The Onset of Subtalar Joint Monoarthritis in a Patient with Rheumatoid Arthritis
Abstract
:1. Introduction
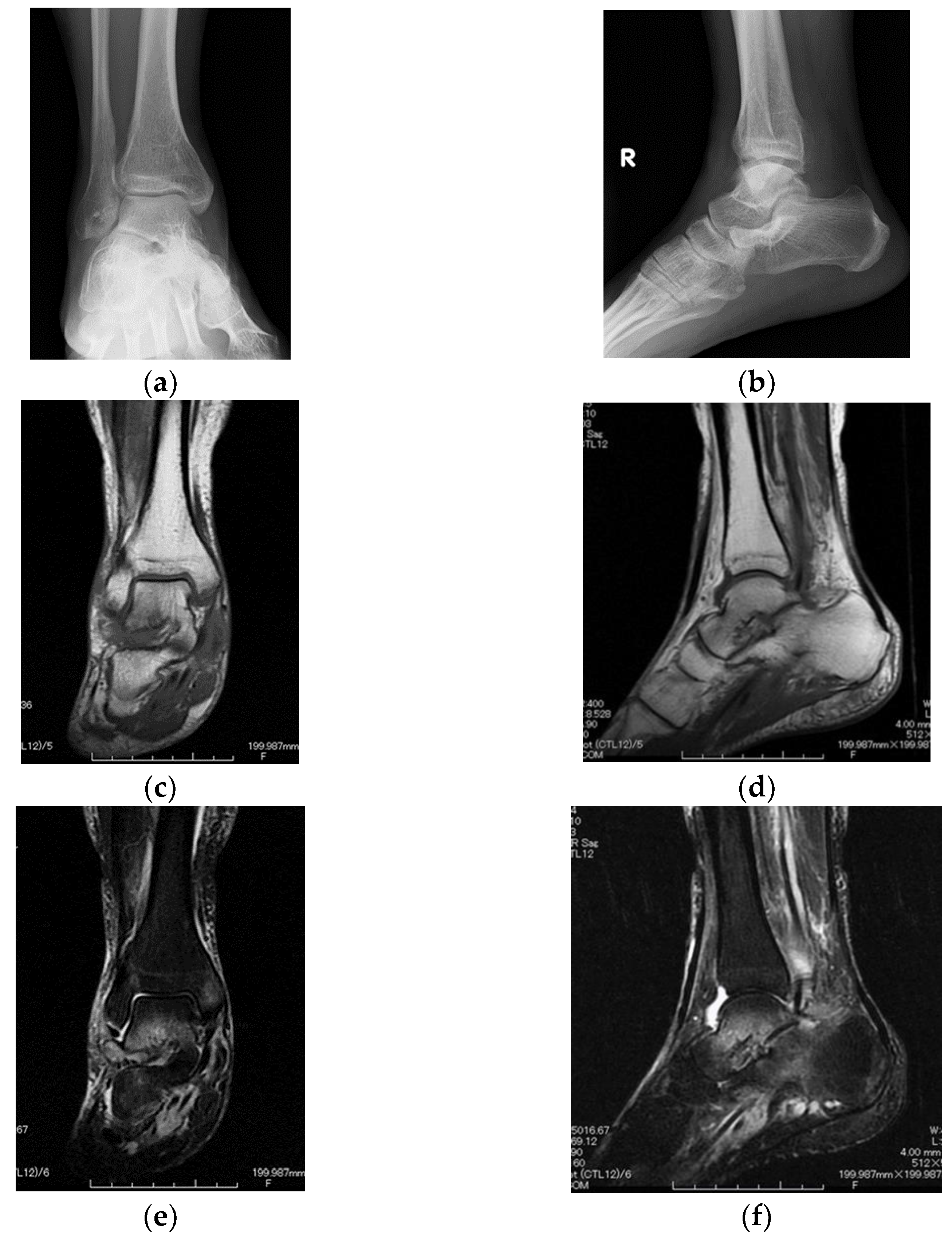
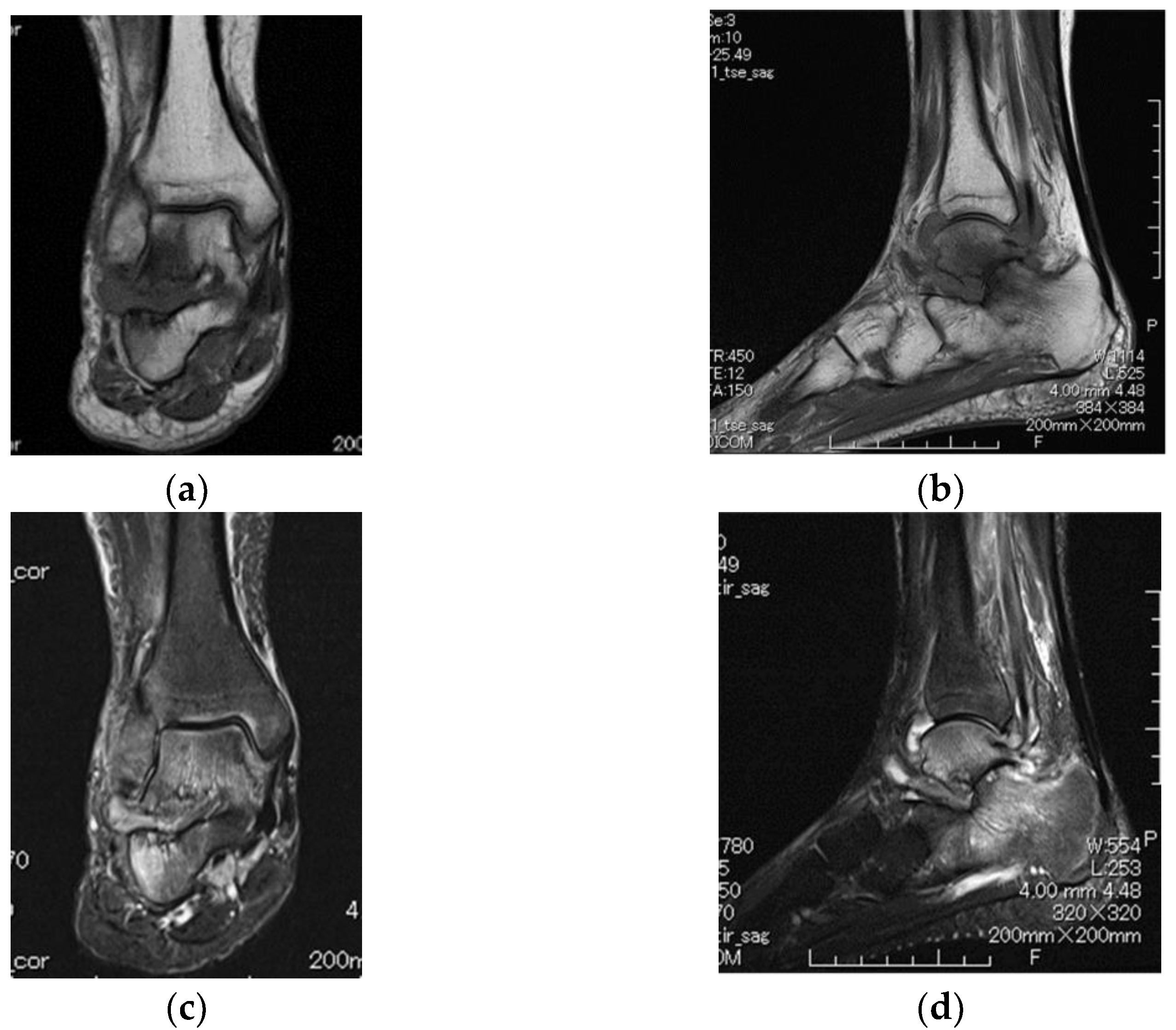
2. Case Presentation
3. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karatepe, A.G.; Gunaydin, R.; Adibelli, Z.H.; Kaya, T.; Duruoz, E. Foot deformities in patients with rheumatoid arthritis: The relationship with foot functions. Int. J. Rheum. Dis. 2010, 13, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, T.M.; Spiegel, J.S. Rheumatoid arthritis in the foot and ankle--diagnosis, pathology, and treatment. The relationship between foot and ankle deformity and disease duration in 50 patients. Foot Ankle 1982, 2, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Fleming, A.; Crown, J.M.; Corbett, M. Incidence of joint involvement in early rheumatoid arthritis. Rheumatol. Rehabil. 1976, 15, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.L.; Coulton, B.L.; Popert, A.J. Long term progression of joint damage in rheumatoid arthritis. Ann. Rheum. Dis. 1986, 45, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Belt, E.A.; Kaarela, K.; Kauppi, M.J. A 20-year follow-up study of subtalar changes in rheumatoid arthritis. Scand. J. Rheumatol. 1997, 26, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Șerban, O.; Papp, I.; Bocșa, C.D.; Micu, M.C.; Bădărînză, M.; Albu, A.; Fodor, D. Do ankle, hindfoot, and heel ultrasound findings predict the symptomatology and quality of life in rheumatoid arthritis patients? J. Ultrason. 2020, 20, e70–e82. [Google Scholar] [CrossRef]
- Bouysset, M.; Tavernier, T.; Tebib, J.; Noel, E.; Tillmann, K.; Bonnin, M.; Eulry, F.; Bouvier, M. CT and MRI evaluation of tenosynovitis of the rheumatoid hindfoot. Clin. Rheumatol. 1995, 14, 303–307. [Google Scholar] [CrossRef]
