Detection of Chronic Blast-Related Mild Traumatic Brain Injury with Diffusion Tensor Imaging and Support Vector Machines
Abstract
:1. Introduction
2. Methods
2.1. Participants and Assessments
2.2. Imaging Protocols
2.3. DTI Analyses
2.4. SVM Analyses with Cross Validation
2.5. Correlations between SVM Model Features and Behavioral Variables
3. Results
3.1. Neuropsychological Test Performance
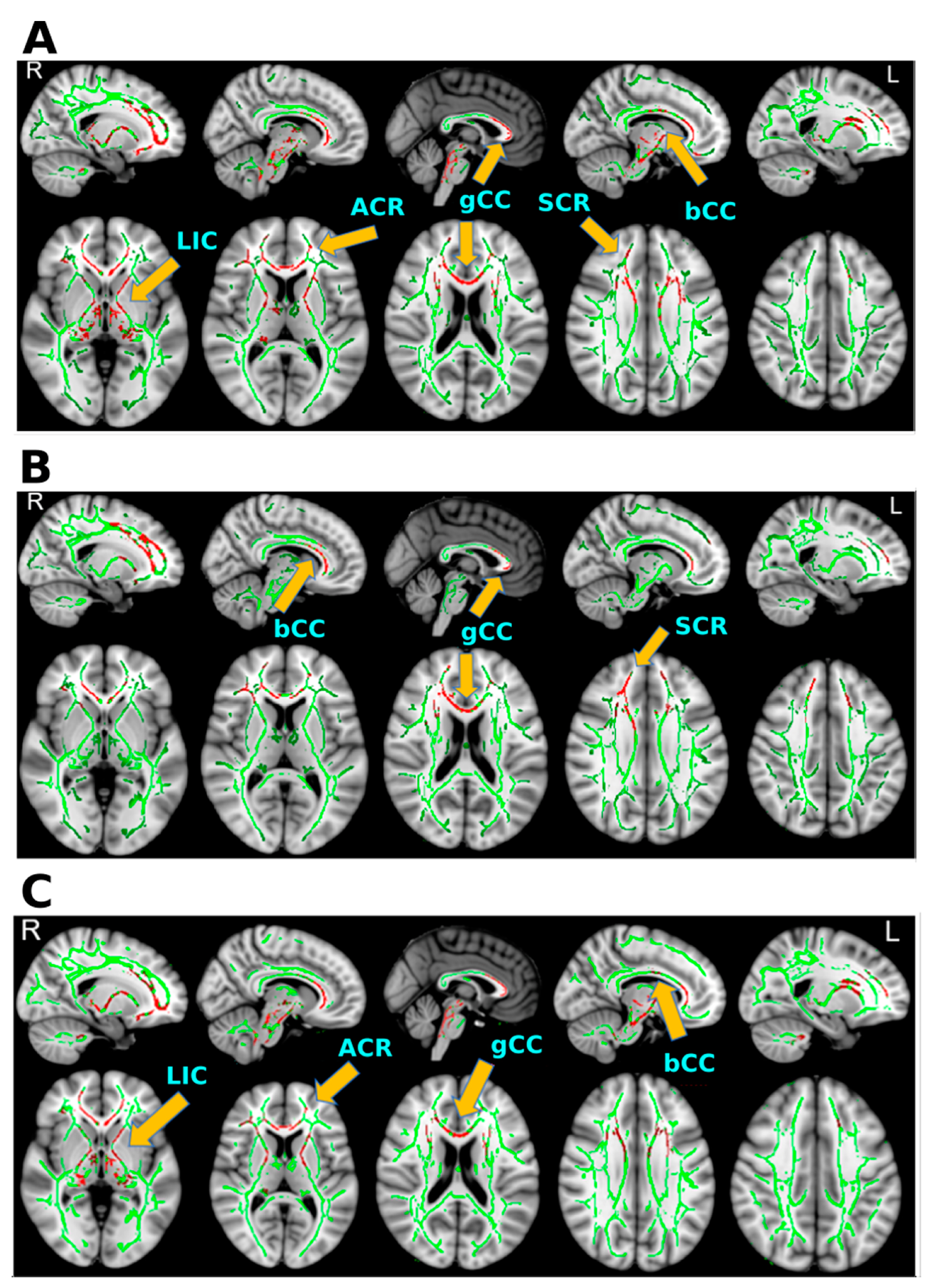
3.2. TBSS Results
3.3. SVM with Cross-Validation Results
3.4. Correlations between the SVM Features and Behavioral Variables
4. Discussion
4.1. Abnormal Diffusivity in bmTBI
4.2. Optimal Features of bmTBI
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Langlois, J.A.; Rutland-Brown, W.; Wald, M.M. The epidemiology and impact of traumatic brain injury: A brief overview. J. Head Trauma Rehabil. 2006, 21, 375–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roozenbeek, B.; Maas, A.I.; Menon, D.K. Changing patterns in the epidemiology of traumatic brain injury. Nat. Rev. Neurol. 2013, 9, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Rubiano, A.M.; Carney, N.; Chesnut, R.; Puyana, J.C. Global neurotrauma research challenges and opportunities. Nature 2015, 527, S193–S197. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.L.; Bangen, K.J.; Sorg, S.F.; Schiehser, D.M.; Evangelista, N.D.; McKenna, B.; Liu, T.T.; Delano-Wood, L. Dynamic association between perfusion and white matter integrity across time since injury in Veterans with history of TBI. Neuroimage Clin. 2017, 14, 308–315. [Google Scholar] [CrossRef]
- Hoge, C.W.; McGurk, D.; Thomas, J.L.; Cox, A.L.; Engel, C.C.; Castro, C.A. Mild traumatic brain injury in US soldiers returning from Iraq. N. Engl. J. Med. 2008, 358, 453–463. [Google Scholar] [CrossRef]
- Porter, K.E.; Stein, M.B.; Martis, B.; Avallone, K.M.; McSweeney, L.B.; Smith, E.R.; Simon, N.M.; Gargan, S.; Liberzon, I.; Hoge, C.W.; et al. Postconcussive symptoms (PCS) following combat-related traumatic brain injury (TBI) in Veterans with posttraumatic stress disorder (PTSD): Influence of TBI, PTSD, and depression on symptoms measured by the Neurobehavioral Symptom Inventory (NSI). J. Psychiatr. Res. 2018, 102, 8–13. [Google Scholar] [CrossRef]
- Turner, P.R. TBI in military and veterans: Incidence, symptoms, and resources. In Proceedings of the North Star Holistic Health Conference, Penrith, UK, 22–23 April 2015. [Google Scholar]
- Bigler, E.D.; Bazarian, J.J. Diffusion tensor imaging: A biomarker for mild traumatic brain injury? Neurology 2010, 74, 626–627. [Google Scholar] [CrossRef] [Green Version]
- DePalma, R.G.; Hoffman, S.W. Combat blast related traumatic brain injury (TBI): Decade of recognition promise of progress. Behav. Brain Res. 2018, 340, 102–105. [Google Scholar] [CrossRef]
- Gardner, R.C.; Yaffe, K. Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol. Cell. Neurosci. 2015, 66, 75–80. [Google Scholar] [CrossRef] [Green Version]
- Bigler, E.D. Structural neuroimaging in sport-related concussion. Int. J. Psychophysiol. 2018, 132, 105–123. [Google Scholar] [CrossRef]
- Bigler, E.D.; Orrison, W.W. Neuroimaging in sports-related brain injury. In Traumatic Brain Injury in Sports; Taylor & Francis: Abingdon, UK, 2020; pp. 71–93. [Google Scholar]
- Johnston, K.M.; Ptito, A.; Chankowsky, J.; Chen, J.K. New frontiers in diagnostic imaging in concussive head injury. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2001, 11, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, M.W.; Yeates, K.O.; Wilson, P.E. Pediatric sport-related concussion: A review of the clinical management of an oft-neglected population. Pediatrics 2006, 117, 1359–1371. [Google Scholar] [CrossRef] [PubMed]
