Low-Dose Abdominal CT for Evaluating Suspected Appendicitis: Recommendations for CT Imaging Techniques and Practical Issues
Abstract
1. Introduction
2. Technical Consideration
2.1. Intravenous Contrast Enhancement
2.2. Contrast-Enhancement Phase
2.3. Enteric Contrast
2.4. Anatomical Coverage
2.5. Tube Current
2.6. Tube Potential
2.7. Iterative Reconstruction
2.8. Image Reconstruction Thickness
2.9. Coronal Reformation
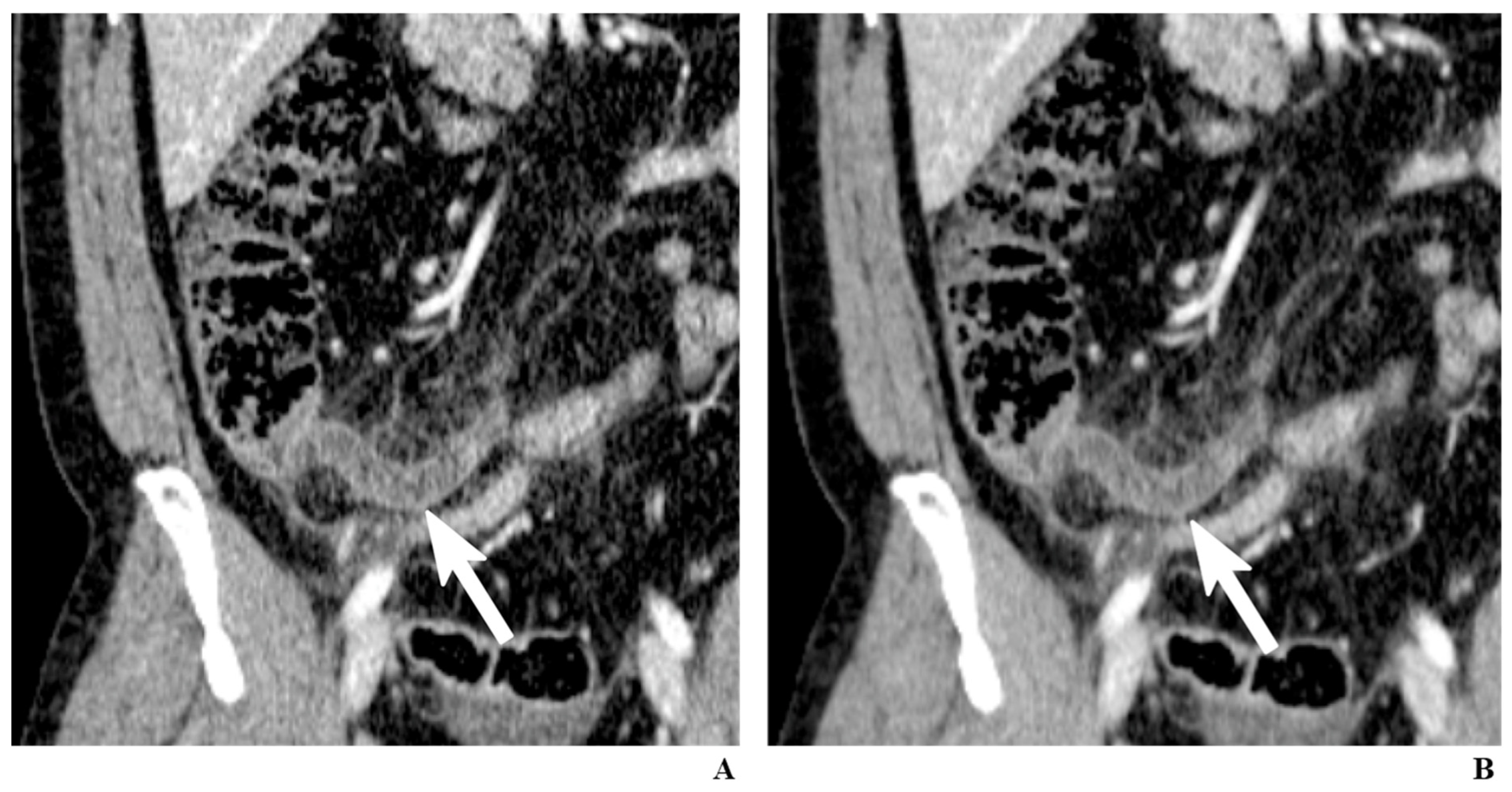
2.10. Sliding-Slab Averaging Technique
3. Other Practical Issues in Implementing LDCT
3.1. Dedicated Protocol for Appendiceal CT
3.2. Education for Referring Physicians and Surgeons
3.3. Education for Radiologists
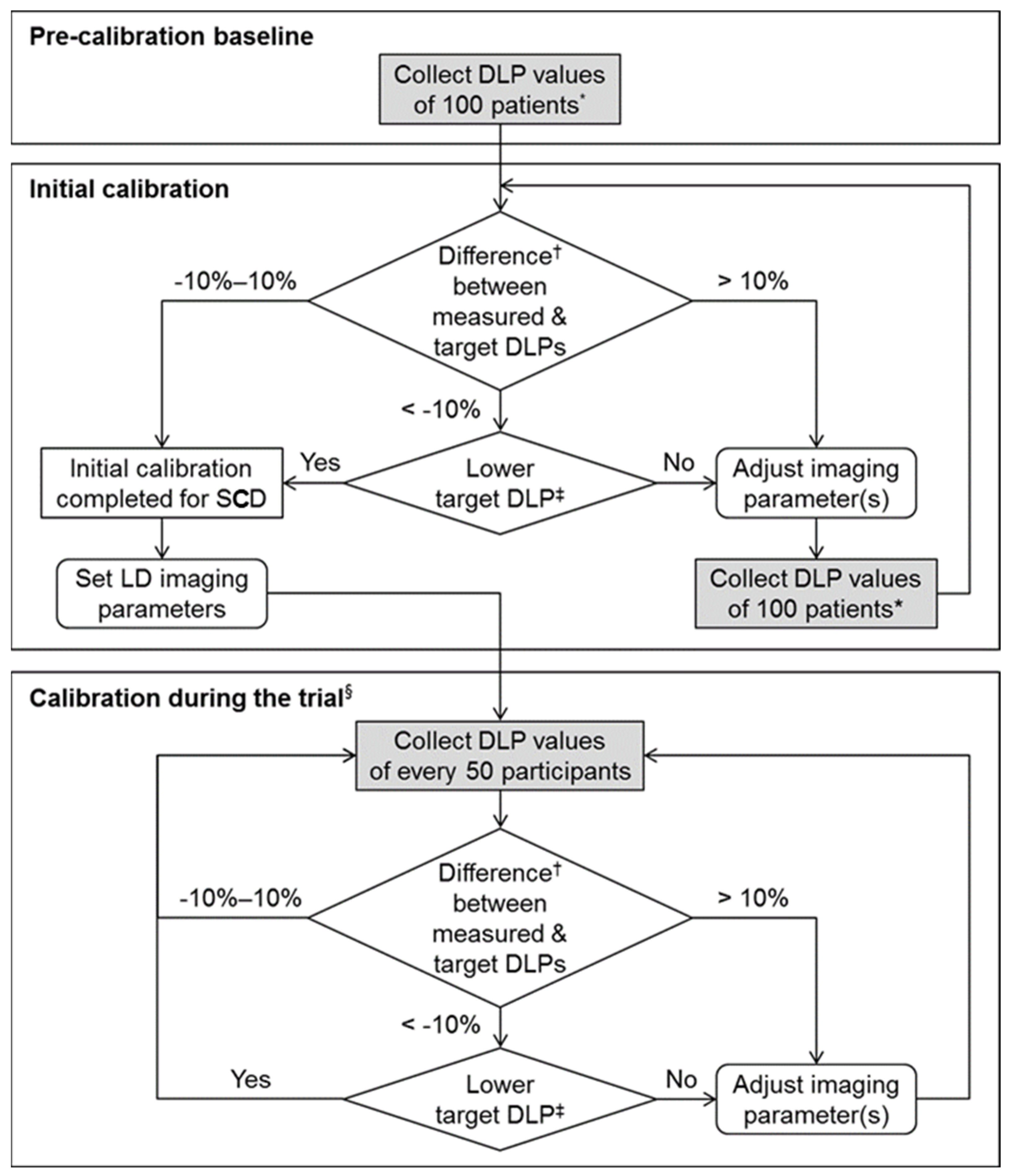
3.4. Dose Calibration and Monitoring
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, K.H.; Lee, S.; Park, J.H.; Lee, S.S.; Kim, H.Y.; Lee, W.J.; Cha, E.S.; Kim, K.P.; Lee, W.; Lee, J.Y.; et al. Risk of hematologic malignancies from abdominopelvic CT radiation in patients who underwent appendectomy: A nationwide population-based cohort study. JAMA Surg. 2021, 156, 343–351. [Google Scholar] [CrossRef]
- Park, J.H.; Salminen, P.; Tannaphai, P.; Lee, K.H. Low-dose abdominal CT for evaluating suspected appendicitis in adolescents and young adults: Review of evidence. Korean J. Radiol. 2022, 23, 517–528. [Google Scholar] [CrossRef]
- Kim, K.; Kim, Y.H.; Kim, S.Y.; Kim, S.; Lee, Y.J.; Kim, K.P.; Lee, H.S.; Ahn, S.; Kim, T.; Hwang, S.S.; et al. Low-dose abdominal CT for evaluating suspected appendicitis. N. Engl. J. Med. 2012, 366, 1596–1605. [Google Scholar] [CrossRef]
- LOCAT Group. Low-dose CT for the diagnosis of appendicitis in adolescents and young adults (LOCAT): A pragmatic, multicentre, randomised controlled non-inferiority trial. Lancet Gastroenterol. Hepatol. 2017, 2, 793–804. [Google Scholar] [CrossRef]
- Kim, H.J.; Lee, K.H.; Kim, M.J.; Park, S.B.; Ko, Y. Using 2-mSv appendiceal CT in usual practice for adolescents and young adults: Willingness survey of 579 radiologists, emergency physicians, and surgeons from 20 hospitals. Korean J. Radiol. 2020, 21, 68–76. [Google Scholar] [CrossRef]
