Maxillary Sinus Dimensions in Skeletal Class I Chinese Population with Different Vertical Skeletal Patterns: A Cone-Beam Computed Tomography Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Sample Size Calculation
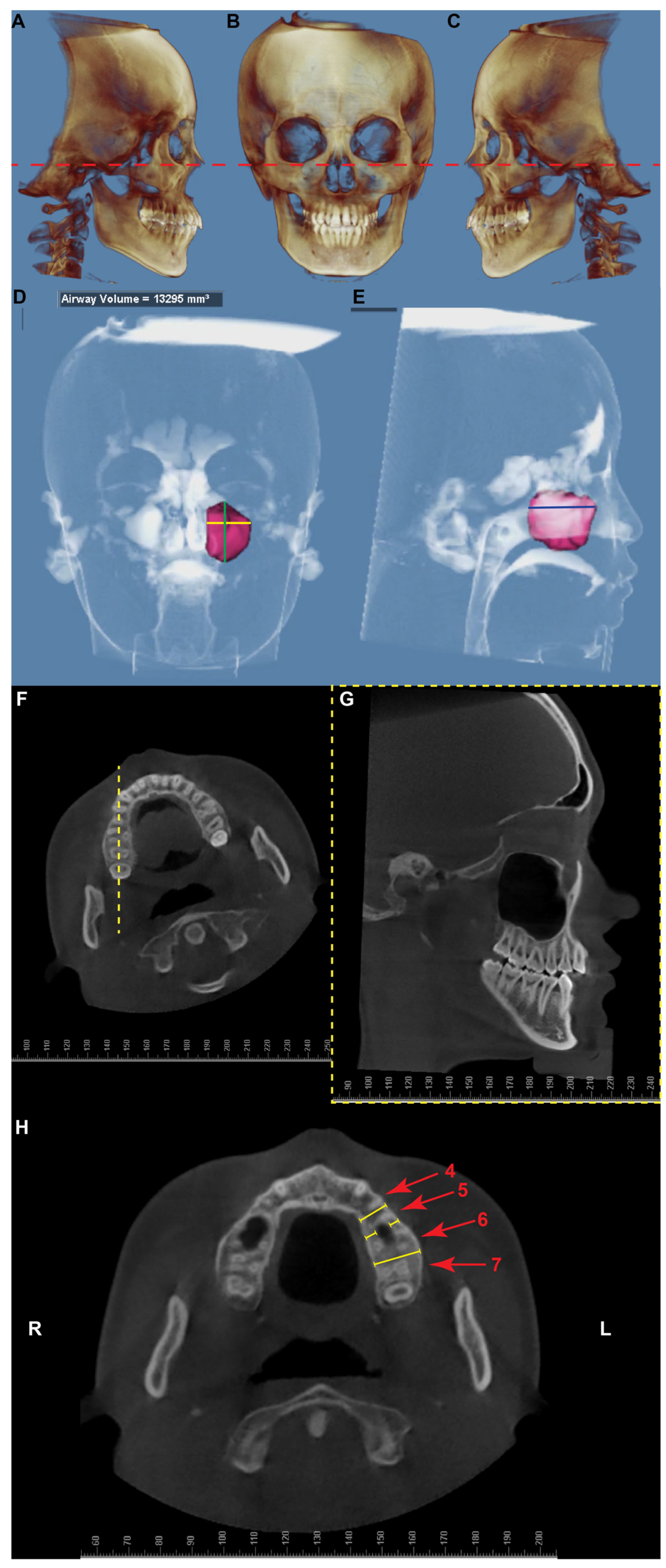
2.3. Maxillary Sinus Size and Location Measurements
2.4. Statistical Analysis
3. Results
3.1. Patient Demographic Information
3.2. Comparison of Maxillary Sinus Size
3.3. Maxillary Sinus Floor to the Alveolar Bone Crest
3.4. Maxillary Sinus Walls to the Buccal and Palatal Alveolar Bone Cortices at Different Vertical Levels
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baker, E.W.; Schuenke, M.; Schulte, E. Head and Neck Anatomy for Dental Medicine; Thieme: New York, NY, USA, 2011. [Google Scholar]
- Iwanaga, J.; Wilson, C.; Lachkar, S.; Tomaszewski, K.A.; Walocha, J.A.; Tubbs, R.S. Clinical anatomy of the maxillary sinus: Application to sinus floor augmentation. Anat. Cell Biol. 2019, 52, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, B.; Shrestha, R.; Lin, T.; Lu, Y.; Lu, H.; Mai, Z.; Chen, L.; Chen, Z.; Ai, H. Evaluation of maxillary sinus volume in different craniofacial patterns: A CBCT study. Oral Radiol. 2021, 37, 647–652. [Google Scholar] [CrossRef] [PubMed]
- Horiuchi, A.; Hotokezaka, H.; Kobayashi, K. Correlation between cortical plate proximity and apical root resorption. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H. Temporary Anchorage Devices in Clinical Orthodontics; Wiley: Hoboken, NJ, USA, 2020. [Google Scholar]
- Syverson, A.; Li, C.; Zheng, Z.; Proskurnin, E.; Chung, C.H.; Zou, M. Maxillary sinus dimensions in skeletal class II population with different vertical skeletal patterns. Clin. Oral Investig. 2022, 26, 5045–5060. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Farronato, M.; Bellincioni, F.; Annibale, A.; Machetti, J.; Abate, A.; Cavagnetto, D. Three-Dimensional Evaluation of Maxillary Sinus Changes in Growing Subjects: A Retrospective Cross-Sectional Study. Materials 2020, 13, 1007. [Google Scholar] [CrossRef] [PubMed]
- Aktuna Belgin, C.; Colak, M.; Adiguzel, O.; Akkus, Z.; Orhan, K. Three-dimensional evaluation of maxillary sinus volume in different age and sex groups using CBCT. Eur. Arch. Otorhinolaryngol. 2019, 276, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Endo, T.; Abe, R.; Kuroki, H.; Kojima, K.; Oka, K.; Shimooka, S. Cephalometric evaluation of maxillary sinus sizes in different malocclusion classes. Odontology 2010, 98, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.; Choi, S.H.; Cha, J.Y.; Lee, K.J.; Hwang, C.J. Retrospective study of maxillary sinus dimensions and pneumatization in adult patients with an anterior open bite. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Göymen, M.; Büyüknacar, G.B.; Güleç, A. Effect of Vertical Growth Pattern on Maxillary and Frontal Sinus Sizes. Eur. J. Ther. 2019, 25, 197–200. [Google Scholar] [CrossRef]