- Douglas, D.B.; Iv, M.; Douglas, P.K.; Anderson, A.; Vos, S.B.; Bammer, R.; Zeineh, M.; Wintermark, M. Diffusion Tensor Imaging of TBI: Potentials and Challenges. Top. Magn. Reson. Imaging 2015, 24, 241–251. [Google Scholar] [CrossRef]
- Niogi, S.N.; Mukherjee, P. Diffusion tensor imaging of mild traumatic brain injury. J. Head Trauma Rehabil. 2010, 25, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Shenton, M.E.; Hamoda, H.M.; Schneiderman, J.S.; Bouix, S.; Pasternak, O.; Rathi, Y.; Vu, M.-A.; Purohit, M.P.; Helmer, K.; Koerte, I.; et al. A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav. 2012, 6, 137–192. [Google Scholar] [CrossRef]
- Wallace, E.J.; Mathias, J.L.; Ward, L. Diffusion tensor imaging changes following mild, moderate and severe adult traumatic brain injury: A meta-analysis. Brain Imaging Behav. 2018, 12, 1607–1621. [Google Scholar] [CrossRef]
- Geschwind, N. Disconnexion syndromes in animals and man. Sel. Pap. Lang. Brain 1974, 105–236. [Google Scholar]
- Peerless, S.J.; Rewcastle, N.B. Shear injuries of the brain. Can. Med. Assoc. J. 1967, 96, 577. [Google Scholar] [PubMed]
- Strich, S.J. Diffuse degeneration of the cerebral white matter in severe dementia following head injury. J. Neurol. Neurosurg. Psychiatry 1956, 19, 163. [Google Scholar] [CrossRef] [Green Version]
- Christopher Fox, W.; Park, M.S.; Belverud, S.; Klugh, A.; Rivet, D.; Tomlin, J.M. Contemporary imaging of mild TBI: The journey toward diffusion tensor imaging to assess neuronal damage. Neurol. Res. 2013, 35, 223–232. [Google Scholar] [CrossRef]
- Xiong, K.; Zhu, Y.; Zhang, W. Diffusion tensor imaging and magnetic resonance spectroscopy in traumatic brain injury: A review of recent literature. Brain Imaging Behav. 2014, 8, 487–496. [Google Scholar] [CrossRef] [PubMed]
- Hayes, J.P.; Bigler, E.D.; Verfaellie, M. Traumatic brain injury as a disorder of brain connectivity. J. Int. Neuropsychol. Soc. 2016, 22, 120–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharp, D.J.; Scott, G.; Leech, R. Network dysfunction after traumatic brain injury. Nat. Rev. Neurol. 2014, 10, 156–166. [Google Scholar] [CrossRef]
- Jellison, B.J.; Field, A.S.; Medow, J.; Lazar, M.; Salamat, M.S.; Alexander, A.L. Diffusion tensor imaging of cerebral white matter: A pictorial review of physics, fiber tract anatomy, and tumor imaging patterns. Am. J. Neuroradiol. 2004, 25, 356–369. [Google Scholar] [PubMed]
- Marrale, M.; Collura, G.; Brai, M.; Toschi, N.; Midiri, F.; La Tona, G.; Casto, A.L.; Gagliardo, C. Physics, techniques and review of neuroradiological applications of diffusion kurtosis imaging (DKI). Clin. Neuroradiol. 2016, 26, 391–403. [Google Scholar] [CrossRef] [PubMed]
- Asken, B.M.; DeKosky, S.T.; Clugston, J.R.; Jaffee, M.S.; Bauer, R.M. Diffusion tensor imaging (DTI) findings in adult civilian, military, and sport-related mild traumatic brain injury (mTBI): A systematic critical review. Brain Imaging Behav. 2018, 12, 585–612. [Google Scholar] [CrossRef] [PubMed]
- Davenport, N.D.; Lim, K.O.; Armstrong, M.T.; Sponheim, S.R. Diffuse and spatially variable white matter disruptions are associated with blast-related mild traumatic brain injury. NeuroImage 2012, 59, 2017–2024. [Google Scholar] [CrossRef]
