Impact of Photon Counting Detector CT Derived Virtual Monoenergetic Images on the Diagnosis of Pulmonary Embolism
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Cohort
2.2. Image Acquisition
2.3. Post Processing
2.4. Objective Image Quality Evaluation
2.5. Subjective Image Quality Evaluation
2.6. Detection of Pulmonary Embolism
2.7. Statistical Analysis
3. Results
3.1. Patient Population
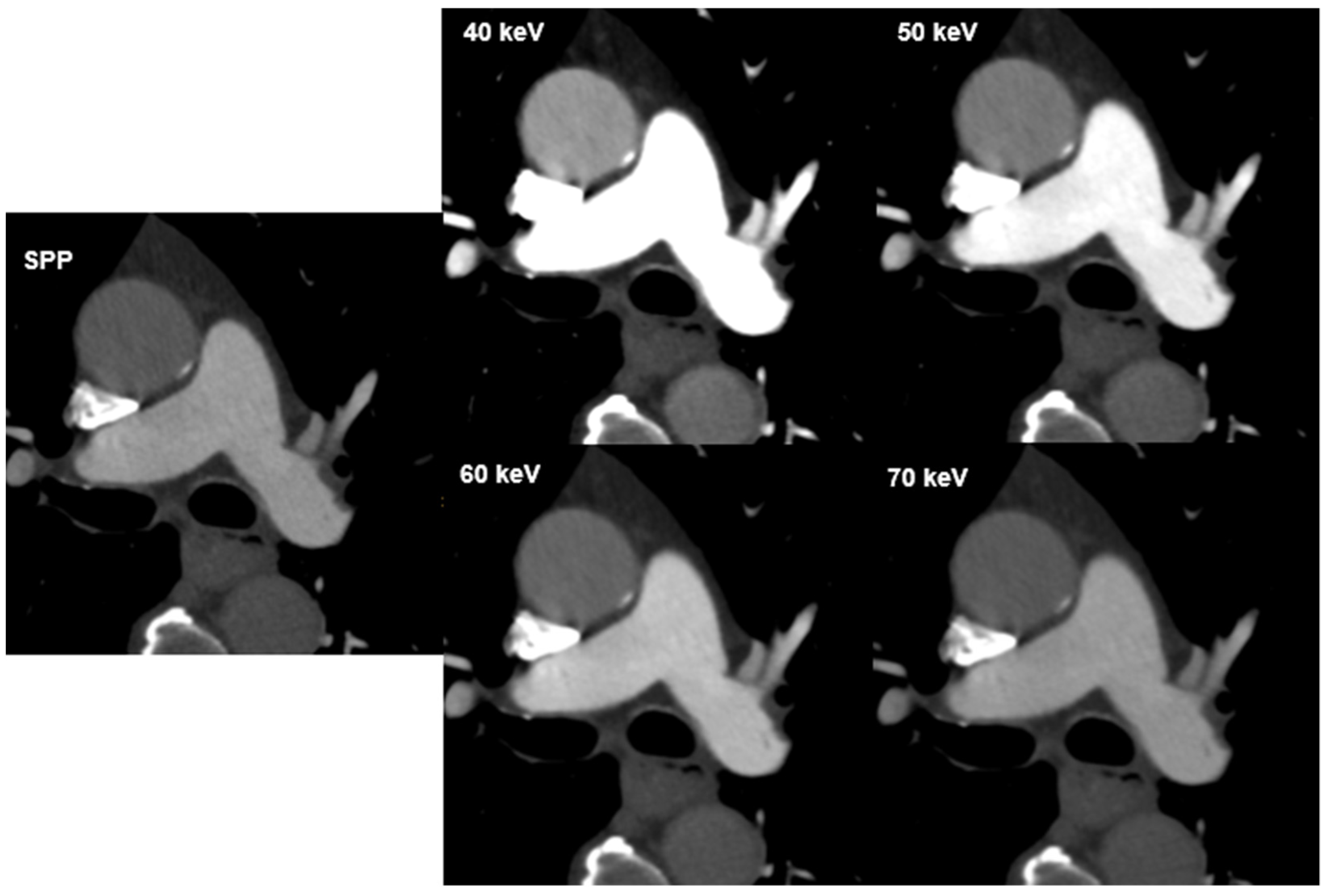
3.2. Objective Image Quality Evaluation
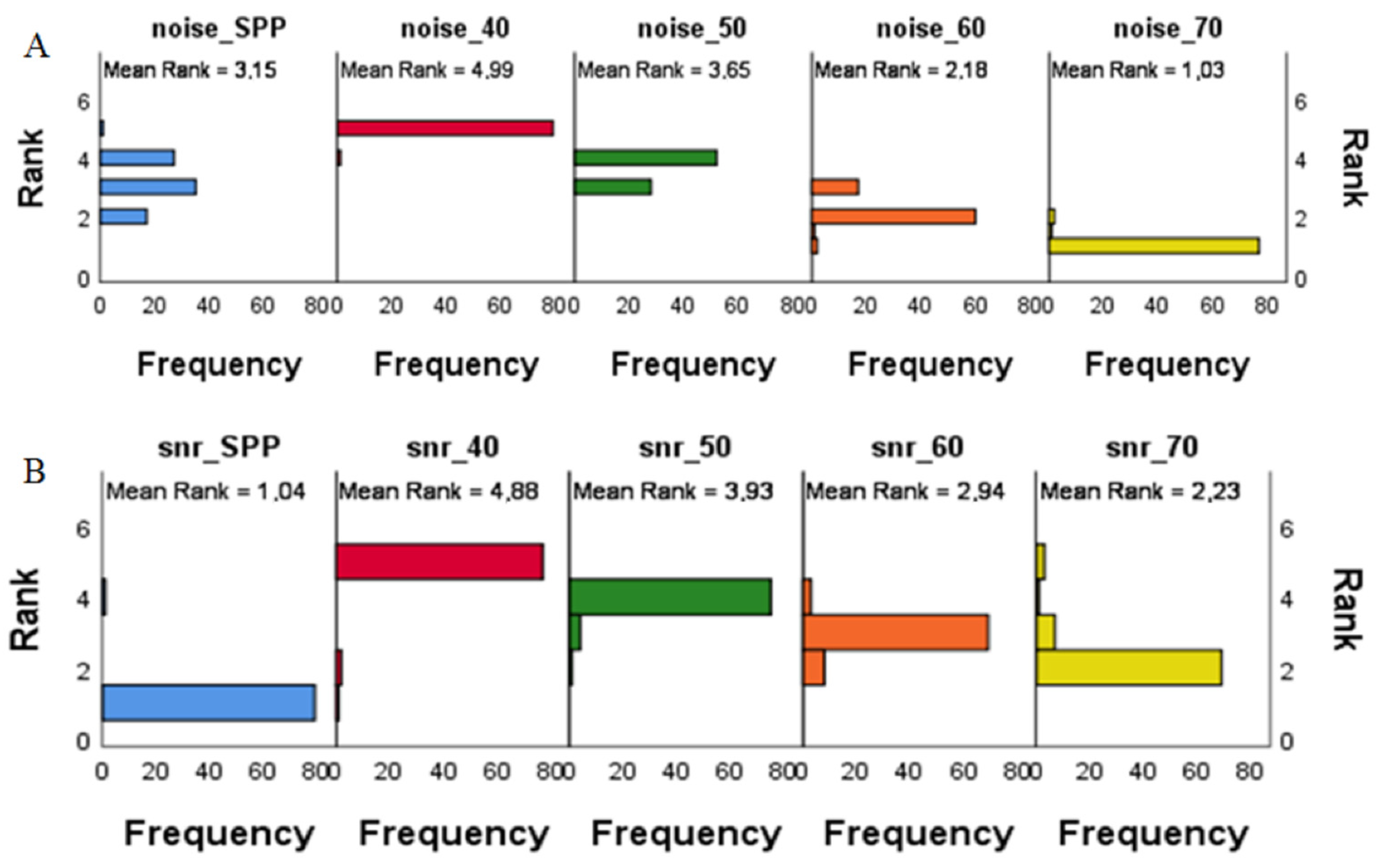
3.3. Subjective Image Quality Evaluation
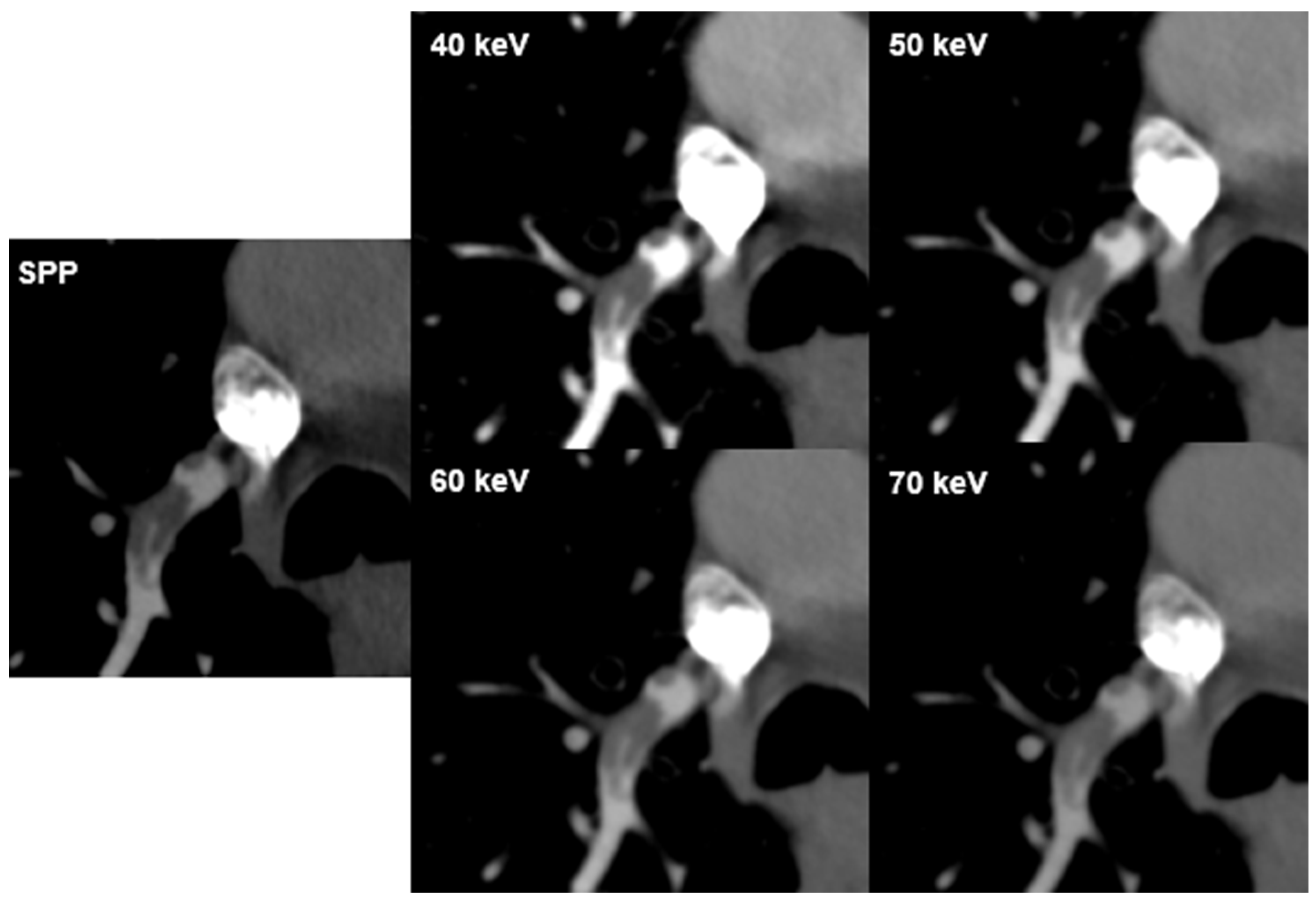
3.4. Detection of Pulmonary Embolism
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leithner, D.; Wichmann, J.L.; Vogl, T.J.; Trommer, J.; Martin, S.S.; Scholtz, J.-E.; Bodelle, B.; de Cecco, C.N.; Duguay, T.; Nance, J.W., Jr.; et al. Virtual monoenergetic imaging and iodine perfusion maps improve diagnostic accuracy of dual-energy computed tomography pulmonary angiography with suboptimal contrast attenuation. Investig. Radiol. 2017, 52, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.J.; Shim, J.; Lee, S.M.; Im, D.J.; Hur, J. Dual-energy CT for pulmonary embolism: Current and evolving clinical applications. Korean J. Radiol. 2021, 22, 1555–1568. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.J.E.; Wachsmann, J.; Chamarthy, M.R.; Panjikaran, L.; Tanabe, Y.; Rajiah, P. Imaging of acute pulmonary embolism: An update. Cardiovasc. Diagn Ther. 2018, 8, 225–243. [Google Scholar] [CrossRef]
- Meier, A.; Wurnig, M.; Desbiolles, L.; Leschka, S.; Frauenfelder, T.; Alkadhi, H. Advanced virtual monoenergetic images: Improving the contrast of dual-energy CT pulmonary angiography. Clin. Radiol. 2015, 70, 1244–1251. [Google Scholar] [CrossRef]
- Monti, C.B.; Zanardo, M.; Cozzi, A.; Schiaffino, S.; Spagnolo, P.; Secchi, F.; De Cecco, C.N.; Sardanelli, F. Dual-energy CT performance in acute pulmonary embolism: A meta-analysis. Eur. Radiol. 2021, 31, 6248–6258. [Google Scholar] [CrossRef]
