Daytime versus Nighttime in Acute Appendicitis
Abstract
:1. Introduction
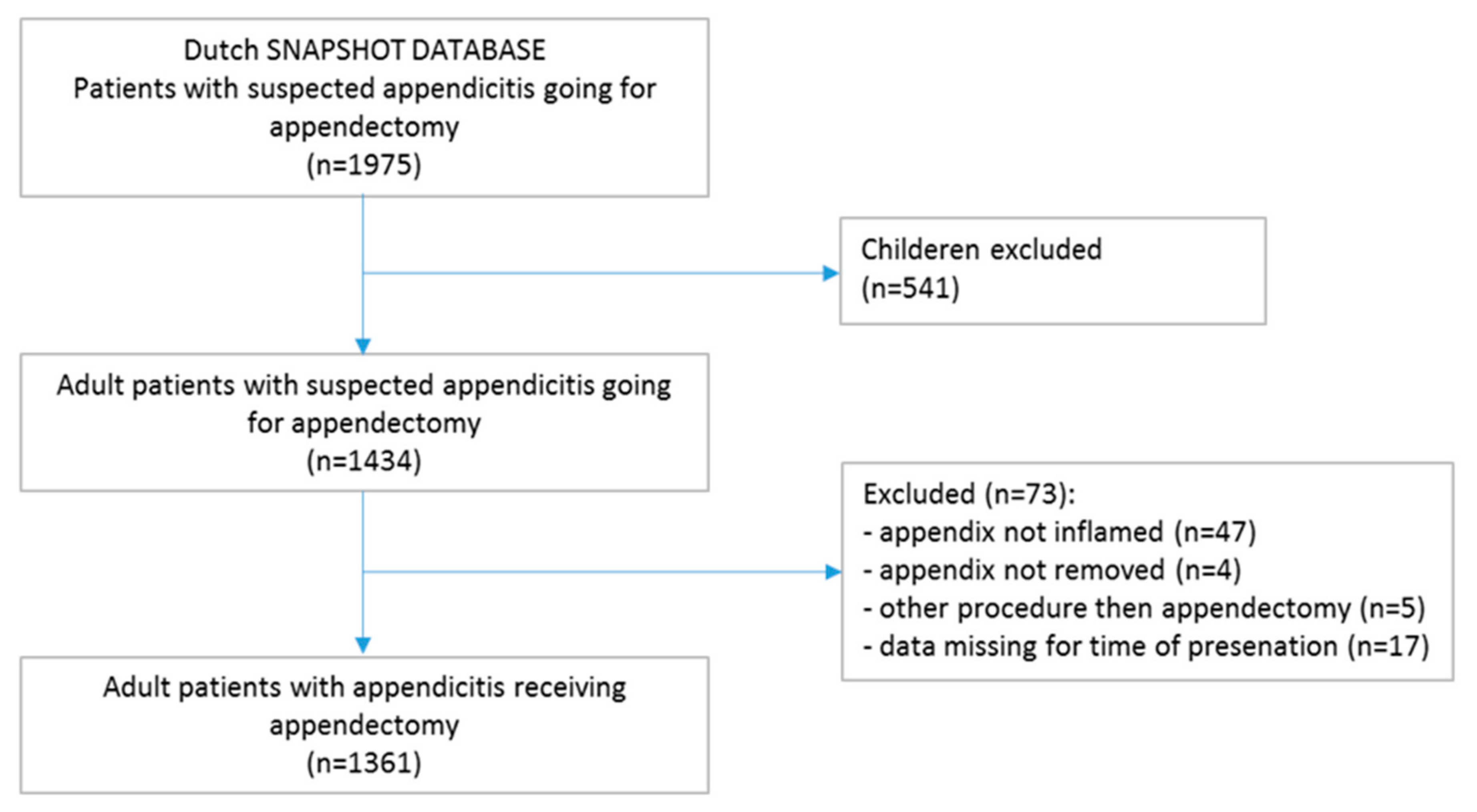
2. Materials and Methods
2.1. Study Design
2.2. Baseline Characteristics
2.3. Primary Outcomes
- The proportion of patients with complicated appendicitis presenting during daytime period versus nighttime period;
- The proportion of patients with a postoperative complication for patients with acute appendicitis who present during daytime versus those at nighttime.
