System 2 Diagnostic Process for the Next Generation of Physicians: “Inside” and “Outside” Brain—The Interplay between Human and Machine
Abstract
:1. Redefining System 2
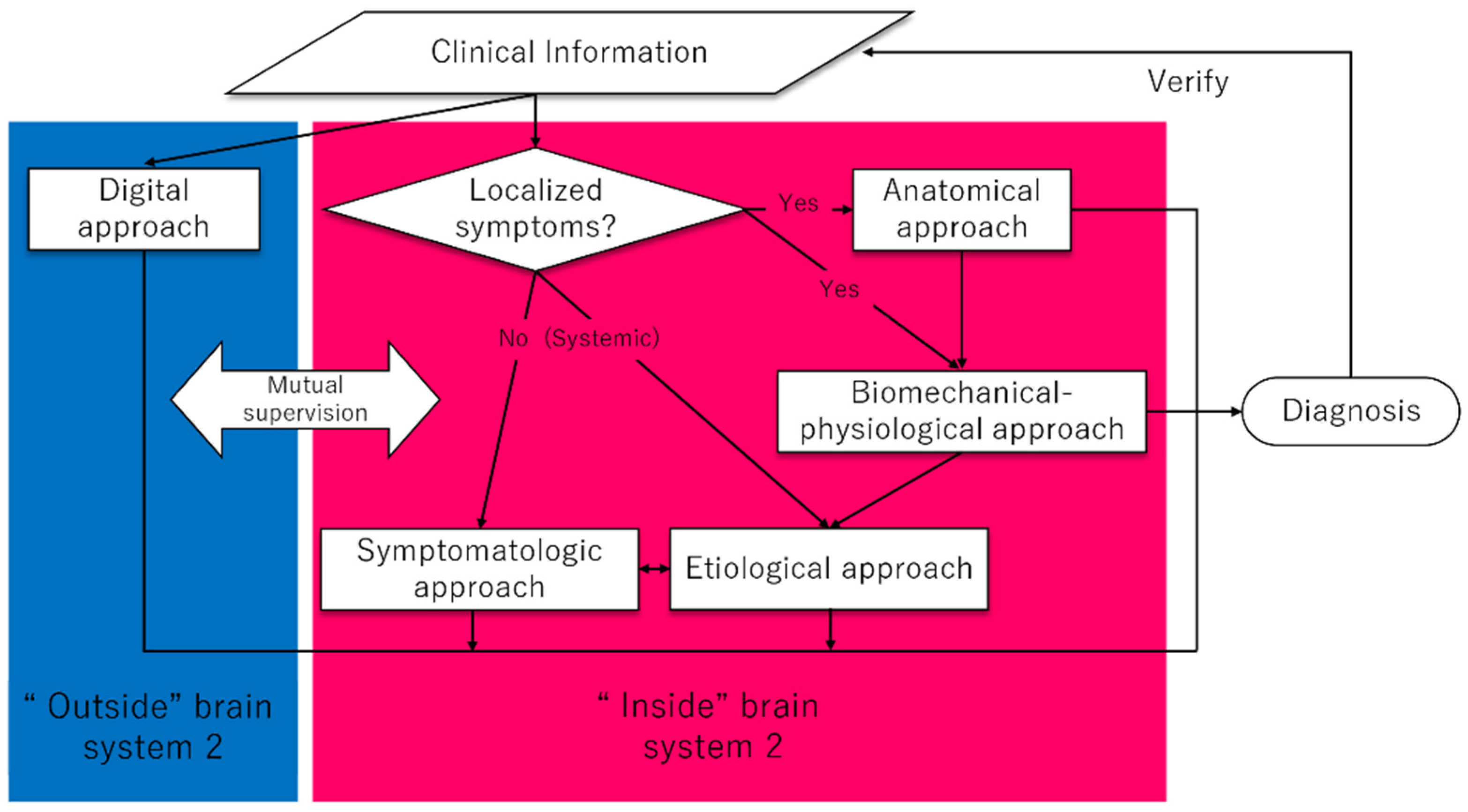
1.1. Dissecting System 2—“Inside” and “Outside”
1.2. Symptomatologic Approach
1.3. Anatomical Approach
1.4. Biomechanical-Physiological Approach
1.5. Etiological Approach
1.6. “ Outside” Brain
1.7. An Overview of the Proposed System 2
2. How to Nurture the Effective Application of system 2
2.1. Building Medical Knowledge as a Basis of System 2 Diagnostic Thinking
2.2. The Importance of Calibration, Reflective Practice, and Adaptive Training
2.3. Maximizing Collective Intelligence
2.4. The Key for Exceeding the Confronting Health Quality Problem from a System 2 Viewpoint
2.5. A Next-Generation Concept That May Compensate for the Weakness of DPT
3. Conclusions
Funding
Conflicts of Interest
References
- Balogh, E.P.; Miller, B.T.; Ball, J.R. The National Academies of Science Engineering and Medicine. In Improving Diagnosis in Health Care; The National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Merkebu, J.; Battistone, M.; McMains, K.; McOwen, K.; Witkop, C.; Konopasky, A.; Torre, D.; Holmboe, E.; Durning, S.J. Situativity: A Family of Social Cognitive Theories for Clinical Reasoning and Error. Diagnosis 2020, 7, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Graber, M.L. Progress understanding diagnosis and diagnostic errors: Thoughts at year 10. Diagnosis 2020, 7, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Croskerry, P. Clinical cognition and diagnostic error: Applications of a dual process model of reasoning. Adv. Health Sci. Educ. 2009, 14, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.; Young, M.; Brooks, L. Non-analytical models of clinical reasoning: The role of experience. Med. Educ. 2007, 41, 1140–1145. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Tokuda, Y. Real-world medical diagnosis: Intuitive process revisited (review). Int. J. Med. Med. Sci. 2012, 4, 177–179. [Google Scholar]
- Shimizu, T.; Matsumoto, K.; Tokuda, Y. Effects of the use of differential diagnosis checklist and general de-biasing checklist on diagnostic performance in comparison to intuitive diagnosis. Med. Teach. 2013, 35, e1218–e1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gopal, G.; Suter-Crazzolara, C.; Toldo, L.; Eberhardt, W. Digital transformation in healthcare—Architectures of present and future information technologies. Clin. Chem. Lab. Med. (CCLM) 2019, 57, 328–335. [Google Scholar] [CrossRef] [Green Version]
- Moya, I.M.A.; Rivas-Gándara, N.; Sarrias-Mercè, A.; Pérez-Rodón, J.; Roca-Luque, I. Syncope. Rev. Esp. Cardiol. 2012, 65, 755–765. [Google Scholar]
