Image Fusion Involving Real-Time Transabdominal or Endoscopic Ultrasound for Gastrointestinal Malignancies: Review of Current and Future Applications
Abstract
1. Introduction
2. Methods
3. Image Modalities for Fusion and Benefits of Image Fusion
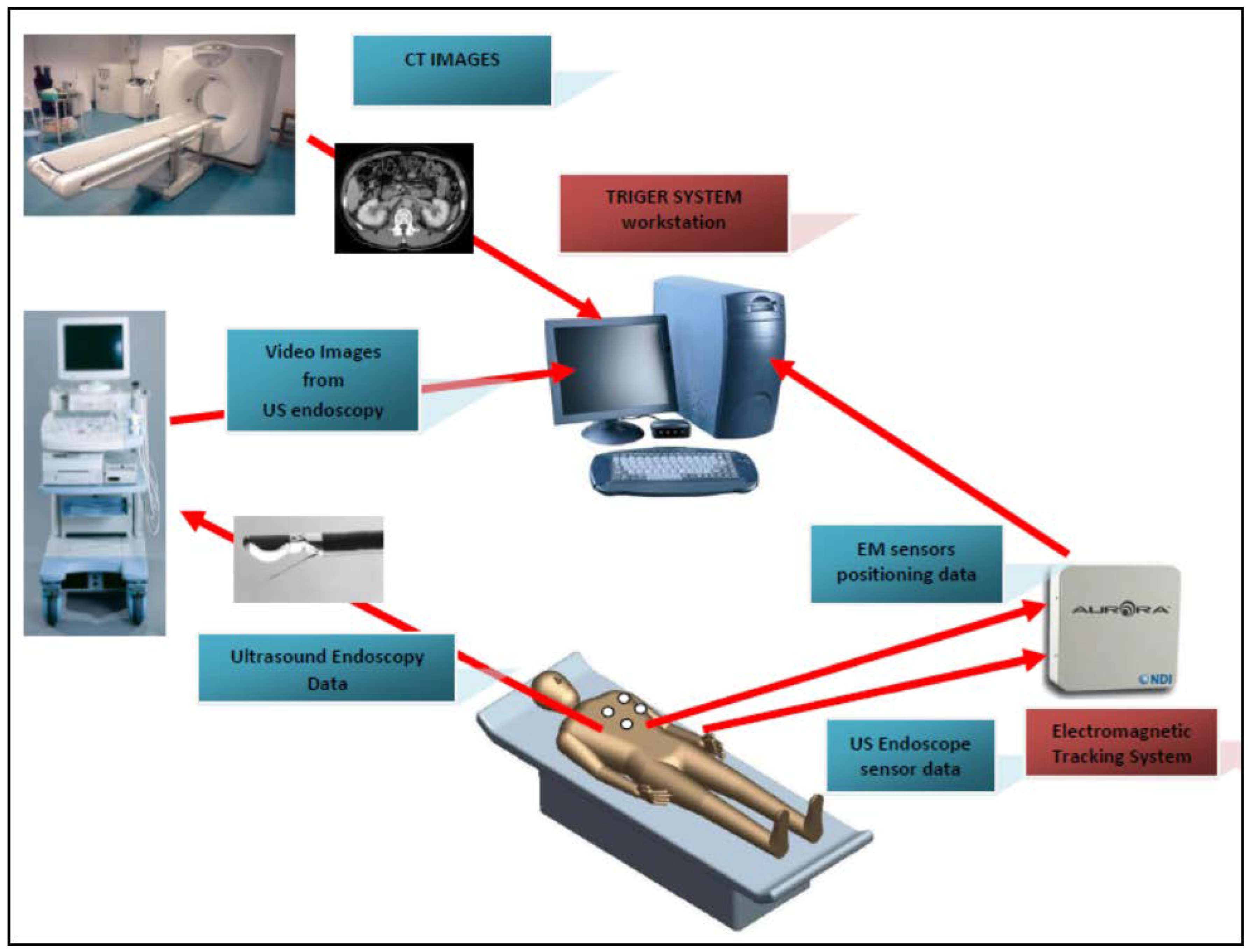
4. Technical Overview
- Place the EM tracking and field generator system in close proximity to or under the patient and connect it to the computer running the fusion imaging (FI) software;
- Place one or more active marker disks on the patient’s xiphoid process;
- Place the EM sensor inside the navigation catheter in the working channel of the endoscope/echoendoscope;
- Load the pre-procedure CT scans in the FI software;
- Create a 3D model of the patient anatomy;
- Co-register the EUS patient space with the CT space;
- Identify and navigate towards the target using dual visualization of the EUS image and its corresponding virtual section through the CT volume;
- Make fine adjustments to the registration if necessary;
- Once the target is reached, the EUS is fixed in place; the navigation catheter is retracted and replaced with a FNA (fine needle aspiration) needle for biopsy collection.
