Pyloric Incompetence Associated with Helicobactor pylori Infection and Correlated to the Severity of Atrophic Gastritis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Protocols
2.2. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Participants
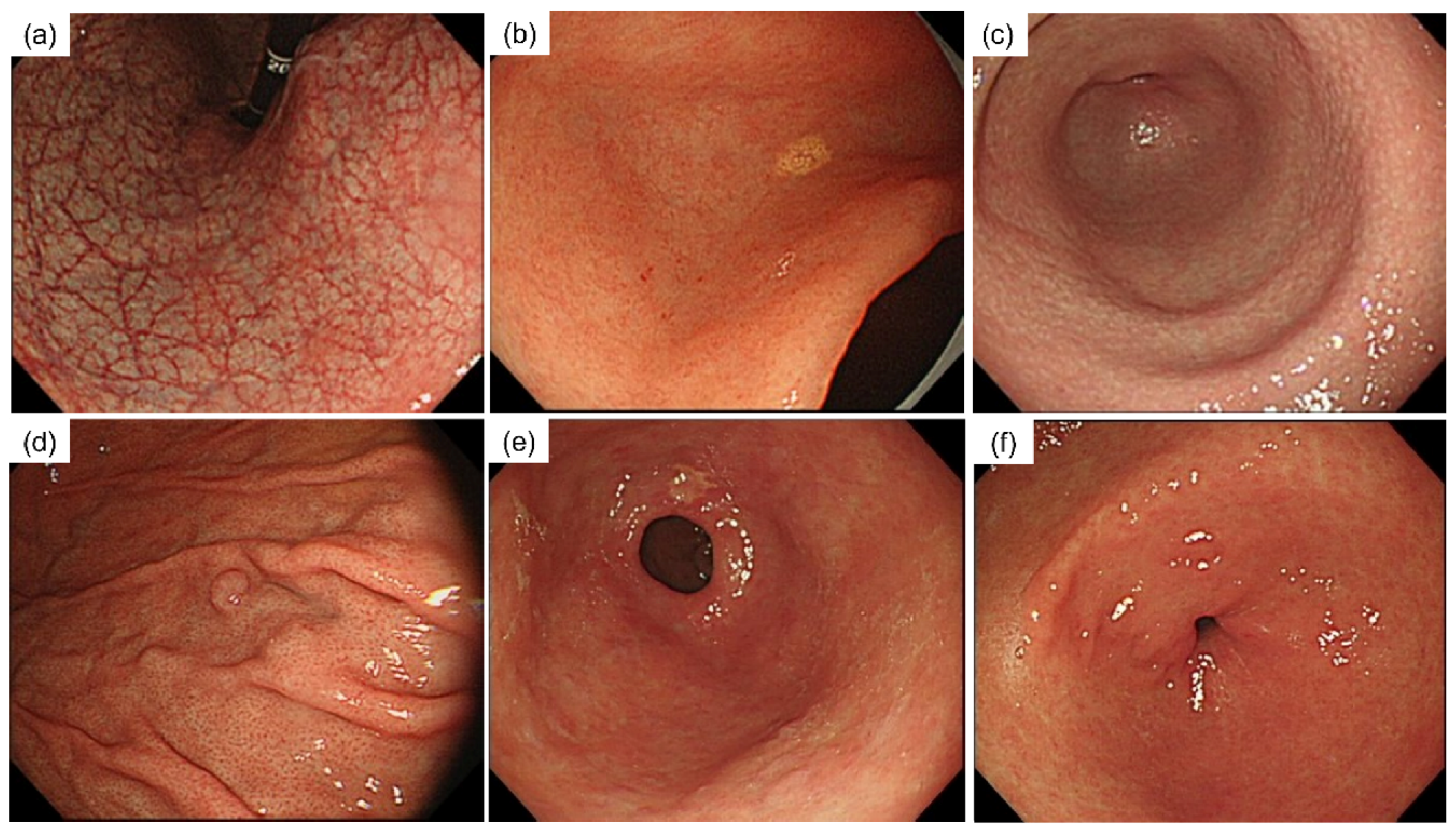
3.2. Comparison of Factors according to the Competency of the Pylorus
3.3. Incompetence of the Pylorus as a Predictive Endoscopic Finding for H. pylori Infection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lord, R.V.N.; DeMeester, S.R.; Peters, J.H.; Hagen, J.A.; Elyssnia, D.; Sheth, C.T.; DeMeester, T.R. Hiatal hernia, lower esophageal sphincter incompetence, and effectiveness of nissen fundoplication in the spectrum of gastroesophageal reflux disease. J. Gastrointest. Surg. 2009, 13, 602–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fein, M.; Fuchs, K.-H.; Bohrer, T.; Freys, S.M.; Thiede, A. Fiberoptic technique for 24-hour bile reflux monitoring: Standards and normal values for gastric monitoring. Dig. Dis. Sci. 1996, 41, 216–225. [Google Scholar] [CrossRef] [PubMed]
- Stein, H.J.; Smyrk, T.C.; Demeester, T.R.; Rouse, J.; Hinder, R.A. Clinical value of endoscopy and histology in the diagnosis of duodenogastric reflux disease. Surgery 1992, 112, 796–803. [Google Scholar] [PubMed]
- Vaezi, M.F.; Richter, J.E. Importance of duodeno-gastro-esophageal reflux in the medical outpatient practice. Hepatogastroenterology 1999, 46, 40–47. [Google Scholar] [PubMed]
- Keane, F.B.; Dimagno, E.P.; Malagelada, J.-R. Duodenogastric reflux in humans: Its relationship to fasting antroduodenal motility and gastric, pancreatic, and biliary secretion. Gastroenterology 1981, 81, 726–731. [Google Scholar] [CrossRef]
- Othman, A.A.; Dwedar, A.A.; ElSadek, H.M.; AbdElAziz, H.R.; Abdelrahman, A.A. Bile reflux gastropathy: Prevalence and risk factors after therapeutic biliary interventions: A retrospective cohort study. Ann. Med. Surg. 2021, 72, 103168. [Google Scholar] [CrossRef]
- Lake, A.; Rao, S.S.C.; Larion, S.; Spartz, H.; Kavuri, S. Bile reflux gastropathy and functional dyspepsia. J. Neurogastroenterol. Motil. 2021, 27, 400–407. [Google Scholar] [CrossRef]
- Ladas, S.D.; Katsogridakis, J.; Malamou, H.; Giannopoulou, H.; Kesse-Elia, M.; Raptis, S.A. Helicobacter pylori may induce bile reflux: Link between H. pylori and bile induced injury to gastric epithelium. Gut 1996, 38, 15–18. [Google Scholar] [CrossRef] [Green Version]
- Tireli, M. The results of the surgical treatment of alkaline reflux gastritis. Hepatogastroenterology 2012, 59, 2352–2356. [Google Scholar] [CrossRef]
- Romagnoli, R.; Collard, J.M.; Bechi, P.; Salizzoni, M. Gastric symptoms and duodenogastric reflux in patients referred for gastroesophageal reflux symptoms and endoscopic esophagitis. Surgery 1999, 125, 480–486. [Google Scholar] [CrossRef]