- Abdellatif, W.; Ebada, M.A.; Alkanj, S.; Negida, A.; Murray, N.; Khosa, F.; Nicolaou, S. Diagnostic accuracy of dual-energy CT in detection of acute pulmonary embolism: A Systematic Review and Meta-Analysis. Can. Assoc. Radiol. J. 2020, 72, 285–292. [Google Scholar] [CrossRef]
- Rawat, K.S.; Buxi, T.B.S.; Sudarsan, H.; Yadav, A.; Ghuman, S.S. Current role of multi-detector computed tomography (MDCT) in diagnosis of pulmonary embolism. Curr. Radiol. Rep. 2014, 2, 68. [Google Scholar] [CrossRef]
- Dane, B.; Patel, H.; O’Donnell, T.; Girvin, F.; Brusca-Augello, G.; Alpert, J.B.; Niu, B.; Attia, M.; Babb, J.; Ko, J.P. Image quality on dual-energy CTPA virtual monoenergetic images: Quantitative and qualitative assessment. Acad. Radiol. 2018, 25, 1075–1086. [Google Scholar] [CrossRef]
- Albrecht, M.H.; Bickford, M.W.; Nance, J.W., Jr.; Zhang, L.; De Cecco, C.N.; Wichmann, J.L.; Vogl, T.J.; Schoepf, U.J. State-of-the-Art pulmonary CT angiography for acute pulmonary embolism. AJR 2017, 208, 495–504. [Google Scholar] [CrossRef]
- Rajiah, P.; Tanabe, Y.; Partovi, S.; Moore, A. State of the art: Utility of multi-energy CT in the evaluation of pulmonary vasculature. Int. J. Cardiovasc. Imaging 2019, 35, 1509–1524. [Google Scholar] [CrossRef]
- Ghandour, A.; Sher, A.; Rassouli, N.; Dhanantwari, A.; Rajiah, P. Evaluation of virtual monoenergetic images on pulmonary vasculature using the dual-layer detector-based spectral computed tomography. J. Comput. Assist. Tomogr. 2018, 42, 858–865. [Google Scholar] [CrossRef] [PubMed]
- Alkadhi, H.; Euler, A. The Future of Computed Tomography Personalized, Functional, and Precise. Investig. Radiol. 2020, 55, 545–555. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, K.; Petersilka, M.; Henning, A.; Shanblatt, E.R.; Schmidt, B.; Flohr, T.G.; Ferrero, A.; Baffour, F.; Diehn, F.E.; Yu, L.; et al. First Clinical Photon-counting Detector CT System: Technical Evaluation. Radiology 2022, 303, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Leng, S.; Jorgensen, S.M.; Li, Z.; Gutjahr, R.; Chen, B.; Halaweish, A.F.; Kappler, S.; Yu, L.; Ritman, E.L.; et al. Evaluation of conventional imaging performance in a research CT system with a photon-counting detector array. Phys. Med. Biol. 2016, 61, 1572–1595. [Google Scholar] [CrossRef]