- Garcia, E.M.; Camacho, M.A.; Karolyi, D.R.; Kim, D.H.; Cash, B.D.; Chang, K.J.; Feig, B.W.; Fowler, K.J.; Kambadakone, A.R.; Lambert, D.L.; et al. ACR Appropriateness Criteria® right lower quadrant pain-suspected appendicitis. J. Am. Coll. Radiol. JACR 2018, 15, S373–S387. [Google Scholar] [CrossRef]
- Keyzer, C.; Tack, D.; de Maertelaer, V.; Bohy, P.; Gevenois, P.A.; Van Gansbeke, D. Acute appendicitis: Comparison of low-dose and standard-dose unenhanced multi-detector row CT. Radiology 2004, 232, 164–172. [Google Scholar] [CrossRef]
- Keyzer, C.; Cullus, P.; Tack, D.; De Maertelaer, V.; Bohy, P.; Gevenois, P.A. MDCT for suspected acute appendicitis in adults: Impact of oral and IV contrast media at standard-dose and simulated low-dose techniques. AJR Am. J. Roentgenol. 2009, 193, 1272–1281. [Google Scholar] [CrossRef]
- Platon, A.; Jlassi, H.; Rutschmann, O.T.; Becker, C.D.; Verdun, F.R.; Gervaz, P.; Poletti, P.A. Evaluation of a low-dose CT protocol with oral contrast for assessment of acute appendicitis. Eur. Radiol. 2009, 19, 446–454. [Google Scholar] [CrossRef]
- Seo, H.; Lee, K.H.; Kim, H.J.; Kim, K.; Kang, S.B.; Kim, S.Y.; Kim, Y.H. Diagnosis of acute appendicitis with sliding slab ray-sum interpretation of low-dose unenhanced CT and standard-dose intravenous contrast-enhanced CT scans. AJR Am. J. Roentgenol. 2009, 193, 96–105. [Google Scholar] [CrossRef]
- Park, J.H.; LOCAT Group. Diagnostic imaging utilization in cases of acute appendicitis: Multi-center experience. J. Korean Med. Sci. 2014, 29, 1308–1316. [Google Scholar] [CrossRef]
- Pooler, B.D.; Lawrence, E.M.; Pickhardt, P.J. Alternative diagnoses to suspected appendicitis at CT. Radiology 2012, 265, 733–742. [Google Scholar] [CrossRef]
- Dym, R.J.; Duncan, D.R.; Spektor, M.; Cohen, H.W.; Scheinfeld, M.H. Renal stones on portal venous phase contrast-enhanced CT: Does intravenous contrast interfere with detection? Abdom. Imaging 2014, 39, 526–532. [Google Scholar] [CrossRef]
- Preminger, G.M.; Tiselius, H.G.; Assimos, D.G.; Alken, P.; Buck, C.; Gallucci, M.; Knoll, T.; Lingeman, J.E.; Nakada, S.Y.; Pearle, M.S.; et al. 2007 guideline for the management of ureteral calculi. J. Urol. 2007, 178, 2418–2434. [Google Scholar] [CrossRef]