2.4. Secondary Outcomes
2.5. Definitions and Outcome Characteristics
2.6. Data Analysis
3. Results
3.1. Baseline Characteristics
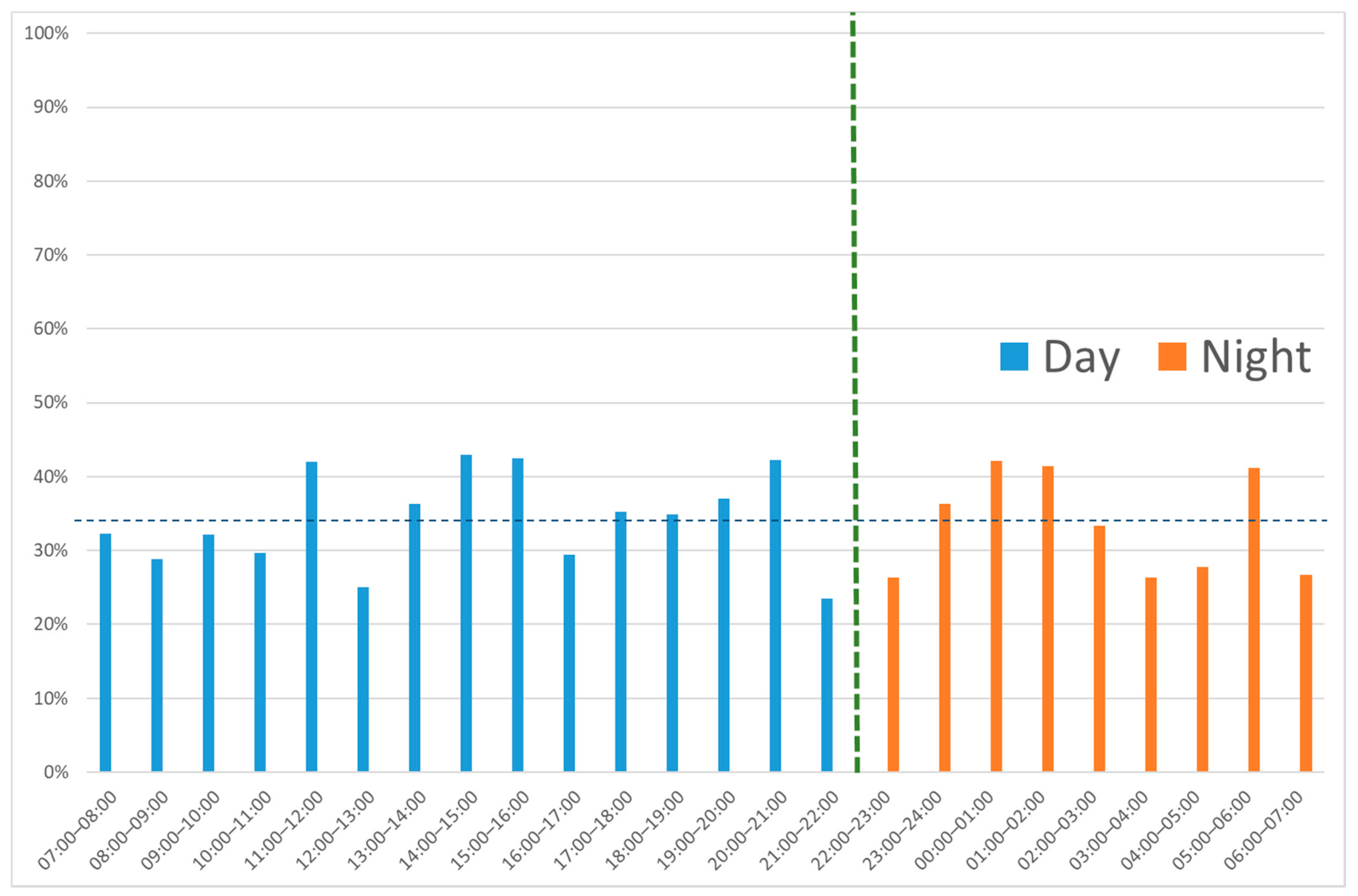
3.2. Primary Outcome
- At daytime, 390 of 1130 patients (34.5%) had a complicated appendicitis compared with 79 of 231 (34.2%) at nighttime (p = 0.93). No statistically significant difference in the proportion of patients with complicated appendicitis per daily hour was found (p = 0.44). (Figure 3).
- Forty-three of 231 (18.6%) nighttime patients developed a postoperative complication versus 137 of 1130 (12.1%) daytime patients (p = 0.008) (Table 2).
