Abstract
Current diagnostic criteria for left ventricular noncompaction (LVNC) may be poorly related to adverse prognosis. Late gadolinium enhancement (LGE) is a predictor of major adverse cardiovascular events (MACE), but risk stratification of LGE in patients with LVNC remains unclear. We retrospectively analyzed the clinical and cardiovascular magnetic resonance (CMR) data of 75 patients from three institutes and examined the correlation between different LGE types and MACE based on the extent, pattern (including a specific ring-like pattern), and locations of LGE in LVNC. A total of 51 patients (68%) presented LGE. A specific ring-like pattern was observed in 9 (12%). MACE occurred in 29 (38.7%) at 4.3 years of follow-up (interquartile range: 2.1–5.7 years). The adjusted hazard ratio (HR) for patients with ring-like LGE were 6.10 (95% CI, 1.39–26.75, p < 0.05). Free-wall or mid-wall LGE was associated with an increased risk of MACE after adjustment (HR 2.85, 95% CI, 1.31–6.21; HR 4.35, 95% CI, 1.23–15.37, respectively, p < 0.05). The risk of MACE in LVNC significantly increased when the LGE extent was greater than 7.5% and ring-like, multiple segments, and free-wall LGE were associated with MACE. These results suggest the value of LGE risk stratification in patients with LVNC.
1. Introduction
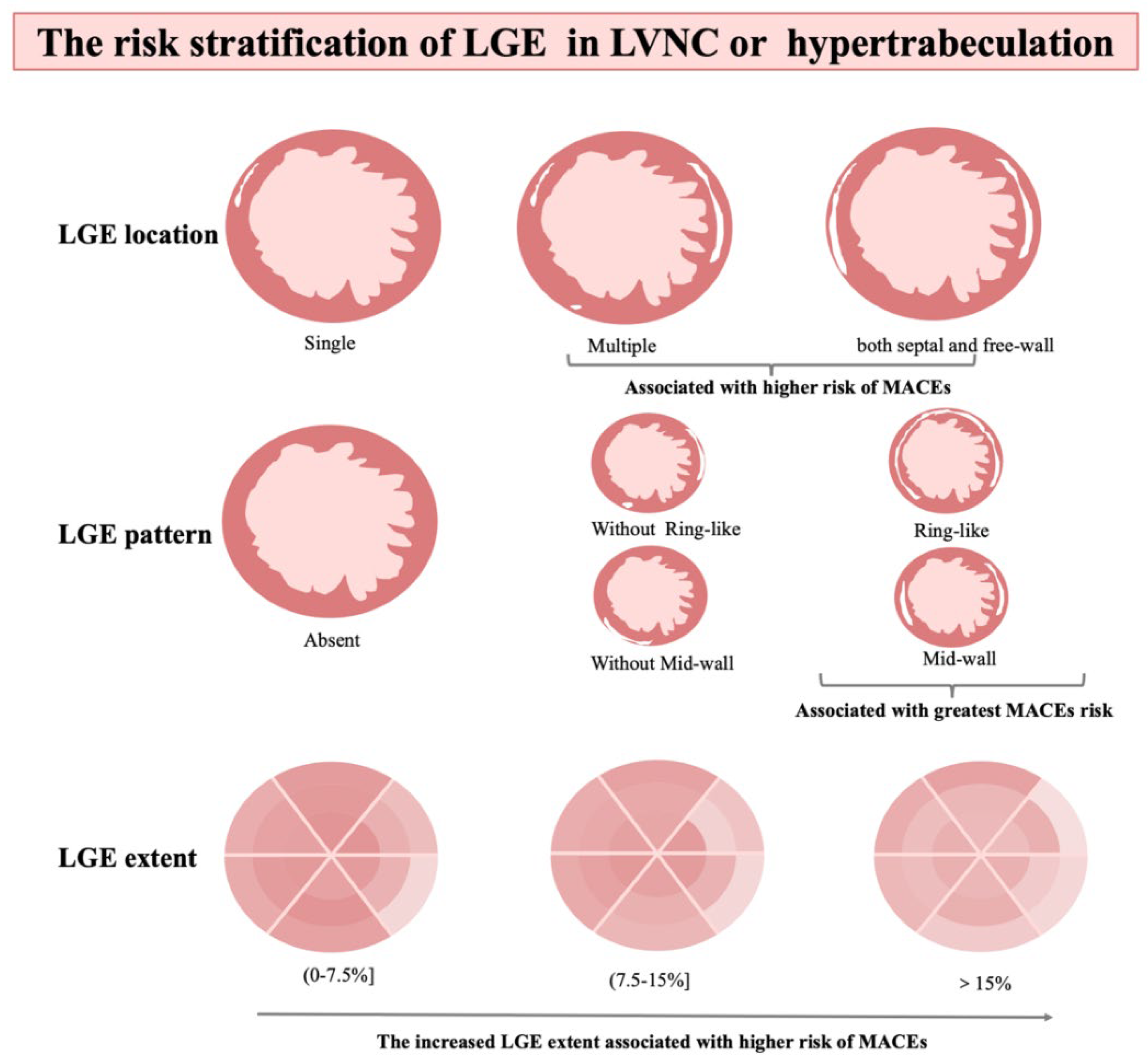
Left ventricular noncompaction (LVNC), an uncommon cardiomyopathy characterized by a thickened endocardial layer with prominent trabeculae and a thinned, compacted epicardial layer [1], can occur as an isolated anomaly or associated with left ventricular dilation or hypertrophy, or various forms of congenital heart disease [2,3,4], and may lead to serious outcomes such as heart failure, thromboembolism, implantable cardioverter-defibrillator (ICD) therapy, heart transplantation, or sudden cardiac death [5,6]. Although several definitions have been proposed, currently diagnosis is mainly based on morphologic findings, and have the risk of overdiagnosis [1,7,8,9]. Several studies show a poor correlation between diagnostic criteria and adverse clinical events [10,11,12]. Furthermore, risk stratification in LVNC is particularly challenging and not available. A recent JACC paper proposes a risk prediction model of LVNC, in which late gadolinium enhancement (LGE) being one of the main prognostic factors [13,14]. LGE has negative prognostic implications in heart diseases, including hypertrophic cardiomyopathy, dilated cardiomyopathy, and LVNC [12,15,16,17,18,19,20]; however, previous studies have focused primarily on the presence of LGE but do not provide a detailed risk stratification analysis. The relationship between dose-response, LGE location and pattern, and specific clinical outcomes are poorly understood [14]. Therefore, we conducted a multicenter study to evaluate the association between the extent, location, or pattern of LGE and the impact on prognosis in patients with LVNC and hypertrabeculation patients. It is of great significance for clinicians and radiologists to judge the risk stratification of LVNC and hypertrabeculation patients intuitively and concisely. The guidelines of LVNC were lacking currently, and this evaluation may contribute to the establishment of hypertrabeculated LVNC guidelines and direct clinical management strategies (Figure 1).