5. Current Clinical Applications of Image Fusion in GI Malignancies
| Reference | Year | Image Modalities for Fusion | No. of Patients | Clinical Application |
|---|---|---|---|---|
| Jung et al. [5] | 2009 | CE-US/CT/MRI | 20 | Assessment of the vascularization and perfusion of liver tumors |
| Rennert et al. [19] | 2011 | CE-US/CT/MRI | 100 | Localization and diagnosis of hepatic lesions in patients with primary hepatic cancer or liver metastases |
| Stang et al. [20] | 2012 | US/CT | 64 | Identification of hepatic metastases in patients with colorectal cancer |
| Song et al. [27,35] | 2013 | US/CT/MRI | 120 | Identification and ablation with RFA of hepatocellular carcinomas not visible on conventional US |
| Hakime et al. [26] | 2017 | US/CT | 35 | Targeting of liver metastases for percutaneous microwave ablation |
| Mauri et al. [28] | 2014 | US/CT/MRI | 295 | Targeting and thermal ablation of liver tumors undetectable with US alone |
| Minami et al. [25] | 2014 | US/CT/MRI | 147 | Guidance of RFA in hepatocellular carcinomas with poor conspicuity on B-mode US |
| Lee et al. [18] | 2013 | US/CT/MRI | 137 | Detection of small hepatocellular carcinomas for RFA |
