The Accuracy of Lateral Cephalogram for Measuring Alveolar Bone Thickness and Root Diameter on Mandibular Incisors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subject Selection
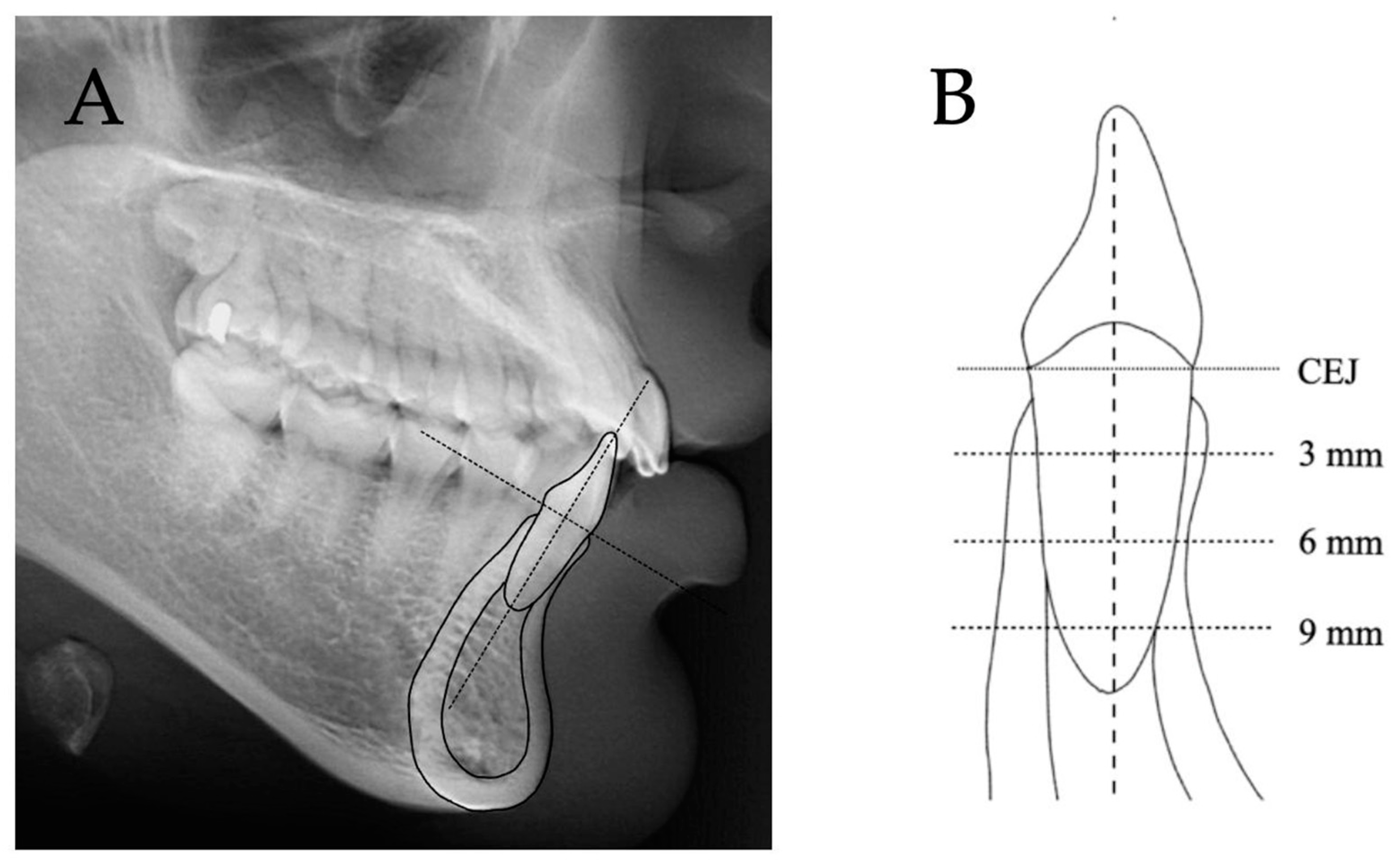
2.2. Lateral Cephalograms
2.3. Cone Beam Computed Tomography (CBCT)
2.4. Statistical Analyses
2.5. Sample Size Calculation
2.6. Quality Control
3. Results
3.1. Comparisons between Labial Ceph, L1CT, and L2CT
3.2. Comparisons between Lingual Ceph, L1CT, and L2CT
3.3. Comparisons of Root Diameters and Total Root-Bone Thicknesses between Ceph, L1CT, and L2CT
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Watson, W.G. Expansion and fenestration or dehiscence. Am. J. Orthod. 1980, 77, 330–332. [Google Scholar] [CrossRef] [PubMed]
- Artun, J.; Krogstad, O. Periodontal status of mandibular incisors following excessive proclination. A study in adults with surgically treated mandibular prognathism. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Handelman, C.S. The anterior alveolus: Its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996, 66, 95–109; discussion 109–110. [Google Scholar] [PubMed]
- Lee, S.; Hwang, S.; Jang, W.; Choi, Y.J.; Chung, C.J.; Kim, K.H. Assessment of lower incisor alveolar bone width using cone-beam computed tomography images in skeletal Class III adults of different vertical patterns. Korean J. Orthod. 2018, 48, 349–356. [Google Scholar] [CrossRef]
- Tian, Y.L.; Liu, F.; Sun, H.J.; Lv, P.; Cao, Y.M.; Yu, M.; Yue, Y. Alveolar bone thickness around maxillary central incisors of different inclination assessed with cone-beam computed tomography. Korean J. Orthod. 2015, 45, 245–252. [Google Scholar] [CrossRef] [Green Version]
- Grimard, B.A.; Hoidal, M.J.; Mills, M.P.; Mellonig, J.T.; Nummikoski, P.V.; Mealey, B.L. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J. Periodontol. 2009, 80, 48–55. [Google Scholar]
- Woelber, J.P.; Fleiner, J.; Rau, J.; Ratka-Krüger, P.; Hannig, C. Accuracy and Usefulness of CBCT in Periodontology: A Systematic Review of the Literature. Int. J. Periodontics Restor. Dent. 2018, 38, 289–297. [Google Scholar] [CrossRef] [Green Version]
- Durão, A.R.; Pittayapat, P.; Rockenbach, M.I.; Olszewski, R.; Ng, S.; Ferreira, A.P.; Jacobs, R. Validity of 2D lateral cephalometry in orthodontics: A systematic review. Prog. Orthod. 2013, 14, 31. [Google Scholar]
