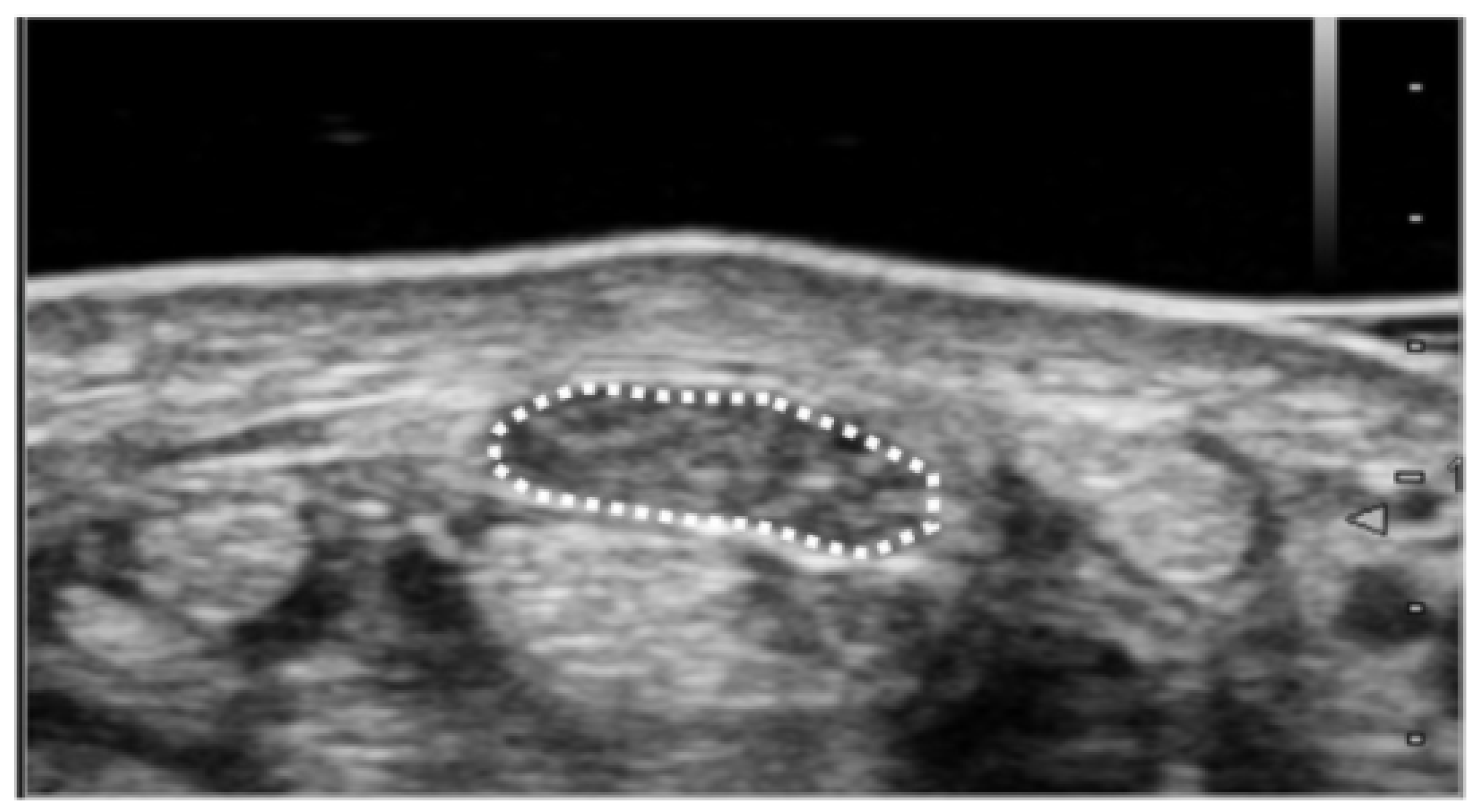
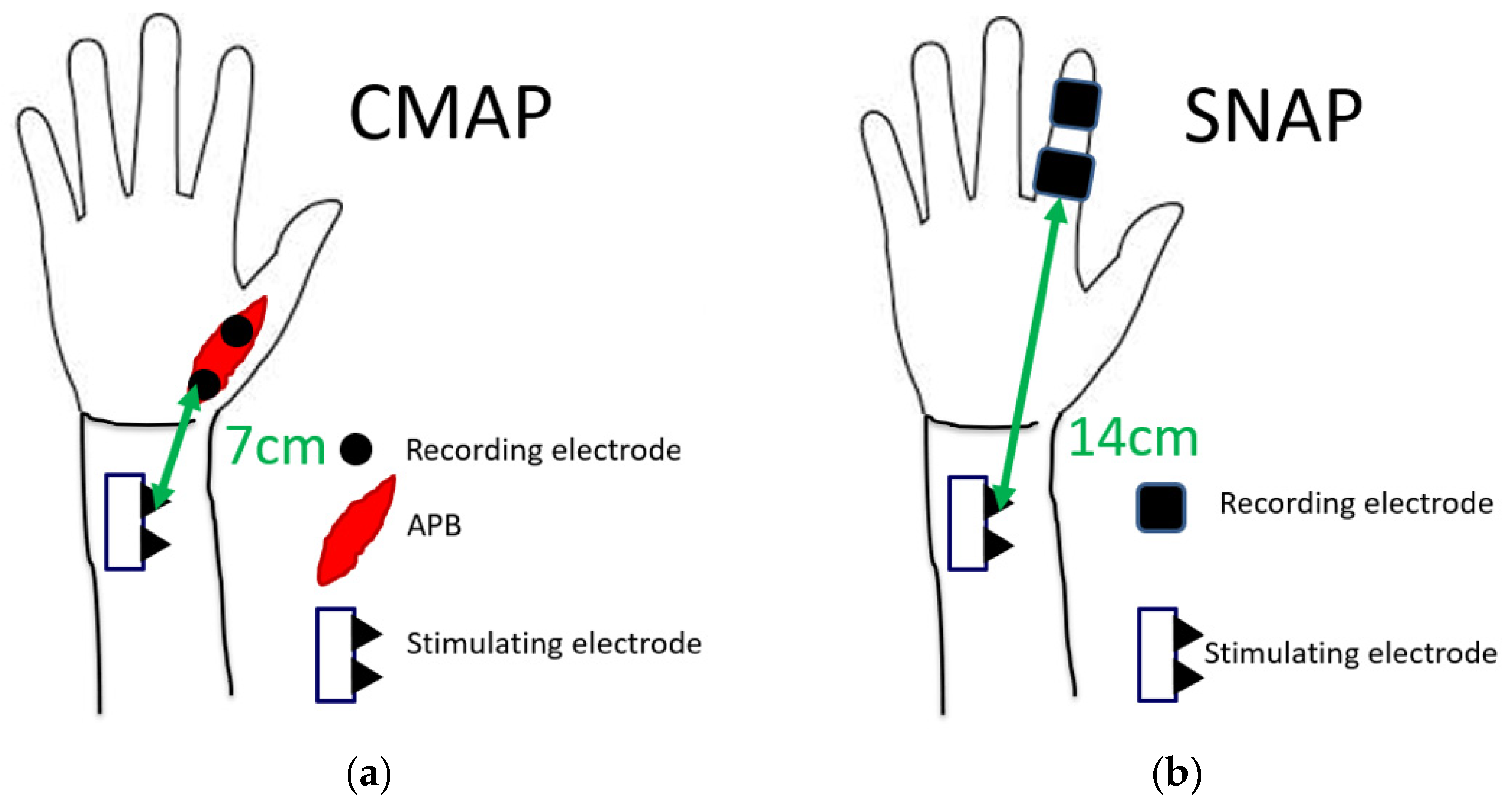
Clinical Relevance of Ultrasonographic and Electrophysiological Findings of the Median Nerve in Unilateral Carpal Tunnel Syndrome Patients
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Robert, M.S.; Robert, R.S.; Thomas, B.F.; Donna, B.S.; Wahida, K.S. The Value of Diagnostic Testing in Carpal Tunnel Syndrome. J. Hand Surg. 1999, 24, 704–714. [Google Scholar] [CrossRef]
- Stevens, J.C.; Smith, B.E.; Weaver, A.L.; Bosch, E.P.; Deen Jr, H.G.; Wilkens, J.A. Symptoms of 100 patients with electromyographically verified carpal tunnel syndrome. Muscle Nerve 1999, 22, 1448–1456. [Google Scholar] [CrossRef]
- Padua, L.; Lo, M.M.; Valente, E.M.; Tonali, P.A. A useful electrophysiologic parameter for diagnosis of carpal tunnel syndrome. Muscle Nerve 1996, 19, 48–53. [Google Scholar] [CrossRef]
- Pinilla, I.; Martin-Hervas, C.; Sordo, G.; Santiago, S. The usefulness of ultrasonography in the diagnosis of carpal tunnel syndrome. J. Hand Surg. Eur. Vol. 2008, 33, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Imaeda, T.; Toh, S.; Nakao, Y.; Nishida, J.; Hirata, H.; Ijichi, M.; Kohri, C.; Nagano, A. Validation of the Japanese Society for Surgery of the Hand version of the Carpal Tunnel Syndrome Instrument. J. Orthop. Sci. 2007, 12, 14–21. [Google Scholar] [CrossRef] [Green Version]
- Jablecki, C.K.; Andary, M.T.; Floeter, M.K.; Miller, R.G.; Quartly, C.A.; Vennix, M.J.; Wilson, J.R. Practice parameter: Electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology 2002, 58, 1589–1592. [Google Scholar] [CrossRef] [Green Version]
- Fowler, J.R.; Cipolli, W.; Hanson, T. A comparison of three diagnostic tests for carpal tunnel syndrome using latent class analysis. J. Bone Jt. Surg. Am. 2015, 97, 1958–1961. [Google Scholar] [CrossRef]
- Ooi, C.C.; Wong, S.K.; Tan, A.B.H.; Chin, A.Y.H.; Bakar, R.A.; Goh, S.Y.; Mohan, P.C.; Yap, R.T.J.; Png, M.A. Diagnostic criteria of carpal tunnel syndrome using high-resolution ultrasonography: Correlation with nerve conduction studies. Skelet. Radiol 2014, 43, 1387–1394. [Google Scholar] [CrossRef]
- Nakamichi, K.; Tachibana, S. Unilateral carpal tunnel syndrome and space-occupying lesions. J. Hand Surg. Br. 1993, 18, 748–749. [Google Scholar] [CrossRef]