- Kosumarl, W.; Patanaporn, V.; Jotikasthira, D.; Janhom, A. Distances from the root apices of posterior teeth to the maxillary sinus and mandibular canal in patients with skeletal open bite: A cone-beam computed tomography study. Imaging Sci. Dent. 2017, 47, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Oksayan, R.; Sokucu, O.; Yesildal, S. Evaluation of maxillary sinus volume and dimensions in different vertical face growth patterns: A study of cone-beam computed tomography. Acta Odontol. Scand. 2017, 75, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Kadioglu, O.; Currier, G.F. Craniofacial 3D Imaging: Current Concepts in Orthodontics and Oral and Maxillofacial Surgery; Springer International Publishing: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Cao, L.; Li, J.; Yang, C.; Hu, B.; Zhang, X.; Sun, J. High-efficiency treatment with the use of traditional anchorage control for a patient with Class II malocclusion and severe overjet. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 411–420. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, H.; Li, S.; Bai, Y. Treatment of a Class II Division 1 malocclusion with the combination of a myofunctional trainer and fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Song, G.; Chen, H.; Xu, T. Nonsurgical treatment of Brodie bite assisted by 3-dimensional planning and assessment. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Sawilowsky, S.S. New effect size rules of thumb. J. Mod. Appl. Stat. Methods 2009, 8, 26. [Google Scholar] [CrossRef]
- Kau, C.H.; English, J.D.; Muller-Delgardo, M.G.; Hamid, H.; Ellis, R.K.; Winklemann, S. Retrospective cone-beam computed tomography evaluation of temporary anchorage devices. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 166.e1–166.e5. [Google Scholar] [CrossRef]
- Oktay, H. The study of the maxillary sinus areas in different orthodontic malocclusions. Am. J. Orthod. Dentofac. Orthop. 1992, 102, 143–145. [Google Scholar] [CrossRef] [PubMed]
- Jun, B.C.; Song, S.W.; Park, C.S.; Lee, D.H.; Cho, K.J.; Cho, J.H. The analysis of maxillary sinus aeration according to aging process; volume assessment by 3-dimensional reconstruction by high-resolutional CT scanning. Otolaryngol. Head Neck Surg. 2005, 132, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Velasco-Torres, M.; Padial-Molina, M.; Avila-Ortiz, G.; Garcia-Delgado, R.; O’Valle, F.; Catena, A.; Galindo-Moreno, P. Maxillary Sinus Dimensions Decrease as Age and Tooth Loss Increase. Implant Dent. 2017, 26, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, C.L. Forensic ethnic identification of crania: The role of the maxillary sinus--a new approach. Am. J. Forensic Med. Pathol. 2004, 25, 302–313. [Google Scholar] [CrossRef] [PubMed]
| Patient Count | Side Count | Age (Years) Median [Min, Max] | ANB Angle (Degrees) Median [Min, Max] | SN-MP Angle Median [Min, Max] | |