- Maguilnik, I.; Neumann, W.L.; Sonnenberg, A.; Genta, R.M. Reactive gastropathy is associated with inflammatory conditions throughout the gastrointestinal tract. Aliment. Pharmacol. Ther. 2012, 36, 736–743. [Google Scholar] [CrossRef] [PubMed]
- Vaezi, M.F.; Richter, J.E. Duodenogastroesophageal reflux and methods to monitor nonacidic reflux. Am. J. Med. 2001, 111, 160–168. [Google Scholar] [CrossRef]
- Atak, I.; Ozdil, K.; Yucel, M.; Caliskan, M.; Kilic, A.; Erdem, H.; Alimoglu, O. The effect of laparoscopic cholecystectomy on the development of alkaline reflux gastritis and intestinal metaplasia. Hepatogastroenterology 2012, 59, 59–61. [Google Scholar] [CrossRef] [PubMed]
- Vere, C.C.; Cazacu, S.; Comănescu, V.; Mogoanta, L.; Rogoveanu, I.; Ciurea, T. Endoscopical and histological features in bile reflux gastritis. Rom. J. Morphol. Embryol. 2005, 46, 269–274. [Google Scholar]
- Chen, L.; Zhu, G.; She, L.; Ding, Y.; Yang, C.; Zhu, F. Analysis of risk factors and establishment of a prediction model for endoscopic primary bile reflux: A single-center retrospective study. Front. Med. 2021, 8, 758771. [Google Scholar] [CrossRef]
- Cocking, J.B.; Grech, P. Pyloric reflux and the healing of gastric ulcers. Gut 1973, 14, 555–557. [Google Scholar] [CrossRef] [Green Version]
- Hermans, D.; Sokal, E.-M.; Collard, J.-M.; Romagnoli, R.; Buts, J.-P. Primary duodenogastric reflux in children and adolescents. Eur. J. Pediatr. 2003, 162, 598–602. [Google Scholar] [CrossRef]
- Davenport, H.W. Destruction of the gastric mucosal barrier by detergents and urea. Gastroenterology 1968, 54, 175–181. [Google Scholar] [CrossRef]
- Rhodes, J.; Barnardo, D.E.; Phillips, S.F.; Rovelstad, R.A.; Hofmann, A.F. Increased reflux of bile into the stomach in patients with gastric ulcer. Gastroenterology 1969, 57, 241–252. [Google Scholar] [CrossRef]
- Rovelstad, R.A. The incompetent pyloric sphincter. Bile and mucosal ulceration. Am. J. Dig. Dis. 1976, 21, 165–173. [Google Scholar] [CrossRef]
- Flint, F.J.; Grech, P. Pyloric regurgitation and gastric ulcer. Gut 1970, 11, 735–737. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Read, N.W.; Grech, P. Effect of cigarette smoking on competence of the pylorus: Preliminary study. BMJ 1973, 3, 313–316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valenzuela, J.E.; Defilippi, C.; Csendes, A. Manometric studies on the human pyloric sphincter: Effect of cigarette smoking, metoclopramide, and atropine. Gastroenterology 1976, 70, 481–483. [Google Scholar] [CrossRef]
- Code, C.F. On pyloric sphincter incompetence in man. Gastroenterology 1970, 59, 645–646. [Google Scholar] [CrossRef]