- Flohr, T.; Ulzheimer, S.; Petersilka, M.; Schmidt, B. Basic principles and clinical potential of photon-counting detector CT. Chin. J. Acad. Radiol. 2020, 3, 19–34. [Google Scholar] [CrossRef]
- Rapp, J.B.; Biko, D.M.; White, A.M.; Ramirez-Suarez, K.I.; Otero, H.J. Spectral imaging in the pediatric chest: Past, present and future. Pediatr. Radiol. 2022, 52, 1910–1920. [Google Scholar] [CrossRef]
- Farhadi, F.; Rajagopal, J.R.; Nikpanah, M.; Sahbaee, P.; Malayeri, A.A.; Pritchard, W.F.; Samei, E.; Jones, E.C.; Chen, M.Y. Review of Technical Advancements and Clinical Applications of Photon-counting Computed Tomography in Imaging of the Thorax. J. Thorac. Imaging 2021, 36, 84–94. [Google Scholar] [CrossRef]
- Leng, S.; Rajendran, K.; Gong, H.; Zhou, W.; Halaweish, A.F.; Henning, A.; Kappler, S.; Baer, M.; Fletcher, J.G.; McCollough, C.H. 150 Micron Spatial Resolution using Photon Counting Detector CT Technology: Technical Performance and First Patient Images. Investig. Radiol. 2018, 53, 655–662. [Google Scholar] [CrossRef]
- Booij, R.; van der Werf, N.R.; Dijkshoorn, M.L.; van der Lugt, A.; van Straten, M. Assessment of iodine contrast-to-noise ratio in virtual monoenergetic images reconstructed from dual-source energy-integrating CT and photon-counting CT data. Diagnostics 2022, 12, 1467. [Google Scholar] [CrossRef]
- Grant, K.L.; Flohr, T.G.; Krauss, B.; Sedlmair, M.; Thomas, C.; Schmidt, B. Assessment of an advanced image-based technique to calculate virtual monoenergetic computed tomographic images from a dual-energy examination to improve contrast-to-noise ratio in examinations using iodinated contrast media. Investig. Radiol. 2014, 49, 586–592. [Google Scholar] [CrossRef]