|---|---|---|---|---|---|
| Female L | 11 | 21 | 20.40 [18.7, 29.3] | 2.50 [1.1, 4.4] | 24.40 [20.8, 26.6] |
| Female N | 11 | 21 | 20.90 [16.1, 35.1] | 3.20 [0.7, 4.2] | 34.30 [31.1, 37.2] |
| Female H | 10 | 20 | 22.50 [18.0, 28.7] | 3.00 [0.8, 4.4] | 38.30 [37.9, 43.6] |
| Male L | 10 | 18 | 19.50 [15.0, 25.7] | 2.45 [0.8, 4.7] | 23.35 [19.3, 26.8] |
| Male N | 11 | 21 | 20.60 [15.2, 29.5] | 3.00 [0.7, 4.3] | 31.50 [28.6, 37.4] |
| Male H | 7 | 14 | 16.70 [15.5, 40.7] | 2.90 [1.0, 4.5] | 40.10 [38.2, 44.7] |
| Parameter | Group | Median [Min, Max] | p-Value of Mann–Whitney U Test | |||||
|---|---|---|---|---|---|---|---|---|
| Compare to Female L | Compare to Female N | Compare to Female H | Compare to Male L | Compare to Male N | Compare to Male H | |||
| Sinus Volume (mm3) | Female L | 15719 [6639, 25419] | - | 0.0257 * | 0.3318 | 0.0431 * | - | - |
| Female N | 13628 [6746, 20944] | 0.0257 * | - | 0.3449 | - | 0.0028 * | - | |
| Female H | 15249 [6936, 21425] | 0.3318 | 0.3449 | - | - | - | 0.0062 * | |
| Male L | 21211 [7731, 24129] | 0.0431 * | - | - | - | 0.3945 | 0.4643 | |
| Male N | 18543 [7796, 25393] | - | 0.0028 * | - | 0.3945 | - | 0.1976 | |
| Male H | 21535 [10817, 33139] | - | - | 0.0062 * | 0.4643 | 0.1976 | - | |
| Sinus Height (mm) | Female L | 36.40 [27.90, 40.60] | - | 0.1661 | 0.6468 | 0.0094 * | - | - |
| Female N | 34.80 [15.20, 40.20] | 0.1661 | - | 0.1790 | - | 0.0001 * | - | |
| Female H | 37.15 [29.30, 44.00] | 0.6468 | 0.1790 | - | - | - | 0.0005 * | |
| Male L | 40.25 [21.60, 45.80] | 0.0094 * | - | - | - | 0.7120 | 0.1535 | |
| Male N | 42.00 [27.70, 45.50] | - | 0.0001 * | - | 0.7120 | - | 0.1468 | |
| Male H | 43.90 [34.20, 52.50] | - | - | 0.0005 * | 0.1535 | 0.1468 | - | |
| Sinus Width (mm) | Female L | 27.80 [20.20, 37.30] | - | 0.0837 | 0.5567 | 0.3244 | - | - |
| Female N | 26.10 [12.70, 30.90] | 0.0837 | - | 0.3897 | - | 0.0205 * | - | |
| Female H | 27.25 [19.40, 30.40] | 0.5567 | 0.3897 | - | - | - | 0.0230 * | |
| Male L | 29.45 [20.60, 35.00] | 0.3244 | - | - | - | 0.8838 | 0.3423 | |
| Male N | 28.60 [19.40, 34.20] | - | 0.0205 * | - | 0.8838 | - | 0.2667 | |
| Male H | 31.30 [23.00, 37.40] | - | - | 0.0230 * | 0.3423 | 0.2667 | - | |
| Sinus Depth (mm) | Female L | 34.70 [30.60, 41.40] | - | 0.0630 | 0.3826 | 0.0502 | - | - |
| Female N | 34.00 [22.60, 38.50] | 0.063 | - | 0.4975 | - | 0.0066 * | - | |
| Female H | 34.75 [25.80, 40.20] | 0.3826 | 0.4975 | - | - | - | 0.0047 * | |
| Male L | 37.95 [29.40, 40.70] | 0.0502 | - | - | - | 0.2783 | 0.3718 | |
| Male N | 36.30 [31.40, 44.40] | - | 0.0066 * | - | 0.2783 | - | 0.1123 | |
| Male H | 37.75 [30.60, 46.30] | - | - | 0.0047 * | 0.3718 | 0.1123 | - | |
| Parameter | Female | Male | |||
|---|---|---|---|---|---|
| r | p-Value | r | p-Value | ||