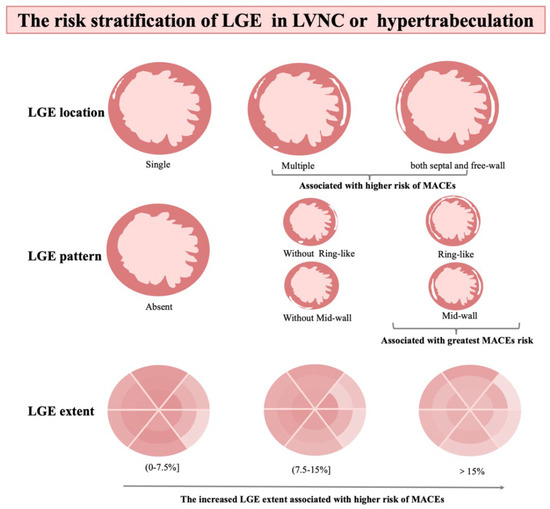
Figure 1.
The graphic abstract. CMR, cardiovascular magnetic resonance; NC/C noncompact–tion/compacted; LGE, late gadolinium enhancement.
2. Materials and Methods
2.1. Study Population
We searched the clinical and cardiovascular magnetic resonance (CMR) databases at three institutions for patients’ diagnosis descripted as LVNC or hypertrabeculation between January 2013 and December 2018, and the total number is 85. The CMR images of these patients were measured again according to Petersen’s criteria by two radiologists with at least two years of experience. The inclusion criteria followed Petersen et al.’s CMR criteria: (1) CMR images with a distinct two-layered appearance of trabeculated and compacted myocardium; (2) There are prominent myocardial trabeculations in the noncompacted myocardium and deep intertrabecular recesses communicating with the LV; and (3) Subjects with increased LV trabeculation as measured by a noncompaction/compacted (NC/C) ratio ≥ 1.0 anywhere in the myocardial segments on the CMR images. Current diagnosis is mainly based on this criterion [8,14]. Both LVNC and hypertrabeculation patients were included in the cohort. The exclusion criteria were as follows: (1) presence of other known coexisting cardiac abnormalities, including congenital heart disease, coronary heart disease, valvular heart disease, hypertrophic cardiomyopathy, dilated cardiomyopathy or other types of cardiomyopathy, and myocarditis; (2) non-enhanced or poor image quality; and (3) incomplete clinical records. A total of 75 patients were eventually included in the cohort. The Ethics Committee of Clinical Trials and Biomedicine at the West China Hospital of Sichuan University and the ethics committees of other authors’ hospitals approved this study. This study was performed in accordance with the Declaration of Helsinki (2000). Informed consent was obtained from all participants before study participation.
2.2. CMR Protocol
Standard gadolinium-enhanced CMR scanning was performed by a 3.0-T whole-body scanner (Skyra; Siemens Medical Solutions, Erlangen, Germany) with a two-element cardiac phased-array coil and ECG-triggering device. After acquiring localization images, 8–12 continuous short-axis cine images that covered the whole left ventricle were obtained by steady-state free-precession sequence. All cine images were acquired at end-expiration. Gadobenate dimeglumine (MultiHance 0.5 mmol/mL; Bracco, Milan, Italy) was injected intravenously at a dose of 0.1–0.2 mL/kg body weight and a flow rate of 2.5–3.0 mL/s after a 20–25 mL saline flush at a rate of 3.0 mL/s. LGE images were obtained using the inversion recovery TrueFISP sequence 10–15 min after contrast injection.
2.3. Image Analysis
All CMR data were analyzed using the commercially available software cvi42 (Circle Cardiovascular Imaging, Inc., Calgary, AB, Canada). Image analysis was performed to evaluate conventional cardiac function. For the cine imaging analysis, left ventricular structure and function parameters were measured on the short and long axis at end-diastole and end-systole, respectively. The left ventricular geometric parameters included the ratio of non-compacted to compacted myocardium, the end-diastolic volume (EDV), and end-systolic volume (ESV) mass. Cardiac function measurements, including the LV EDV, LV ESV, LV ejection fraction (EF), LV stroke volume, and LV mass, were analyzed by manually tracing the endocardial and epicardial contours. When delineated, the papillary muscles were excluded from the compacted myocardium. The end-diastolic and end-systolic phases were defined as those with maximum and minimum visual areas, respectively. The endocardial and epicardial boundaries of all images were manually delineated by a radiologist with at least two years of experience who was blinded to the clinical information. In addition, the ratio of NC/C was calculated in end-diastole. In each of three diastolic long-axis views (i.e., horizontal and vertical long-axis and LV outflow tract), the segment with the most pronounced trabeculations was chosen for measurement of the thickness of the non-compacted and the compacted myocardium perpendicular to the compacted myocardium, and only the maximal ratio was then used for analysis. The presence and extent of LGE were assessed and quantified on short-axis images, and LGE was deemed present if myocardial enhancement was confirmed on short-axis areas by using a signal intensity threshold of 5 standard deviations (SD) [21,22] above the mean signal of the remote normal myocardium, expressed as a percentage of scar mass/total LV mass. The presence of LGE was determined by two independent radiologists, with a third providing adjudication if necessary. An experienced radiologist categorized the LGE location and pattern. Visual assessment for the presence and distribution of LGE areas for each left ventricular (LV) myocardial segment was done using a standard 17-segment cardiac model. The definition of ring-like was that LGE present in at least three contiguous segments in the same short-axis slice [23].
2.4. Follow-Up
All patients were followed up on the telephone by using the standard questionnaire interview and the clinical medical records, which was performed by experienced physicians blinded to the clinical and CMR data. The clinical endpoint of this study was MACEs, defined as HF hospitalizations, thromboembolic events, appropriate ICD therapy, heart transplant, and sudden cardiac death. The duration of follow-up was calculated from the date of first CMR examination to the first occurrence of an endpoint. The median follow-up was 4.3 years (interquartile range: 2.1–5.7 years).