| Minami et al. [30] | 2016 | US/US | 10 | Visualization of the ablative margin of RFA for liver metastases |
| Li et al. [31] | 2017 | CE-US/CT/MRI | 24 (phantom models) | Evaluation of radiofrequency ablative margin |
| Liu et al. [32] | 2012 | US/CT/MRI | 18 | Real-time guidance of microwave ablation for hepatocellular carcinoma undetectable by conventional US |
| Zhang et al. [33] | 2017 | US/CT | 19 | Real-time three-dimensional guidance of percutaneous microwave ablation for hepatocellular carcinoma |
| Ross et al. [34] | 2010 | CE-US/CT/MRI | 20 | Evaluation of the results after transcatheter arterial chemoembolization for hepatocellular carcinoma |
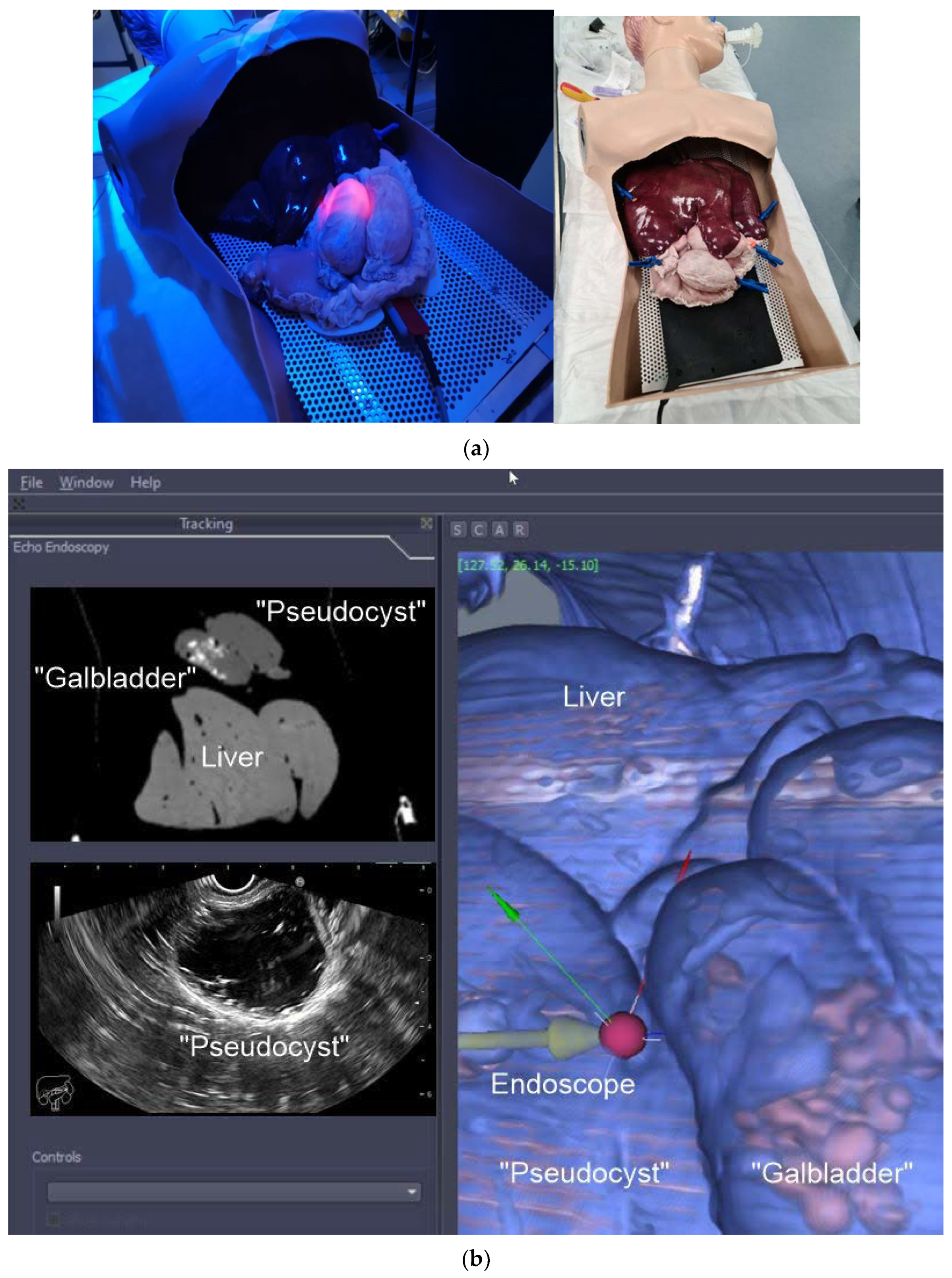
6. EUS Image Fusion—Is It Feasible?
7. Summary Points
- Real-time US fusion imaging (CT/MR) allows for a better detection and characterization of focal liver lesions;
- Image fusion can offer important advantages for targeting liver lesions during minimally invasive procedures such as biopsies and percutaneous ablations or for radiation treatment planning;
- EUS–CT image fusion allows for easier navigation and profiling of the target tumor and/or surrounding anatomical structure;
- EUS–CT image fusion can lower the learning curve for understanding and navigating EUS.