| SN-MP angle | Sinus volume | −0.2088 | 0.1034 | 0.0131 | 0.9257 |
| Sinus height | 0.0023 | 0.9860 | 0.1586 | 0.2566 | |
| Sinus width | −0.2133 | 0.0961 | −0.0897 | 0.5230 | |
| Sinus depth | −0.1859 | 0.1479 | 0.0957 | 0.4955 | |
| Alveolar bone height between 4 & 5 | 0.1990 | 0.1210 | −0.0808 | 0.5654 | |
| Alveolar bone height between 5 & 6 | 0.2173 | 0.0898 | −0.1045 | 0.4563 | |
| Alveolar bone height between 6 & 7 | 0.1068 | 0.4087 | −0.1037 | 0.4599 | |
| ANB angle | Sinus volume | 0.0794 | 0.5397 | 0.1919 | 0.1687 |
| Sinus height | −0.0656 | 0.6127 | 0.0924 | 0.5103 | |
| Sinus width | −0.0901 | 0.4863 | 0.1003 | 0.4749 | |
| Sinus depth | 0.0734 | 0.5708 | 0.2590 | 0.0611 | |
| Alveolar bone height between 4 & 5 | −0.0416 | 0.7485 | −0.3224 | 0.0186 * | |
| Alveolar bone height between 5 & 6 | 0.0474 | 0.6131 | −0.2775 | 0.0442 * | |
| Alveolar bone height between 6 & 7 | 0.1850 | 0.1500 | −0.3224 | 0.0186 * | |
| Parameter | Group | Median [Min, Max] | p-Value of Mann–Whitney U Test | |||||
|---|---|---|---|---|---|---|---|---|
| Compare to Female L | Compare to Female N | Compare to Female H | Compare to Male L | Compare to Male N | Compare to Male H | |||
| between 4 & 5 (mm) | Female L | 12.40 [7.20, 15.90] | - | 0.7889 | 0.2303 | 0.0676 | - | - |
| Female N | 12.50 [9.00, 26.80] | 0.7889 | - | 0.3896 | - | 0.1474 | - | |
| Female H | 14.15 [8.00, 19.30] | 0.2303 | 0.3896 | - | - | - | 0.3274 | |
| Male L | 13.60 [10.10, 21.60] | 0.0676 | - | - | - | 0.8618 | 0.2026 | |
| Male N | 14.00 [7.00, 27.00] | - | 0.1474 | - | 0.8618 | - | 0.1162 | |
| Male H | 12.30 [5.80, 22.30] | - | - | 0.3274 | 0.2026 | 0.1162 | - | |
| between 5 & 6 (mm) | Female L | 9.50 [4.50, 14.00] | - | 0.9059 | 0.2253 | 0.2540 | - | - |
| Female N | 9.00 [7.10, 24.00] | 0.9059 | - | 0.3414 | - | 0.4888 | - | |
| Female H | 10.55 [3.70, 16.90] | 0.2253 | 0.3414 | - | - | - | 0.1061 | |
| Male L | 9.75 [5.40, 19.40] | 0.2540 | - | - | - | 0.8291 | 0.0928 | |
| Male N | 10.60 [5.10, 17.20] | - | 0.4888 | - | 0.8291 | - | 0.1285 | |
| Male H | 8.55 [4.50, 17.20] | - | - | 0.1061 | 0.0928 | 0.1285 | - | |
| between 6 & 7 (mm) | Female L | 8.90 [5.00, 10.60] | - | 0.8763 | 0.3752 | 0.7015 | - | - |
| Female N | 8.60 [5.20, 24.40] | 0.8763 | - | 0.6283 | - | 0.4067 | - | |
| Female H | 9.25 [4.10, 12.80] | 0.3752 | 0.6283 | - | - | - | 0.2939 | |
| Male L | 8.90 [6.90, 15.50] | 0.7015 | - | - | - | 0.7329 | 0.3051 | |
| Male N | 9.60 [4.60, 16.50] | - | 0.4067 | - | 0.7329 | - | 0.2064 | |
| Male H | 8.40 [3.60, 12.60] | - | - | 0.2939 | 0.3051 | 0.2064 | - | |
| Parameter | Group | Median [Min, Max] | p-Value of Mann–Whitney U Test | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Compare to Female L | Compare to Female N | Compare to Female H | Compare to Male L | Compare to Male N | Compare to Male H | ||||
| Buccal | between 4 & 5 (mm) | Female L | 9.70 [7.60, 11.80] | - | 0.4499 | 0.7714 | 0.0007 * | - | - |
