Effect of Body Mass Index in Coronary CT Angiography Performed on a 256-Slice Multi-Detector CT Scanner
Abstract
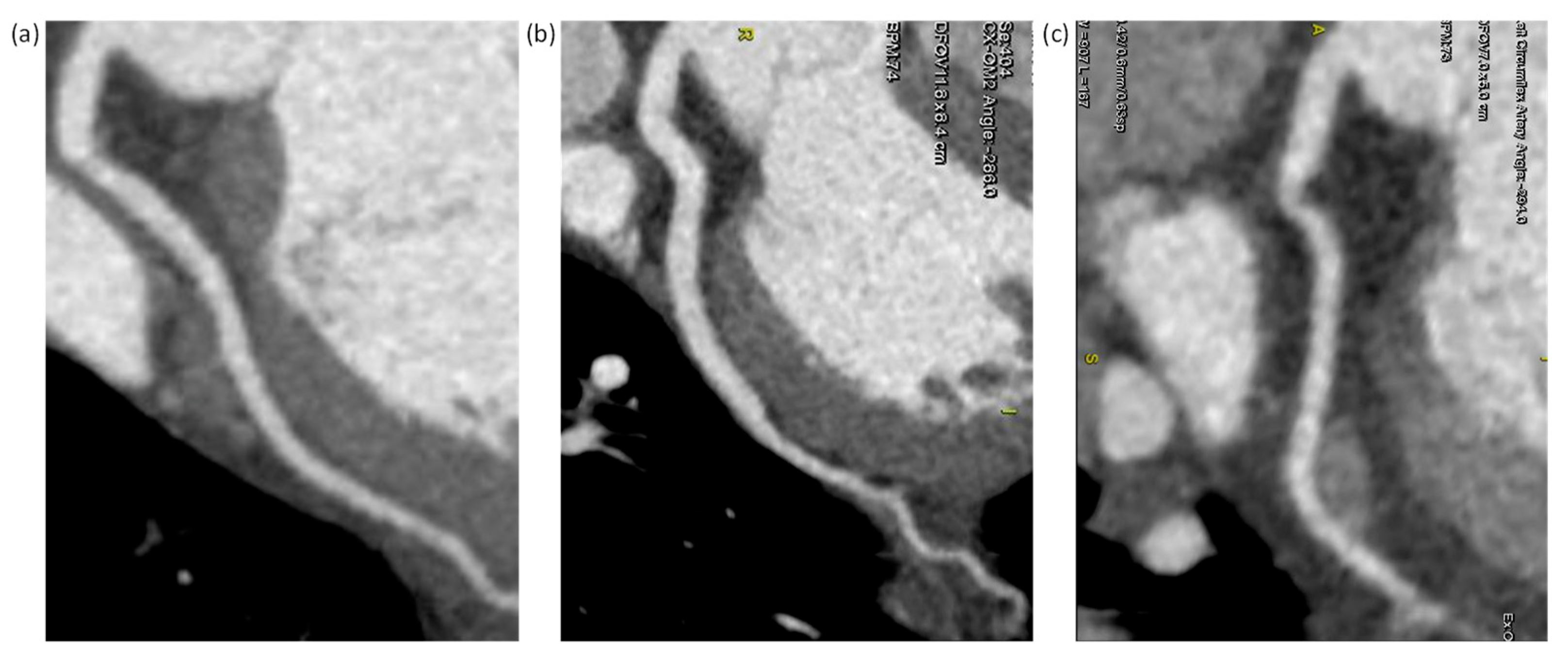
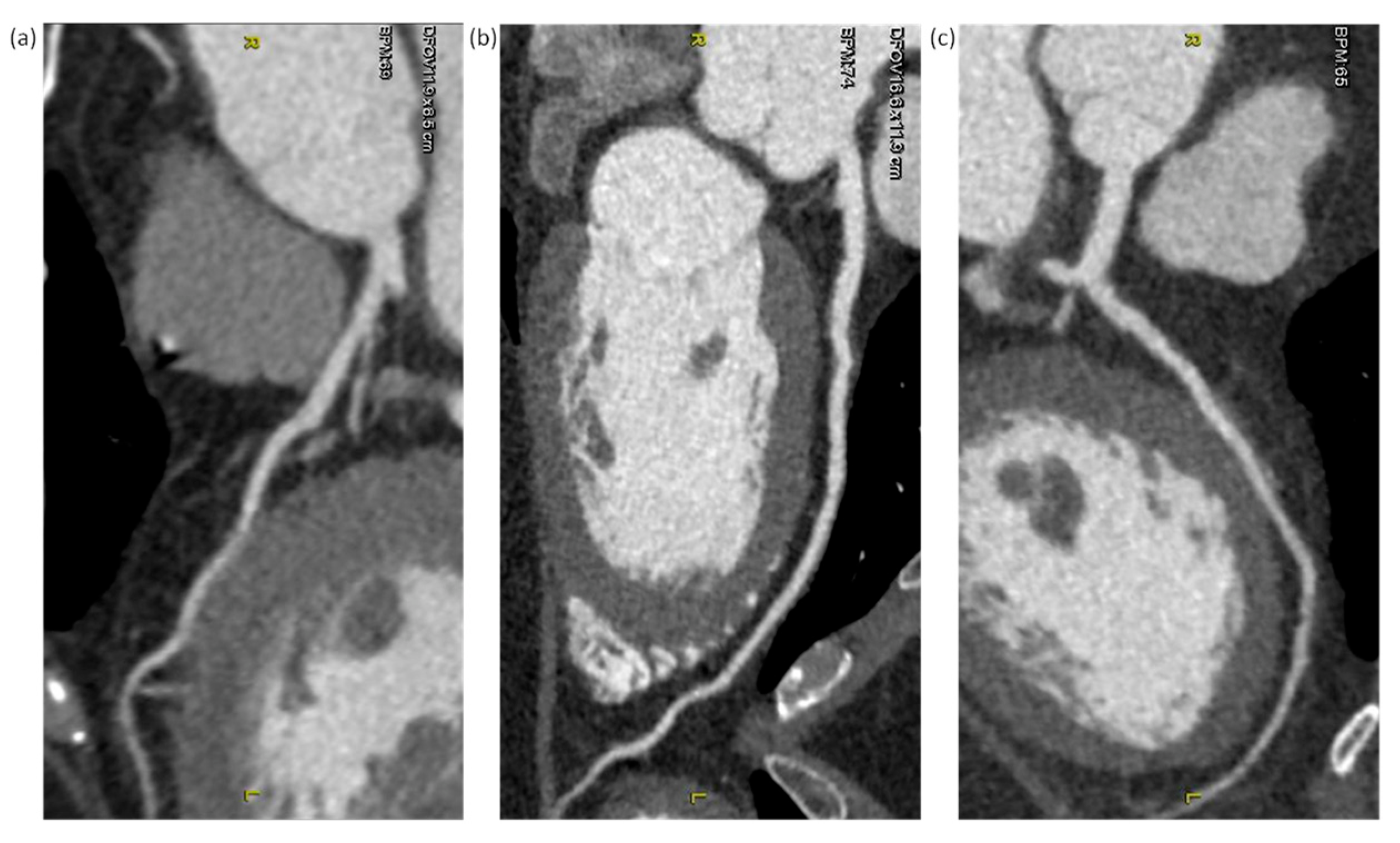
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. CCTA Acquisition
2.3. Image Quality Evaluation
2.4. Radiation Dose
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; Report of a WHO Consultation; Technical Report Series 894; World Health Organization: Geneva, Switzerland, 2000; 253p.