8. Conclusions
Author Contributions
Funding
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ewertsen, C.; Săftoiu, A.; Gruionu, L.G.; Karstrup, S.; Nielsen, M.B. Real-time image fusion involving diagnostic ultrasound. Am. J. Roentgenol. 2013, 200, W249–W255. [Google Scholar] [CrossRef] [PubMed]
- Gruionu, L.G.; Saftoiu, A.; Gruionu, G. A novel fusion imaging system for endoscopic ultrasound. Endosc. Ultrasound 2016, 5, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Rajagopal, M.; Venkatesan, A.M. Image fusion and navigation platforms for percutaneous image-guided interventions. Abdom. Radiol. 2016, 41, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Sandulescu, D.L.; Dumitrescu, D.; Rogoveanu, I.; Saftoiu, A.J. Hybrid ultrasound imaging techniques (fusion imaging). World J. Gastroenterol. 2011, 17, 49. [Google Scholar] [CrossRef]
- Jung, E.; Schreyer, A.; Schacherer, D.; Menzel, C.; Farkas, S.; Loss, M.; Feuerbach, S.; Zorger, N.; Fellner, C. New real-time image fusion technique for characterization of tumor vascularisation and tumor perfusion of liver tumors with contrast-enhanced ultrasound, spiral CT or MRI: First results. Clin. Hemorheol. Microcirc. 2009, 43, 57–69. [Google Scholar] [CrossRef]
- Chehab, M.A.; Brinjikji, W.; Copelan, A.; Venkatesan, A.M. Navigational tools for interventional radiology and interventional oncology applications. Semin. Interv. Radiol. 2015, 32, 416–427. [Google Scholar] [CrossRef]
- Ewertsen, C.; Henriksen, B.; Torp-Pedersen, S.; Nielsen, M.B. Characterization by biopsy or CEUS of liver lesions guided by image fusion between ultrasonography and CT, PET/CT or MRI. Ultraschall der Med. Eur. J. Ultrasound 2011, 32, 191–197. [Google Scholar] [CrossRef]
- Du, T.; Bill, K.A.; Ford, J.; Barawi, M.; Hayward, R.D.; Alame, A.; Berri, R.N. The diagnosis and staging of pancreatic cancer: A comparison of endoscopic ultrasound and computed tomography with pancreas protocol. Am. J. Surg. 2018, 215, 472–475. [Google Scholar] [CrossRef]
- Jemaa, Y.; Houissa, F.; Trabelsi, S.; Moussa, A.; Belhouchet, H.; Mouelhi, L.; Bouraoui, M.; Bouzaidi, S.; Debbeche, R.; Yedder, B.J.; et al. Endoscopic ultrasonography versus helical CT in diagnosis and staging of pancreatic cancer. La Tunis. Medicale 2008, 86, 346–349. [Google Scholar]
- Wahl, R.L.; Herman, J.M.; Ford, E. The promise and pitfalls of positron emission tomography and single-photon emission computed tomography molecular imaging–guided radiation therapy. Semin. Radiat. Oncol. 2011, 21, 88–100. [Google Scholar] [CrossRef][Green Version]
- Chirindel, A.; Alluri, K.C.; Chaudhry, M.A.; Wahl, R.L.; Pawlik, T.M.; Herman, J.M.; Subramaniam, R.M. Prognostic value of FDG PET/CT-derived parameters in pancreatic adenocarcinoma at initial PET/CT staging. Am. J. Roentgenol. 2015, 204, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Paparo, F.; Piccazzo, R.; Cevasco, L.; Piccardo, A.; Pinna, F.; Belli, F.; Bacigalupo, L.; Biscaldi, E.; De Caro, G.; Rollandi, G.A. Advantages of percutaneous abdominal biopsy under PET-CT/ultrasound fusion imaging guidance: A pictorial essay. Abdom. Imaging 2014, 39, 1102–1113. [Google Scholar] [CrossRef] [PubMed]