- Leo, M.; Betts, T.R. Risk stratification key in patients with syncope. Practitioner 2014, 257, 15–19. [Google Scholar]
- Anderson, M.; Hills-Meyer, P.R.; Stamm, J.M.; Brown, K. Integrating Clinical Reasoning Skills in a Pre-professional Undergraduate Human Anatomy Course. Anat. Sci. Educ. 2021. [Google Scholar] [CrossRef]
- Elizondo-Omaña, R.E.; López, S.G. The development of clinical reasoning skills: A major objective of the anatomy course. Anat. Sci. Educ. 2008, 1, 267–268. [Google Scholar] [CrossRef] [PubMed]
- Garibaldi, B.T.; Olson, A.P. The Hypothesis-Driven Physical Examination. Med. Clin. N. Am. 2018, 102, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Linardatos, P.; Papastefanopoulos, V.; Kotsiantis, S. Explainable AI: A Review of Machine Learning Interpretability Methods. Entropy 2020, 23, 18. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Tokuda, Y. Pivot and cluster strategy: A preventive measure against diagnostic errors. Int. J. Gen. Med. 2012, 5, 917–921. [Google Scholar] [CrossRef] [Green Version]
- May, J.E.; Blackburn, R.J.; Centor, R.M.; Dhaliwal, G. Pivot and Cluster: An Exercise in Clinical Reasoning. J. Gen. Intern. Med. 2017, 33, 226–230. [Google Scholar] [CrossRef] [Green Version]
- Yaguchi, Y.; Omura, M.; Okumura, T. Geometrical mapping of diseases with calculated similarity measure. In Proceedings of the 2017 IEEE International Conference on Bioinformatics and Biomedicine (BIBM), Kansas City, MO, USA, 13–16 November 2017; pp. 1131–1134. [Google Scholar]
- Shimizu, T. Horizontal and vertical tracing: A cognitive forcing strategy to improve diagnostic accuracy. Postgrad. Med. J. 2020, 96, 581–583. [Google Scholar] [CrossRef]
- Welsby, P.D. Does horizontal and vertical thinking provide the right angle of approach to complex problems? Postgrad. Med. J. 2020, 96, 580. [Google Scholar] [CrossRef]
- Norman, G.R.; Monteiro, S.D.; Sherbino, J.; Ilgen, J.S.; Schmidt, H.G.; Mamede, S. The Causes of Errors in Clinical Reasoning: Cognitive Biases, Knowledge Deficits, and Dual Process Thinking. Acad. Med. 2017, 92, 23–30. [Google Scholar] [CrossRef]
- Klement, B.J.; Paulsen, D.F.; Wineski, L.E. Clinical Correlations as a Tool in Basic Science Medical Education. J. Med. Educ. Curric. Dev. 2016, 3, 3. [Google Scholar] [CrossRef] [Green Version]
- Crosskerry, P. The Feedback Sanction. Acad. Emerg. Med. 2000, 7, 1232–1238. [Google Scholar] [CrossRef]
- Branson, C.F.; Williams, M.; Chan, T.M.; Graber, M.L.; Lane, K.P.; Grieser, S.; Landis-Lewis, Z.; Cooke, J.; Upadhyay, D.K.; Mondoux, S.; et al. Improving diagnostic performance through feedback: The Diagnosis Learning Cycle. BMJ Qual. Saf. 2021, 30, 1002–1009. [Google Scholar] [CrossRef] [PubMed]