| Female N | 9.70 [8.30, 12.40] | 0.4499 | - | 0.2100 | - | 0.0848 | - | ||
| Female H | 9.30 [7.50, 11.10] | 0.7714 | 0.2100 | - | - | - | 0.0094 * | ||
| Male L | 10.85 [8.60, 12.40] | 0.0007 * | - | - | - | 0.3978 | 0.3416 | ||
| Male N | 10.70 [8.60, 12.60] | - | 0.0848 | - | 0.3978 | - | 0.9536 | ||
| Male H | 10.60 [9.20, 12.10] | - | - | 0.0094 * | 0.3416 | 0.9536 | - | ||
| between 5 & 6 (mm) | Female L | 11.60 [3.00, 14.60] | - | 0.3023 | 0.6840 | 0.0051 * | - | - | |
| Female N | 11.70 [9.30, 14.50] | 0.3023 | - | 0.4890 | - | 0.0707 | - | ||
| Female H | 11.70 [2.30, 12.80] | 0.684 | 0.4890 | - | - | - | 0.0179 * | ||
| Male L | 12.30 [10.90, 14.50] | 0.0051 * | - | - | - | 0.8399 | 0.9477 | ||
| Male N | 12.60 [1.50, 15.80] | - | 0.0707 | - | 0.8399 | - | 0.9801 | ||
| Male H | 12.50 [11.20, 15.20] | - | - | 0.0179 * | 0.9477 | 0.9801 | - | ||
| between 6 & 7 (mm) | Female L | 14.90 [12.60, 16.50] | - | 0.0788 | 0.2096 | 0.0082 * | - | - | |
| Female N | 14.30 [12.10, 16.60] | 0.0788 | - | 0.6556 | - | 0.0005 * | - | ||
| Female H | 14.15 [13.50, 15.90] | 0.2096 | 0.6556 | - | - | - | 0.6222 | ||
| Male L | 15.95 [13.30, 17.80] | 0.0082 * | - | - | - | 0.9389 | 0.2961 | ||
| Male N | 15.70 [1.70, 18.20] | - | 0.0005 * | - | 0.9389 | - | 0.3724 | ||
| Male H | 14.75 [1.30, 17.90] | - | - | 0.6222 | 0.2961 | 0.3724 | - | ||
| Palatal | between 4 & 5 (mm) | Female L | 9.70 [7.60, 11.80] | - | 0.4499 | 0.7714 | 0.0007 * | - | - |
| Female N | 9.70 [8.30, 12.40] | 0.4499 | - | 0.2100 | - | 0.0848 | - | ||
| Female H | 9.30 [7.50, 11.10] | 0.7714 | 0.2100 | - | - | - | 0.0094 * | ||
| Male L | 10.85 [8.60, 12.40] | 0.0007 * | - | - | - | 0.3978 | 0.3416 | ||
| Male N | 10.70 [8.60, 12.60] | - | 0.0848 | - | 0.3978 | - | 0.9536 | ||
| Male H | 10.60 [9.20, 12.10] | - | - | 0.0094 * | 0.3416 | 0.9536 | - | ||
| between 5 & 6 (mm) | Female L | 11.60 [3.70, 14.60] | - | 0.3023 | 0.6840 | 0.0051 * | - | - | |
| Female N | 11.70 [9.30, 14.50] | 0.3023 | - | 0.4890 | - | 0.0707 | - | ||
| Female H | 11.70 [2.40, 12.80] | 0.6840 | 0.4890 | - | - | - | 0.0179 * | ||
| Male L | 12.30 [10.90, 14.50] | 0.0051 * | - | - | - | 0.8399 | 0.9477 | ||
| Male N | 12.60 [2.20, 15.80] | - | 0.0707 | - | 0.8399 | - | 0.9801 | ||
| Male H | 12.50 [11.20, 15.20] | - | - | 0.0179 * | 0.9477 | 0.9801 | - | ||
| between 6 & 7 (mm) | Female L | 14.90 [12.60, 16.50] | - | 0.0788 | 0.2096 | 0.0082 * | - | - | |
| Female N | 14.30 [12.10, 16.60] | 0.0788 | - | 0.6556 | - | 0.0005 * | - | ||
| Female H | 14.15 [13.50, 15.90] | 0.2096 | 0.6556 | - | - | - | 0.6222 | ||
| Male L | 15.95 [13.30, 17.80] | 0.0082 * | - | - | - | 0.9389 | 0.2961 | ||
| Male N | 15.70 [3.90, 18.20] | - | 0.0005 * | - | 0.9389 | - | 0.3724 | ||
| Male H | 14.75 [3.10, 17.90] | - | - | 0.6222 | 0.2961 | 0.3724 | - | ||