- Oz, U.; Orhan, K.; Abe, N. Comparison of linear and angular measurements using two-dimensional conventional methods and three-dimensional cone beam CT images reconstructed from a volumetric rendering program in vivo. Dentomaxillofac. Radiol. 2011, 40, 492–500. [Google Scholar]
- Liedke, G.S.; Delamare, E.L.; Vizzotto, M.B.; da Silveira, H.L.; Prietsch, J.R.; Dutra, V.; da Silveira, H.E. Comparative study between conventional and cone beam CT-synthesized half and total skull cephalograms. Dentomaxillofac. Radiol. 2012, 41, 136–142. [Google Scholar] [CrossRef] [Green Version]
- Park, C.S.; Park, J.K.; Kim, H.; Han, S.S.; Jeong, H.G.; Park, H. Comparison of conventional lateral cephalograms with corresponding CBCT radiographs. Imaging Sci. Dent. 2012, 42, 201–205. [Google Scholar] [CrossRef] [Green Version]
- Hariharan, A.; Diwakar, N.R.; Jayanthi, K.; Hema, H.M.; Deepukrishna, S.; Ghaste, S.R. The reliability of cephalometric measurements in oral and maxillofacial imaging: Cone beam computed tomography versus two-dimensional digital cephalograms. Indian J. Dent. Res. 2016, 27, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Teerakanok, S.; Charoemratrote, C.; Chanmanee, P. The Accuracy of Lateral Cephalogram in Representing the Anterior Maxillary Dentoalveolar Position. Diagnostics 2022, 12, 1840. [Google Scholar] [CrossRef] [PubMed]
- Foosiri, P.; Mahatumarat, K.; Panmekiate, S. Relationship between mandibular symphysis dimensions and mandibular anterior alveolar bone thickness as assessed with cone-beam computed tomography. Dent. Press J. Orthod. 2018, 23, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Yagci, A.; Veli, I.; Uysal, T.; Ucar, F.I.; Ozer, T.; Enhos, S. Dehiscence and fenestration in skeletal Class I, II, and III malocclusions assessed with cone-beam computed tomography. Angle Orthod. 2012, 82, 67–74. [Google Scholar] [CrossRef]
- Chanmanee, P.; Charoemratrote, C. Maxillary bone characteristics between thick and thin gingival biotypes with dentoalveolar protrusion. J. World Fed. Orthod. 2019, 8, 118–123. [Google Scholar] [CrossRef]
- Chanmanee, P.; Charoemratrote, C. Maxillary anterior gingiva and dentoalveolar changes after en-masse retraction between thick and thin gingival biotypes. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 838–848. [Google Scholar] [CrossRef]
- Ahn, J.-H.; Bae, K.-H.; Park, Y.-J.; Hong, R.-K.; Nam, J.-H.; Kim, M.-J. Assessment of antero-posterior skeletal relationships in adult Korean patients in the natural head position and centric relation. Korean J. Orthod. 2010, 40, 421–431. [Google Scholar] [CrossRef] [Green Version]
