Abstract
Twin pregnancy contributes to perinatal mortality, particularly monochorionic diamniotic twin pregnancy. Placental abnormalities are much more common in twin pregnancies than in singletons. In MCDA pregnancy, vascular anastomoses are always present and are accountable for severe complications such as Twin-to-Twin transfusion syndrome (TTTS). In TTTS, umbilical cords are usually inserted at a distance from each other. We present a rare type of MCDA pregnancy, TTTS gr 1 case with bordering umbilical cord insertions.
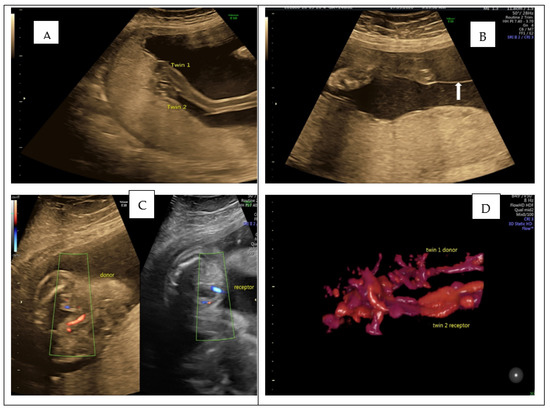
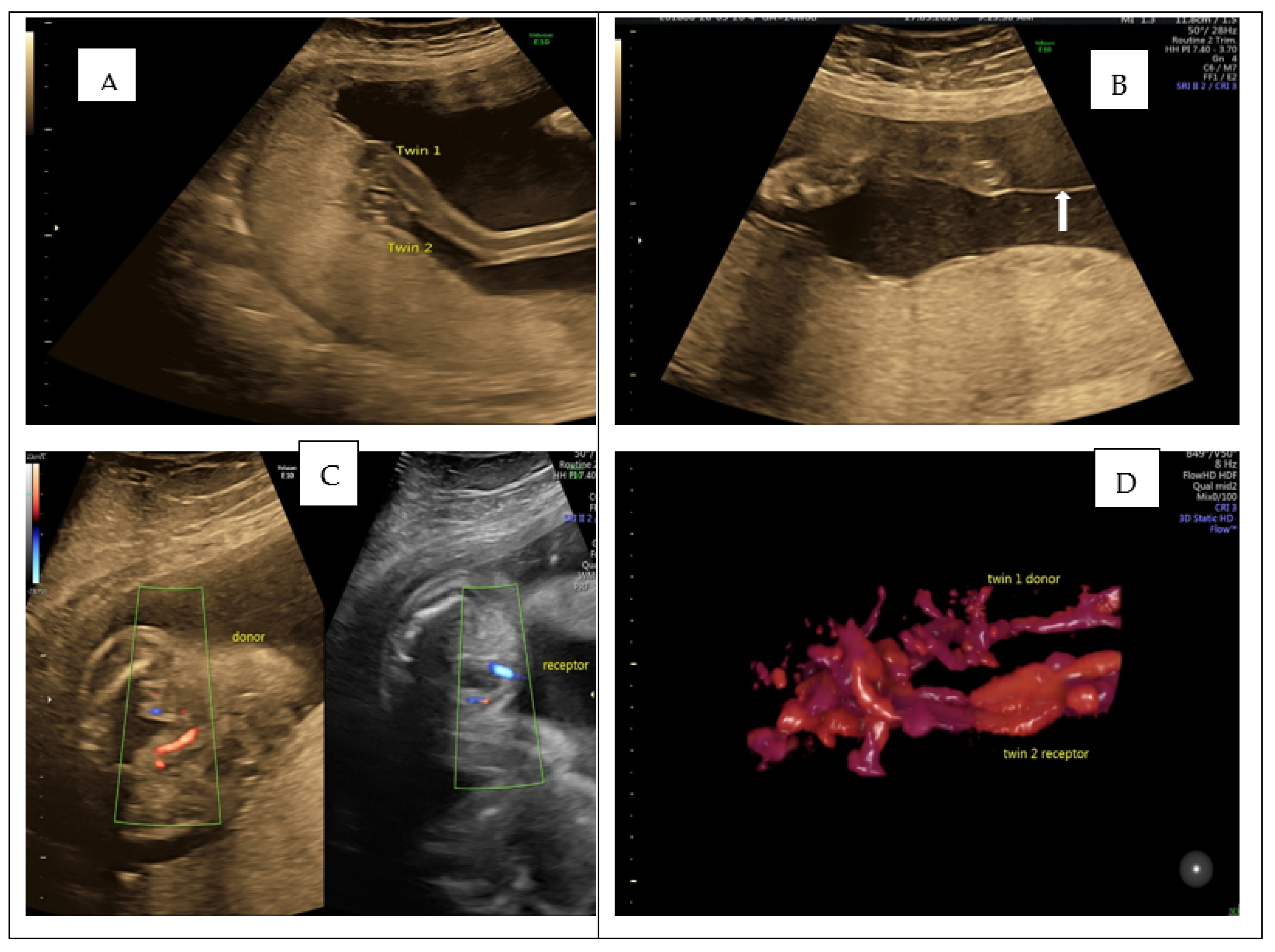
Figure 1.
