C1-C2 Rotatory Subluxation in Adults “A Narrative Review”
Abstract
:1. Introduction
Objective
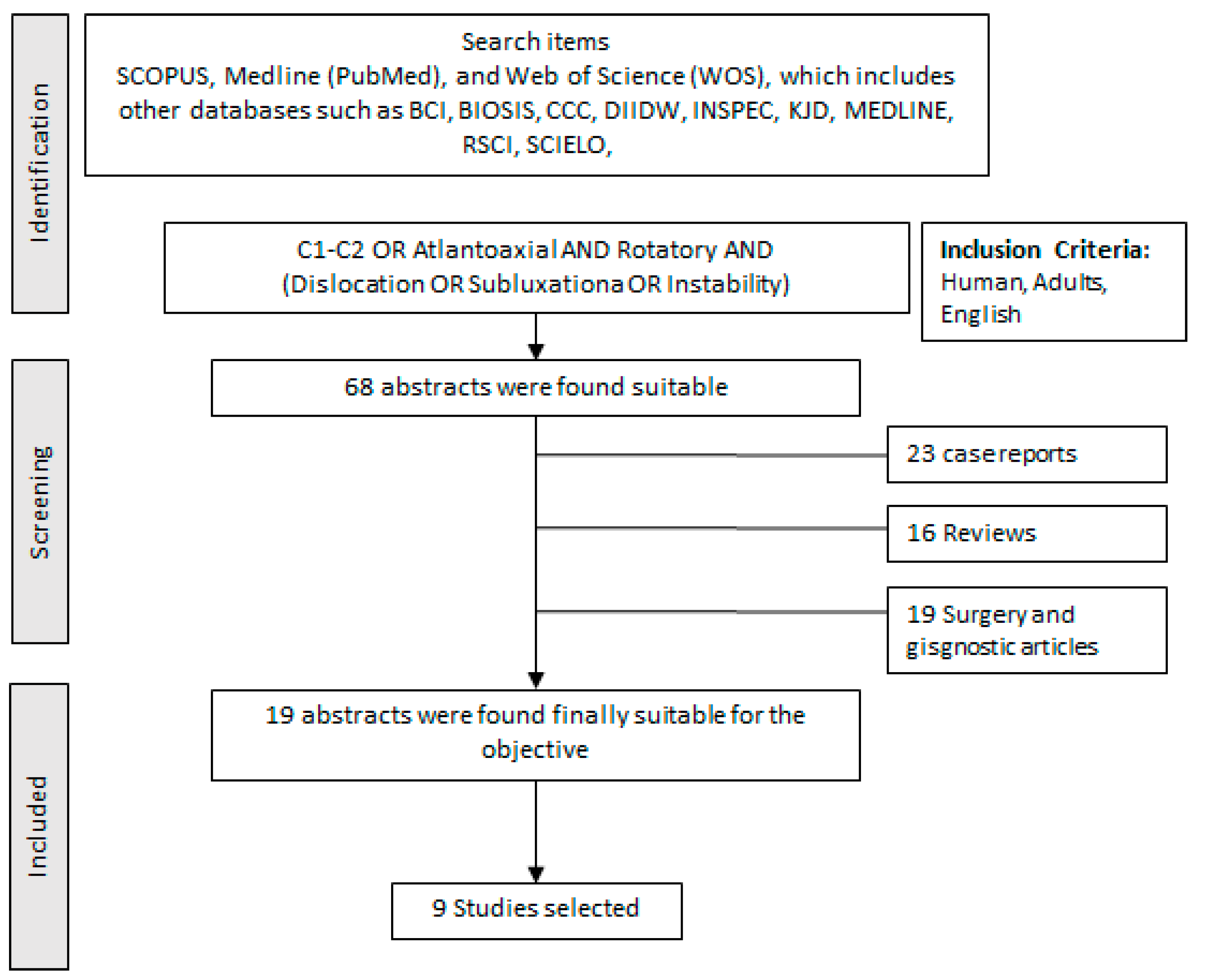
2. Materials and Methods
3. Etiology
3.1. Biomechanics of C1-C2
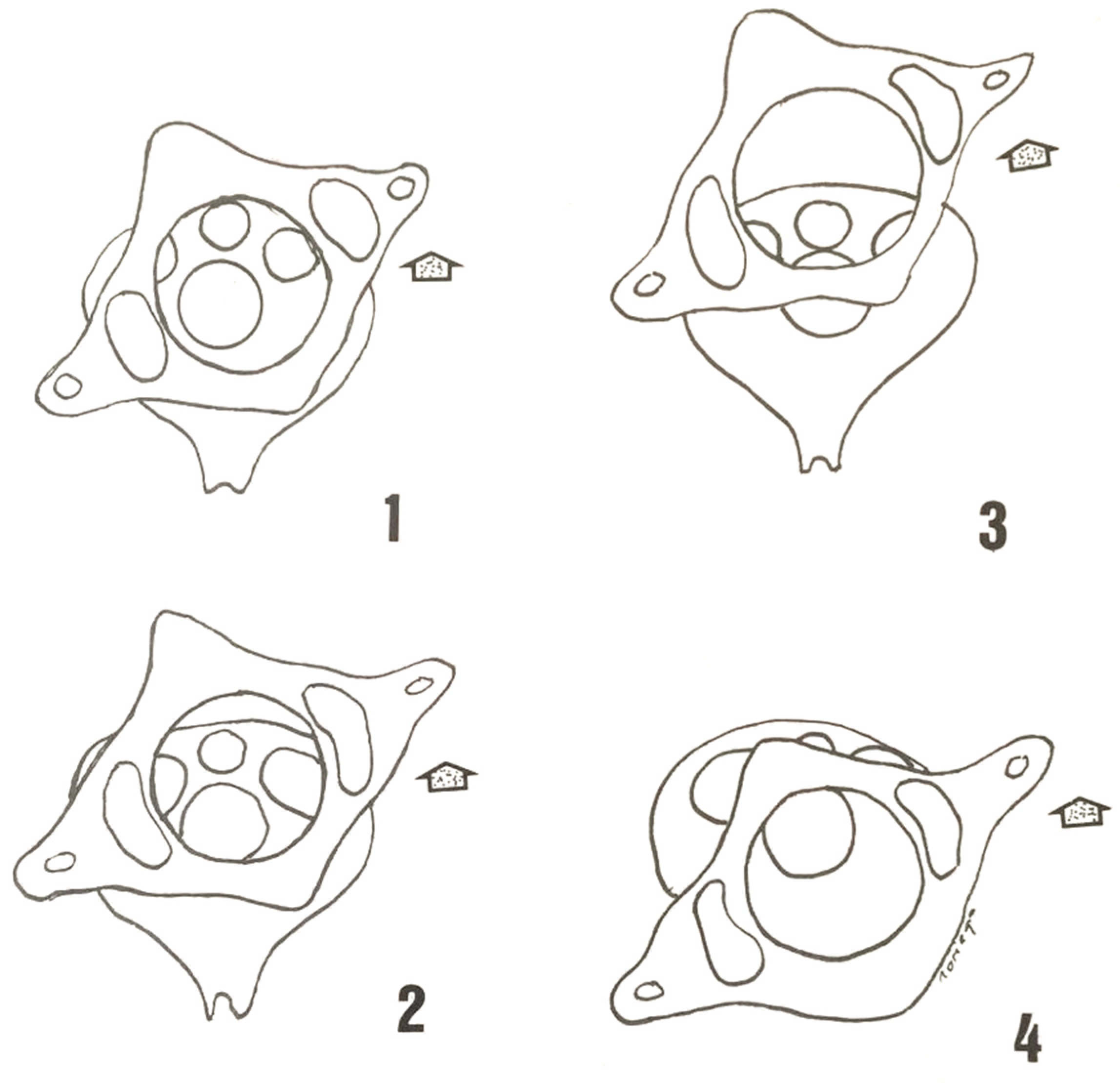
3.2. Classification
- (a)
- Traumatic basis (Table 1)
- (b)
- Based on the image
4. Clinical (Symptomatology)
5. Diagnosis
5.1. Simple X-ray
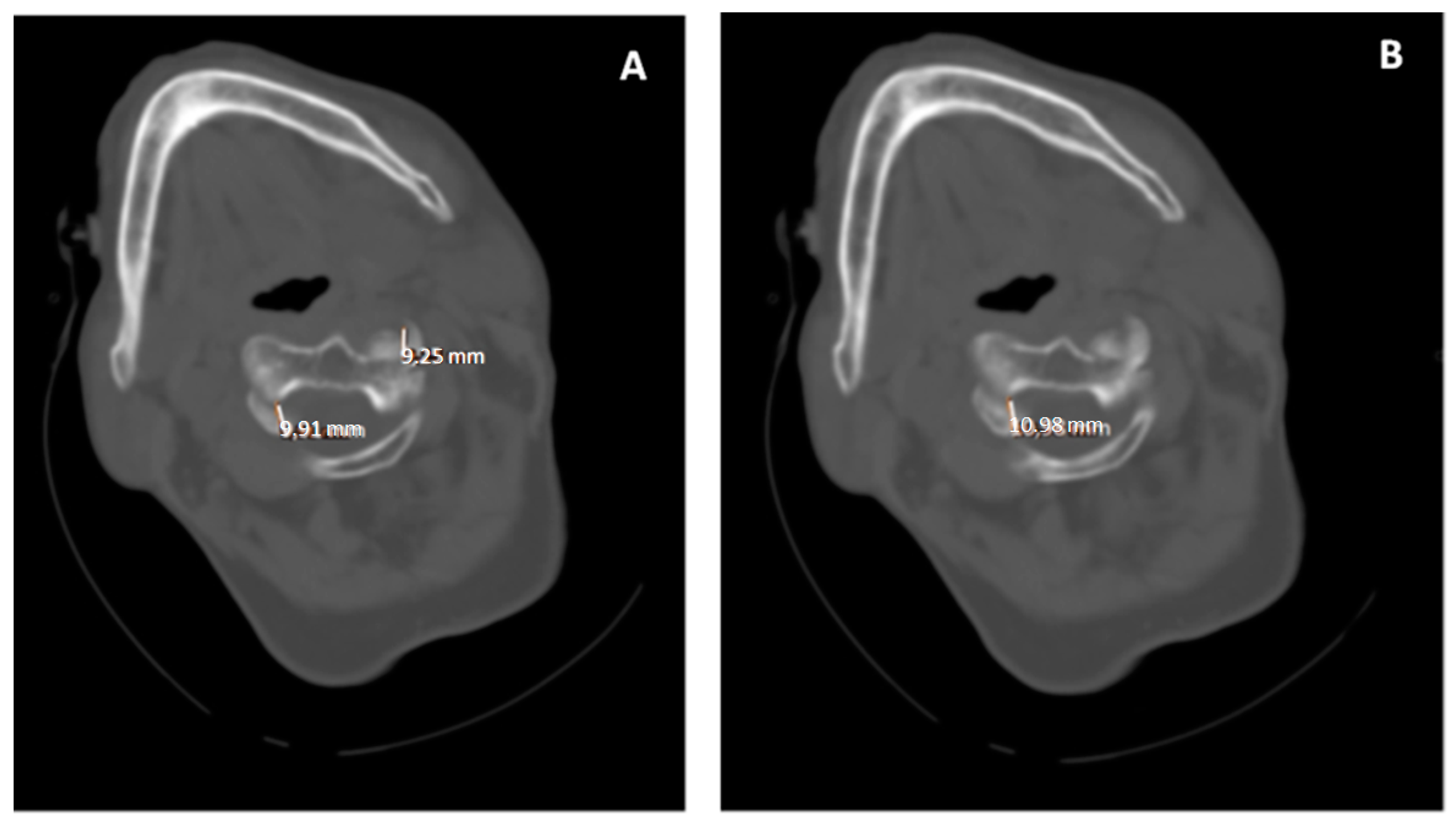
5.2. Computed Tomography (CT)
5.3. Magnetic Resonance Imaging (MRI)
6. Treatment
6.1. Conservative Treatment
- Philadelphia or Aspen-type rigid collar. It restricts cervical mobility partially, and above all in flexion-extension, being less effective for rotation and lateral flexion.
- SOMI (sternal occipital mandibular immobilization): is a system that allows immobilization in extension, flexion, or neutral position. The support is by means of anterior and posterior bars that are adjustable for the flexion-extension position and the support base extends over the scapulae and thorax.
- Cranial-thoracic halo with mentonian and occipital support. The support is by means of anterior and posterior bars that are adjustable for the flexion-extension position and the support base extends over the scapulae and thorax.
- Cervicothoracic Minerva. Provides frontal, occipital and mentonian support.
6.2. Surgical Treatment
Arthrodesis
- Magerl’s technique indicated for posterior cervical spine fixation.