- Zeng, Y.; Geng, D.; Zhang, J. Noise-optimized virtual monoenergetic imaging technology of the third-generation dual-source computed tomography and its clinical applications. Quant. Imaging Med. Surg. 2021, 11, 4627–4643. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, T.; Cicero, G.; Mazziotti, S.; Ascenti, G.; Albrecht, M.H.; Martin, S.S.; Othman, A.E.; Vogl, T.J.; Wichmann, J.L. Dual energy computed tomography virtual monoenergetic imaging: Technique and clinical applications. Br. J. Radiol. 2019, 92, 20180546. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, M.H.; Vogl, T.J.; Martin, S.S.; Nance, J.W.; Duguay, T.M.; Wichmann, J.L.; De Cecco, C.N.; Varga-Szemes, A.; van Assen, M.; Tesche, C.; et al. Review of clinical applications for virtual monoenergetic dual-energy CT. Radiology 2019, 293, 260–271. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Euler, A.; Higashigaito, K.; Mergen, V.; Sartoretti, T.; Zanini, B.; Schmidt, B.; Flohr, T.G.; Ulzheimer, S.; Eberhard, M.; Alkadhi, H. High-Pitch Photon-Counting Detector Computed Tomography Angiography of the Aorta Intraindividual Comparison to Energy-Integrating Detector Computed Tomography at Equal Radiation Dose. Investig. Radiol. 2022, 57, 115–121. [Google Scholar] [CrossRef]
- Leng, S.; Zhou, W.; Yu, Z.; Halaweish, A.; Krauss, B.; Schmidt, B.; Yu, L.; Kappler, S.; McCollough, C. Spectral performance of a whole body research photon counting detector CT: Quantitative accuracy in derived image sets. Phys. Med. Biol. 2017, 62, 7216–7232. [Google Scholar] [CrossRef]
- Leng, S.; Bruesewitz, M.; Tao, S.; Rajendran, K.; Halaweish, A.F.; Campeau, N.G.; Fletcher, J.G.; McCollough, C.H. Photon-counting Detector CT: System Design and Clinical Applications of an Emerging Technology. RadioGraphics 2019, 39, 729–743. [Google Scholar] [CrossRef]
- Si-Mohamed, S.A.; Miailhes, J.; Rodesch, P.-A.; Boccalini, S.; Lacombe, H.; Leitman, V. Spectral Photon-Counting CT Technology in Chest Imaging. J. Clin. Med. 2021, 10, 5757. [Google Scholar] [CrossRef]