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; De Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics-2017 Update: A Report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; Cohen, A.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef] [Green Version]
- Roth, G.A.; Huffman, M.D.; Moran, A.E.; Feigin, V.; Mensah, G.A.; Naghavi, M.; Murray, C.J. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 2015, 132, 1667–1678. [Google Scholar] [CrossRef] [Green Version]
- MacDougall, R.D.; Kleinman, P.L.; Callahan, M.J. Size-based protocol optimization using automatic tube current modulation and automatic kV selection in computed tomography. J. Appl. Clin. Med. Phys. 2016, 17, 328–341. [Google Scholar] [CrossRef] [Green Version]
- Soderberg, M.; Gunnarsson, M. Automatic exposure control in computed tomography--an evaluation of systems from different manufacturers. Acta Radiol. 2010, 51, 625–634. [Google Scholar] [CrossRef]
- Schindera, S.T.; Nelson, R.C.; Yoshizumi, T.; Toncheva, G.; Nguyen, G.; DeLong, D.M.; Szucs-Farkas, Z. Effect of automatic tube current modulation on radiation dose and image quality for low tube voltage multidetector row CT angiography: Phantom study. Acad. Radiol. 2009, 16, 997–1002. [Google Scholar] [CrossRef]
- Den Harder, A.M.; Willemink, M.J.; De Ruiter, Q.M.; De Jong, P.A.; Schilham, A.M.; Krestin, G.P.; Leiner, T.; Budde, R.P. Dose reduction with iterative reconstruction for coronary CT angiography: A systematic review and meta-analysis. Br. J. Radiol. 2016, 89, 20150068. [Google Scholar] [CrossRef] [Green Version]
- Aschoff, A.J.; Catalano, C.; Kirchin, M.A.; Krix, M.; Albrecht, T. Low radiation dose in computed tomography: The role of iodine. Br. J. Radiol. 2017, 90, 20170079. [Google Scholar] [CrossRef]
- Wang, R.; Schoepf, U.J.; Wu, R.; Nance, J.W., Jr.; Lv, B.; Yang, H.; Li, F.; Lu, D.; Zhang, Z. Diagnostic accuracy of coronary CT angiography: Comparison of filtered back projection and iterative reconstruction with different strengths. J. Comput. Assist. Tomogr. 2014, 38, 179–184. [Google Scholar] [CrossRef]
- Buls, N.; Van Gompel, G.; Van Cauteren, T.; Nieboer, K.; Willekens, I.; Verfaillie, G.; Evans, P.; Macholl, S.; Newton, B.; De Mey, J. Contrast agent and radiation dose reduction in abdominal CT by a combination of low tube voltage and advanced image reconstruction algorithms. Eur. Radiol. 2015, 25, 1023–1031. [Google Scholar] [CrossRef] [Green Version]
- Klink, T.; Obmann, V.; Heverhagen, J.; Stork, A.; Adam, G.; Begemann, P. Reducing CT radiation dose with iterative reconstruction algorithms: The influence of scan and reconstruction parameters on image quality and CTDIvol. Eur. J. Radiol. 2014, 83, 1645–1654. [Google Scholar] [CrossRef] [PubMed]
- Padole, A.; Ali Khawaja, R.D.; Kalra, M.K.; Singh, S. CT radiation dose and iterative reconstruction techniques. AJR Am. J. Roentgenol. 2015, 204, W384–W392. [Google Scholar] [CrossRef] [PubMed]
- Geyer, L.L.; Schoepf, U.J.; Meinel, F.G.; Nance, J.W., Jr.; Bastarrika, G.; Leipsic, J.A.; Paul, N.S.; Rengo, M.; Laghi, A.; De Cecco, C.N. State of the Art: Iterative CT Reconstruction Techniques. Radiology 2015, 276, 339–357. [Google Scholar] [CrossRef] [PubMed]
- Mangold, S.; Wichmann, J.L.; Schoepf, U.J.; Litwin, S.E.; Canstein, C.; Varga-Szemes, A.; Muscogiuri, G.; Fuller, S.R.; Stubenrauch, A.C.; Nikolaou, K.; et al. Coronary CT angiography in obese patients using 3(rd) generation dual-source CT: Effect of body mass index on image quality. Eur. Radiol. 2016, 26, 2937–2946. [Google Scholar] [CrossRef]