- Drake, F.T.; Alfonso, R.; Bhargava, P.; Cuevas, C.; Dighe, M.K.; Florence, M.G.; Johnson, M.G.; Jurkovich, G.J.; Steele, S.R.; Symons, R.G.; et al. Enteral contrast in the computed tomography diagnosis of appendicitis: Comparative effectiveness in a prospective surgical cohort. Ann. Surg. 2014, 260, 311–316. [Google Scholar] [CrossRef]
- Rao, P.M.; Rhea, J.T.; Novelline, R.A.; Mostafavi, A.A.; Lawrason, J.N.; McCabe, C.J. Helical CT combined with contrast material administered only through the colon for imaging of suspected appendicitis. AJR Am. J. Roentgenol. 1997, 169, 1275–1280. [Google Scholar] [CrossRef][Green Version]
- Fefferman, N.R.; Roche, K.J.; Pinkney, L.P.; Ambrosino, M.M.; Genieser, N.B. Suspected appendicitis in children: Focused CT technique for evaluation. Radiology 2001, 220, 691–695. [Google Scholar] [CrossRef]
- Brassart, N.; Winant, C.; Tack, D.; Gevenois, P.A.; De Maertelaer, V.; Keyzer, C. Optimised z-axis coverage at multidetector-row CT in adults suspected of acute appendicitis. Br. J. Radiol. 2013, 86, 20130115. [Google Scholar] [CrossRef]
- Kamel, I.R.; Goldberg, S.N.; Keogan, M.T.; Rosen, M.P.; Raptopoulos, V. Right lower quadrant pain and suspected appendicitis: Nonfocused appendiceal CT--review of 100 cases. Radiology 2000, 217, 159–163. [Google Scholar] [CrossRef]
- Jacobs, J.E.; Birnbaum, B.A.; Macari, M.; Megibow, A.J.; Israel, G.; Maki, D.D.; Aguiar, A.M.; Langlotz, C.P. Acute appendicitis: Comparison of helical CT diagnosis focused technique with oral contrast material versus nonfocused technique with oral and intravenous contrast material. Radiology 2001, 220, 683–690. [Google Scholar] [CrossRef]
- Zanca, F.; Demeter, M.; Oyen, R.; Bosmans, H. Excess radiation and organ dose in chest and abdominal CT due to CT acquisition beyond expected anatomical boundaries. Eur. Radiol. 2012, 22, 779–788. [Google Scholar] [CrossRef]
- Lee, C.H.; Goo, J.M.; Ye, H.J.; Ye, S.J.; Park, C.M.; Chun, E.J.; Im, J.G. Radiation dose modulation techniques in the multidetector CT era: From basics to practice. Radiogr. A Rev. Publ. Radiol. Soc. N. Am. Inc. 2008, 28, 1451–1459. [Google Scholar] [CrossRef]
- Coakley, F.V.; Gould, R.; Yeh, B.M.; Arenson, R.L. CT radiation dose: What can you do right now in your practice? AJR Am. J. Roentgenol. 2011, 196, 619–625. [Google Scholar] [CrossRef]