- Apfaltrer, P.; Sudarski, S.; Schneider, D.; Nance, J.W., Jr.; Haubenreisser, H.; Fink, C.; Schoenberg, S.O.; Henzler, T. Value of monoenergetic low-kV dual energy CT datasets for improved image quality of CT pulmonary angiography. Eur. J. Radiol. 2014, 83, 322–328. [Google Scholar] [CrossRef]
- Bae, K.; Jeon, K.N.; Cho, S.B.; Park, S.E.; Moon, J.I.; Baek, H.J.; Choi, B.H. Improved Opacification of a Suboptimally Enhanced Pulmonary Artery in Chest CT: Experience Using a Dual-Layer Detector Spectral CT. AJR 2018, 210, 734–741. [Google Scholar] [CrossRef]
- Weiss, J.; Notohamiprodjo, M.; Bongers, M.; Schabel, C.; Mangold, S.; Nikolaou, K.; Bamberg, F.; Othman, A.E. Effect of Noise-Optimized Monoenergetic Postprocessing on Diagnostic Accuracy for Detecting Incidental Pulmonary Embolism in Portal-Venous Phase Dual-Energy Computed Tomography. Investig. Radiol. 2017, 52, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.; Notohamiprodjo, M.; Bongers, M.; Schabel, C.; Mangold, S.; Nikolaou, K.; Bamberg, F.; Othman, A.E. Noise-optimized monoenergetic post-processing improves visualization of incidental pulmonary embolism in cancer patients undergoing single-pass dual-energy computed tomography. Radiol. Med. 2017, 122, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, M.H.; Trommer, J.; Wichmann, J.L.; Scholtz, J.-E.; Martin, S.S.; Lehnert, T.; Vogl, T.J.; Bodelle, B. Comprehensive Comparison of Virtual Monoenergetic and Linearly Blended Reconstruction Techniques in Third-Generation Dual-Source Dual-Energy Computed Tomography Angiography of the Thorax and Abdomen. Investig. Radiol. 2016, 51, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Jungblut, L.; Kronenberg, D.; Mergen, V.; Higashigaito, K.; Schmidt, B.; Euler, A.; Alkadhi, H.; Frauenfelder, T.; Martini, K. Impact of Contrast Enhancement and Virtual Monoenergetic Image Energy Levels on Emphysema Quantification Experience with Photon-Counting Detector Computed Tomography. Investig. Radiol. 2022, 57, 359–365. [Google Scholar] [CrossRef]