- Mamede, S.; Schmidt, H.; Rikers, R. Diagnostic errors and reflective practice in medicine. J. Eval. Clin. Pract. 2007, 13, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Lambe, K.A.; O’Reilly, G.; Kelly, B.D.; Curristan, S. Dual-process cognitive interventions to enhance diagnostic reasoning: A systematic review. BMJ Qual. Saf. 2016, 25, 808–820. [Google Scholar] [CrossRef] [PubMed]
- Bass, A.; Geddes, C.; Wright, B.; Coderre, S.; Rikers, R.; McLaughlin, K. Experienced physicians benefit from analyzing initial diagnostic hypotheses. Can. Med. Educ. J. 2013, 4, e7–e15. [Google Scholar] [CrossRef]
- Mamede, S.; Schmidt, H.G. The structure of reflective practice in medicine. Med. Educ. 2004, 38, 1302–1308. [Google Scholar] [CrossRef]
- Shimizu, T. Reflection Of Reflections: Building Diagnostic Expertise. Int. J. Gen. Med. 2019, 2019, 363–365. [Google Scholar] [CrossRef] [Green Version]
- Ball, D.R.; Frerk, C. A new view of safety: Safety 2. Br. J. Anaesth. 2015, 115, 645–647. [Google Scholar] [CrossRef] [Green Version]
- Rudolph, J.W.; Simon, R.; Dufresne, R.L.; Raemer, D.B. There’s No Such Thing as "Nonjudgmental" Debriefing: A Theory and Method for Debriefing with Good Judgment. Simul. Healthc. 2006, 1, 49–55. [Google Scholar] [CrossRef] [Green Version]
- Croskerry, P. Adaptive expertise in medical decision making. Med. Teach. 2018, 40, 803–808. [Google Scholar] [CrossRef]
- Carpenter, J.; Sherman, M.T.; Kievit, R.A.; Seth, A.K.; Lau, H.; Fleming, S.M. Domain-general enhancements of metacognitive ability through adaptive training. J. Exp. Psychol. Gen. 2019, 148, 51–64. [Google Scholar] [CrossRef]
- Barnett, M.L.; Boddupalli, D.; Nundy, S.; Bates, D.W. Comparative Accuracy of Diagnosis by Collective Intelligence of Multiple Physicians vs Individual Physicians. JAMA Netw. Open 2019, 2, e190096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurvers, R.H.J.M.; Herzog, S.M.; Hertwig, R.; Krause, J.; Carney, P.A.; Bogart, A.; Argenziano, G.; Zalaudek, I.; Wolf, M. Boosting medical diagnostics by pooling independent judgments. Proc. Natl. Acad. Sci. USA 2016, 113, 8777–8782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kahneman, D.; Sibony, O.; Sunstein, C. Noise: A Flaw in Human Judgment; Little, Brown Spark: New York, NY, USA, 2021. [Google Scholar]
- Singh, H.; Meyer, A.N.D.; Thomas, E.J. The frequency of diagnostic errors in outpatient care: Estimations from three large observational studies involving US adult populations. BMJ Qual. Saf. 2014, 23, 727–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chi, C.-L.; Street, W.N.; Katz, D.A. A decision support system for cost-effective diagnosis. Artif. Intell. Med. 2010, 50, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Elkin, P.L.; Liebow, M.; Bauer, B.A.; Chaliki, S.; Wahner-Roedler, D.; Bundrick, J.; Lee, M.; Brown, S.H.; Froehling, D.; Bailey, K.; et al. The introduction of a diagnostic decision support system (DXplain™) into the workflow of a teaching hospital service can decrease the cost of service for diagnostically challenging Diagnostic Related Groups (DRGs). Int. J. Med. Inform. 