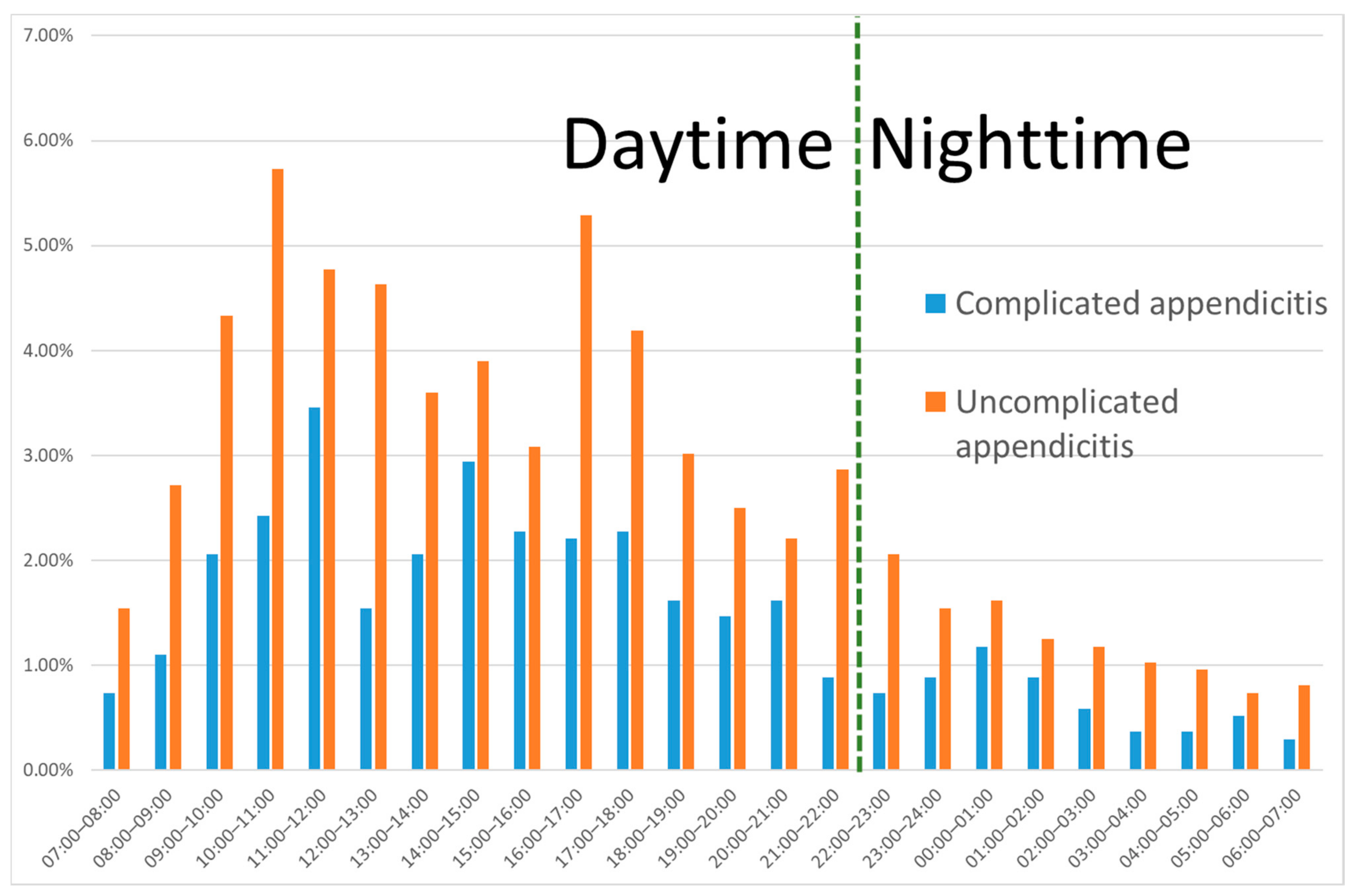
3.3. All Appendicitis
3.4. Uncomplicated Appendicitis
3.5. Complicated Appendicitis
3.6. Multivariate Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- van Dijk, S.T.; van Dijk, A.H.; Dijkgraaf, M.G.; Boermeester, M.A. Meta-analysis of in-hospital delay before surgery as a risk factor for complications in patients with acute appendicitis. Br. J. Surg. 2018, 105, 933–945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NvvH. Richtlijn Beleid Rondom Spoedoperaties [Guideline]. 2018. Available online: https://richtlijnendatabase.nl/richtlijn/beleid_rondom_spoedoperaties/startpagina_-_beleid_rondom_spoedoperaties.html (accessed on 1 January 2022).
- NVvH. Richtlijn Acute Appendicitis [Guideline]. 2019. Available online: https://richtlijnendatabase.nl/richtlijn/acute_appendicitis/startpagina_-_acute_appendicitis.html (accessed on 1 January 2022).