- Lee, K.H.; Lee, J.M.; Moon, S.K.; Baek, J.H.; Park, J.H.; Flohr, T.G.; Kim, K.W.; Kim, S.J.; Han, J.K.; Choi, B.I. Attenuation-based automatic tube voltage selection and tube current modulation for dose reduction at contrast-enhanced liver CT. Radiology 2012, 265, 437–447. [Google Scholar] [CrossRef]
- Willemink, M.J.; Leiner, T.; de Jong, P.A.; de Heer, L.M.; Nievelstein, R.A.; Schilham, A.M.; Budde, R.P. Iterative reconstruction techniques for computed tomography part 2: Initial results in dose reduction and image quality. Eur. Radiol. 2013, 23, 1632–1642. [Google Scholar] [CrossRef]
- Park, J.H.; Kim, B.; Kim, M.S.; Kim, H.J.; Ko, Y.; Ahn, S.; Karul, M.; Fletcher, J.G.; Lee, K.H. Comparison of filtered back projection and iterative reconstruction in diagnosing appendicitis at 2-mSv CT. Abdom. Radiol. 2016, 41, 1227–1236. [Google Scholar] [CrossRef]
- Park, J.H.; Jeon, J.J.; Lee, S.S.; Dhanantwari, A.C.; Sim, J.Y.; Kim, H.Y.; Lee, K.H. Can we perform CT of the appendix with less than 1 mSv? A de-escalating dose-simulation study. Eur. Radiol. 2018, 28, 1826–1834. [Google Scholar] [CrossRef]
- Johnson, P.T.; Horton, K.M.; Kawamoto, S.; Eng, J.; Bean, M.J.; Shan, S.J.; Fishman, E.K. MDCT for suspected appendicitis: Effect of reconstruction section thickness on diagnostic accuracy, rate of appendiceal visualization, and reader confidence using axial images. AJR Am. J. Roentgenol. 2009, 192, 893–901. [Google Scholar] [CrossRef]
- Sprawls, P. AAPM tutorial. CT image detail and noise. Radiogr. A Rev. Publ. Radiol. Soc. N. Am. Inc. 1992, 12, 1041–1046. [Google Scholar] [CrossRef]
- Paulson, E.K.; Harris, J.P.; Jaffe, T.A.; Haugan, P.A.; Nelson, R.C. Acute appendicitis: Added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology 2005, 235, 879–885. [Google Scholar] [CrossRef]
- Lee, K.H.; Kim, Y.H.; Hahn, S.; Lee, K.W.; Kim, T.J.; Kang, S.B.; Shin, J.H. Computed tomography diagnosis of acute appendicitis: Advantages of reviewing thin-section datasets using sliding slab average intensity projection technique. Investig. Radiol. 2006, 41, 579–585. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kim, B.; Ko, Y.; Cho, K.E.; Hong, S.S.; Kim, D.H.; Song, H.; Lee, K.H. 2-mSv CT in adolescents and young adults with suspected appendicitis: Advantages of additional review of thin sections using multiplanar sliding-slab averaging technique. AJR Am. J. Roentgenol. 2015, 205, W485–W491. [Google Scholar] [CrossRef]