- Dholakia, A.S.; Chaudhry, M.; Leal, J.P.; Chang, D.T.; Raman, S.P.; Hacker-Prietz, A.; Su, Z.; Pai, J.; Oteiza, K.E.; Griffith, M.E.; et al. Baseline metabolic tumor volume and total lesion glycolysis are associated with survival outcomes in patients with locally advanced pancreatic cancer receiving stereotactic body radiation therapy. Int. J. Radiat. Oncol. 2014, 89, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Amer, A.M.; Zaid, M.; Chaudhury, B.; Elganainy, D.; Lee, Y.; Wilke, C.T.; Cloyd, J.; Wang, H.; Maitra, A.; Wolff, R.A.; et al. Imaging-based biomarkers: Changes in the tumor interface of pancreatic ductal adenocarcinoma on computed tomography scans indicate response to cytotoxic therapy. Cancer 2018, 1124, 1701–1709. [Google Scholar] [CrossRef]
- Cha, D.I.; Lee, M.W.; Song, K.D.; Oh, Y.-T.; Jeong, J.-Y.; Chang, J.-W.; Ryu, J.; Lee, K.J.; Kim, J.; Bang, W.-C.; et al. A prospective comparison between auto-registration and manual registration of real-time ultrasound with MR images for percutaneous ablation or biopsy of hepatic lesions. Abdom. Radiol. 2017, 42, 1799–1808. [Google Scholar] [CrossRef]
- Liu, H.H.; Koch, N.; Starkschall, G.; Jacobson, M.; Forster, K.; Liao, Z.; Komaki, R.; Stevens, C.W. Evaluation of internal lung motion for respiratory-gated radiotherapy using MRI: Part II—Margin reduction of internal target volume. Int. J. Radiat. Oncol. 2004, 60, 1473–1483. [Google Scholar] [CrossRef]
- Yang, M.; Ding, H.; Kang, J.; Zhu, L.; Wang, G. Subject-specific real-time respiratory liver motion compensation method for ultrasound-MRI/CT fusion imaging. Assist. Radiol. Surg. 2015, 10, 517–529. [Google Scholar] [CrossRef]
- Lee, M.W.; Rhim, H.; Cha, D.I.; Kim, Y.J.; Lim, H.K.J.J.o.V.; Radiology, I. Planning US for percutaneous radiofrequency ablation of small hepatocellular carcinomas (1–3 cm): Value of fusion imaging with conventional US and CT/MR images. J. Vasc. Interv. Radiol. 2013, 24, 958–965. [Google Scholar] [CrossRef]
- Rennert, J.; Georgieva, M.; Schreyer, A.; Jung, W.; Ross, C.; Stroszczynski, C.; Jung, E.M. Image fusion of contrast enhanced ultrasound (CEUS) with computed tomography (CT) or magnetic resonance imaging (MRI) using volume navigation for detection, characterization and planning of therapeutic interventions of liver tumors. Clin. Hemorheol. Microcirc. 2011, 49, 67–81. [Google Scholar] [CrossRef]
- Stang, A.; Keles, H.; Hentschke, S.; Seydewitz, C.; Keuchel, M.; Pohland, C.; Dahlke, J.; Weilert, H.; Wessling, J.; Malzfeldt, E.J. Real-time ultrasonography-computed tomography fusion imaging for staging of hepatic metastatic involvement in patients with colorectal cancer: Initial results from comparison to US seeing separate CT images and to multidetector-row CT alone. Invest. Radiol. 2010, 45, 491–501. [Google Scholar] [CrossRef]
- Lee, D.H.; Lee, J.M. Recent advances in the image-guided tumor ablation of liver malignancies: Radiofrequency ablation with multiple electrodes, real-time multimodality fusion imaging, and new energy sources. Korean J. Radiol. 2018, 19, 545–559. [Google Scholar] [CrossRef] [PubMed]
- N′Kontchou, G.; Mahamoudi, A.; Aout, M.; Ganne-Carrié, N.; Grando, V.; Coderc, E.; Vicaut, E.; Trinchet, J.C.; Sellier, N.; Beaugrand, M.; et al. Radiofrequency ablation of hepatocellular carcinoma: Long-term results and prognostic factors in 235 Western patients with cirrhosis. Hepatology 2009, 50, 1475–1483. [Google Scholar] [CrossRef]
- Solbiati, L.; Livraghi, T.; Goldberg, S.N.; Ierace, T.; Meloni, F.; Dellanoce, M.; Cova, L.; Halpern, E.F.; Gazelle, G.S. Percutaneous radio-frequency ablation of hepatic metastases from colorectal cancer: Long-term results in 117 patients. Radiology 2001, 221, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-S.; Lim, H.K.; Rhim, H.; Lee, M.W.; Choi, D.; Lee, W.J.; Paik, S.W.; Koh, K.C.; Lee, J.H.; Choi, M.S.; et al. Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: Analysis of prognostic factors. J. Hepatol. 2013, 58, 89–97. [Google Scholar] [CrossRef]