- Li, L.; Sun, G.; Liu, K.; Li, M.; Li, B.; Qian, S.-W.; Yu, L.-L. White matter changes in posttraumatic stress disorder following mild traumatic brain injury: A prospective longitudinal diffusion tensor imaging study. Chin. Med. J. 2016, 129, 1091. [Google Scholar] [CrossRef]
- Mac Donald, C.L.; Johnson, A.M.; Cooper, D.; Nelson, E.C.; Werner, N.J.; Shimony, J.S.; Snyder, A.Z.; Raichle, M.E.; Witherow, J.R.; Fang, R.; et al. Detection of blast-related traumatic brain injury in U.S. military personnel. N. Engl. J. Med. 2011, 364, 2091–2100. [Google Scholar] [CrossRef] [Green Version]
- Costanzo, M.E.; Chou, Y.-Y.; Leaman, S.; Pham, D.L.; Keyser, D.; Nathan, D.E.; Coughlin, M.; Rapp, P.; Roy, M.J. Connecting combat-related mild traumatic brain injury with posttraumatic stress disorder symptoms through brain imaging. Neurosci. Lett. 2014, 577, 11–15. [Google Scholar] [CrossRef]
- Warden, D.L.; French, L.M.; Shupenko, L.; Fargus, J.; Riedy, G.; Erickson, M.E.; Jaffee, M.S.; Moore, D.F. Case report of a soldier with primary blast brain injury. Neuroimage 2009, 47, T152–T153. [Google Scholar] [CrossRef] [PubMed]
- Davenport, N.D.; Lim, K.O.; Sponheim, S.R. White matter abnormalities associated with military PTSD in the context of blast TBI. Hum. Brain Mapp. 2015, 36, 1053–1064. [Google Scholar] [CrossRef] [PubMed]
- Holtkamp, M.D.; Grimes, J.; Ling, G. Concussion in the military: An evidence-base review of mTBI in US military personnel focused on posttraumatic headache. Curr. Pain Headache Rep. 2016, 20, 37. [Google Scholar] [CrossRef] [PubMed]
- Isaac, L.; Main, K.L.; Soman, S.; Gotlib, I.H.; Furst, A.J.; Kinoshita, L.M.; Fairchild, J.K.; Yesavage, J.A.; Ashford, J.W.; Bayley, P.J. The impact of depression on Veterans with PTSD and traumatic brain injury: A diffusion tensor imaging study. Biol. Psychol. 2015, 105, 20–28. [Google Scholar] [CrossRef]
- Hayes, J.P.; Miller, D.R.; Lafleche, G.; Salat, D.H.; Verfaellie, M. The nature of white matter abnormalities in blast-related mild traumatic brain injury. Neuroimage Clin. 2015, 8, 148–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matthews, S.C.; Strigo, I.A.; Simmons, A.N.; O’Connell, R.M.; Reinhardt, L.E.; Moseley, S.A. A multimodal imaging study in US veterans of Operations Iraqi and Enduring Freedom with and without major depression after blast-related concussion. Neuroimage 2011, 54, S69–S75. [Google Scholar] [CrossRef]
- Jorge, R.E.; Acion, L.; White, T.; Tordesillas-Gutierrez, D.; Pierson, R.; Crespo-Facorro, B.; Magnotta, V.A. White matter abnormalities in veterans with mild traumatic brain injury. Am. J. Psychiatry 2012, 169, 1284–1291. [Google Scholar] [CrossRef] [Green Version]
- Miller, D.R.; Hayes, J.P.; Lafleche, G.; Salat, D.H.; Verfaellie, M. White matter abnormalities are associated with chronic postconcussion symptoms in blast-related mild traumatic brain injury. Hum. Brain Mapp. 2016, 37, 220–229. [Google Scholar] [CrossRef] [Green Version]
- Budde, M.D.; Kim, J.H.; Liang, H.-F.; Schmidt, R.E.; Russell, J.H.; Cross, A.H.; Song, S.-K. Toward accurate diagnosis of white matter pathology using diffusion tensor imaging. Magn. Reson. Med. 2007, 57, 688–695. [Google Scholar] [CrossRef]
- Hoogenboom, W.S.; Rubin, T.G.; Ye, K.; Cui, M.-H.; Branch, K.C.; Liu, J.; Branch, C.A.; Lipton, M.L. Diffusion Tensor Imaging of the Evolving Response to Mild Traumatic Brain Injury in Rats. J. Exp. Neurosci. 2019, 13, 1179069519858627. [Google Scholar] [CrossRef]