- Wong, D.T.; Soh, S.Y.; Ko, B.S.; Cameron, J.D.; Crossett, M.; Nasis, A.; Troupis, J.; Meredith, I.T.; Seneviratne, S.K. Superior CT coronary angiography image quality at lower radiation exposure with second generation 320-detector row CT in patients with elevated heart rate: A comparison with first generation 320-detector row CT. Cardiovasc. Diagn. Ther. 2014, 4, 299–306. [Google Scholar] [CrossRef]
- Austen, W.G.; Edwards, J.E.; Frye, R.L.; Gensini, G.G.; Gott, V.L.; Griffith, L.S.; McGoon, D.C.; Murphy, M.L.; Roe, B.B. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 1975, 51, 5–40. [Google Scholar] [CrossRef] [Green Version]
- Deak, P.D.; Smal, Y.; Kalender, W.A. Multisection CT protocols: Sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 2010, 257, 158–166. [Google Scholar] [CrossRef] [Green Version]
- Modica, M.J.; Kanal, K.M.; Gunn, M.L. The obese emergency patient: Imaging challenges and solutions. Radiographics 2011, 31, 811–823. [Google Scholar] [CrossRef]
- Van Hamersvelt, R.W.; Eijsvoogel, N.G.; Mihl, C.; De Jong, P.A.; Schilham, A.M.R.; Buls, N.; Das, M.; Leiner, T.; Willemink, M.J. Contrast agent concentration optimization in CTA using low tube voltage and dual-energy CT in multiple vendors: A phantom study. Int. J. Cardiovasc. Imaging 2018, 34, 1265–1275. [Google Scholar] [CrossRef] [Green Version]
- Scholtz, J.E.; Ghoshhajra, B. Advances in cardiac CT contrast injection and acquisition protocols. Cardiovasc. Diagn. Ther. 2017, 7, 439–451. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Bolen, M.; Sydow, G.; Kottha, A.; Soufan, K.; Bullen, J.; Kemper, C.; Kalafut, J.; Halliburton, S.S. Adaptation of contrast injection protocol to tube potential for cardiovascular CT. AJR Am. J. Roentgenol. 2014, 203, 1181–1191. [Google Scholar] [CrossRef] [PubMed]
- Gudjonsdottir, J.; Ween, B.; Olsen, D.R. Optimal use of AEC in CT: A literature review. Radiol. Technol. 2010, 81, 309–317. [Google Scholar]
- Goenka, A.H.; Herts, B.R.; Obuchowski, N.A.; Primak, A.N.; Dong, F.; Karim, W.; Baker, M.E. Effect of reduced radiation exposure and iterative reconstruction on detection of low-contrast low-attenuation lesions in an anthropomorphic liver phantom: An 18-reader study. Radiology 2014, 272, 154–163. [Google Scholar] [CrossRef]
- Stocker, T.J.; Deseive, S.; Leipsic, J.; Hadamitzky, M.; Chen, M.Y.; Rubinshtein, R.; Heckner, M.; Bax, J.J.; Fang, X.-M.; Grove, E.L.; et al. Reduction in radiation exposure in cardiovascular computed tomography imaging: Results from the PROspective multicenter registry on radiaTion dose Estimates of cardiac CT angIOgraphy iN daily practice in 2017 (PROTECTION VI). Eur. Heart J. 2018, 39, 3715–3723. [Google Scholar] [CrossRef] [Green Version]
- Hamilton-Craig, C.R.; Tandon, K.; Kwan, B.; DeBoni, K.; Burley, C.; Wesley, A.J.; O’Rourke, R.; Neill, J.; Branch, K.R. Coronary CT radiation dose reduction strategies at an Australian Tertiary Care Center—Improvements in radiation exposure through an evidence-based approach. J. Med. Radiat. Sci. 2020, 67, 25–33. [Google Scholar] [CrossRef]
- Hedgire, S.S.; Baliyan, V.; Ghoshhajra, B.B.; Kalra, M.K. Recent advances in cardiac computed tomography dose reduction strategies: A review of scientific evidence and technical developments. J. Med. Imaging 2017, 4, 031211. [Google Scholar] [CrossRef] [Green Version]
- Litmanovich, D.E.; Tack, D.M.; Shahrzad, M.; Bankier, A.A. Dose reduction in cardiothoracic CT: Review of currently available methods. Radiographics 2014, 34, 1469–1489. [Google Scholar] [CrossRef] [Green Version]