- Nakamichi, K. Ultrasonography for the management of carpal tunnel syndrome. Clin. Neurol. 2013, 23, 1217–1219. [Google Scholar] [CrossRef]
- Obuchowicz, R.; Kruszynska, J.; Strzelecki, M. Classifying median nerves in carpal tunnel syndrome: Ultrasound image analysis. Biocybern. Biomed. Eng. 2021, 41, 335–351. [Google Scholar] [CrossRef]
- Miwa, T.; Miwa, H. Ultrasonography of carpal tunnel syndrome: Clinical significance and limitations in elderly patients. Intern. Med. 2011, 50, 2157–2161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, I.J.; Chang, K.V.; Lou, Y.M.; Wu, W.T.; Özçakar, L. Can ultrasound imaging be used for the diagnosis of carpal tunnel syndrome in diabetic patients? A systemic review and network meta-analysis. J. Neurol. 2020, 267, 1887–1895. [Google Scholar] [CrossRef] [PubMed]
- Byra, M.; Hentzen, E.; Du, J.; Andre, M.; Chang, E.Y.; Shah, S. Assessing the performance of morphologic and echogenic features in median nerve ultrasound for carpal tunnel syndrome diagnosis. J. Ultrasound Med. 2020, 39, 1165–1174. [Google Scholar] [CrossRef]
- Fowler, J.R.; Gaughan, J.P.; Ilyas, A.M. The sensitivity and specificity of ultrasound for the diagnosis of carpal tunnel syndrome: A meta-analysis. Clin. Orthop. Relat. Res. 2011, 469, 1089–1094. [Google Scholar] [CrossRef] [Green Version]
- Ozsoy-Unubol, T.; Bahar-Ozdemir, Y.; Yagci, I. Diagnosis and grading of carpal tunnel syndrome with quantitative ultrasound: Is it possible? J. Clin. Neurosci. 2020, 75, 25–29. [Google Scholar] [CrossRef]
- Fujimoto, K.; Kanchiku, T.; Kido, K.; Imajo, Y.; Funaba, M.; Taguchi, T. Diagnosis of severe carpal tunnel syndrome using nerve conduction study and ultrasonography. Ultrasound Med. Biol. 2015, 41, 2575–25780. [Google Scholar] [CrossRef]
- Padua, L.; Coraci, D.; Erra, C.; Pazzaglia, C.; Paolasso, I.; Loreti, C.; Caliandro, P.; Hosbon-Webb, L.D. Carpal tunnel syndrome: Clinical features, diagnosis, and management. Lancet Neurol. 2016, 15, 1273–1284. [Google Scholar] [CrossRef]
- Cartwright, M.S.; Hobson-Webb, L.D.; Boon, A.J.; Alter, K.E.; Hunt, C.H.; Flores, V.H.; Werner, R.A.; Shook, S.J.; Thomas, T.D.; Primack, S.J.; et al. Evidence-based guideline: Neuromuscular ultrasound for the diagnosis of carpal tunnel syndrome. Muscle Nerve 2012, 46, 287–293. [Google Scholar] [CrossRef] [Green Version]
- Nakamichi, K.; Tachibana, S. Enlarged median nerve in idiopathic carpal tunnel syndrome. Muscle Nerve 2000, 23, 1713–1718. [Google Scholar] [CrossRef]