2.5. Statistical Analysis
Statistical analysis was performed with SPSS software (version 26.0, IBM Corp., Armonk, NY, USA). Continuous variables are expressed as means ± SD and categorical data as percentages. Baseline characteristics were compared using the Kruskal–Wallis rank test for continuous data and the Fisher exact test for categorical data. The Kaplan–Meier method was used to evaluate survival, and multivariate Cox regression analyses were performed to compute the hazard ratio (HR) and 95% confidence interval (CI). A p-value < 0.05 was significant. The proportional hazard models were adjusted for LVEF, sex, and age, which may confound the association between LGE and results.
3. Results
3.1. Study Population
The final cohort comprised 75 patients; a total of 52 (69.3%) were men, the median LVEF was 29.1% (IQ range: 17.5–37.7%), and LGE was present in 51 (68%). Patients with and without LGE had similar baseline ages. Patients with LGE had higher diastolic blood pressures (p = 0.023), lower LVEF (p = 0.005), greater LVEDV (p = 0.001) and LVESV (p < 0.001), larger left ventricular systolic mass (p = 0.001), and diastolic mass (p = 0.001). NYHA class ≥ III (n = 38, 50.7%) were common in all participants, and patients with LGE tended to have a poor NYHA functional (p = 0.01). Baseline characteristics are presented in Table 1. Two experienced radiologists determined LGE, and there was no significant difference between the two diagnoses.

Table 1.
Baseline Characteristic.
Of the patients with LGE, 9 (12%) patients displayed a ring-like pattern and 42 (56%) a non-ring-like scar pattern. LGE was present only in the septum in 27 (36%) patients, only in the LV free wall in 16 (21.3%), and in both locations in 8 (10.7%). LGE was present only in a single segment in 37 (49.3%) patients, and in multiple segments in 14 (18.7%). LGE was categorized as mid-wall in 43 (57.3%) patients, and non-mid-wall in 8 (10.7%). Additionally, the LGE extent was categorized as three groups ( >0 and ≤7.5%, >7.5% and ≤15%, and >15%).
3.2. Outcome of Follow-Up
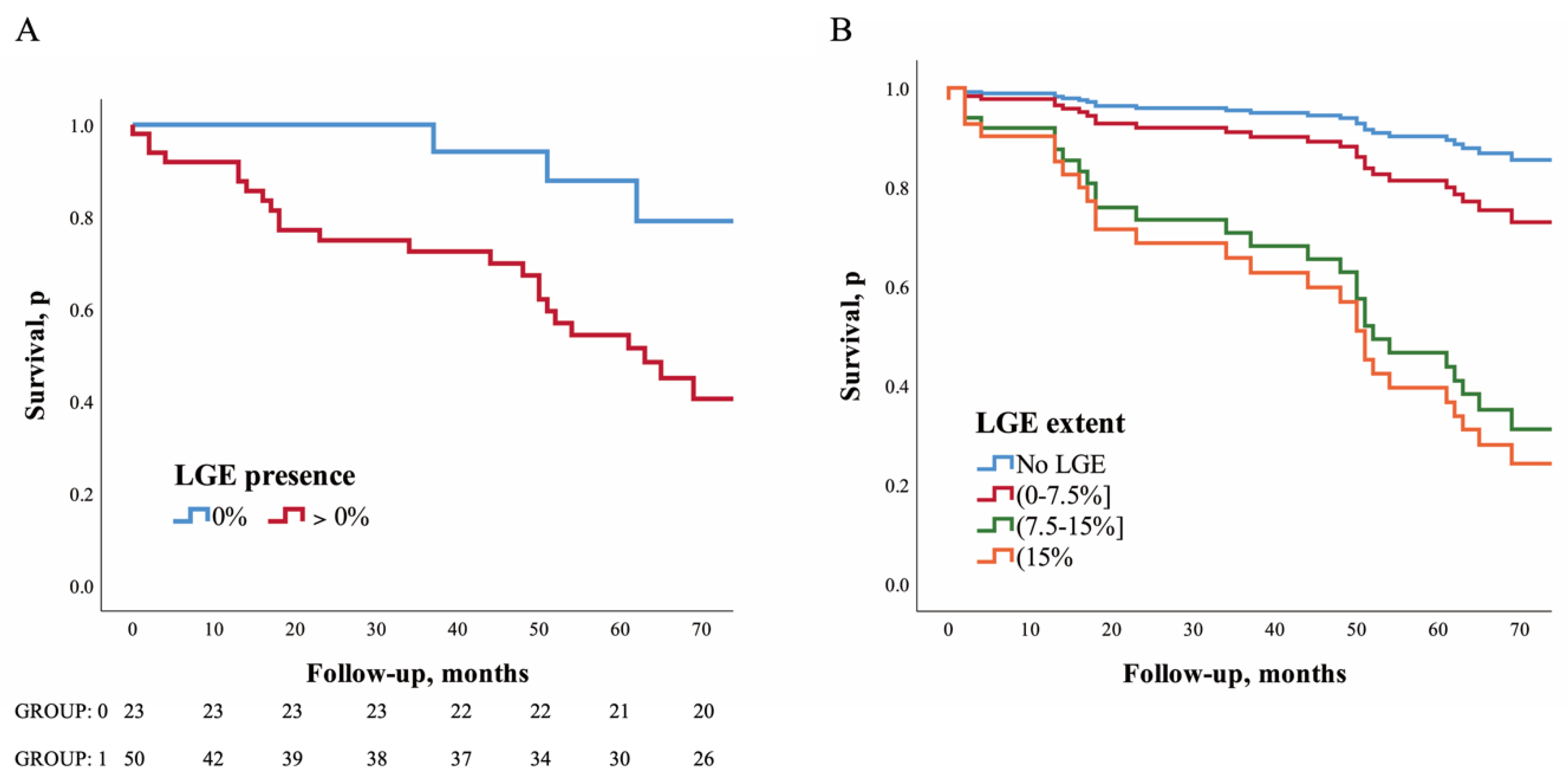
Over a median follow-up period of 4.3 years (IQ range: 2.1–5.7 years), two patients were lost. Of the 73 patients who completed follow-up, MACEs occurred in 29 (38.7%) patients. A total of 9 (31.0%) had HF hospitalizations, 8 (27.6%) underwent primary prevention ICD implantation, 2 (6.9%) had cardiac transplantation, and 10 (34.5%) had sudden cardiac death. MACEs occurred in 25 (50%) patients with LGE and in 4 (17.4%) without LGE (HR: 5.39; 95% CI: 1.59–18.31; p = 0.007). After adjustment of LVEF, age, and sex, LGE was associated with a higher risk of MACEs (HR: 3.84; 95% CI: 1.10–13.40; p = 0.035, Table 2 and Figure 2A).