- Garrett, J.M.; Summerskill, W.H.J.; Code, C.F. Antral motility in patients with gastric ulcer. Am. J. Dig. Dis. 1966, 11, 780–789. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.R.; Marshall, B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet 1983, 1, 1273–1275. [Google Scholar]
- Li, D.; Zhang, J.; Yao, W.Z.; Zhang, D.L.; Feng, C.C.; He, Q.; Lv, H.H.; Cao, Y.P.; Wang, J.; Qi, Y.; et al. The relationship between gastric cancer, its precancerous lesions and bile reflux: A retrospective study. J. Dig. Dis. 2020, 21, 222–229. [Google Scholar] [CrossRef]
- Szőke, A.; Mocan, S.; Negovan, A. Helicobacter pylori infection over bile reflux: No influence on the severity of endoscopic or premalignant gastric lesion development. Exp. Ther. Med. 2021, 22, 766. [Google Scholar] [CrossRef]
- Itoh, T.; Kawahira, H.; Nakashima, H.; Yata, N. Deep learning analyzes Helicobacter pylori infection by upper gastrointestinal endoscopy images. Endosc. Int. Open 2018, 6, E139–E144. [Google Scholar] [CrossRef] [Green Version]
- Toyoshima, O.; Nishizawa, T.; Sakitani, K.; Yamakawa, T.; Takahashi, Y.; Yamamichi, N.; Hata, K.; Seto, Y.; Koike, K.; Watanabe, H.; et al. Serum anti-Helicobacter pylori antibody titer and its association with gastric nodularity, atrophy, and age: A cross-sectional study. World J. Gastroenterol. 2018, 24, 4061–4068. [Google Scholar] [CrossRef]
- Terasawa, T.; Nishida, H.; Kato, K.; Miyashiro, I.; Yoshikawa, T.; Takaku, R.; Hamashima, C. Prediction of gastric cancer development by serum pepsinogen test and Helicobacter pylori seropositivity in eastern Asians: A systematic review and meta-analysis. PLoS ONE 2014, 9, e109783. [Google Scholar] [CrossRef] [PubMed]
- Dacha, S.; Razvi, M.; Massaad, J.; Cai, Q.; Wehbi, M. Hypergastrinemia. Gastroenterol. Rep. 2015, 3, 201–208. [Google Scholar] [CrossRef] [Green Version]
- Graham, D.Y.; Osato, M.S. H. pylori in the pathogenesis of duodenal ulcer: Interaction between duodenal acid load, bile, and H. pylori. Am. J. Gastroenterol. 2000, 95, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Sobala, G.M.; O’Connor, H.J.; Dewar, E.P.; King, R.F.; Axon, A.T.; Dixon, M.F. Bile reflux and intestinal metaplasia in gastric mucosa. J. Clin. Pathol. 1993, 46, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Matsuhisa, T.; Arakawa, T.; Watanabe, T.; Tokutomi, T.; Sakurai, K.; Okamura, S.; Chono, S.; Kamada, T.; Sugiyama, A.; Fujimura, Y.; et al. Relation between bile acid reflux into the stomach and the risk of atrophic gastritis and intestinal metaplasia: A multicenter study of 2283 cases. Dig. Endosc. 2013, 25, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.C.; Piazuelo, M.B.; Kuipers, E.J.; Li, D. AGA clinical practice update on the diagnosis and management of atrophic gastritis: Expert review. Gastroenterology 2021, 161, 1325–1332.e7. [Google Scholar] [CrossRef] [PubMed]