- Audrey, J.T.N.; Ramya, C.; Prakash, A.; Mogali, S.R. A systematic review: Normative reference values of the median nerve cross-sectional area using ultrasonography in healthy individuals. Sci. Rep. 2022, 12, 9217. [Google Scholar] [CrossRef]
- Nakamichi, K.; Tachibana, S. Ultrasonographic measurement of median nerve cross-sectional area in idiopathic carpal tunnel syndrome: Diagnostic accuracy. Muscle Nerve 2002, 26, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Hobson-Webb, L.D.; Massey, J.M.; Juel, V.C.; Sandres, D.B. The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clin. Neurophysiol. 2008, 119, 1353–1357. [Google Scholar] [CrossRef] [PubMed]
- Venderschueren, G.A.; Meys, V.E.; Beekman, R. Doppler sonography for the diagnosis of carpal tunnel syndrome: A critical review. Muscle Nerve 2014, 50, 159–163. [Google Scholar] [CrossRef]
- Mallouhi, A.; Pülzl, P.; Trieb, T.; Piza, H.; Bodner, G. Predictors of carpal tunnel syndrome: Accuracy of gray-scale and color Doppler sonography. AJR Am. J. Roentgenol. 2006, 186, 1240–1245. [Google Scholar] [CrossRef]
- Tagliafico, A.S. Peripheral nerve imaging: Not only crosssectional area. World J. Radiol. 2016, 8, 726–728. [Google Scholar] [CrossRef]
- El-Hajj, T.; Tohme, R.; Sawaya, R. Changes in electrophysiological parameters after surgery for the carpal tunnel syndrome. J. Clin. Neurophysiol. 2010, 27, 224–226. [Google Scholar] [CrossRef]
- Rivner, M.H.; Swift, T.R.; Malik, K. Influence of age and height on nerve conduction. Muscle Nerve 2001, 24, 1134–1141. [Google Scholar] [CrossRef]
- Stetson, D.S.; Albers, J.W.; Silverstein, B.A.; Wolfe, R.A. Effects of age, sex, and anthropometric factors on nerve conduction measures. Muscle Nerve 1992, 15, 1095–1104. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.R.; Chang, W.N.; Chang, H.W.; Tsai, N.W.; Lu, C.H. Effects of age, gender, height, and weight on late responses and nerve conduction study parameters. Acta Neurol. Taiwan 2009, 18, 242–249. [Google Scholar]
- Ludin, H.P.; Bayeler, F. Temperature dependence of normal sensory nerve action potentials. J. Neurol. 1977, 216, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Werner, R.A.; Andary, M. Carpal tunnel syndrome: Pathophysiology and clinical neurophysiology. Clin. Neurophysiol. 2002, 113, 1373–1381. [Google Scholar] [CrossRef]