- Albrecht, M.H.; Trommer, J.; Wichmann, J.L.; Scholtz, J.-E.; Martin, S.S.; Lehnert, T.; Vogl, T.J.; Bodelle, B. First Performance Evaluation of an Artificial Intelligence-Based Computer-Aided Detection System for Pulmonary Nodule Evaluation in Dual-Source Photon-Counting Detector CT at Different Low-Dose Levels. Investig. Radiol. 2022, 57, 108–114. [Google Scholar]
- Stals, M.A.M.; Takada, T.; Kraaijpoel, N.; van Es, N.; Büller, H.R.; Courtney, D.M.; Freund, Y.; Galipienzo, J.; Le Gal, G.; Ghanima, W.; et al. Safety and Efficiency of Diagnostic Strategies for Ruling Out Pulmonary Embolism in Clinically Relevant Patient Subgroups: A Systematic Review and Individual-Patient Data Meta-analysis. Ann. Intern. Med. 2022, 175, 244–255. [Google Scholar] [CrossRef]
| PE | n (%) |
|---|---|
| Central | 2 (5.7) |
| Lobar | 18 (51.4) |
| Segmental | 19 (54.3) |
| Subsegmental | 23 (65.7) |
| Unilateral | 18 (51.4) |
| Bilateral | 17 (48.6) |
| Imaging Parameter | SPP | 40 keV | 50 keV | 60 keV | 70 keV |
|---|---|---|---|---|---|
| Image noise median CI95% [range] | 20.85 [19.5–21.80] | 27.25 [25.80–29.85] | 21.70 [20.60–22.70] | 17.65 [17.25–19.00] | 15.60 [14.30–16.45] |
| Signal median CI95% [range] | 358.83 [340.67–393.66] | 1053.50 [976.01–1146.33] | 703.16 [655.36–748.00] | 488.33 [459.67–536.33] | 358.83 [341.00–394.65] |
| SNR median CI95% [range] | 17.78 [14.29–20.13] | 37.56 [32.48–40.48] | 33.18 [27.83–35.08] | 28.06 [23.60–30.78] | 23.61 [19.84–27.04] |
| SNR | pa | Image Noise | pa |
|---|---|---|---|
| 40/50 | 0.001 | 40/50 | 0.000 |
| 50/60 | 0.001 | 50/60 | 0.000 |
| 60/70 | 0.044 | 60/70 | 0.000 |
| 40/70 | 0.000 | 40/70 | 0.000 |
| 50/70 | 0.000 | 50/70 | 0.000 |
| 40/60 | 0.000 | 40/60 | 0.000 |
| Imaging Parameter | VMI Energies, keV | R1 (Mean, Range) | R2 (Mean, Range) | Cohen’s Kappa (k) | p | n |
|---|---|---|---|---|---|---|
| Image noise | 40 | 4.1 [3–5] | 4.1 [3–5] | 0.584 | 0.000 | 80 |
| 50 | 4.2 [3–5] | 4.3 [3–5] | 0.681 | 0.000 | 80 | |
| 60 | 4.4 [3–5] | 4.4 [3–5] | 0.644 | 0.000 | 80 | |
| 70 | 4.6 [3–5] | 4.6 [3–5] | 0.682 | 0.000 | 80 | |