Table 2.
Individual proportional hazard models investigating the association between major adverse cardiovascular events and late gadolinium enhancement (Presence and Extent).
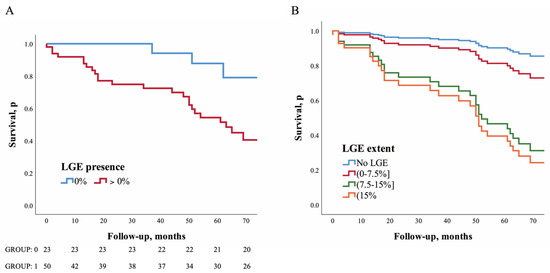
Figure 2.
Impact of LGE presence and extent of left ventricular on long–term outcomes. Kaplan–Meier and COX regression analysis survival curves depicting time to MACE. Kaplan–Meier curve for LGE presence (A) and Cox regression analysis for LGE extent (B); MACE, major adverse cardi–ovascular events.
Extent of LGE. Estimated adjusted HRs for patients with LGE extents of 0–7.5%, 7.5–15%, and >15% were 2.01 (95% CI: 0.50–8.03; p = 0.323), 7.42 (95% CI: 1.76–31.3; p = 0.006), and 9.02 (95% CI: 2.11–38.52; p = 0.003), respectively, compared to the patients without LGE (Table 2 and Figure 2B).
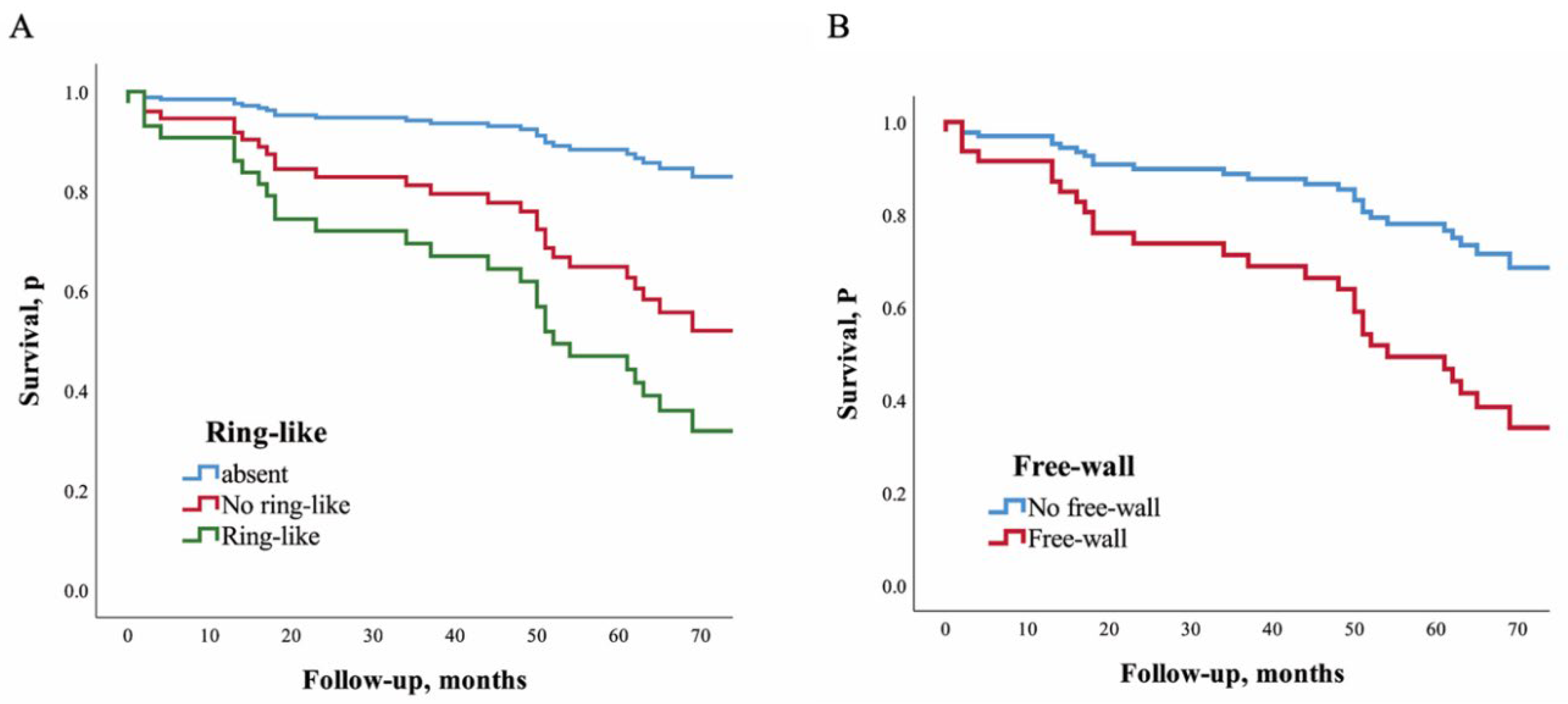
Pattern of LGE. Estimated adjusted HRs for patients with ring-like and non-ring-like scar were 6.10 (95% CI: 1.39–26.75; p = 0.016) and 3.59 (95% CI: 0.99–12.39; p = 0.053) compared to those patients without LGE. Patients with LGE only in single segment and in multiple segments had adjusted HRs for the MACEs of 2.96 (95% CI: 0.82–10.69; p = 0.098) and 8.35 (95% CI: 2.10–33.17; p = 0.003) compared to those patients without LGE (Table 3 and Figure 3A).

Table 3.
Individual proportional hazard models investigating the association between major ad–verse cardiovascular events and late gadolinium enhancement (Location and Pattern).