2010, 79, 772–777. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozkan, I.A.; Koklu, M.; Sert, I.U. Diagnosis of urinary tract infection based on artificial intelligence methods. Comput. Methods Programs Biomed. 2018, 166, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Bright, T.J.; Wong, A.; Dhurjati, R.; Bristow, E.; Bastian, L.; Coeytaux, R.R.; Samsa, G.; Hasselblad, V.; Williams, J.W.; Musty, M.D.; et al. Effect of Clinical Decision-Support Systems. Ann. Intern. Med. 2012, 157, 29–43. [Google Scholar] [CrossRef] [PubMed]
- Chima, S.; Reece, J.; Milley, K.; Milton, S.; McIntosh, J.G.; Emery, J.D. Decision support tools to improve cancer diagnostic decision making in primary care: A systematic review. Br. J. Gen. Pract. 2019, 69, e809–e818. [Google Scholar] [CrossRef]
- Yoshida, E.; Fei, S.; Bavuso, K.; Lagor, C.; Maviglia, S. The Value of Monitoring Clinical Decision Support Interventions. Appl. Clin. Inform. 2018, 9, 163–173. [Google Scholar] [CrossRef] [Green Version]
- Lim, T.K. The predictive brain model in diagnostic reasoning. Asia Pac. Sch. 2021, 6, 1–8. [Google Scholar] [CrossRef]
| “Inside” Brain |
| Symptomatologic approach |
| Anatomical approach |
| Biomechanical-physiological approach |
| Etiological approach |
| “Outside” Brain |
| Digital approach |
| M | ental |
| E | ndocrine/Metabolic: GLUT-HUBS * |
| D | rug (Toxin, Drug, Nutritional, Lytes) |
| I | nflammation: Infection and Immune |
| C | urrent disturbance: ABCDEF-RUV † |
| I | atrogenic (including Foreign body)/Traumatic |
| N | eoplastic-Infiltrative |
| E | lse: Epidemiologic, Essential, Ectopic, Environmental |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shimizu, T. System 2 Diagnostic Process for the Next Generation of Physicians: “Inside” and “Outside” Brain—The Interplay between Human and Machine. Diagnostics 2022, 12, 356. https://doi.org/10.3390/diagnostics12020356
Shimizu T. System 2 Diagnostic Process for the Next Generation of Physicians: “Inside” and “Outside” Brain—The Interplay between Human and Machine. Diagnostics. 2022; 12(2):356. https://doi.org/10.3390/diagnostics12020356
Chicago/Turabian StyleShimizu, Taro. 2022. "System 2 Diagnostic Process for the Next Generation of Physicians: “Inside” and “Outside” Brain—The Interplay between Human and Machine" Diagnostics 12, no. 2: 356. https://doi.org/10.3390/diagnostics12020356
APA StyleShimizu, T. (2022). System 2 Diagnostic Process for the Next Generation of Physicians: “Inside” and “Outside” Brain—The Interplay between Human and Machine. Diagnostics, 12(2), 356. https://doi.org/10.3390/diagnostics12020356