- Niogi, S.N.; Mukherjee, P.; Ghajar, J.; Johnson, C.; Kolster, R.A.; Sarkar, R.; Lee, H.; Meeker, M.; Zimmerman, R.D.; Manley, G.T. Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: A 3T diffusion tensor imaging study of mild traumatic brain injury. Am. J. Neuroradiol. 2008, 29, 967–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kou, Z.; Wu, Z.; Tong, K.A.; Holshouser, B.; Benson, R.R.; Hu, J.; Haacke, E.M. The role of advanced MR imaging findings as biomarkers of traumatic brain injury. J. Head Trauma Rehabil. 2010, 25, 267–282. [Google Scholar] [CrossRef] [PubMed]
- Jeter, C.B.; Hergenroeder, G.W.; Hylin, M.J.; Redell, J.B.; Moore, A.N.; Dash, P.K. Biomarkers for the diagnosis and prognosis of mild traumatic brain injury/concussion. J. Neurotrauma 2013, 30, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Zetterberg, H.; Smith, D.H.; Blennow, K. Biomarkers of mild traumatic brain injury in cerebrospinal fluid and blood. Nat. Rev. Neurol. 2013, 9, 201–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burges, C.J. A tutorial on support vector machines for pattern recognition. Data Min. Knowl. Discov. 1998, 2, 121–167. [Google Scholar] [CrossRef]
- Vergara, V.M.; Mayer, A.R.; Damaraju, E.; Kiehl, K.A.; Calhoun, V. Detection of Mild Traumatic Brain Injury by Machine Learning Classification Using Resting State Functional Network Connectivity and Fractional Anisotropy. J. Neurotrauma 2017, 34, 1045–1053. [Google Scholar] [CrossRef] [Green Version]
- Watts, R.; Thomas, A.; Filippi, C.G.; Nickerson, J.P.; Freeman, K. Potholes and molehills: Bias in the diagnostic performance of diffusion-tensor imaging in concussion. Radiology 2014, 272, 217–223. [Google Scholar] [CrossRef] [Green Version]
- Ling, J.M.; Pena, A.; Yeo, R.A.; Merideth, F.L.; Klimaj, S.; Gasparovic, C.; Mayer, A.R. Biomarkers of increased diffusion anisotropy in semi-acute mild traumatic brain injury: A longitudinal perspective. Brain 2012, 135, 1281–1292. [Google Scholar] [CrossRef]
- Ball, T.M.; Squeglia, L.M.; Tapert, S.F.; Paulus, M.P. Double Dipping in Machine Learning: Problems and Solutions. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2020, 5, 261–263. [Google Scholar] [CrossRef]
- Statements, Q. VA/DoD clinical practice guideline for management of concussion/mild traumatic brain injury. J. Rehabil. Res. Dev. 2009, 46, 1–60. [Google Scholar]
- Teasdale, G.; Jennett, B. Assessment of coma and impaired consciousness: A practical scale. Lancet 1974, 304, 81–84. [Google Scholar] [CrossRef]
- Alvin, M., Jr.; Sureyya, D.; Allen, R.W.; James, L.G. Psychosocial functioning at 1 month after head injury. Neurosurgery 1984, 14, 393–399. [Google Scholar] [CrossRef]
- Delis, D.C.; Kaplan, E.; Kramer, J.H. Delis-Kaplan Executive Function System; The Psychological Corporation: San Antonio, TX, USA, 2001. [Google Scholar]
- Wechsler, D. WAIS-III Wechsler Adult Intelligence Scale; The Psychological Corporation: San Antonio, TX, USA, 1997; Volume 3. [Google Scholar]
- Robb Swan, A.; Nichols, S.; Drake, A.; Angeles, A.; Diwakar, M.; Song, T.; Lee, R.R.; Huang, M.-X. Magnetoencephalography Slow-Wave Detection in Patients with Mild Traumatic Brain Injury and Ongoing Symptoms Correlated with Long-Term Neuropsychological Outcome. J. Neurotrauma 2015, 32, 1510–1521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Behrens, T.E.; Woolrich, M.W.; Jenkinson, M.; Johansen-Berg, H.; Nunes, R.G.; Clare, S.; Matthews, P.M.; Brady, J.M.; Smith, S.M. Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magn. Reson. Med. 2003, 50, 1077–1088. [Google Scholar] [CrossRef] [PubMed]
- Hasan, K.M.; Narayana, P.A. Retrospective measurement of the diffusion tensor eigenvalues from diffusion anisotropy and mean diffusivity in DTI. Magn. Reson. Med. 2006, 56, 130–137. [Google Scholar] [CrossRef]