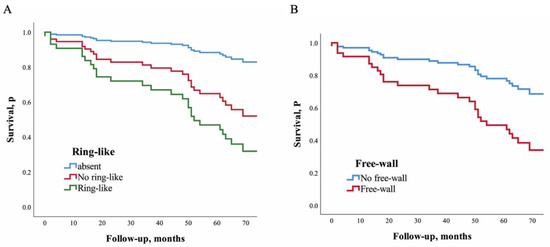
Figure 3.
Impact of ring–like and free–wall LGE of left ventricular on long–term outcomes. Cox re–gression analysis for ring–like LGE (A) and free–wall LGE (B).
Location of LGE. Estimated adjusted HRs for patients with LGE only in the septum, only in the free-wall, and in both locations were 2.57 (95% CI: 0.69–9.60; p = 0.16), 4.92 (95% CI: 1.18–20.58; p = 0.029), and 10.29 (95% CI: 2.42–43.75; p = 0.002), respectively, compared to the patients without LGE. Patients with free-wall LGE had an estimated adjusted HR of 2.85 (95% CI: 1.31–6.21; p = 0.008) compared to those without free-wall LGE. Patients with mid-wall LGE and other myocardial locations had adjusted HRs for the MACEs of 4.35 (95% CI: 1.23–15.37; p = 0.023) and 1.86 (95% CI: 0.30–11.61; p = 0.507), respectively, compared to those without LGE (Table 3 and Figure 3B).
NC/C ratio. The NC/C ratio was categorized as hypertrabeculation (NC/C ratio ≥1 and <2.3) and non-compaction (NC/C ratio ≥ 2.3); the risk between the two groups did not reach statistical significance (HR: 1.03 95% CI, 0.49–2.17; p = 0.93) (Table 4).

Table 4.
Individual proportional hazard models investigating the association between major adverse cardiovascular events and NC/C ratio.
4. Discussion
The major clinical messages arising from our study were as follows:
- (1)
- The >7.5% LGE extent may be associated with a significantly poor long-term prognosis in hypertrabeculation and LVNC patients.
- (2)
- Ring-like LGE and multiple segments LGE were associated with a particularly high risk of MACEs, which deserves extra clinical attention.
- (3)
- The NC/C ratio poorly correlates with clinical outcomes, LGE should be considered in diagnoses as a risk predictor, and our study provided useful risk stratification.
Myocardial fibrosis can significantly affect patients’ prognoses. LGE is of great significance in identifying high-risk patients. This finding has been widely confirmed in heart diseases [24,25]. However, the detail risk stratification about LGE and specific LGE pattern in the prognosis of patients with myocardial hypertrabeculation and LVNC are not yet clear [20]. Seventy-five patients from three study centers with CMR-confirmed hypertrabeculation and LVNC were enrolled. During the median follow-up of 4.3 years (IQ range: 2.1–5.7 years), major cardiovascular events (cardiac death, heart failure, thromboembolism, appropriate ICD therapy, and cardiac transplantation) were endpoints. The risk stratification of LGE extent, pattern, and location was determined. The results showed that LGE had a significant impact on the prognosis of patients with hypertrabeculation or LVNC. Risk of MACEs increased significantly with a greater extent of LGE. Our data also showed that patients with different LGE locations or patterns had a different MACE risk, which facilitates the use of CMR for prognostic risk stratification in hypertrabeculation or LVNC patients with LGE.
Patients with LGE were placed in three groups according to the extent of enhancement. After being adjusted for LVEF, sex, and age, the absence of LGE was still associated with a lower risk of MACE. The risks increased significantly when the LGE extent was greater than 7.5%; HRs were 7.42 and 9.02 in the 7.5–15% and >15% groups, respectively. In a prior study, a ≥15% LGE extent was considered a potentially clinically relevant threshold in HCM [26]; however, our data indicate that the prognosis relevant threshold may be lower in patients with LVNC.
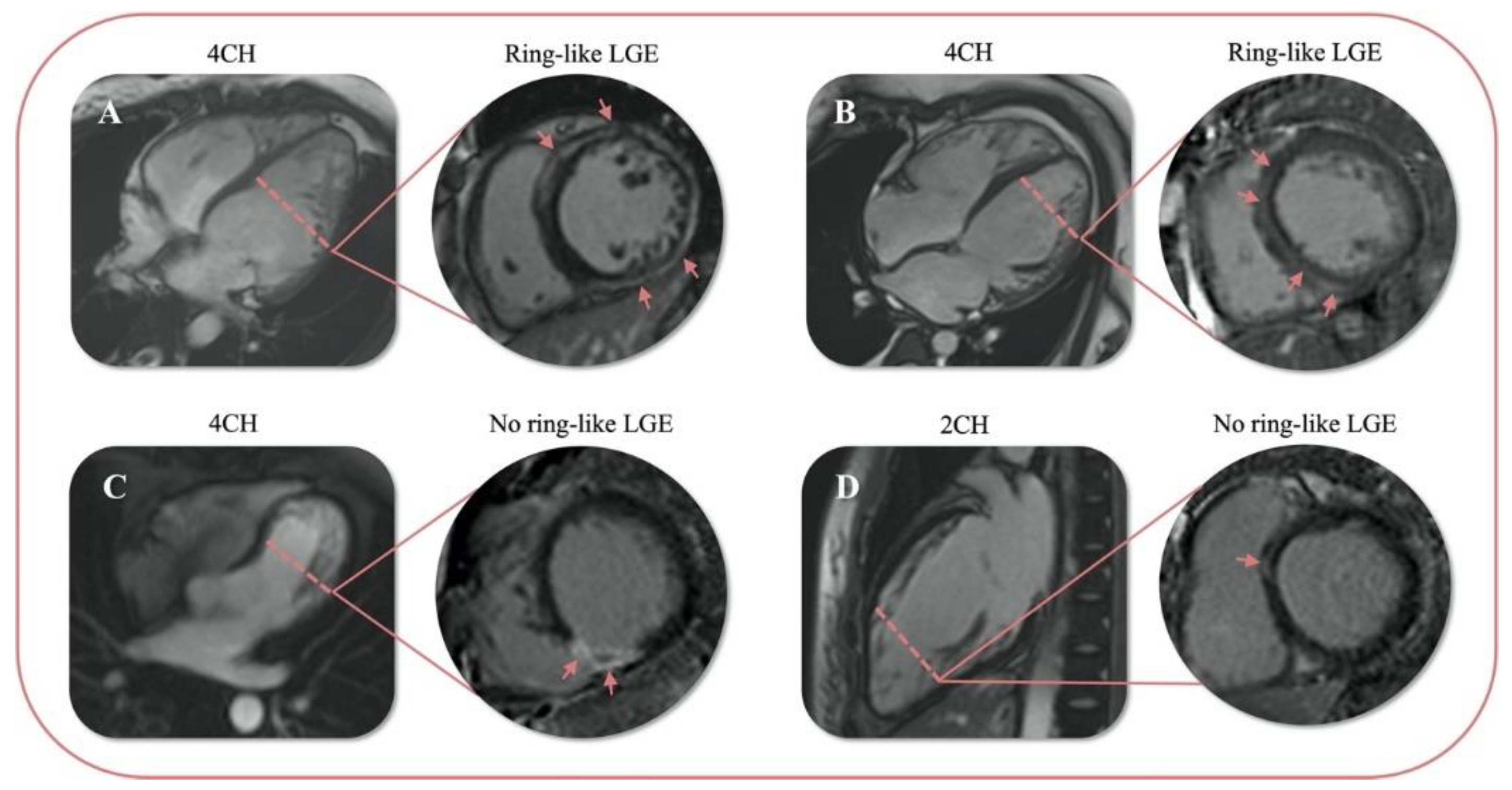