- Wilson, O.; Hewlett, S.; Woodburn, J.; Pollock, J.; Kirwan, J. Prevalence, impact and care of foot problems in people with rheumatoid arthritis: Results from a United Kingdom based cross-sectional survey. J. Foot Ankle Res. 2017, 27, 10:46. [Google Scholar] [CrossRef]
- Jeong, H.J.; Sohn, I.W.; Kim, D.; Cho, S.K.; Park, S.B.; Sung, I.H.; Sung, Y.K. Impact of midfoot and hindfoot involvement on functional disability in Korean patients with rheumatoid arthritis. BMC Musculoskelet Disord. 2017, 18, 365. [Google Scholar] [CrossRef]
- Yano, K.; Ikari, K.; Inoue, E.; Sakuma, Y.; Mochizuki, T.; Koenuma, N.; Tobimatsu, H.; Tanaka, E.; Taniguchi, A.; Okazaki, K.; et al. Features of patients with rheumatoid arthritis whose debut joint is a foot or ankle joint: A 5479-case study from the IORRA cohort. PLoS ONE 2018, 13, e0202427. [Google Scholar] [CrossRef] [PubMed]
- Otter, S.J.; Lucas, K.; Springett, K.; Moore, A.; Davies, K.; Cheek, L.; Young, A.; Walker-Bone, K. Foot pain in rheumatoid arthritis prevalence, risk factors and management: An epidemiological study. Clin. Rheumatol. 2010, 29, 255–271. [Google Scholar] [CrossRef] [PubMed]
- Grondal, L.; Tengstrand, B.; Nordmark, B.; Wretenberg, P.; Stark, A. The foot: Still the most important reason for walking incapacity in rheumatoid arthritis: Distribution of symptomatic joints in 1000 RA patients. Acta Orthop. 2008, 79, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Jernberg, E.T.; Simkin, P.; Kravette, M.; Lowe, P.; Gardner, G. The posterior tibial tendon and the tarsal sinus in rheumatoid flat foot: Magnetic resonance imaging of 40 feet. J. Rheumatol. 1999, 26, 289–293. [Google Scholar] [PubMed]