| Parameter | Group | Median [Min, Max] | p-Value of Mann–Whitney U test | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Compare to Female L | Compare to Female N | Compare to Female H | Compare to Male L | Compare to Male N | Compare to Male H | ||||
| Buccal | between 4 & 5 (mm) | Female L | 10.10 [7.60, 14.80] | - | 0.6948 | 0.0006 * | 0.0098 * | - | - |
| Female N | 10.00 [7.00, 13.00] | 0.6948 | - | 0.0014 * | - | 0.8763 | - | ||
| Female H | 8.55 [6.10, 11.00] | 0.0006 * | 0.0014 * | - | - | - | 0.0266 * | ||
| Male L | 11.50 [8.80, 13.10] | 0.0098 * | - | - | - | 0.0037 * | 0.0097 * | ||
| Male N | 10.50 [2.00, 14.20] | - | 0.8763 | - | 0.0037 * | - | 0.8877 | ||
| Male H | 9.90 [1.60, 12.70] | - | - | 0.0266 * | 0.0097 * | 0.8877 | - | ||
| between 5 & 6 (mm) | Female L | 11.50 [1.10, 14.90] | - | 0.8960 | 0.3030 | 0.3385 | - | - | |
| Female N | 12.20 [2.40, 16.20] | 0.8960 | - | 0.1663 | - | 0.7890 | - | ||
| Female H | 11.05 [0.80, 13.20] | 0.3030 | 0.1663 | - | - | - | 0.5982 | ||
| Male L | 12.75 [2.70, 14.60] | 0.3385 | - | - | - | 0.7433 | 0.4815 | ||
| Male N | 11.90 [1.20, 15.60] | - | 0.7890 | - | 0.7433 | - | 0.7209 | ||
| Male H | 11.45 [1.20, 15.90] | - | - | 0.5982 | 0.4815 | 0.7209 | - | ||
| between 6 & 7 (mm) | Female L | 14.70 [1.10, 16.60] | - | 0.5539 | 0.5831 | 0.0010 * | - | - | |
| Female N | 14.30 [1.00, 17.00] | 0.5539 | - | 0.8515 | - | 0.0984 | - | ||
| Female H | 14.60 [1.50, 16.10] | 0.5831 | 0.8515 | - | - | - | 0.3630 | ||
| Male L | 16.10 [5.40, 18.70] | 0.0010 * | - | - | - | 0.7016 | 0.4139 | ||
| Male N | 15.80 [1.10, 18.60] | - | 0.0984 | - | 0.7016 | - | 0.7332 | ||
| Male H | 14.80 [1.20, 18.30] | - | - | 0.3630 | 0.4139 | 0.7332 | - | ||
| Palatal | between 4 & 5 (mm) | Female L | 10.10 [7.60, 14.80] | - | 0.6948 | 0.0006 * | 0.0098 * | - | - |
| Female N | 10.00 [7.00, 13.00] | 0.6948 | - | 0.0014 * | - | 0.8763 | - | ||
| Female H | 8.55 [3.40, 11.00] | 0.0006 * | 0.0014 * | - | - | - | 0.0266 * | ||
| Male L | 11.50 [8.80, 13.10] | 0.0098 * | - | - | - | 0.0037 * | 0.0097 * | ||
| Male N | 10.50 [2.20, 14.20] | - | 0.8763 | - | 0.0037 * | - | 0.8877 | ||
| Male H | 9.90 [1.60, 12.70] | - | - | 0.0266 * | 0.0097 * | 0.8877 | - | ||
| between 5 & 6 (mm) | Female L | 11.50 [2.40, 14.90] | - | 0.9256 | 0.2009 | 0.4385 | - | - | |
| Female N | 12.20 [1.60, 16.20] | 0.9256 | - | 0.2056 | - | 0.6675 | - | ||
| Female H | 11.05 [1.10, 13.20] | 0.2009 | 0.2056 | - | - | - | 0.5982 | ||
| Male L | 12.75 [2.30, 14.60] | 0.4385 | - | - | - | 0.7752 | 0.4358 | ||
| Male N | 11.90 [2.20, 15.60] | - | 0.6675 | - | 0.7752 | - | 0.7085 | ||
| Male H | 11.45 [2.00, 15.90] | - | - | 0.5982 | 0.4358 | 0.7085 | - | ||
| between 6 & 7 (mm) | Female L | 14.70 [4.40, 16.60] | - | 0.4734 | 0.3755 | 0.0037 * | - | - | |
| Female N | 14.30 [2.20, 17.00] | 0.4734 | - | 0.9948 | - | 0.1405 | - | ||