- Lahner, E.; Conti, L.; Annibale, B.; Corleto, V.D. Current perspectives in atrophic gastritis. Curr. Gastroenterol. Rep. 2020, 22, 38. [Google Scholar] [CrossRef]
- Butt, J.; Varga, M.G.; Wang, T.; Tsugane, S.; Shimazu, T.; Zheng, W.; Abnet, C.C.; Yoo, K.-Y.; Park, S.K.; Kim, J.; et al. Smoking, Helicobacter pylori serology, and gastric cancer risk in prospective studies from China, Japan, and Korea. Cancer Prev. Res. 2019, 12, 667–674. [Google Scholar] [CrossRef] [Green Version]
- Xiao, S.; Fan, Y.; Yin, Z.; Zhou, L. Endoscopic grading of gastric atrophy on risk assessment of gastric neoplasia: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2021, 36, 55–63. [Google Scholar] [CrossRef]
- Shichijo, S.; Hirata, Y.; Niikura, R.; Hayakawa, Y.; Yamada, A.; Koike, K. Association between gastric cancer and the Kyoto classification of gastritis. J. Gastroenterol. Hepatol. 2017, 32, 1581–1586. [Google Scholar] [CrossRef]
- Masuyama, H.; Yoshitake, N.; Sasai, T.; Nakamura, T.; Masuyama, A.; Zuiki, T.; Kurashina, K.; Mieda, M.; Sunada, K.; Yamamoto, H.; et al. Relationship between the degree of endoscopic atrophy of the gastric mucosa and carcinogenic risk. Digestion 2015, 91, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Öztekin, M.; Yılmaz, B.; Ağagündüz, D.; Capasso, R. Overview of Helicobacter pylori infection: Clinical features, treatment, and nutritional aspects. Diseases 2021, 9, 66. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.K.S.; Luiz, L.; Silva, D.L.; Miguel, M.P.; José, A.; Blanco, V.; Carneiro, L.C.; Barbosa, M.S. Helicobacter pylori cagA virulence gene and severe esogastroduodenal diseases: Is there an association? Arq. Gastroenterol. 2021, 54, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Vdovychenko, A. Is a bile reflux an additional cancerogenic factor in peptic ulcer, associated with Helicobacter pylori infection? Rocz. Akad. Med. Bialymst. 2004, 49, 72–74. [Google Scholar]
- Hooi, J.K.Y.; Lai, W.Y.; Ng, W.K.; Suen, M.M.Y.; Underwood, F.E.; Tanyingoh, D.; Malfertheiner, P.; Graham, D.Y.; Wong, V.W.S.; Wu, J.C.Y.; et al. Global prevalence of Helicobacter pylori infection: Systematic review and meta-analysis. Gastroenterology 2017, 153, 420–429. [Google Scholar] [CrossRef] [Green Version]
- Yoshii, S.; Mabe, K.; Watano, K.; Ohno, M.; Matsumoto, M.; Ono, S.; Kudo, T.; Nojima, M.; Kato, M.; Sakamoto, N. Validity of endoscopic features for the diagnosis of Helicobacter pylori infection status based on the Kyoto classification of gastritis. Dig. Endosc. 2020, 32, 74–83. [Google Scholar] [CrossRef] [Green Version]
- Lim, H.-J.; Kim, H.D.; Soh, J.S.; Kim, S.-Y.; Jung, Y.-J.; Lim, H.; Kang, H.S.; Kim, J.H. Discrete terminal ileal ulcers in patients diagnosed with ulcerative colitis: Clinical significance and natural course. BMC Gastroenterol. 2021, 21, 285. [Google Scholar] [CrossRef]