- Turner, D.E.; Woodburn, J.; Helliwell, P.S.; Cornwall, M.W.; Emery, P. Pes planovalgus in RA: A descriptive and analytical study of foot function determined by gait analysis. Musculoskelet. Care 2003, 1, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Hirao, M.; Tsuboi, H.; Akita, S.; Matsushita, M.; Ohshima, S.; Saeki, Y.; Hashimoto, J. Effect of correction of hindfoot valgus deformity on ankle joint pain relief in rheumatoid arthritis cases: A report of two cases. Sage Open Med. Case Rep. 2014, 2, 2050313X14553694. [Google Scholar] [CrossRef] [PubMed]
- Sarazin, J.; Schiopu, E.; Namas, R. Case series: Monoarticular rheumatoid arthritis. Eur. J. Rheumatol. 2017, 4, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Amendola, A.; Lee, K.B.; Saltzman, C.L.; Suh, J.S. Technique and early experience with posterior arthroscopic subtalar arthrodesis. Foot Ankle Int. 2007, 28, 298–302. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wakabayashi, H.; Nakata, K.; Nishimura, A.; Hasegawa, M.; Sudo, A. The Onset of Subtalar Joint Monoarthritis in a Patient with Rheumatoid Arthritis. Diagnostics 2022, 12, 2311. https://doi.org/10.3390/diagnostics12102311
Wakabayashi H, Nakata K, Nishimura A, Hasegawa M, Sudo A. The Onset of Subtalar Joint Monoarthritis in a Patient with Rheumatoid Arthritis. Diagnostics. 2022; 12(10):2311. https://doi.org/10.3390/diagnostics12102311
Chicago/Turabian StyleWakabayashi, Hiroki, Kenta Nakata, Akinobu Nishimura, Masahiro Hasegawa, and Akihiro Sudo. 2022. "The Onset of Subtalar Joint Monoarthritis in a Patient with Rheumatoid Arthritis" Diagnostics 12, no. 10: 2311. https://doi.org/10.3390/diagnostics12102311
APA StyleWakabayashi, H., Nakata, K., Nishimura, A., Hasegawa, M., & Sudo, A. (2022). The Onset of Subtalar Joint Monoarthritis in a Patient with Rheumatoid Arthritis. Diagnostics, 12(10), 2311. https://doi.org/10.3390/diagnostics12102311