| BMI < 25 | BMI ≥ 25 | p-Value | ||
|---|---|---|---|---|
| Number of patients | 45 | 42 | - | |
| Age | 60.80 ± 8.75 | 56.64 ± 10.67 | 0.049 * | |
| BMI (kg/m2) | 22.74 ± 1.33 | 27.93 ± 2.47 | <0.001 * | |
| SFOV | small | 0 | 0 | 0.583 |
| medium | 39 | 38 | ||
| large | 6 | 4 | ||
| Z-axis coverage | 12 cm | 0 | 2 | 0.293 |
| 14 cm | 18 | 18 | ||
| 16 cm | 27 | 22 | ||
| HR (bpm) | 65.16 ± 9.55 | 62.71 ± 8.61 | 0.215 | |
| HR variability (bpm) | 5.71 ± 4.72 | 5.57 ± 3.28 | 0.874 | |
| Tube voltage (kVp) | 112.44 ± 9.81 | 120.95 ± 6.17 | <0.001 * | |
| Tube current (mA) | 637.38 ± 92.17 | 701.67 ± 39.94 | <0.001 * | |
| Exposure time (s) | 0.74 ± 0.09 | 0.71 ± 0.11 | 0.259 | |
| CTDIvol (mGy) | 20.03 ± 6.22 | 24.83 ± 5.78 | <0.001 * | |
| DLP (mGy × cm) | 303.49 ± 96.21 | 372.89 ± 90.84 | 0.001 * | |
| Effective dose (mSv) | 4.25 ± 1.35 | 5.22 ± 1.27 | 0.001* | |
| BMI (kg/m2) | Number of Patients | Contrast Agent (mL) | Tube Voltage (kVp) | Tube Current (mA) | CTDIvol (mGy) | Effective Dose (mSv) | |
|---|---|---|---|---|---|---|---|
| BMI < 25 | <23 | 25 | 55.28 | 111.20 | 627.56 | 19.42 | 4.13 |
| 23–24 | 20 | 60.45 (p = 0.180) | 114.00 (p = 0.347) | 649.65 (p = 0.431) | 20.80 (p = 0.467) | 4.40 (p = 0.506) | |
| BMI ≥ 25 | 25–26 | 17 | 68.47 * (p < 0.001) | 118.82 * (p = 0.002) | 707.82 * (p = 0.001) | 24.32 * (p = 0.022) | 5.09 * (p = 0.040) |
| 27–28 | 14 | 73.14 * (p < 0.001) | 121.43 * (p < 0.001) | 705.71 * (p = 0.001) | 25.10 * (p = 0.012) | 5.20 * (p = 0.031) | |
| >28 | 11 | 82.36 * (p < 0.001) | 123.64 * (p = 0.001) | 687.00 * (p = 0.02) | 25.27 * (p = 0.026) | 5.44 * (p = 0.021) |
| BMI (kg/m2) | Number of Patients | NI (HU) | Noise Score | Image Noise (HU) | CNR | SNRL | SNRR | |||
|---|---|---|---|---|---|---|---|---|---|---|
| RCA | LAD | LCX | ||||||||
| BMI < 25 | <23 | 25 | 22.82 | 1.73 | 1.66 | 1.67 | 26.40 | 16.57 | 25.15 | 25.44 |
| 23–24 | 20 | 23.56 (p = 0.237) | 1.75 (p = 0.689) | 1.57 (p = 0.808) | 1.58 (p = 0.735) | 27.57 (p = 0.636) | 15.19 (p = 0.346) | 24.00 (p = 0.779) | 25.49 (p = 0.990) | |
| BMI ≥ 25 | 25–26 | 17 | 25.68 * (p < 0.001) | 1.76 (p = 0.460) | 1.65 (p = 0.739) | 1.63 (p = 0.755) | 29.45 (p = 0.272) | 14.24 (p = 0.148) | 19.92 (p = 0.080) | 18.16 * (p = 0.018) |
| 27–28 | 14 | 28.11 * (p < 0.001) | 2.18 * (p = 0.002) | 2.05 * (p = 0.006) | 2.07 * (p = 0.005) | 27.88 (p = 0.628) | 15.59 (p = 0.582) | 28.77 (p = 0.348) | 27.82 (p = 0.564) | |
| >28 | 11 | 30.64 * (p = 0.002) | 2.18 * (p = 0.011) | 2.09 * (p = 0.008) | 2.171 * (p = 0.014) | 30.93 (p = 0.133) | 12.79 * (p = 0.033) | 16.29 * (p = 0.004) | 18.46 * (p = 0.028) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Law, W.-Y.; Huang, G.-L.; Yang, C.-C. Effect of Body Mass Index in Coronary CT Angiography Performed on a 256-Slice Multi-Detector CT Scanner. Diagnostics 2022, 12, 319. https://doi.org/10.3390/diagnostics12020319
Law W-Y, Huang G-L, Yang C-C. Effect of Body Mass Index in Coronary CT Angiography Performed on a 256-Slice Multi-Detector CT Scanner. Diagnostics. 2022; 12(2):319. https://doi.org/10.3390/diagnostics12020319
Chicago/Turabian StyleLaw, Wei-Yip, Guan-Lin Huang, and Ching-Ching Yang. 2022. "Effect of Body Mass Index in Coronary CT Angiography Performed on a 256-Slice Multi-Detector CT Scanner" Diagnostics 12, no. 2: 319. https://doi.org/10.3390/diagnostics12020319
APA StyleLaw, W.-Y., Huang, G.-L., & Yang, C.-C. (2022). Effect of Body Mass Index in Coronary CT Angiography Performed on a 256-Slice Multi-Detector CT Scanner. Diagnostics, 12(2), 319. https://doi.org/10.3390/diagnostics12020319