A recent study points out that a specific ring-like LGE pattern is associated with a particularly high risk of malignant arrhythmic events, which are significant and independent of the total LGE burden and the presence of other additional risk factors; the HR of a ring-like pattern in this study was 68.98 (95% CI, 14.67–324.39; p < 0.01) compared to the absence of LGE [27]. In our study, the LGE pattern was classified as a ring-like and non-ring-like scar. The definition of ring-like was that LGE was present in at least three contiguous segments in the same short-axis slice (Figure 4) [23]. The result of our study is in line with previous reports. The risk of MACE was significantly higher in ring-like LGE patients than patients with non-ring-like LGE and without LGE by Kaplan–Meier analysis. After multivariate adjustment, the presence of ring-like LGE remained associated with an increased risk of the endpoint (HR: 6.10 95% CI, 1.39–26.75; p = 0.016). This finding indicates that ring-like LGE is also a predictor of adverse events in patients with LVNC or hypertrabeculation. In particular, ring-like LGE also presented even the extent of LGE was low (<7.5%). The worse prognosis may relate to insults of the conduction system. In this regard, qualitative indicators are more convenient for radiologists to diagnose than quantitative analyses by CVi.
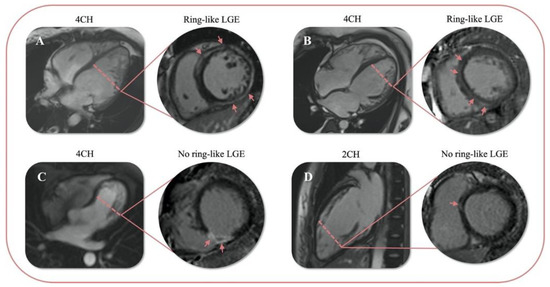
Figure 4.
Examples of 4 patients with ring-like or no ring-like LGE. Ring-like LGE (A,B) and no ring-like LGE (C,D); 4CH: the four-cavity heart; 2CH: the two-cavity heart.
Analogously, it is more intuitive to determine whether LGE is present in multiple segments of the left ventricle. We showed that patients with multiple LGE segments were at higher risk of MACEs. In contrast, those with single-segment LGE were at similar risk to those without LGE. In patients with multiple LGE segments, LGE is not only present in consecutive segments at the same short-axis level but also scattered in a total of 17 segments.
Mahrholdt et al. showed that in a setting of HHV6 and combined PVB19/HHV6 myocarditis, LGE is predominantly located in the anteroseptal region [28]. Aquaro et al. found that LGE present in the anteroseptal wall in patients with acute myocarditis was associated with a worse prognosis [17]. This finding is similar in DCM in those patients with septal LGE had a higher risk of all-cause mortality [15]. However, we showed that free-wall LGE was associated with increased MACEs in LVNC. A greater risk was seen in concomitant free-wall and septum LGE, which indicates that the prognosis of patients with LVNC or hypertrabeculation may have greater relevance with free-wall LGE. In agreement with previous studies, we observed that the most common distribution of LGE in LVNC or hypertrabeculation patients was mid-myocardial and associated with a poor prognosis, similar to other cardiac diseases [29].
Current criteria for the diagnosis of LVNC lead to high disease prevalence in patients referred for CMR, and the NC/C ratio > 2.3 is common in a large population-based cohort, indicating that the NC/C ratio alone for LVNC or hypertrabeculation diagnosis may have low specificity [10,30]. Some studies suggest that the NC/C ratio and the extent of trabeculation do not correlate with adverse outcomes [31], which is in line with our data. These results suggest that a more comprehensive criteria model including LGE should be used. Our study provides several risk stratification models of LGE that are significantly associated with the prognosis in patients with LVNC.
Study limitation. This study has some limitations. Although this is a multicenter study, the low number of patients limited statistical power. Secondly, all the three centers are large referral hospitals. Some patients who came to our hospitals were referred by multiple primary hospitals with more severe symptoms, therefore, they had a lower LVEF overall, and there may be some selection bias. However, this study also provides more prognostic information for patients with relatively severe symptoms.
5. Conclusions
In LVNC or hypertrabeculation, the risk of MACE increases significantly when the LGE extent is greater than 7.5% or presence as ring-like LGE. Moreover, multiple segments and free-wall LGE are associated with MACE. The detailed study and risk stratification of LGE in LVNC or hypertrabeculation patients will help improve the diagnostic criteria and make this criterion more closely to clinical prognosis. This study provided useful models based on the extent, pattern, and location of LGE, which provide a much-needed approach to quantify risk.