- Harms and Melcher [64]: atlantoaxial stabilization technique by individual fixation of the lateral mass of C1 and the pedicle of C2 with minipoliaxial screws and rods.
- Gallie fusion technique. Gallie, in 1939, described the first posterior wiring technique for C1-C2 fixation, this technique used a single, central wire displaced sublaminarly under the posterior arch of C1 and around the spinous process of C2 that fixed in place a bone graft.
- Brooks and Jenkins introduced the fusion technique using two trapezoidal bone grafts between the posterior arch of C1 and the laminae of C2 secured with two wires that were placed sublaminarly [66].
- Dickmann and Sonntag technique, consisting of a modification of the previous techniques. In this case, the sublaminar wires were eliminated at C2, and the spinous process of C2 was used as the anchor point. Intraoperatively, the C1-C2 interlaminar space was widened.
- Goel and Laheri technique [67,68] developed an atlantoaxial fusion technique that was later popularized by Jurgen Harms and Robert Melchor in 2001 [61]. The technique consists of using polyaxial screws in the lateral mass of C1 and in the pedicle of C2 and rods. Once the screws have been placed, reduction in the dislocation is achieved, and the rods are then placed.
- Interlaminar clamp technique provides a fusion similar to the Brooks–Jenkins method, but without the disadvantage of sublaminar wires.
- Halifax technique uses a double hook and screw that stabilizes the laminae of C1 and C2 bilaterally and secures bilateral interlaminar bone grafts [69].
7. Discussion
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guleryuz, A.; Bagdatoglu, C.; Duce, M.N.; Talas, D.U.; Celikbas, H.; Köksel, T. Grisel’s syndrome. J. Clin. Neurosci. 2002, 9, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Tortora, G.J.; Derrickson, B. Principios de Anatomía y Fisiología, 15th ed.; Médica Panamericana: Madrid, Spain, 2021. [Google Scholar]
- White, A.A., 3rd; Panjabi, M.M. The clinical biomechanics of the occipitoatlantoaxial complex. Orthop. Clin. N. Am. 1978, 9, 867–878. [Google Scholar] [CrossRef]
- Tulsi, R.S. Some specific anatomical features of the atlas and axis: Dens, epitransverse process and articular facets. Aust. N. Z. J. Surg. 1978, 48, 570–574. [Google Scholar] [CrossRef]
- De Beer, J.; Thomas, M.; Walters, J.; Anderson, P. Traumatic atlanto-axial subluxation. J. Bone Jt. Surg. Br. Vol. 1988, 70, 652–655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Khoury, G.Y.; Clark, C.R.; Gravett, A.W. Acute traumatic rotatory atlanto-axial dislocation in children. A report of three cases. J. Bone Joint Surg. Am. 1984, 66, 774–777. [Google Scholar] [CrossRef]
- Hutton, B.; Catalá-López, F.; Moher, D. La extensión de la declaración PRISMA para revisiones sistemáticas que incorporan metaanálisis en red: PRISMA-NMA. Med. Clín. 2016, 147, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Battiata, A.P.; Pazos, G. Grisel’s syndrome: The two-hit hypothesis--a case report and literature review. Ear Nose Throat J. 2004, 83, 553–555. [Google Scholar] [CrossRef] [Green Version]
- Serdaroğlu, B.; Duygu, D.; Erhan, Ç.; Haydar, U.; Mehmet, T.; Ahmet, S. Grisel’s Syndrome-Case. Turk. J. Rheumatol. 2011, 26, 243–247. [Google Scholar] [CrossRef]
- Fernández Cornejo, V.J.; Martínez-Lage, J.F.; Piqueras, C.; Gelabert, A.; Poza, M. Inflammatory atlanto-axial subluxation (Grisel’s syndrome) in children: Clinical diagnosis and management. Child’s Nerv. Syst. 2003, 19, 342–347. [Google Scholar] [CrossRef]