- Qin, Y.; Li, G.-L.; Xu, X.-H.; Sun, Z.-Y.; Gu, J.-W.; Gao, F.-B. Brain structure alterations and cognitive impairment following repetitive mild head impact: An in vivo MRI and behavioral study in rat. Behav. Brain Res. 2018, 340, 41–48. [Google Scholar] [CrossRef]
- Raikes, A.C.; Bajaj, S.; Dailey, N.S.; Smith, R.S.; Alkozei, A.; Satterfield, B.C.; Killgore, W.D.S. Diffusion Tensor Imaging (DTI) Correlates of Self-Reported Sleep Quality and Depression Following Mild Traumatic Brain Injury. Front. Neurol. 2018, 9, 468. [Google Scholar] [CrossRef]
- Khong, E.; Odenwald, N.; Hashim, E.; Cusimano, M.D. Diffusion Tensor Imaging Findings in Post-Concussion Syndrome Patients after Mild Traumatic Brain Injury: A Systematic Review. Front. Neurol. 2016, 7, 156. [Google Scholar] [CrossRef] [Green Version]
- Smith, S.M.; Jenkinson, M.; Johansen-Berg, H.; Rueckert, D.; Nichols, T.E.; Mackay, C.E.; Watkins, K.E.; Ciccarelli, O.; Cader, M.Z.; Matthews, P.M. Tract-based spatial statistics: Voxelwise analysis of multi-subject diffusion data. Neuroimage 2006, 31, 1487–1505. [Google Scholar] [CrossRef]
- Smith, S.M.; Nichols, T.E. Threshold-free cluster enhancement: Addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 2009, 44, 83–98. [Google Scholar] [CrossRef] [Green Version]
- Hua, K.; Zhang, J.; Wakana, S.; Jiang, H.; Li, X.; Reich, D.S.; Calabresi, P.A.; Pekar, J.J.; van Zijl, P.C.; Mori, S. Tract probability maps in stereotaxic spaces: Analyses of white matter anatomy and tract-specific quantification. Neuroimage 2008, 39, 336–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, D.; Wu, G.; Suk, H.-I. Deep learning in medical image analysis. Annu. Rev. Biomed. Eng. 2017, 19, 221–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breiman, L. Statistical modeling: The two cultures. Qual. Control. Appl. Stat. 2003, 48, 81–82. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Miller, D.R.; Hayes, J.P.; Lafleche, G.; Salat, D.H.; Verfaellie, M. White matter abnormalities are associated with overall cognitive status in blast-related mTBI. Brain Imaging Behav. 2017, 11, 1129–1138. [Google Scholar] [CrossRef]
- Browne, K.D.; Chen, X.-H.; Meaney, D.F.; Smith, D.H. Mild traumatic brain injury and diffuse axonal injury in swine. J. Neurotrauma 2011, 28, 1747–1755. [Google Scholar] [CrossRef] [Green Version]
- Povlishock, J.T.; Katz, D.I. Update of neuropathology and neurological recovery after traumatic brain injury. J. Head Trauma Rehabil. 2005, 20, 76–94. [Google Scholar] [CrossRef] [Green Version]
- Rosenblum, W.I. Cytotoxic edema: Monitoring its magnitude and contribution to brain swelling. J. Neuropathol. Exp. Neurol. 2007, 66, 771–778. [Google Scholar] [CrossRef] [Green Version]
- Chu, Z.; Wilde, E.A.; Hunter, J.V.; McCauley, S.R.; Bigler, E.D.; Troyanskaya, M.; Yallampalli, R.; Chia, J.M.; Levin, H.S. Voxel-based analysis of diffusion tensor imaging in mild traumatic brain injury in adolescents. Am. J. Neuroradiol. 2010, 31, 340–346. [Google Scholar] [CrossRef] [Green Version]
- Wilde, E.A.; Hunter, J.V.; Bigler, E.D. Neuroimaging in neurorehabilitation. NeuroRehabilitation 2012, 31, 223–226. [Google Scholar] [CrossRef]
- Henry, L.C.; Tremblay, J.; Tremblay, S.; Lee, A.; Brun, C.; Lepore, N.; Theoret, H.; Ellemberg, D.; Lassonde, M. Acute and chronic changes in diffusivity measures after sports concussion. J. Neurotrauma 2011, 28, 2049–2059. [Google Scholar] [CrossRef] [PubMed]