| n = 502 | ||
|---|---|---|
| Age (yr) | 53.0 ± 10.9 | |
| Male Sex | 217 | (43.2) |
| PG I (ng/mL) | 54.50 | (39.4) |
| PG II (ng/mL) | 15.25 | (11.4) |
| Serum gastrin * (pg/mL) | 158.21 ± 100.34 | |
| PG I/PG II ratio | 4.31 ± 1.84 | |
| anti-H. pylori-Ab positivity | 200 | (39.8) |
| Endoscopic atrophy classification | ||
| C-0 | 90 | (17.9) |
| C-I | 163 | (32.5) |
| C-II | 101 | (20.1) |
| C-III | 38 | (7.6) |
| O-I | 63 | (12.5) |
| O-II | 22 | (4.4) |
| O-III | 25 | (5.0) |
| Nodular gastritis | 11 | (2.2) |
| Incompetent pylorus | 55 | (11.0) |
| Pylorus | p-Value | ||
|---|---|---|---|
| Normal (n = 447) | Incompetent (n = 55) | ||
| Male | 192 (43.0) | 25 (45.5) | 0.834 |
| Age (yr), | 52.8 ± 10.8 | 54.8 ± 11.3 | 0.214 |
| Serum gastrin * (pg/mL) | 157.3 ± 97.7 | 165.2 ± 120.2 | 0.647 |
| PG I (ng/mL) | 55.3 ± 40.9 | 48.0 ± 23.5 | 0.054 |
| PG II (ng/mL) | 15.3 (11.7) | 14.7 ± 7.8 | 0.612 |
| PG I/PG II ratio | 4.4 ± 1.8 | 3.8 ± 1.9 | 0.043 |
| anti-H. pylori-Ab positivity | 166 (37.1) | 34 (61.8) | <0.001 |
| Atrophic gastritis ** | 358 (80.1) | 54 (98.2) | 0.001 |
| Nodular_gastritis | 10 (2.2) | 1 (1.8) | 1.000 |
| Xanthoma | 21 (4.7) | 6 (10.9) | 0.054 |
| β * | SE | z Value | Odds Ratio | 95% CI | p-Value | |
|---|---|---|---|---|---|---|
| Age > 53 | 0.05 | 0.29 | 0.34 | 0.91 | 0.51–1.60 | 0.733 |
| Male Sex | −0.10 | 0.31 | 0.17 | 1.05 | 0.58–1.93 | 0.868 |
| anti-H. pylori-Ab positivity | 0.99 | 0.31 | 3.22 | 2.70 | 1.47–4.94 | 0.001 |
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| NG | 4.3 | 99.8 | 81.8 | 58.9 |
| Xanthoma | 11.4 | 99.0 | 88.9 | 60.6 |
| FGP absence | 16.5 | 97.6 | 90.6 | 60.6 |
| IP | 16.6 | 93.1 | 63.6 | 60.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakaguchi, T.; Sugihara, T.; Ohnita, K.; Fukuda, D.; Honda, T.; Ogihara, R.; Kurumi, H.; Yashima, K.; Isomoto, H. Pyloric Incompetence Associated with Helicobactor pylori Infection and Correlated to the Severity of Atrophic Gastritis. Diagnostics 2022, 12, 572. https://doi.org/10.3390/diagnostics12030572
Sakaguchi T, Sugihara T, Ohnita K, Fukuda D, Honda T, Ogihara R, Kurumi H, Yashima K, Isomoto H. Pyloric Incompetence Associated with Helicobactor pylori Infection and Correlated to the Severity of Atrophic Gastritis. Diagnostics. 2022; 12(3):572. https://doi.org/10.3390/diagnostics12030572
Chicago/Turabian StyleSakaguchi, Takuki, Takaaki Sugihara, Ken Ohnita, Daisuke Fukuda, Tetsuro Honda, Ryohei Ogihara, Hiroki Kurumi, Kazuo Yashima, and Hajime Isomoto. 2022. "Pyloric Incompetence Associated with Helicobactor pylori Infection and Correlated to the Severity of Atrophic Gastritis" Diagnostics 12, no. 3: 572. https://doi.org/10.3390/diagnostics12030572