- Sarikaya, S.; Haydar, B.; Ciǧer, S.; Ariyürek, M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 15–26. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Dahlberg, G. Statistical methods for medical and biological students; George Allen and Unwin: London, UK, 1940; pp. 122–132. [Google Scholar]
- Nahm, K.Y.; Kang, J.H.; Moon, S.C.; Choi, Y.S.; Kook, Y.A.; Kim, S.H.; Huang, J. Alveolar bone loss around incisors in Class I bidentoalveolar protrusion patients: A retrospective three-dimensional cone beam CT study. Dentomaxillofac. Radiol. 2012, 41, 481–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oh, S.H.; Nahm, K.-Y.; Kim, S.-H.; Nelson, G. Alveolar bone thickness and fenestration of incisors in untreated Korean patients with skeletal class III malocclusion: A retrospective 3-dimensional cone-beam computed tomography study. Imaging Sci. Dent. 2020, 50, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Ahlqvist, J.; Eliasson, S.; Welander, U. The effect of projection errors on angular measurements in cephalometry. Eur. J. Orthod. 1988, 10, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Rino Neto, J.; de Paiva, J.B.; Queiroz, G.V.; Attizzani, M.F.; Miasiro Junior, H. Evaluation of radiographic magnification in lateral cephalograms obtained with different X-ray devices: Experimental study in human dry skull. Dent. Press J. Orthod. 2013, 18, e11–e17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baumrind, S.; Frantz, R.C. The reliability of head film measurements. 1. Landmark identification. Am. J. Orthod. 1971, 60, 111–127. [Google Scholar] [CrossRef]
- Bjork, A.; Solow, B. Measurement on radiographs. J. Dent. Res. 1962, 41, 672–683. [Google Scholar] [CrossRef]
- Becker, W.; Ochsenbein, C.; Tibbetts, L.; Becker, B.E. Alveolar bone anatomic profiles as measured from dry skulls. Clinical ramifications. J. Clin. Periodontol. 1997, 24, 727–731. [Google Scholar] [CrossRef]
- Lang, N.P.; Bartold, P.M. Periodontal health. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S9–S16. [Google Scholar] [CrossRef] [Green Version]
- Schei, O.; Waerhaug, J.; Lovdal, A.; Arno, A. Alveolar bone loss as related to oral hygiene and age. J. Periodontol. 1959, 30, 7–16. [Google Scholar] [CrossRef]
- Wikner, S.; Söder, P.O.; Frithiof, L.; Wouters, F. The approximal bone height and intrabony defects in young adults, related to the salivary buffering capacity and counts of Streptococcus mutans and Lactobacilli. Arch. Oral Biol. 1990, 35, 213s–215s. [Google Scholar] [CrossRef]