- Drake, F.T.; Mottey, N.E.; Castelli, A.A.; Florence, M.G.; Johnson, M.G.; Steele, S.R.; Writing Group for SCOAP-CERTAIN. Time-of-Day and Appendicitis: Impact on Management and Outcomes. Surgery 2017, 161, 405–414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Rossem, C.C.; Bolmers, M.D.; Schreinemacher, M.H.; van Geloven, A.A.; Bemelman, W.A. Prospective nationwide outcome audit of surgery for suspected acute appendicitis. Br. J. Surg. 2016, 103, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Bolmers, M.D.M.; de Jonge, J.; van Rossem, C.C.; van Geloven, A.A.W.; Bemelman, W.A. Discrepancies between Intraoperative and Histological Evaluation of the Appendix in Acute Appendicitis. J. Gastrointest. Surg. 2019, 24, 2088–2095. [Google Scholar] [CrossRef] [PubMed]
| % Missing | All Appendicitis (n = 1361) | Uncomplicated Appendicitis (n = 892) | Complicated Appendicitis (n = 469) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Day (n = 1130) | Night (n = 231) | p-Value | Day (n = 740) | Night (n = 152) | p-Value | Day (n = 390) | Night (n = 79) | p-Value | ||
| Age (years) | 0% | 40 (28–55) | 33 (25–48) | <0.001 | 36 (25–50) | 29 (22–42) | <0.001 | 50 (35–62) | 49 (32–63) | 0.68 |
| % male | 0% | 50.2% | 58.1% | 0.55 | 49.7% | 46.1% | 0.41 | 51.0% | 51.9% | 0.89 |
| Days of complaints | 2.2% | 1 (1–2) | 1 (1–2) | <0.001 | 1 (1–2) | 1 (1–1) | <0.001 | 2 (1–3) | 1 (1–1) | 0.15 |
| Absence of diffuse peritonitis | 3.7% | 90.1% | 91.0% | 0.69 | 93.6% | 95.9% | 0.28 | 83.5% | 81.3% | 0.65 |
| Migrating pain | 2.9% | 44.0% | 40.4% | 0.32 | 44.7% | 45.0% | 0.95 | 42.8% | 31.6% | 0.069 |
| Vomiting | 2.2% | 33.1% | 42.7% | 0.005 | 27.6% | 37.3% | 0.017 | 43.5% | 53.2% | 0.12 |
| ASA 1 or 2 | 0% | 95.8% | 98.3% | 0.077 | 96.5% | 100% | 0.014 # | 94.6% | 94.9% | 1.0 # |
| Temperature (°C) * | 5.6% | 37.4 (0.8) | 37.4 (0.7) | 0.57 | 37.3 (0.7) | 37.4 (0.7) | 0.034 | 37.7 (0.8) | 37.5 (0.7) | 0.108 * |
| Leucocytes (109/L) * | 0.1% | 13.6 (4.5) | 14.6 (4.5) | 0.004 | 13.1 (4.4) | 14.2 (4.2) | 0.007 | 14.5 (4.4) | 15.3 (5.0) | 0.194 * |
| Complicated appendicitis on imaging | 0% | 15.9% | 16.0% | 0.97 | 6.6% | 7.2% | 0.78 | 33.6% | 32.9% | 0.91 |
| CRP (mmol/L) | 0.4% | 41 (16–88) | 20 (6–66) | <0.001 | 30 (11–60) | 13 (4–38) | <0.001 | 86 (36–173) | 68 (17–141) | 0.049 |
| Time to surgery (h) | 0.6% | 6.3 (4.3–10.8) | 13.9 (10–17) | <0.001 | 6 (4–11) | 14 (11–17) | <0.001 | 6 (4–11) | 14 (10–18) | <0.001 |
| Surgery < 8 h | 0.6% | 64.1% | 14.7% | <0.001 | 66% | 13.2% | <0.001 | 61.1% | 17.7% | <0.001 |
| Surgery by resident without supervision | 0% | 18.4% | 23.4% | 0.081 | 19.7% | 28.3% | 0.019 | 15.9% | 13.9% | 0.66 |
| Surgical time (min) | 4.5% | 42 (32–55) | 45 (35–57) | 0.11 | 40(30–50) | 42 (32–54) | 0.06 | 48 (36–64) | 51 (37–60) | 0.91 |
| Laparoscopic surgery | 0% | 79.2% | 81.8% | 0.37 | 79.1% | 82.9% | 0.28 | 79.5% | 79.7% | 0.96 |