- Minami, Y.; Kudo, M.J.G. Radiofrequency ablation of liver metastases from colorectal cancer: A literature review. Gut Liver 2013, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Hakime, A.; Yevich, S.; Tselikas, L.; Deschamps, F.; Petrover, D.; De Baere, T. Percutaneous Thermal Ablation with Ultrasound Guidance. Fusion Imaging Guidance to Improve Conspicuity of Liver Metastasis. Cardiovasc. Interv. Radiol. 2017, 40, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Song, K.D.; Lee, M.W.; Rhim, H.; Cha, D.I.; Chong, Y.; Lim, H.K. Fusion Imaging–Guided Radiofrequency Ablation for Hepatocellular Carcinomas Not Visible on Conventional Ultrasound. Am. J. Roentgenol. 2013, 201, 1141–1147. [Google Scholar] [CrossRef]
- Mauri, G.; Cova, L.; De Beni, S.; Ierace, T.; Tondolo, T.; Cerri, A.; Goldberg, S.N.; Solbiati, L. Real-Time US-CT/MRI Image Fusion for Guidance of Thermal Ablation of Liver Tumors Undetectable with US: Results in 295 Cases. Cardiovasc. Interv. Radiol. 2014, 38, 143–151. [Google Scholar] [CrossRef]
- Minami, T.; Minami, Y.; Chishina, H.; Arizumi, T.; Takita, M.; Kitai, S.; Yada, N.; Inoue, T.; Hagiwara, S.; Ueshima, K.; et al. Combination Guidance of Contrast-Enhanced US and Fusion Imaging in Radiofrequency Ablation for Hepatocellular Carcinoma with Poor Conspicuity on Contrast-Enhanced US/Fusion Imaging. Oncology 2014, 87, 55–62. [Google Scholar] [CrossRef]
- Minami, Y.; Minami, T.; Chishina, H.; Kono, M.; Arizumi, T.; Takita, M.; Yada, N.; Hagiwara, S.; Ida, H.; Ueshima, K.; et al. US-US Fusion Imaging in Radiofrequency Ablation for Liver Metastases. Dig. Dis. 2016, 34, 687–691. [Google Scholar] [CrossRef]
- Li, K.; Su, Z.; Xu, E.; Huang, Q.; Zeng, Q.; Zheng, R. Evaluation of the ablation margin of hepatocellular carcinoma using CEUS-CT/MR image fusion in a phantom model and in patients. BMC Cancer 2017, 17, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.-Y.; Yu, X.-L.; Liang, P.; Cheng, Z.-G.; Han, Z.-Y.; Dong, B.-W.; Zhang, X.-H. Microwave ablation assisted by a real-time virtual navigation system for hepatocellular carcinoma undetectable by conventional ultrasonography. Eur. J. Radiol. 2012, 81, 1455–1459. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Liang, W.; Zhang, M.; Liang, P.; Gu, Y.; Kuang, M.; Cao, F.; Yu, X.; Liu, F.; Yu, J. Multiple antenna placement in microwave ablation assisted by a three-dimensional fusion image navigation system for hepatocellular carcinoma. Int. J. Hyperth. 2018, 35, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.; Rennert, J.; Schacherer, D.; Girlich, C.; Hoffstetter, P.; Heiss, P.; Jung, W.; Feuerbach, S.; Zorger, N.; Jung, E. Image fusion with volume navigation of contrast enhanced ultrasound (CEUS) with computed tomography (CT) or magnetic resonance imaging (MRI) for post-interventional follow-up after transcatheter arterial chemoembolization (TACE) of hepatocellular carcinomas (HCC): Preliminary results. Clin. Hemorheol. Microcirc. 2010, 46, 101–115. [Google Scholar]
- Choi, J.-H.; Seo, D.-W.; Song, T.J.; Park, D.H.; Lee, S.S.; Lee, S.K.; Kim, M.-H. Utility of Contrast-Enhanced Harmonic Endoscopic Ultrasound for the Guidance and Monitoring of Endoscopic Radiofrequency Ablation. Gut Liver 2020, 14, 826–832. [Google Scholar] [CrossRef]