- Elnagar, M.H.; Handelman, C.S.; Lippincott, J.S.; Kim, M.R.; BeGole, E. Alveolar cortical plate changes associated with incisor retraction and its influence on the limits of orthodontic tooth movement. Orthod. Craniofac. Res. 2021, 24, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Aldawla, M.A.; Mufadhal, A.A.; Madfa, A.A. External and Internal Anatomy of Mandibular Permanent Incisors. In Human Teeth-Key Skills and Clinical Illustrations; Akarslan, Z., Bourzgui, F., Eds.; IntechOpen: London, UK, 2019; pp. 41–49. [Google Scholar]
- Stanley J., N. Wheeler’s Dental Anatomy, Physiology and Occlusion-E-Book, 10th ed.; Elsevier Health Sciences: St. Louis, MI, USA, 2014; p. 118. [Google Scholar]
- Ahlbrecht, C.A.; Ruellas, A.C.O.; Paniagua, B.; Schilling, J.A.; McNamara, J.A., Jr.; Cevidanes, L.H.S. Three-dimensional characterization of root morphology for maxillary incisors. PLoS ONE 2017, 12, e0178728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spolyar, J.L. Head Positioning Error in Cephalometric Radiography: —An Implant Study. Angle Orthod. 1987, 57, 77–88. [Google Scholar] [PubMed]
- Kamburoğlu, K.; Murat, S.; Kolsuz, E.; Kurt, H.; Yüksel, S.; Paksoy, C. Comparative assessment of subjective image quality of cross-sectional cone-beam computed tomography scans. J. Oral Sci. 2011, 53, 501–508. [Google Scholar] [CrossRef] [Green Version]
- Spin-Neto, R.; Gotfredsen, E.; Wenzel, A. Impact of voxel size variation on CBCT-based diagnostic outcome in dentistry: A systematic review. J. Digit. Imaging 2013, 26, 813–820. [Google Scholar] [CrossRef] [Green Version]
- Dong, T.; Yuan, L.; Liu, L.; Qian, Y.; Xia, L.; Ye, N.; Fang, B. Detection of alveolar bone defects with three different voxel sizes of cone-beam computed tomography: An in vitro study. Sci. Rep. 2019, 9, 8146. [Google Scholar] [CrossRef] [Green Version]
- Wenzel, A.; Haiter-Neto, F.; Frydenberg, M.; Kirkevang, L.L. Variable-resolution cone-beam computerized tomography with enhancement filtration compared with intraoral photostimulable phosphor radiography in detection of transverse root fractures in an in vitro model. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, 939–945. [Google Scholar] [CrossRef]
- Icen, M.; Orhan, K.; Şeker, Ç.; Geduk, G.; Cakmak Özlü, F.; Cengiz, M. Comparison of CBCT with different voxel sizes and intraoral scanner for detection of periodontal defects: An in vitro study. Dentomaxillofac. Radiol. 2020, 49, 20190197. [Google Scholar] [CrossRef]