| All Appendicitis (n = 1361) | Uncomplicated Appendicitis (n = 892) | Complicated Appendicitis (n = 469) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Day (n = 1130) | Night (n = 231) | p-Value | Day (n = 740) | Night (n = 152) | p-Value | Day (n = 390) | Night (n = 79) | p-Value | |
| Perforated appendicitis 1 | 19.1% | 22.1% | 0.30 | - | - | - | 55.4% | 64.6% | 0.13 |
| Complications (overall) | 12.1% | 18.6% | 0.008 | 7.7% | 11.8% | 0.09 | 20.5% | 31.6% | 0.03 |
| Infectious complications | 6.8% | 10.8% | 0.04 | 4.2% | 5.9% | 0.35 | 11.8% | 20.3% | 0.04 |
| Mortality | 0.2% | 0% | 1.0 # | 0.1 | 0 | 1.0 # | 0.3% | 0% | 1.0 # |
| Reinterventions | 2.4% | 6.1% | 0.003 | 1.4% | 3.9% | 0.04 # | 4.4% | 10.1% | 0.05 # |
| Hospitalization days | 2 (1–4) | 2 (1–4) | 0.89 | 2 (1–2) | 2 (1–2) | 0.46 | 5 (3–6) | 4 (3–7) | 0.70 |
| Re-admission | 5.5% | 8.7% | 0.07 | 4.5% | 7.9% | 0.08 | 7.4% | 10.1% | 0.42 |
| Univariable Odds Ratio | Multivariate Adjusted Odds Ratio | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Age (per year) | 1.03 | 1.02–1.04 | <0.001 | 1.02 | 1.01–1.03 | <0.001 |
| Days of complaints | 1.14 | 1.05–1.24 | 0.001 | - | - | - |
| Diffuse peritonitis | 1.71 | 1.07–2.73 | 0.025 | - | - | - |
| Vomiting | 1.08 | 0.77–1.50 | 0.66 | - | - | - |
| ASA 3 or 4 | 2.89 | 1.55–5.40 | 0.001 | - | - | - |
| Temperature (per °C) | 1.31 | 1.06–1.60 | 0.01 | - | - | - |
| Leucocytes (per 109/L) | 1.03 | 0.99–1.06 | 0.11 | - | - | - |
| CRP (per mmol/L) | 1.004 | 1.003–1.006 | <0.001 | 1.003 | 1.001–1.005 | 0.002 |
| Complicated appendicitis on imaging | 2.26 | 1.56–3.25 | <0.001 | 1.67 | 1.13–2.48 | 0.01 |
| Surgery > 8 h | 1.54 | 1.12–2.11 | 0.008 | 1.37 | 0.97–1.95 | 0.078 |
| Presenting at nighttime | 1.66 | 1.14–2.42 | 0.008 | 1.74 | 1.14–2.66 | 0.010 |
| Surgery by resident without supervision | 1.06 | 0.71–1.57 | 0.78 | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bom, W.J.; de Jonge, J.; Scheijmans, J.C.G.; van Geloven, A.A.W.; Gans, S.L.; Boermeester, M.A.; Bemelman, W.A.; van Rossem, C.C.; on behalf of the SNAPSHOT. Daytime versus Nighttime in Acute Appendicitis. Diagnostics 2022, 12, 788. https://doi.org/10.3390/diagnostics12040788
Bom WJ, de Jonge J, Scheijmans JCG, van Geloven AAW, Gans SL, Boermeester MA, Bemelman WA, van Rossem CC, on behalf of the SNAPSHOT. Daytime versus Nighttime in Acute Appendicitis. Diagnostics. 2022; 12(4):788. https://doi.org/10.3390/diagnostics12040788
Chicago/Turabian StyleBom, Wouter J., Joske de Jonge, Jochem C. G. Scheijmans, Anna A. W. van Geloven, Sarah L. Gans, Marja A. Boermeester, Willem A. Bemelman, Charles C. van Rossem, and on behalf of the SNAPSHOT. 2022. "Daytime versus Nighttime in Acute Appendicitis" Diagnostics 12, no. 4: 788. https://doi.org/10.3390/diagnostics12040788
APA StyleBom, W. J., de Jonge, J., Scheijmans, J. C. G., van Geloven, A. A. W., Gans, S. L., Boermeester, M. A., Bemelman, W. A., van Rossem, C. C., & on behalf of the SNAPSHOT. (2022). Daytime versus Nighttime in Acute Appendicitis. Diagnostics, 12(4), 788. https://doi.org/10.3390/diagnostics12040788