- Rubovitch, V.; Ten-Bosch, M.; Zohar, O.; Harrison, C.R.; Tempel-Brami, C.; Stein, E.; Hoffer, B.J.; Balaban, C.D.; Schreiber, S.; Chiu, W.-T. A mouse model of blast-induced mild traumatic brain injury. Exp. Neurol. 2011, 232, 280–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morey, R.A.; Haswell, C.C.; Selgrade, E.S.; Massoglia, D.; Liu, C.; Weiner, J.; Marx, C.E.; MIRECC Work Group; Cernak, I.; McCarthy, G. Effects of chronic mild traumatic brain injury on white matter integrity in Iraq and Afghanistan war veterans. Hum. Brain Mapp. 2013, 34, 2986–2999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petrie, E.C.; Cross, D.J.; Yarnykh, V.L.; Richards, T.; Martin, N.M.; Pagulayan, K.; Hoff, D.; Hart, K.; Mayer, C.; Tarabochia, M.; et al. Neuroimaging, behavioral, and psychological sequelae of repetitive combined blast/impact mild traumatic brain injury in Iraq and Afghanistan war veterans. J. Neurotrauma 2014, 31, 425–436. [Google Scholar] [CrossRef] [Green Version]
- Taber, K.H.; Hurley, R.A.; Haswell, C.C.; Rowland, J.A.; Hurt, S.D.; Lamar, C.D.; Morey, R.A. White matter compromise in veterans exposed to primary blast forces. J. Head Trauma Rehabil. 2015, 30, E15. [Google Scholar] [CrossRef]
- Johnson, V.E.; Stewart, W.; Smith, D.H. Axonal pathology in traumatic brain injury. Exp. Neurol. 2013, 246, 35–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Council, N.R. Linking Helmet Protection to Brain Injury. In Review of Department of Defense Test Protocols for Combat Helmets; National Academies Press (US): Washington, DC, USA, 2014. [Google Scholar]
- Hulkower, M.B.; Poliak, D.B.; Rosenbaum, S.B.; Zimmerman, M.E.; Lipton, M.L. A decade of DTI in traumatic brain injury: 10 years and 100 articles later. Am. J. Neuroradiol. 2013, 34, 2064–2074. [Google Scholar] [CrossRef] [Green Version]
- Taylor, P.A.; Ford, C.C. Simulation of blast-induced early-time intracranial wave physics leading to traumatic brain injury. J. Biomech. Eng. 2009, 131, 061007. [Google Scholar] [CrossRef]
- Zappala, G.; de Schotten, M.T.; Eslinger, P.J. Traumatic brain injury and the frontal lobes: What can we gain with diffusion tensor imaging? Cortex 2012, 48, 156–165. [Google Scholar] [CrossRef]
- Aoki, Y.; Inokuchi, R.; Gunshin, M.; Yahagi, N.; Suwa, H. Diffusion tensor imaging studies of mild traumatic brain injury: A meta-analysis. J. Neurol. Neurosurg. Psychiatry 2012, 83, 870–876. [Google Scholar] [CrossRef] [Green Version]
- Gennarelli, T.A.; Thibault, L.E.; Adams, J.H.; Graham, D.I.; Thompson, C.J.; Marcincin, R.P. Diffuse axonal injury and traumatic coma in the primate. Ann. Neurol 1982, 12, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Gentry, L.R.; Thompson, B.; Godersky, J.C. Trauma to the corpus callosum: MR features. Am. J. Neuroradiol. 1988, 9, 1129–1138. [Google Scholar] [PubMed]
- Arfanakis, K.; Haughton, V.M.; Carew, J.D.; Rogers, B.P.; Dempsey, R.J.; Meyerand, M.E. Diffusion tensor MR imaging in diffuse axonal injury. Am. J. Neuroradiol. 2002, 23, 794–802. [Google Scholar] [PubMed]
- Friedman, J.; Hastie, T.; Tibshirani, R. The Elements of Statistical Learning; Springer: New York, NY, USA, 2001. [Google Scholar]
- Liu, H.; Motoda, H. Computational Methods of Feature Selection; CRC Press: Boca Raton, FL, USA, 2007. [Google Scholar]