| Female H | 14.60 [3.10, 16.10] | 0.3755 | 0.9948 | - | - | - | 0.4019 | ||
| Male L | 16.10 [3.30, 18.70] | 0.0037 * | - | - | - | 0.8074 | 0.4139 | ||
| Male N | 15.80 [1.80, 18.60] | - | 0.1405 | - | 0.8074 | - | 0.6355 | ||
| Male H | 14.80 [2.40, 18.30] | - | - | 0.4019 | 0.4139 | 0.6355 | - | ||
| Parameter | Group | Median [Min, Max] | p-Value of Mann–Whitney U Test | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Compare to Female L | Compare to Female N | Compare to Female H | Compare to Male L | Compare to Male N | Compare to Male H | ||||
| Buccal | between 4 & 5 (mm) | Female L | 11.10 [1.30, 13.60] | - | 0.8960 | 0.0553 | 0.0437 * | - | - |
| Female N | 10.70 [2.00, 15.10] | 0.8960 | - | 0.0036 * | - | 0.8665 | - | ||
| Female H | 8.65 [1.80, 11.10] | 0.0553 | 0.0036 * | - | - | - | 0.0180 * | ||
| Male L | 11.95 [4.80, 15.30] | 0.0437 * | - | - | - | 0.0272 * | 0.0295 * | ||
| Male N | 9.90 [1.80, 13.90] | - | 0.8665 | - | 0.0272 * | - | 0.9934 | ||
| Male H | 10.10 [1.20, 14.30] | - | - | 0.0180 * | 0.0295 * | 0.9934 | - | ||
| between 5 & 6 (mm) | Female L | 2.90 [1.30, 15,20] | - | 0.6764 | 0.8923 | 0.0157 * | - | - | |
| Female N | 2.90 [1.20, 16.00] | 0.6764 | - | 0.9846 | - | 0.3206 | - | ||
| Female H | 10.50 [0.50, 14.10] | 0.8923 | 0.9846 | - | - | - | 0.7363 | ||
| Male L | 13.05 [1.90, 16.30] | 0.0157 * | - | - | - | 0.2720 | 0.0663 | ||
| Male N | 10.60 [1.00, 16.30] | - | 0.3206 | - | 0.2720 | - | 0.3367 | ||
| Male H | 2.90 [0.60, 18.40] | - | - | 0.7363 | 0.0663 | 0.3367 | - | ||
| between 6 & 7 (mm) | Female L | 3.50 [1.00, 17.10] | - | 0.8960 | 0.4264 | 0.1072 | - | - | |
| Female N | 4.70 [1.00, 17.10] | 0.8960 | - | 0.2852 | - | 0.4504 | - | ||
| Female H | 14.40 [1.10, 16.70] | 0.4264 | 0.2852 | - | - | - | 0.5982 | ||
| Male L | 6.65 [3.20, 17.10] | 0.1072 | - | - | - | 0.2975 | 0.6460 | ||
| Male N | 4.70 [1.20, 18.50] | - | 0.4504 | - | 0.2975 | - | 0.7711 | ||
| Male H | 10.10 [0.90, 17.90] | - | - | 0.5982 | 0.6460 | 0.7711 | - | ||
| Palatal | between 4 & 5 (mm) | Female L | 11.10 [1.50, 13.60] | - | 0.9454 | 0.0504 | 0.0613 | - | - |
| Female N | 10.70 [1.50, 15.10] | 0.9454 | - | 0.0038 * | - | 0.8764 | - | ||
| Female H | 8.65 [1.90, 11.10] | 0.0504 | 0.0038 * | - | - | - | 0.0180 * | ||
| Male L | 11.95 [1.70, 15.30] | 0.0613 | - | - | - | 0.0341 * | 0.0295 * | ||
| Male N | 9.90 [2.40, 13.90] | - | 0.8764 | - | 0.0341 * | - | 0.9934 | ||
| Male H | 10.10 [0.90, 14.30] | - | - | 0.0180 * | 0.0295 * | 0.9934 | - | ||
| between 5 & 6 (mm) | Female L | 7.30 [1.30, 15.20] | - | 0.3927 | 0.9127 | 0.2908 | - | - | |
| Female N | 4.50 [1.20, 16.00] | 0.3927 | - | 0.4975 | - | 0.5128 | - | ||
| Female H | 10.50 [1.20, 14.10] | 0.9127 | 0.4975 | - | - | - | 0.3404 | ||
| Male L | 13.05 [1.80, 16.30] | 0.2908 | - | - | - | 0.3312 | 0.2310 | ||
| Male N | 10.60 [1.00, 16.30] | - | 0.5128 | - | 0.3312 | - | 0.5887 | ||