| Labial Side | |||||||
|---|---|---|---|---|---|---|---|
| Mandibular Teeth (n = 38) | Ceph (C) | L1CT (L1) | L2CT (L2) | ANOVA p-Value | Differences | ||
| C-L1 | C-L2 | L1-L2 | |||||
| (1) Alveolar bone thicknesses | |||||||
| 3 mm apical to CEJ | 0.64 ± 0.08 | 0.48 ± 0.15 | 0.41 ± 0.11 | <0.001 | 0.16 ** ± 0.03 | 0.23 ** ± 0.03 | 0.07 ± 0.03 |
| 6 mm apical to CEJ | 0.59 ± 0.18 | 0.41 ± 0.13 | 0.30 ± 0.17 | <0.001 | 0.18 ** ± 0.04 | 0.29 ** ± 0.04 | 0.10 ± 0.04 |
| 9 mm apical to CEJ | 1.56 ± 0.13 | 1.37 ± 0.34 | 1.25 ± 0.28 | <0.001 | 0.19 * ± 0.05 | 0.31 ** ± 0.05 | 0.12 ± 0.05 |
| (2) Alveolar bone height | 1.03 ± 0.38 | 1.49 ± 0.37 | 1.51 ± 0.39 | <0.001 | −0.46 ** ± 0.09 | −0.48 ** ± 0.09 | −0.02 ± 0.09 |
| (3) Cortical bone thicknesses | |||||||
| 3 mm apical to CEJ | 0.64 ± 0.08 | 0.48 ± 0.15 | 0.41 ± 0.11 | <0.001 | 0.16 ** ± 0.03 | 0.23 ** ± 0.03 | 0.07 ± 0.03 |
| 6 mm apical to CEJ | 0.59 ± 0.18 | 0.41 ± 0.13 | 0.30 ± 0.17 | <0.001 | 0.18 ** ± 0.04 | 0.29 ** ± 0.04 | 0.10 ± 0.04 |
| 9 mm apical to CEJ | 1.56 ± 0.13 | 1.37 ± 0.34 | 1.25 ± 0.28 | <0.001 | 0.19 * ± 0.05 | 0.31 ** ± 0.05 | 0.12 ± 0.05 |
| (4) Cancellous bone thicknesses | |||||||
| 3 mm apical to CEJ | - | - | - | N/A | - | - | - |
| 6 mm apical to CEJ | - | - | - | N/A | - | - | - |
| 9 mm apical to CEJ | - | - | - | N/A | - | - | - |
| Lingual Side | |||||||
|---|---|---|---|---|---|---|---|
| Mandibular Teeth (n = 38) | Ceph (C) | L1CT (L1) | L2CT (L2) | ANOVA p-Value | Differences | ||
| C-L1 | C-L2 | L1-L2 | |||||
| (1) Alveolar bone thicknesses | |||||||
| 3 mm apical to CEJ | 1.05 ± 0.06 | 0.79 ± 0.27 | 0.89 ± 0.04 | <0.001 | 0.26 ** ± 0.04 | 0.17 ** ± 0.04 | −0.10 ± 0.04 |
| 6 mm apical to CEJ | 1.94 ± 0.24 | 1.69 ± 0.16 | 1.80 ± 0.10 | <0.001 | 0.25 ** ± 0.04 | 0.14 ** ± 0.04 | −0.11 ± 0.04 |
| 9 mm apical to CEJ | 2.83 ± 0.05 | 2.54 ± 0.25 | 2.64 ± 0.08 | <0.001 | 0.29 ** ± 0.04 | 0.19 * ± 0.04 | −0.10 ± 0.04 |
| (2) Alveolar bone height | 1.54 ± 0.40 | 1.92 ± 0.39 | 1.93 ± 0.38 | <0.001 | −0.38 ** ± 0.09 | −0.39 ** ± 0.09 | −0.01 ± 0.09 |
| (3) Cortical bone thicknesses | |||||||
| 3 mm apical to CEJ | 1.05 ± 0.06 | 0.79 ± 0.27 | 0.89 ± 0.04 | <0.001 | 0.26 ** ± 0.04 | 0.17 ** ± 0.04 | −0.10 ± 0.04 |
| 6 mm apical to CEJ | 1.94 ± 0.24 | 1.69 ± 0.16 | 1.80 ± 0.10 | <0.001 | 0.25 ** ± 0.04 | 0.14 ** ± 0.04 | −0.11 ± 0.04 |