| SPP | 4.8 [3–5] | 4.6 [3–5] | 0.644 | 0.000 | 80 | |
| Vessel attenuation | 40 | 5.0 [4–5] | 5.0 [4–5] | 1.000 | 0.000 | 80 |
| 50 | 4.9 [4–5] | 4.9 [4–5] | 1.000 | 0.000 | 80 | |
| 60 | 4.5 [3–5] | 4.5 [3–5] | 0.977 | 0.000 | 80 | |
| 70 | 4.2 [3–5] | 4.1 [3–5] | 0.899 | 0.000 | 80 | |
| SPP | 4.0 [3–5] | 4.1 [3–5] | 0.593 | 0.000 | 80 | |
| Vessel sharpness | 40 | 4.7 [3–5] | 4.8 [4–5] | 0717 | 0.000 | 80 |
| 50 | 4.5 [3–5] | 4.7 [4–5] | 0.794 | 0.000 | 80 | |
| 60 | 4.3 [4–5] | 4.7 [4–5] | 0.830 | 0.000 | 80 | |
| 70 | 4.2 [3–5] | 4.6 [3–5] | 0.783 | 0.000 | 80 | |
| SPP | 4.2 [3–5] | 4.3 [3–5] | 0.783 | 0.000 | 80 | |
| PE visualization | 40 | 4.5 [3–5] | 4.4 [3–5] | 0.515 | 0.001 | 35 |
| 50 | 4.7 [4–5] | 4.7 [4–5] | 0.612 | 0.000 | 35 | |
| 60 | 4.1 [3–5] | 3.8 [3–5] | 0.392 | 0.001 | 35 | |
| 70 | 3.7 [2–5] | 3.5 [2–4] | 0.373 | 0.001 | 35 | |
| SPP | 3.8 [2–5] | 3.4 [2–4] | 0.373 | 0.000 | 80 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yalynska, T.; Polacin, M.; Frauenfelder, T.; Martini, K. Impact of Photon Counting Detector CT Derived Virtual Monoenergetic Images on the Diagnosis of Pulmonary Embolism. Diagnostics 2022, 12, 2715. https://doi.org/10.3390/diagnostics12112715
Yalynska T, Polacin M, Frauenfelder T, Martini K. Impact of Photon Counting Detector CT Derived Virtual Monoenergetic Images on the Diagnosis of Pulmonary Embolism. Diagnostics. 2022; 12(11):2715. https://doi.org/10.3390/diagnostics12112715
Chicago/Turabian StyleYalynska, Tetyana, Malgorzata Polacin, Thomas Frauenfelder, and Katharina Martini. 2022. "Impact of Photon Counting Detector CT Derived Virtual Monoenergetic Images on the Diagnosis of Pulmonary Embolism" Diagnostics 12, no. 11: 2715. https://doi.org/10.3390/diagnostics12112715
APA StyleYalynska, T., Polacin, M., Frauenfelder, T., & Martini, K. (2022). Impact of Photon Counting Detector CT Derived Virtual Monoenergetic Images on the Diagnosis of Pulmonary Embolism. Diagnostics, 12(11), 2715. https://doi.org/10.3390/diagnostics12112715