| Male H | 4.20 [0.90, 18.40] | - | - | 0.3404 | 0.2310 | 0.5887 | - | ||
| between 6 & 7 (mm) | Female L | 5.70 [1.40, 17.10] | - | 0.7227 | 0.6938 | 0.4986 | - | - | |
| Female N | 8.60 [1.80, 17.10] | 0.7227 | - | 0.5743 | - | 0.6949 | - | ||
| Female H | 14.40 [1.60, 16.70] | 0.6938 | 0.5743 | - | - | - | 0.5510 | ||
| Male L | 6.45 [2.80, 17.10] | 0.4986 | - | - | - | 0.5441 | 0.5672 | ||
| Male N | 5.50 [1.20, 18.50] | - | 0.6949 | - | 0.5441 | - | 0.7585 | ||
| Male H | 9.95 [1.30, 17.90] | - | - | 0.5510 | 0.5672 | 0.7585 | - | ||
| % of <5 mm | 5 mm Height | 8 mm Height | 10 mm Height | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4–5 | 5–6 | 6–7 | 4–5 | 5–6 | 6–7 | 4–5 | 5–6 | 6–7 | ||||||||||
| B | P | B | P | B | P | B | P | B | P | B | P | B | P | B | P | B | P | |
| Female L | 0.00 | 0.00 | 9.52 | 9.52 | 0.00 | 0.00 | 0.00 | 0.00 | 28.57 | 23.81 | 28.57 | 4.76 | 28.57 | 23.81 | 57.14 | 28.57 | 52.38 | 42.86 |
| Female N | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 23.81 | 23.81 | 23.81 | 19.05 | 14.29 | 9.52 | 66.67 | 57.14 | 52.38 | 42.86 |
| Female H | 0.00 | 0.00 | 5.00 | 5.00 | 0.00 | 0.00 | 0.00 | 5.00 | 20.00 | 15.00 | 20.00 | 15.00 | 15.00 | 15.00 | 40.00 | 35.00 | 40.00 | 35.00 |
| Male L | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 22.22 | 16.67 | 0.00 | 11.11 | 5.56 | 5.56 | 38.89 | 38.89 | 27.78 | 33.33 |
| Male N | 0.00 | 0.00 | 4.76 | 4.76 | 4.76 | 4.76 | 9.52 | 9.52 | 23.81 | 19.05 | 28.57 | 28.57 | 14.29 | 14.29 | 47.62 | 47.62 | 57.14 | 47.62 |
| Male H | 0.00 | 0.00 | 0.00 | 0.00 | 14.29 | 14.29 | 14.29 | 14.29 | 28.57 | 21.43 | 21.43 | 21.43 | 14.29 | 14.29 | 64.29 | 57.14 | 42.86 | 42.86 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.; Zou, M.; Syverson, A.; Zheng, Z.; Li, C. Maxillary Sinus Dimensions in Skeletal Class I Chinese Population with Different Vertical Skeletal Patterns: A Cone-Beam Computed Tomography Study. Diagnostics 2022, 12, 3144. https://doi.org/10.3390/diagnostics12123144
Wang J, Zou M, Syverson A, Zheng Z, Li C. Maxillary Sinus Dimensions in Skeletal Class I Chinese Population with Different Vertical Skeletal Patterns: A Cone-Beam Computed Tomography Study. Diagnostics. 2022; 12(12):3144. https://doi.org/10.3390/diagnostics12123144
Chicago/Turabian StyleWang, Jingyi, Min Zou, Abby Syverson, Zhong Zheng, and Chenshuang Li. 2022. "Maxillary Sinus Dimensions in Skeletal Class I Chinese Population with Different Vertical Skeletal Patterns: A Cone-Beam Computed Tomography Study" Diagnostics 12, no. 12: 3144. https://doi.org/10.3390/diagnostics12123144
APA StyleWang, J., Zou, M., Syverson, A., Zheng, Z., & Li, C. (2022). Maxillary Sinus Dimensions in Skeletal Class I Chinese Population with Different Vertical Skeletal Patterns: A Cone-Beam Computed Tomography Study. Diagnostics, 12(12), 3144. https://doi.org/10.3390/diagnostics12123144