| 9 mm apical to CEJ | 2.14 ± 0.21 | 1.91 ± 0.35 | 1.95 ± 0.27 | <0.01 | 0.23 * ± 0.06 | 0.19 * ± 0.06 | −0.04 ± 0.06 |
| (4) Cancellous bone thicknesses | |||||||
| 3 mm apical to CEJ | - | - | - | N/A | - | - | - |
| 6 mm apical to CEJ | - | - | - | N/A | - | - | - |
| 9 mm apical to CEJ | 0.69 ± 0.13 | 0.63 ± 0.16 | 0.68 ± 0.20 | 0.257 | 0.06 ± 0.04 | 0.01 ± 0.04 | −0.05 ± 0.04 |
| Mandibular Teeth (n = 34) | Ceph (C) | L1CT (L1) | L2CT (L2) | ANOVA p-Value | Differences | ||
|---|---|---|---|---|---|---|---|
| C-L1 | C-L2 | L1-L2 | |||||
| (1) Root diameters | |||||||
| 3 mm apical to CEJ | 5.52 ± 0.15 | 5.75 ± 0.10 | 6.00 ± 0.19 | <0.001 | −0.23 **± 0.03 | −0.48 ** ± 0.03 | −0.24 ** ± 0.03 |
| 6 mm apical to CEJ | 4.86 ± 0.09 | 5.08 ± 0.05 | 5.45 ± 0.09 | <0.001 | −0.22 ** ± 0.02 | −0.59 ** ± 0.02 | −0.37 ** ± 0.02 |
| 9 mm apical to CEJ | 3.81 ± 0.13 | 3.99 ± 0.15 | 4.20 ± 0.17 | <0.001 | −0.18 ** ± 0.03 | −0.39 ** ± 0.03 | −0.21 ** ± 0.03 |
| (2) Total root−bone thicknesses | |||||||
| 3 mm apical to CEJ | 7.21 ± 0.12 | 7.02 ± 0.18 | 7.30 ± 0.15 | <0.001 | 0.19 ** ± 0.04 | −0.09 ± 0.04 | −0.28 ** ± 0.04 |
| 6 mm apical to CEJ | 7.39 ± 0.04 | 7.18 ± 0.37 | 7.55 ± 0.19 | <0.001 | 0.22 ** ± 0.06 | −0.16 ± 0.06 | −0.37 ** ± 0.06 |
| 9 mm apical to CEJ | 8.20 ± 0.12 | 7.90 ± 0.40 | 8.09 ± 0.22 | <0.001 | 0.30 ** ± 0.06 | 0.11 ± 0.06 | −0.19 * ± 0.06 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Limsakul, T.; Chanmanee, P.; Charoemratrote, C. The Accuracy of Lateral Cephalogram for Measuring Alveolar Bone Thickness and Root Diameter on Mandibular Incisors. Diagnostics 2022, 12, 3159. https://doi.org/10.3390/diagnostics12123159
Limsakul T, Chanmanee P, Charoemratrote C. The Accuracy of Lateral Cephalogram for Measuring Alveolar Bone Thickness and Root Diameter on Mandibular Incisors. Diagnostics. 2022; 12(12):3159. https://doi.org/10.3390/diagnostics12123159
Chicago/Turabian StyleLimsakul, Thippawan, Pannapat Chanmanee, and Chairat Charoemratrote. 2022. "The Accuracy of Lateral Cephalogram for Measuring Alveolar Bone Thickness and Root Diameter on Mandibular Incisors" Diagnostics 12, no. 12: 3159. https://doi.org/10.3390/diagnostics12123159
APA StyleLimsakul, T., Chanmanee, P., & Charoemratrote, C. (2022). The Accuracy of Lateral Cephalogram for Measuring Alveolar Bone Thickness and Root Diameter on Mandibular Incisors. Diagnostics, 12(12), 3159. https://doi.org/10.3390/diagnostics12123159







