; Yildirim, A.K.; Sir, E.; Karabacak, K.; Eksert, S.; Ozgurtas, T.; Tasci, C.; Dogan, D.; et al. A New COVID-19 Prediction Scoring Model for in-Hospital Mortality: Experiences from Turkey, Single Center Retrospective Cohort Analysis. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 10247–10257. [Google Scholar] [PubMed]

| Total | Survivors 91 (84.3%) | Deaths 17 (15.7%) | p Value | |
|---|---|---|---|---|
| Age (Mean ± SD) | 63.31 ± 14.83 | 62.02 ± 14.73 | 70.18 ± 13.83 | 0.03 |
| Comorbidities No. (%) | ||||
| Diabetes | 50 (46.3%) | 40 (44.0%) | 10 (58.8%) | 0.29 |
| Hypertension | 76 (70.4%) | 62 (68.1%) | 14 (82.4%) | 0.38 |
| Heart diseases | 51 (47.2%) | 38 (41.8%) | 13 (76.5%) | 0.01 |
| Chronic lung diseases | 23 (21.3%) | 17 (18.7%) | 6 (35.3%) | 0.19 |
| Complete blood count (Mean ± SD) | ||||
| White blood cell (×1012/L) | 8.71 ± 5.74 | 8.71 ± 5.76 | 8.73 ± 5.81 | 0.98 |
| Neutrophil count (×109/L) | 6.96 ± 4.36 | 6.75 ± 4.18 | 8.06 ± 5.19 | 0.25 |
| Lymphocyte count (×109/L) | 0.98 ± 0.78 | 1.03 ± 0.82 | 0.73 ± 0.44 | 0.03 |
| Monocyte count (×109/L) | 0.47 ± 0.32 | 0.47 ± 0.32 | 0.51 ± 0.33 | 0.64 |
| Hemoglobin (g/dL) | 13.15 ± 1.78 | 13.27 ± 1.64 | 12.50 ± 2.36 | 0.10 |
| Platelet count (×109/L) | 242 ± 109 | 252 ± 112 | 192 ± 79 | 0.03 |
| Inflammatory markers | ||||
| NLR | 9.18 ± 6.7 | 8.31 ± 5.74 | 13.83 ± 9.23 | 0.001 |
| MLR | 0.58 ±0.44 | 0.53 ± 0.39 | 0.83 ± 0.59 | 0.01 |
| PLR | 327 ± 72 | 324 ± 219 | 345 ± 235 | 0.71 |
| dNLR | 5.16 ± 3.76 | 4.77 ± 3.45 | 7.07 ± 4.64 | 0.01 |
| SII | 2280 ± 1950 | 2183 ± 1847 | 2798.± 2429 | 0.23 |
| SIRI | 4.57 ± 5.12 | 4.11 ± 4.67 | 7.02 ± 6.72 | 0.03 |
| O2 Saturation * | 91.96 ± 6.16 | 92.26 ± 5.96 | 90.35 ± 7.13 | 0.24 |
| Hospitalization length | 11.89 (6.56) | 12.96 | 6.18 | <0.001 |
| Variables | Area | Std. Error | Asymptotic Sig. | 95% Confidence Interval | Sensitivity | Sensibility | Cut-Off | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| NLR | 0.689 | 0.074 | 0.014 | 0.544 | 0.833 | 70% | 67% | 9.1 |
| MLR | 0.661 | 0.078 | 0.036 | 0.508 | 0.813 | 58% | 74% | 0.69 |
| SIRI | 0.655 | 0.074 | 0.042 | 0.511 | 0.800 | 76% | 52% | 2.2 |
| dNLR | 0.652 | 0.082 | 0.047 | 0.491 | 0.813 | 41% | 92% | 9.6 |
| Variables | HR (95%CI) | p Value |
|---|---|---|
| NLR | 3.85 (1.35–10.95) | 0.01 |
| dNLR | 6.4 (2.40–17.18) | <0.001 |
| MLR | 3.05 (1.16–8.05) | 0.02 |
| Variables | Adjusted OR * | p Value |
|---|---|---|
| NLR | 4.14 | 0.002 |
| dNLR | 14.09 | 0.001 |
| MLR | 3.29 | 0.04 |
| SIRI | 3.06 | 0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Citu, C.; Gorun, F.; Motoc, A.; Sas, I.; Gorun, O.M.; Burlea, B.; Tuta-Sas, I.; Tomescu, L.; Neamtu, R.; Malita, D.; et al. The Predictive Role of NLR, d-NLR, MLR, and SIRI in COVID-19 Mortality. Diagnostics 2022, 12, 122. https://doi.org/10.3390/diagnostics12010122
Citu C, Gorun F, Motoc A, Sas I, Gorun OM, Burlea B, Tuta-Sas I, Tomescu L, Neamtu R, Malita D, et al. The Predictive Role of NLR, d-NLR, MLR, and SIRI in COVID-19 Mortality. Diagnostics. 2022; 12(1):122. https://doi.org/10.3390/diagnostics12010122
Chicago/Turabian StyleCitu, Cosmin, Florin Gorun, Andrei Motoc, Ioan Sas, Oana Maria Gorun, Bogdan Burlea, Ioana Tuta-Sas, Larisa Tomescu, Radu Neamtu, Daniel Malita, and et al. 2022. "The Predictive Role of NLR, d-NLR, MLR, and SIRI in COVID-19 Mortality" Diagnostics 12, no. 1: 122. https://doi.org/10.3390/diagnostics12010122
APA StyleCitu, C., Gorun, F., Motoc, A., Sas, I., Gorun, O. M., Burlea, B., Tuta-Sas, I., Tomescu, L., Neamtu, R., Malita, D., & Citu, I. M. (2022). The Predictive Role of NLR, d-NLR, MLR, and SIRI in COVID-19 Mortality. Diagnostics, 12(1), 122. https://doi.org/10.3390/diagnostics12010122