We present the case of a 33-year-old lady, 24 weeks G1P0, referred to our hospital, having been diagnosed with MCDA twin pregnancy and TTTS grade. A viable MCDA pregnancy with TTTS grade 1 was confirmed. Placental cord insertions were extremely close, almost touching one another (A). (B) White arrow shows a thin amniotic membrane, with bladder visible in both twins in (C). A 3D Power Doppler Rendering image, depicting both twins’ close umbilical cord insertion, is shown in (D). Captured using Convex Probe 2D-4DRAB6D Voluson E10BT16 (GE Zipfer, Austria). According to ISUOG guidelines, conservative management and laser treatment are sensible options for TTTS gr 1 [1]. We decided to proceed with conservative management, considering cord insertions location, as laser surgery could lead to a catastrophic haemorrhage. The patient was counselled accordingly, and a follow-up plan was set up with a fortnightly assessment. At 33 weeks of gestation, she was admitted to the labour ward with PPROM (preterm prelabour rupture of membrane). She delivered through C section two male foetuses of 1.8 Kg and 2.1 Kg. The babies are now three years of age and thriving.
Figure 1.
We present the case of a 33-year-old lady, 24 weeks G1P0, referred to our hospital, having been diagnosed with MCDA twin pregnancy and TTTS grade. A viable MCDA pregnancy with TTTS grade 1 was confirmed. Placental cord insertions were extremely close, almost touching one another (A). (B) White arrow shows a thin amniotic membrane, with bladder visible in both twins in (C). A 3D Power Doppler Rendering image, depicting both twins’ close umbilical cord insertion, is shown in (D). Captured using Convex Probe 2D-4DRAB6D Voluson E10BT16 (GE Zipfer, Austria). According to ISUOG guidelines, conservative management and laser treatment are sensible options for TTTS gr 1 [1]. We decided to proceed with conservative management, considering cord insertions location, as laser surgery could lead to a catastrophic haemorrhage. The patient was counselled accordingly, and a follow-up plan was set up with a fortnightly assessment. At 33 weeks of gestation, she was admitted to the labour ward with PPROM (preterm prelabour rupture of membrane). She delivered through C section two male foetuses of 1.8 Kg and 2.1 Kg. The babies are now three years of age and thriving.
Author Contributions
Conceptualization: L.G.P. and V.R.; writing: M.P. and N.B.; supervision O.D.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board nr 64/3 March 2022.
Informed Consent Statement
Informed consent was obtained from the mother.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Reference
- Khalil, A.; Rodgers, M.; Baschat, A.; Bhide, A.; Gratacos, E.; Hecher, K.; Kilby, M.D.; Lewi, L.; Nicolaides, K.H.; Oepkes, D.; et al. ISUOG Practice Guidelines: Role of ultrasound in twin pregnancy. Ultrasound Obstet. Gynecol. 2016, 47, 247–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