- Fani, N.; King, T.Z.; Jovanovic, T.; Glover, E.M.; Bradley, B.; Choi, K.; Ely, T.; Gutman, D.A.; Ressler, K.J. White Matter Integrity in Highly Traumatized Adults With and Without Post-Traumatic Stress Disorder. Neuropsychopharmacology 2012, 37, 2740–2746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Doherty, D.C.M.; Ryder, W.; Paquola, C.; Tickell, A.; Chan, C.; Hermens, D.F.; Bennett, M.R.; Lagopoulos, J. White matter integrity alterations in post-traumatic stress disorder. Hum. Brain Mapp. 2018, 39, 1327–1338. [Google Scholar] [CrossRef] [PubMed]
- Weis, C.N.; Belleau, E.L.; Pedersen, W.S.; Miskovich, T.A.; Larson, C.L. Structural Connectivity of the Posterior Cingulum Is Related to Reexperiencing Symptoms in Posttraumatic Stress Disorder. Chronic Stress Thousand Oaks Calif 2018, 2, 2470547018807134. [Google Scholar] [CrossRef]
- Kaplan, G.B.; Leite-Morris, K.A.; Wang, L.; Rumbika, K.K.; Heinrichs, S.C.; Zeng, X.; Wu, L.; Arena, D.T.; Teng, Y.D. Pathophysiological Bases of Comorbidity: Traumatic Brain Injury and Post-Traumatic Stress Disorder. J. Neurotrauma 2018, 35, 210–225. [Google Scholar] [CrossRef]
- Huang, M.-X.; Swan, A.R.; Quinto, A.A.; Matthews, S.; Harrington, D.L.; Nichols, S.; Bruder, B.J.; Snook, C.C.; Huang, C.W.; Baker, D.G.; et al. A pilot treatment study for mild traumatic brain injury: Neuroimaging changes detected by MEG after low-intensity pulse-based transcranial electrical stimulation. Brain Inj. 2017, 31, 1951–1963. [Google Scholar] [CrossRef]
- Lee, S.A.; Kim, M.-K. Effect of Low Frequency Repetitive Transcranial Magnetic Stimulation on Depression and Cognition of Patients with Traumatic Brain Injury: A Randomized Controlled Trial. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2018, 24, 8789–8794. [Google Scholar] [CrossRef]
- Leung, A.; Shukla, S.; Fallah, A.; Song, D.; Lin, L.; Golshan, S.; Tsai, A.; Jak, A.; Polston, G.; Lee, R. Repetitive Transcranial Magnetic Stimulation in Managing Mild Traumatic Brain Injury-Related Headaches. Neuromodul. J. Int. Neuromodul. Soc. 2016, 19, 133–141. [Google Scholar] [CrossRef]
- Mollica, A.; Safavifar, F.; Fralick, M.; Giacobbe, P.; Lipsman, N.; Burke, M.J. Transcranial Magnetic Stimulation for the Treatment of Concussion: A Systematic Review. Neuromodul. J. Int. Neuromodul. Soc. 2021, 24, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Vaninetti, M.; Lim, M.; Khalaf, A.; Metzger-Smith, V.; Flowers, M.; Kunnel, A.; Yang, E.; Song, D.; Lin, L.; Tsai, A.; et al. fMRI findings in MTBI patients with headaches following rTMS. Sci. Rep. 2021, 11, 9573. [Google Scholar] [CrossRef] [PubMed]

| Control Group | bmTBI Group | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p-Value | Cohen’s d | |
| Age | 28.00 | 3.500 | 27.40 | 6.227 | 0.6453 | 0.1234 |
| Years of education | 12.58 | 0.769 | 13.05 | 2.059 | 0.2635 | −0.3324 |
| Months post-injury | 10.38 | 6.271 | ||||
| D-KEFS | ||||||
| Number-Letter Sequencing | 11.37 | 1.383 | 10.55 | 1.669 | 0.1049 | 0.5374 |
| Letter Fluency | 10.79 | 3.326 | 8.750 | 3.093 | 0.0547 ^ | 0.6356 |
| Category Fluency | 11.58 | 3.097 | 10.40 | 2.963 | 0.2321 | 0.3894 |
| Category Switching (total correct) | 11.79 | 2.974 | 9.800 | 3.002 | 0.0447 * | 0.6660 |
| Category Switching (total switching accuracy) | 12.05 | 2.368 | 10.75 | 2.100 | 0.0938 | 0.5819 |
| WAIS-III | ||||||
| Symbol Search | 10.79 | 3.794 | 10.55 | 2.417 | 0.8145 | 0.0773 |
| Digit Symbol Coding | 10.16 | 2.754 | 8.800 | 2.608 | 0.1222 | 0.5073 |
| Symptoms | bmTBI (%) | Control (%) | Symptoms | bmTBI (%) | Control (%) |
|---|---|---|---|---|---|
| Headaches | 90.0 | 5.26 | Lack of spontaneity | 0.00 | 0.00 |
| Dizziness | 70.0 | 5.26 | Affective lability | 10.0 | 5.26 |
| Fatigue | 50.0 | 10.5 | Depression | 20.0 | 5.26 |