- Wani, S.; Coté, G.A.; Keswani, R.; Mullady, D.; Azar, R.; Murad, F.; Edmundowicz, S.; Komanduri, S.; McHenry, L.; Al-Haddad, M.A.; et al. Learning curves for EUS by using cumulative sum analysis: Implications for American Society for Gastrointestinal Endoscopy recommendations for training. Gastrointest. Endosc. 2013, 77, 558–565. [Google Scholar] [CrossRef]
- Rösch, T. State of the art lecture: Endoscopic ultrasonography: Training and competence. Endoscopy 2006, 38, 69–72. [Google Scholar] [CrossRef]
- Vilmann, P.; Seicean, A.; Săftoiu, A. Tips to Overcome Technical Challenges in EUS-guided Tissue Acquisition. Gastrointest. Endosc. Clin. North Am. 2014, 24, 109–124. [Google Scholar] [CrossRef]
- Kawakubo, K.; Kawakami, H.; Kuwatani, M.; Haba, S.; Kawahata, S.; Abe, Y.; Kubota, Y.; Kubo, K.; Isayama, H.; Sakamoto, N. Recent advances in endoscopic ultrasonography-guided biliary interventions. World J. Gastroenterol. 2015, 21, 9494–9502. [Google Scholar] [CrossRef]
- Bhutani, M.S.; Cazacu, I.M.; Chavez, A.A.L.; Saftoiu, A.; Vilmann, P. A quarter century of EUS-FNA: Progress, milestones, and future directions. Endosc. Ultrasound 2018, 7, 141–160. [Google Scholar] [CrossRef]
- Eisen, G.M.; Dominitz, J.A.; Faigel, D.O.; Goldstein, J.A.; Petersen, B.T.; Raddawi, H.M.; Ryan, M.E.; Vargo, J.J., III.; Young, H.S.; Wheeler-Harbaugh, J.; et al. Guidelines for credentialing and granting privileges for endoscopic ultrasound. Gastrointest. Endosc. 2001, 54, 811–814. [Google Scholar] [CrossRef] [PubMed]
- Obstein, K.L.; Estépar, R.S.J.; Jayender, J.; Patil, V.D.; Spofford, I.S.; Ryan, M.B.; Lengyel, B.I.; Shams, R.; Vosburgh, K.G.; Thompson, C.C.J.E. Image Registered Gastroscopic Ultrasound (IRGUS) in human subjects: A pilot study to assess feasibility. Endoscopy 2011, 43, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Ding, H.; Zhu, L.; Wang, G. Ultrasound fusion image error correction using subject-specific liver motion model and automatic image registration. Comput. Biol. Med. 2016, 79, 99–109. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, B.S.; Cazacu, I.M.; Deza, C.A.; Rigaud, B.S.; Saftoiu, A.; Gruionu, G.; Guionu, L.; Brock, K.K.; Koay, E.J.; Herman, J.M.; et al. Image Fusion Involving Real-Time Transabdominal or Endoscopic Ultrasound for Gastrointestinal Malignancies: Review of Current and Future Applications. Diagnostics 2022, 12, 3218. https://doi.org/10.3390/diagnostics12123218
Singh BS, Cazacu IM, Deza CA, Rigaud BS, Saftoiu A, Gruionu G, Guionu L, Brock KK, Koay EJ, Herman JM, et al. Image Fusion Involving Real-Time Transabdominal or Endoscopic Ultrasound for Gastrointestinal Malignancies: Review of Current and Future Applications. Diagnostics. 2022; 12(12):3218. https://doi.org/10.3390/diagnostics12123218
Chicago/Turabian StyleSingh, Ben S., Irina M. Cazacu, Carlos A. Deza, Bastien S. Rigaud, Adrian Saftoiu, Gabriel Gruionu, Lucian Guionu, Kristy K. Brock, Eugene J. Koay, Joseph M. Herman, and et al. 2022. "Image Fusion Involving Real-Time Transabdominal or Endoscopic Ultrasound for Gastrointestinal Malignancies: Review of Current and Future Applications" Diagnostics 12, no. 12: 3218. https://doi.org/10.3390/diagnostics12123218
APA StyleSingh, B. S., Cazacu, I. M., Deza, C. A., Rigaud, B. S., Saftoiu, A., Gruionu, G., Guionu, L., Brock, K. K., Koay, E. J., Herman, J. M., & Bhutani, M. S. (2022). Image Fusion Involving Real-Time Transabdominal or Endoscopic Ultrasound for Gastrointestinal Malignancies: Review of Current and Future Applications. Diagnostics, 12(12), 3218. https://doi.org/10.3390/diagnostics12123218