- Nathan, P.A.; Takigawa, K.; Keniston, R.C.; Meadows, K.D.; Lockwood, R.S. Slowing of sensory conduction of the median nerve and carpal tunnel syndrome in Japanese and American industrial workers. J. Hand Surg. Br. 1994, 19, 30–34. [Google Scholar] [CrossRef]
- Hirani, S. A study to further develop and refine carpal tunnel syndrome (CTS) nerve conduction grading tool. BMC Musculoskelet. Disord. 2019, 20, 581. [Google Scholar] [CrossRef] [Green Version]
- Sonoo, M.; Menkes, D.L.; Bland, J.D.P.; Burke, D. Nerve conduction studies and EMG in carpal tunnel syndrome: Do they add value? Clin. Neurophysiol. 2018, 3, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Wild, D.K.; Seligman, P.J.; Halperin, W.E.; Behrens, V.J.; Putz-Andeson, V. Prevalence and work-relatedness of self-reported carpal tunnel syndrome among U.S. workers: Analysis of the Occupational Health Supplement data of 1988 National Health Interview Survey. Am. J. Ind. Med. 1995, 27, 451–470. [Google Scholar] [CrossRef] [PubMed]
- Koskimies, K.; Färkkilä, M.; Pyykkö, I.; Jäntti, V.; Aatola, S.; Starck, J.; Inaba, R. Carpal tunnel syndrome in vibration disease. Br. J. Ind. Med. 1990, 47, 411–416. [Google Scholar] [CrossRef] [Green Version]
- Osorio, A.M.; Ames, R.G.; Jones, J.; Castorina, J.; Rempel, D.; Estrin, W.; Thompson, D. Carpal tunnel syndrome among grocery store workers. Am. J. Ind. Med. 1994, 25, 229–245. [Google Scholar] [CrossRef]
- Isolani, L.; Bonfiglioli, R.; Raffi, G.B.; Violante, F.S. Different case definitions to describe the prevalence of occupational carpal tunnel syndrome in meat industry workers. Int. Arch. Occup. Environ. Health 2002, 75, 229–234. [Google Scholar] [CrossRef]
- Hamann, C.; Werner, R.A.; Franzblau, A.; Rodgers, P.A.; Siew, C.; Gruinger, S. Prevalence of carpal tunnel syndrome and median mononeuropathy among dentists. J. Am. Dent. Assoc. 2001, 132, 163–170. [Google Scholar] [CrossRef]
- Neary, D.; Ochoa, J.; Gilliatt, R.W. Sub-clinical entrapment neuropathy in man. J. Neurol. Sci. 1975, 24, 283–298. [Google Scholar] [CrossRef]
- Bouche, P.; Cattelin, F.; Saint-Jean, O.; Léger, J.M.; Queslati, S.; Guez, D.; Moulonguet, A.; Brault, Y.; Aquino, J.P.; Simunek, P. Clinical and electrophysiological study on the peripheral nerves system in the elderly. J. Neurol. 1993, 240, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Verdú, E.; Ceballos, D.; Vilches, J.J.; Navarro, X. Influence of aging on peripheral nerve function and regeneration. J. Peripher. Nerv. Syst. 2000, 5, 191–208. [Google Scholar] [CrossRef]