- Weisenthal, K.; Karthik, P.; Shaw, M.; Sengupta, D.; Bhargavan-Chatfield, M.; Burleson, J.; Mustafa, A.; Kalra, M.; Moore, C. Evaluation of kidney stones with reduced-radiation dose CT: Progress from 2011–2012 to 2015–2016—Not there yet. Radiology 2018, 286, 581–589. [Google Scholar] [CrossRef]
- Ahn, S.; LOCAT Group. LOCAT (low-dose computed tomography for appendicitis trial) comparing clinical outcomes following low- vs standard-dose computed tomography as the first-line imaging test in adolescents and young adults with suspected acute appendicitis: Study protocol for a randomized controlled trial. Trials 2014, 15, 28. [Google Scholar] [CrossRef][Green Version]
- Aly, N.E.; McAteer, D.; Aly, E.H. Low vs. standard dose computed tomography in suspected acute appendicitis: Is it time for a change? Int. J. Surg. 2016, 31, 71–79. [Google Scholar] [CrossRef]
- Yun, S.J.; Ryu, C.W.; Choi, N.Y.; Kim, H.C.; Oh, J.Y.; Yang, D.M. Comparison of low- and standard-dose CT for the diagnosis of acute appendicitis: A meta-analysis. AJR Am. J. Roentgenol. 2017, 208, W198–W207. [Google Scholar] [CrossRef]
- Yoon, H.M.; Suh, C.H.; Cho, Y.A.; Kim, J.R.; Lee, J.S.; Jung, A.Y.; Kim, J.H.; Lee, J.Y.; Kim, S.Y. The diagnostic performance of reduced-dose CT for suspected appendicitis in paediatric and adult patients: A systematic review and diagnostic meta-analysis. Eur. Radiol. 2018, 28, 2537–2548. [Google Scholar] [CrossRef]
- Brown, T.W.; McCarthy, M.L.; Kelen, G.D.; Levy, F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2010, 17, 553–560. [Google Scholar] [CrossRef]
- Howell, J.M.; Eddy, O.L.; Lukens, T.W.; Thiessen, M.E.; Weingart, S.D.; Decker, W.W. Clinical policy: Critical issues in the evaluation and management of emergency department patients with suspected appendicitis. Ann. Emerg. Med. 2010, 55, 71–116. [Google Scholar] [CrossRef]
- Mayo-Smith, W.W.; Hara, A.K.; Mahesh, M.; Sahani, D.V.; Pavlicek, W. How I do it: Managing radiation dose in CT. Radiology 2014, 273, 657–672. [Google Scholar] [CrossRef]