Author Contributions
Conceptualization, Y.G.; Data curation, W.H., R.S., Z.Z., W.B., W.L., R.H. and L.Y. (Li Yu); Methodology, L.Y. (Lu Ye); Project administration, Y.G.; Writing—Original draft, W.H.; Writing—Review and editing, R.X. and H.X. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by National Natural Science Foundation of China (82120108015, 82102020, 82071874, 81971586) and Sichuan Science and Technology Program (2020YJ0029, 2017TD0005); Clinical Research Grant of Chinese Society of Cardiovascular Disease (CSC) of 2019 (No. HFCSC2019B01); and the Fundamental Research Funds for the Central Universities (SCU2020D4132).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Decla-ration of Helsinki, and approved by the Institutional Ethics Review Board of Sichuan University (K2019059), West China Hospital; Sichuan University (756/2019; 27-09-2019); and Peking Union Medical College Hospital and was carried out in accordance with the tenets of the Declaration of Helsinki. The written informed consent was obtained from all participants before they were included in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chin, T.K.; Perloff, J.K.; Williams, R.G.; Jue, K.; Mohrmann, R. Isolated noncompaction of left ventricular myocardium. A study of eight cases. Circulation 1990, 82, 507–513. [Google Scholar] [CrossRef]
- Oechslin, E.; Attenhofer Jost, C.; Rojas, J.; Kaufmann, P.; Jenni, R. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: A distinct cardiomyopathy with poor prognosis. J. Am. Coll. Cardiol. 2000, 36, 493–500. [Google Scholar] [CrossRef]
- Stöllberger, C.; Finsterer, J.; Blazek, G. Left ventricular hypertrabeculation/noncompaction and association with additional cardiac abnormalities and neuromuscular disorders. Am. J. Cardiol. 2002, 90, 899–902. [Google Scholar] [CrossRef]
- Towbin, J.; Lorts, A.; Jefferies, J. Left ventricular non-compaction cardiomyopathy. Lancet 2015, 386, 813–825. [Google Scholar] [CrossRef]
- Brescia, S.; Rossano, J.; Pignatelli, R.; Jefferies, J.; Price, J.; Decker, J.; Denfield, S.; Dreyer, W.; Smith, O.; Towbin, J.; et al. Mortality and sudden death in pediatric left ventricular noncompaction in a tertiary referral center. Circulation 2013, 127, 2202–2208. [Google Scholar] [CrossRef] [PubMed]
- Stanton, C.; Bruce, C.; Connolly, H.; Brady, P.; Syed, I.; Hodge, D.; Asirvatham, S.; Friedman, P. Isolated left ventricular noncompaction syndrome. Am. J. Cardiol. 2009, 104, 1135–1138. [Google Scholar] [CrossRef] [PubMed]
- Jenni, R.; Oechslin, E.; Schneider, J.; Attenhofer Jost, C.; Kaufmann, P. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: A step towards classification as a distinct cardiomyopathy. Heart 2001, 86, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.; Selvanayagam, J.; Wiesmann, F.; Robson, M.; Francis, J.; Anderson, R.; Watkins, H.; Neubauer, S. Left ventricular non-compaction: Insights from cardiovascular magnetic resonance imaging. J. Am. Coll. Cardiol. 2005, 46, 101–105. [Google Scholar] [CrossRef]
- Jacquier, A.; Thuny, F.; Jop, B.; Giorgi, R.; Cohen, F.; Gaubert, J.; Vidal, V.; Bartoli, J.; Habib, G.; Moulin, G. Measurement of trabeculated left ventricular mass using cardiac magnetic resonance imaging in the diagnosis of left ventricular non-compaction. Eur. Heart J. 2010, 31, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, A.; Dabiesingh, D.; Bhumireddy, G.; Mohamed, A.; Asfour, A.; Briggs, W.; Ho, J.; Khan, S.; Grossman, A.; Klem, I.; et al. Prevalence and Prognostic Significance of Left Ventricular Noncompaction in Patients Referred for Cardiac Magnetic Resonance Imaging. Circ. Cardiovasc. Imaging 2017, 10, e006174. [Google Scholar] [CrossRef]
- Ross, S.; Jones, K.; Blanch, B.; Puranik, R.; McGeechan, K.; Barratt, A.; Semsarian, C. A systematic review and meta-analysis of the prevalence of left ventricular non-compaction in adults. Eur. Heart J. 2020, 41, 1428–1436. [Google Scholar] [CrossRef] [PubMed]
- Andreini, D.; Pontone, G.; Bogaert, J.; Roghi, A.; Barison, A.; Schwitter, J.; Mushtaq, S.; Vovas, G.; Sormani, P.; Aquaro, G.D.; et al. Long-Term Prognostic Value of Cardiac Magnetic Resonance in Left Ventricle Noncompaction: A Prospective Multicenter Study. J. Am. Coll. Cardiol. 2016, 68, 2166–2181. [Google Scholar] [CrossRef] [PubMed]
- Jefferies, J. Risk Prediction in a Debated Diagnosis: Is it Time for LVNC Guidelines? J. Am. Coll. Cardiol. 2021, 78, 663–665. [Google Scholar] [CrossRef] [PubMed]
- Casas, G.; Limeres, J.; Oristrell, G.; Gutierrez-Garcia, L.; Andreini, D.; Borregan, M.; Larrañaga-Moreira, J.; Lopez-Sainz, A.; Codina-Solà, M.; Teixido-Tura, G.; et al. Clinical Risk Prediction in Patients with Left Ventricular Myocardial Noncompaction. J. Am. Coll. Cardiol. 2021, 78, 643–662. [Google Scholar] [CrossRef]
- Halliday, B.; Baksi, A.; Gulati, A.; Ali, A.; Newsome, S.; Izgi, C.; Arzanauskaite, M.; Lota, A.; Tayal, U.; Vassiliou, V.; et al. Outcome in Dilated Cardiomyopathy Related to the Extent, Location, and Pattern of Late Gadolinium Enhancement. JACC Cardiovasc. Imaging 2019, 12, 1645–1655. [Google Scholar] [CrossRef]