- Futami, T.; Kobayashi, A.; Ukita, T.; Endoh, T.; Fujita, T. Carpal tunnel syndrome; Its natural history. Hand Surg. 1997, 2, 129–130. [Google Scholar] [CrossRef]

| Gender | Male | 22 |
| Female | 39 | |
| Age | Ave (SD) | 65.3 ± 11.2 |
| Min | 30 | |
| Max | 89 | |
| Height (cm) | Ave (SD) | 157.6 ± 8.6 |
| Weight (kg) | Ave (SD) | 61.3 ± 11.9 |
| BMI | Ave (SD) | 24.6 ± 3.8 |
| Work Status (%) | Manual work | 44.8 |
| Desk work | 13.8 | |
| Unemployed | 41.4 | |
| Disease period (%) | Less than 3 months | 38.6 |
| 3 months to 1 year | 33.3 | |
| More than 1 year | 28.1 | |
| APB strength (MMT, %) | 0~1 | 19.3 |
| 2~3 | 40.4 | |
| 4~5 | 40.4 |
| Affected Side | Unaffected Side | AUC | Cut-Off Values | |
|---|---|---|---|---|
| Cross-sectional area (mm2) | 14.2 ± 4.0 | 11.3 ± 2.7 | 0.74 | 11.9 |
| Distal Latency for CMAP (ms) | 6.6 ± 1.8 | 4.4 ± 0.9 | 0.88 | 5.1 |
| Distal Latency for SNAP (ms) | 3.5 ± 0.8 | 2.8 ± 0.4 | 0.73 | 3.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kudo, T.; Yoshii, Y.; Hara, Y.; Ogawa, T.; Ishii, T. Clinical Relevance of Ultrasonographic and Electrophysiological Findings of the Median Nerve in Unilateral Carpal Tunnel Syndrome Patients. Diagnostics 2022, 12, 2799. https://doi.org/10.3390/diagnostics12112799
Kudo T, Yoshii Y, Hara Y, Ogawa T, Ishii T. Clinical Relevance of Ultrasonographic and Electrophysiological Findings of the Median Nerve in Unilateral Carpal Tunnel Syndrome Patients. Diagnostics. 2022; 12(11):2799. https://doi.org/10.3390/diagnostics12112799
Chicago/Turabian StyleKudo, Takamasa, Yuichi Yoshii, Yuki Hara, Takeshi Ogawa, and Tomoo Ishii. 2022. "Clinical Relevance of Ultrasonographic and Electrophysiological Findings of the Median Nerve in Unilateral Carpal Tunnel Syndrome Patients" Diagnostics 12, no. 11: 2799. https://doi.org/10.3390/diagnostics12112799
APA StyleKudo, T., Yoshii, Y., Hara, Y., Ogawa, T., & Ishii, T. (2022). Clinical Relevance of Ultrasonographic and Electrophysiological Findings of the Median Nerve in Unilateral Carpal Tunnel Syndrome Patients. Diagnostics, 12(11), 2799. https://doi.org/10.3390/diagnostics12112799