| Memory difficulty | 85.0 | 15.8 | Concentration | 10.0 | 10.5 |
| Irritability | 60.0 | 15.8 | Bothered by noise | 0.00 | 0.00 |
| Anxiety | 55.0 | 0.00 | Bothered by light | 0.00 | 5.26 |
| Sleep problems | 60.0 | 5.26 | Coordination/balance | 15.0 | 10.5 |
| Hearing difficulties | 60.0 | 10.5 | Motor difficulty | 10.0 | 0.00 |
| Visual difficulties | 10.0 | 0.00 | Speech difficulty | 0.00 | 5.26 |
| Personality changes | 25.0 | 5.26 | Numbness/tingling | 20.0 | 0.00 |
| Apathy | 5.00 | 0.00 |
| Table | Group | FA | p Value | RD ± | p Value | AD/RD | p Value | Voxels |
|---|---|---|---|---|---|---|---|---|
| lACR | HC | 0.44 ± 0.024 | <0.001 | 0.54 ± 0.027 | 0.0098 | 2.04 ± 0.11 | <0.001 | |
| bmTBI | 0.47 ± 0.018 | 0.52 ± 0.021 | 2.15 ± 0.08 | 675 | ||||
| rACR | HC | 0.45 ± 0.029 | <0.001 | 0.56 ± 0.033 | <0.001 | 2.11 ± 0.13 | <0.001 | |
| bmTBI | 0.48 ± 0.024 | 0.53 ± 0.025 | 2.24 ± 0.13 | 1073 | ||||
| lALIC | HC | 0.54 ± 0.015 | <0.001 | 0.47 ± 0.018 | <0.001 | 2.63 ± 0.10 | <0.001 | 580 |
| bmTBI | 0.56 ± 0.013 | 0.45 ± 0.014 | 2.83 ± 0.10 | |||||
| rALIC | HC | 0.57 ± 0.020 | <0.001 | 0.45 ± 0.023 | 0.0026 | 2.80 ± 0.14 | <0.001 | 364 |
| bmTBI | 0.60 ± 0.019 | 0.43 ± 0.018 | 3.03 ± 0.16 | |||||
| lPLIC | HC | 0.62 ± 0.017 | <0.001 | 0.41 ± 0.016 | 0.0608 | 3.18 ± 0.14 | <0.001 | |
| bmTBI | 0.64 ± 0.019 | 0.40 ± 0.021 | 3.40 ± 0.23 | 1107 | ||||
| rPLIC | HC | 0.63 ± 0.017 | 0.0015 | 0.40 ± 0.017 | 0.0056 | 3.29 ± 0.17 | <0.001 | |
| bmTBI | 0.65 ± 0.020 | 0.38 ± 0.020 | 3.54 ± 0.26 | 1472 | ||||
| lSCR | HC | 0.45 ± 0.027 | <0.001 | 0.53 ± 0.023 | 0.0058 | 2.10 ± 0.13 | 0.0088 | |
| bmTBI | 0.48 ± 0.027 | 0.50 ± 0.022 | 2.23 ± 0.15 | 260 | ||||
| rSCR | HC | 0.45 ± 0.022 | 0.0026 | 0.53 ± 0.022 | 0.0215 | 2.15 ± 0.10 | 0.0067 | |
| bmTBI | 0.48 ± 0.026 | 0.51 ± 0.026 | 2.27 ± 0.14 | 247 | ||||
| gCC | HC | 0.64 ± 0.032 | 0.0014 | 0.46 ± 0.043 | 0.001 | 3.45 ± 0.32 | <0.001 | |
| bmTBI | 0.68 ± 0.024 | 0.42 ± 0.029 | 3.94 ± 0.35 | 222 | ||||
| bCC | HC | 0.66 ± 0.028 | <0.001 | 0.43 ± 0.042 | <0.001 | 4.08 ± 0.39 | 0.0031 | |
| bmTBI | 0.69 ± 0.020 | 0.39 ± 0.028 | 4.41 ± 0.32 | 170 |
| Model | Accuracy | Sensitivity | Specificity | Kernel | Features: Weightings (Mean ± Standard Deviation) |
|---|---|---|---|---|---|
| FA and AD/RD | 89% | 90% | 88% | Linear | Normalized AD/RD lALIC: (1.43 ± 0.16) AD/RD gCC: (0.84 ± 0.14) AD/RD rALIC: (0.77 ± 0.14) FA rACR: (−1.08 ± 0.15) FA lSCR: (0.69 ± 0.12) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harrington, D.L.; Hsu, P.-Y.; Theilmann, R.J.; Angeles-Quinto, A.; Robb-Swan, A.; Nichols, S.; Song, T.; Le, L.; Rimmele, C.; Matthews, S.; et al. Detection of Chronic Blast-Related Mild Traumatic Brain Injury with Diffusion Tensor Imaging and Support Vector Machines. Diagnostics 2022, 12, 987. https://doi.org/10.3390/diagnostics12040987
Harrington DL, Hsu P-Y, Theilmann RJ, Angeles-Quinto A, Robb-Swan A, Nichols S, Song T, Le L, Rimmele C, Matthews S, et al. Detection of Chronic Blast-Related Mild Traumatic Brain Injury with Diffusion Tensor Imaging and Support Vector Machines. Diagnostics. 2022; 12(4):987. https://doi.org/10.3390/diagnostics12040987
Chicago/Turabian StyleHarrington, Deborah L., Po-Ya Hsu, Rebecca J. Theilmann, Annemarie Angeles-Quinto, Ashley Robb-Swan, Sharon Nichols, Tao Song, Lu Le, Carl Rimmele, Scott Matthews, and et al. 2022. "Detection of Chronic Blast-Related Mild Traumatic Brain Injury with Diffusion Tensor Imaging and Support Vector Machines" Diagnostics 12, no. 4: 987. https://doi.org/10.3390/diagnostics12040987