- Kim, S.Y.; Lee, K.H.; Kim, K.; Kim, T.Y.; Lee, H.S.; Hwang, S.S.; Song, K.J.; Kang, H.S.; Kim, Y.H.; Rhee, J.E. Acute appendicitis in young adults: Low- versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology 2011, 260, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.K.; Ko, Y.; Lee, M.H.; Woo, H.; Ahn, S.; Kim, B.; Pickhardt, P.J.; Kim, M.S.; Park, S.B.; Lee, K.H. Initial performance of radiologists and radiology residents in interpreting low-dose (2-mSv) appendiceal CT. AJR Am. J. Roentgenol. 2015, 205, W594–W611. [Google Scholar] [CrossRef] [PubMed]
- Parakh, A.; Kortesniemi, M.; Schindera, S.T. CT radiation dose management: A comprehensive optimization process for improving patient safety. Radiology 2016, 280, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Deak, P.D.; Smal, Y.; Kalender, W.A. Multisection CT protocols: Sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 2010, 257, 158–166. [Google Scholar] [CrossRef]
- Huda, W.; Mettler, F.A. Volume CT dose index and dose-length product displayed during CT: What good are they? Radiology 2011, 258, 236–242. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.H.; Kim, H.Y.; Sim, J.Y.; Lee, K.H. Low-Dose Abdominal CT for Evaluating Suspected Appendicitis: Recommendations for CT Imaging Techniques and Practical Issues. Diagnostics 2022, 12, 1585. https://doi.org/10.3390/diagnostics12071585
Park JH, Kim HY, Sim JY, Lee KH. Low-Dose Abdominal CT for Evaluating Suspected Appendicitis: Recommendations for CT Imaging Techniques and Practical Issues. Diagnostics. 2022; 12(7):1585. https://doi.org/10.3390/diagnostics12071585
Chicago/Turabian StylePark, Ji Hoon, Hae Young Kim, Ji Ye Sim, and Kyoung Ho Lee. 2022. "Low-Dose Abdominal CT for Evaluating Suspected Appendicitis: Recommendations for CT Imaging Techniques and Practical Issues" Diagnostics 12, no. 7: 1585. https://doi.org/10.3390/diagnostics12071585
APA StylePark, J. H., Kim, H. Y., Sim, J. Y., & Lee, K. H. (2022). Low-Dose Abdominal CT for Evaluating Suspected Appendicitis: Recommendations for CT Imaging Techniques and Practical Issues. Diagnostics, 12(7), 1585. https://doi.org/10.3390/diagnostics12071585