- Mentias, A.; Raeisi-Giglou, P.; Smedira, N.; Feng, K.; Sato, K.; Wazni, O.; Kanj, M.; Flamm, S.; Thamilarasan, M.; Popovic, Z.; et al. Late Gadolinium Enhancement in Patients with Hypertrophic Cardiomyopathy and Preserved Systolic Function. J. Am. Coll. Cardiol. 2018, 72, 857–870. [Google Scholar] [CrossRef]
- Aquaro, G.; Perfetti, M.; Camastra, G.; Monti, L.; Dellegrottaglie, S.; Moro, C.; Pepe, A.; Todiere, G.; Lanzillo, C.; Scatteia, A.; et al. Cardiac MR with Late Gadolinium Enhancement in Acute Myocarditis with Preserved Systolic Function: ITAMY Study. J. Am. Coll. Cardiol. 2017, 70, 1977–1987. [Google Scholar] [CrossRef]
- Di Marco, A.; Anguera, I.; Schmitt, M.; Klem, I.; Neilan, T.; White, J.; Sramko, M.; Masci, P.; Barison, A.; Mckenna, P.; et al. Late Gadolinium Enhancement and the Risk for Ventricular Arrhythmias or Sudden Death in Dilated Cardiomyopathy: Systematic Review and Meta-Analysis. JACC Heart Fail. 2017, 5, 28–38. [Google Scholar] [CrossRef]
- Halliday, B.; Gulati, A.; Ali, A.; Guha, K.; Newsome, S.; Arzanauskaite, M.; Vassiliou, V.; Lota, A.; Izgi, C.; Tayal, U.; et al. Association Between Midwall Late Gadolinium Enhancement and Sudden Cardiac Death in Patients with Dilated Cardiomyopathy and Mild and Moderate Left Ventricular Systolic Dysfunction. Circulation 2017, 135, 2106–2115. [Google Scholar] [CrossRef]
- Grigoratos, C.; Barison, A.; Ivanov, A.; Andreini, D.; Amzulescu, M.; Mazurkiewicz, L.; De Luca, A.; Grzybowski, J.; Masci, P.; Marczak, M.; et al. Meta-Analysis of the Prognostic Role of Late Gadolinium Enhancement and Global Systolic Impairment in Left Ventricular Noncompaction. JACC Cardiovasc. Imaging 2019, 12, 2141–2151. [Google Scholar] [CrossRef]
- Bondarenko, O.; Beek, A.; Hofman, M.; Kühl, H.; Twisk, J.; van Dockum, W.; Visser, C.; van Rossum, A. Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR. J. Cardiovasc. Magn. Reson. 2005, 7, 481–485. [Google Scholar] [CrossRef] [PubMed]
- Schulz-Menger, J.; Bluemke, D.; Bremerich, J.; Flamm, S.; Fogel, M.; Friedrich, M.; Kim, R.; von Knobelsdorff-Brenkenhoff, F.; Kramer, C.; Pennell, D.; et al. Standardized image interpretation and post processing in cardiovascular magnetic resonance: Society for Cardiovascular Magnetic Resonance (SCMR) board of trustees task force on standardized post processing. J. Cardiovasc. Magn. Reson. 2013, 15, 35. [Google Scholar] [CrossRef] [PubMed]
- Augusto, J.; Eiros, R.; Nakou, E.; Moura-Ferreira, S.; Treibel, T.; Captur, G.; Akhtar, M.; Protonotarios, A.; Gossios, T.; Savvatis, K.; et al. Dilated cardiomyopathy and arrhythmogenic left ventricular cardiomyopathy: A comprehensive genotype-imaging phenotype study. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 326–336. [Google Scholar] [CrossRef]
- Alba, A.C.; Gaztanaga, J.; Foroutan, F.; Thavendiranathan, P.; Merlo, M.; Alonso-Rodriguez, D.; Vallejo-Garcia, V.; Vidal-Perez, R.; Corros-Vicente, C.; Barreiro-Perez, M.; et al. Prognostic Value of Late Gadolinium Enhancement for the Prediction of Cardiovascular Outcomes in Dilated Cardiomyopathy: An International, Multi-Institutional Study of the MINICOR Group. Circ. Cardiovasc. Imaging 2020, 13, e010105. [Google Scholar] [CrossRef] [PubMed]
- Disertori, M.; Rigoni, M.; Pace, N.; Casolo, G.; Masè, M.; Gonzini, L.; Lucci, D.; Nollo, G.; Ravelli, F. Myocardial Fibrosis Assessment by LGE Is a Powerful Predictor of Ventricular Tachyarrhythmias in Ischemic and Nonischemic LV Dysfunction: A Meta-Analysis. JACC Cardiovasc. Imaging 2016, 9, 1046–1055. [Google Scholar] [CrossRef] [PubMed]
- Habib, M.; Adler, A.; Fardfini, K.; Hoss, S.; Hanneman, K.; Rowin, E.; Maron, M.; Maron, B.; Rakowski, H.; Chan, R. Progression of Myocardial Fibrosis in Hypertrophic Cardiomyopathy: A Cardiac Magnetic Resonance Study. JACC Cardiovasc. Imaging 2021, 14, 947–958. [Google Scholar] [CrossRef]
- Muser, D.; Nucifora, G.; Pieroni, M.; Castro, S.; Casado Arroyo, R.; Maeda, S.; Benhayon, D.; Liuba, I.; Sadek, M.; Magnani, S.; et al. Prognostic Value of Non-Ischemic Ring-Like Left Ventricular Scar in Patients with Apparently Idiopathic Non-Sustained Ventricular Arrhythmias. Circulation 2021, 143, 1359–1373. [Google Scholar] [CrossRef]
- Mahrholdt, H.; Wagner, A.; Deluigi, C.; Kispert, E.; Hager, S.; Meinhardt, G.; Vogelsberg, H.; Fritz, P.; Dippon, J.; Bock, C.; et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation 2006, 114, 1581–1590. [Google Scholar] [CrossRef]
- Wan, J.; Zhao, S.; Cheng, H.; Lu, M.; Jiang, S.; Yin, G.; Gao, X.; Yang, Y. Varied distributions of late gadolinium enhancement found among patients meeting cardiovascular magnetic resonance criteria for isolated left ventricular non-compaction. J. Cardiovasc. Magn. Reson. 2013, 15, 20. [Google Scholar] [CrossRef]
- Kawel, N.; Nacif, M.; Arai, A.E.; Gomes, A.S.; Hundley, W.G.; Johnson, W.C.; Prince, M.R.; Stacey, R.B.; Lima, J.A.; Bluemke, D.A. Trabeculated (noncompacted) and compact myocardium in adults: The multi-ethnic study of atherosclerosis. Circ. Cardiovasc. Imaging 2012, 5, 357–366. [Google Scholar] [CrossRef]
- Aung, N.; Doimo, S.; Ricci, F.; Sanghvi, M.; Pedrosa, C.; Woodbridge, S.; Al-Balah, A.; Zemrak, F.; Khanji, M.; Munroe, P.; et al. Prognostic Significance of Left Ventricular Noncompaction: Systematic Review and Meta-Analysis of Observational Studies. Circ. Cardiovasc. Imaging 2020, 13, e009712. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).