- Das, S.; Chakraborty, S.; Das, S. Grisel Syndrome in Otolaryngology: A Case Series with Literature Review. Indian J. Otolaryngol. Head Neck Surg. 2019, 71, 66–69. [Google Scholar] [CrossRef]
- Parke, W.W.; Rothman, R.H.; Brown, M.D. The pharyngovertebral veins: An anatomical rationale for Grisel’s syndrome. J. Bone Jt. Surg. Am. 1984, 66, 568–574. [Google Scholar] [CrossRef]
- Alqroom, R.Y.; Jeszenszky, D.J.; Michalitsis, G.S.; Franke, J. Non-traumatic Atlanto-axial Rotatory Subluxation-Grisel’s Syndrome Case Report and Literature Review. J. Spine 2016, 5. [Google Scholar] [CrossRef] [Green Version]
- Matos, T.D.; Pinheiro, R.P.; Costa, H.R.T.; Defino, H.L.A. Rotational dislocation C1-C2 after otoplasty under local anesthesia. J. Craniovertebral Junction Spine 2020, 11, 237–239. [Google Scholar] [CrossRef] [PubMed]
- Chechik, O.; Wientroub, S.; Danino, B.; Lebel, D.E.; Ovadia, D. Successful Conservative Treatment for Neglected Rotatory Atlantoaxial Dislocation. J. Pediatr. Orthop. 2013, 33, 389–392. [Google Scholar] [CrossRef] [PubMed]
- Pang, D.; Li, V. Atlantoaxial Rotatory Fixation: Part 2—New Diagnostic Paradigm and a New Classification Based on Motion Analysis Using Computed Tomographic Imaging. Neurosurgery 2005, 57, 941–953. [Google Scholar] [CrossRef]
- Barcelos, A.C.E.S.; Patriota, G.C.; Netto, A.U. Nontraumatic Atlantoaxial Rotatory Subluxation: Grisel Syndrome. Case Report and Literature Review. Glob. Spine J. 2014, 4, 179–185. [Google Scholar] [CrossRef] [Green Version]
- Roche, C.J.; O’Malley, M.; Dorgan, J.C.; Carty, H.M. A Pictorial Review of Atlanto-axial Rotatory Fixation: Key Points for the Radiologist. Clin. Radiol. 2001, 56, 947–958. [Google Scholar] [CrossRef]
- Pang, D.; Li, V. Atlantoaxial Rotatory Fixation: Part 1—Biomechanics OF Normal Rotation at the Atlantoaxial Joint in Children. Neurosurgery 2004, 55, 614–626. [Google Scholar] [CrossRef]
- Fielding, J.W.; Hawkins, R.J.; Ratzan, S.A. Spine fusion for atlanto-axial instability. J. Bone Jt. Surg. 1976, 58, 400–407. [Google Scholar] [CrossRef]
- Martín-Ferrer, S. Traumatismos de la columna cervical alta: Clasificación tipológica, indicaciones terapéuticas y abordajes quirúrgicos (a propósito de 286 casos). Neurocirugía 2006, 17, 391–419. [Google Scholar] [CrossRef] [Green Version]
- Horsfall, H.L.; Gharooni, A.-A.; Al-Mousa, A.; Shtaya, A.; Pereira, E. Traumatic atlantoaxial rotatory subluxation in adults—A case report and literature review. Surg. Neurol. Int. 2020, 11, 376. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.; Dominguez, J.F.; Feldstein, E.; Houten, J.K.; Spirollari, E.; Gandhi, C.D.; Cole, C.D.; Kinon, M.D. Does alar ligament injury predict conservative treatment failure of atlantoaxial rotatory subluxation in adults: Case report and review of the literature. Spinal Cord Ser. Cases 2021, 7, 103. [Google Scholar] [CrossRef] [PubMed]
- McGuire, K.J.; Silber, J.; Flynn, J.M.; Levine, M.; Dormans, J.P. Torticollis in children: Can dynamic computed tomography help determine severity and treatment. J. Pediatr. Orthop. 2002, 22, 766–770. [Google Scholar] [CrossRef] [PubMed]
- Scapinelli, R. Three-dimensional computed tomography in infantile atlantoaxial rotatory fixation. J. Bone Jt. Surg. Br. 1994, 76, 367–370. [Google Scholar] [CrossRef]
- Ishii, K.; Chiba, K.; Maruiwa, H.; Nakamura, M.; Matsumoto, M.; Toyama, Y. Pathognomonic radiological signs for predicting prognosis in patients with chronic atlantoaxial rotatory fixation. J. Neurosurg. Spine 2006, 5, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, M.S. Handbook of Neurosurgery, 6th ed.; Thieme: Lakeland, FL, USA, 2006; pp. 623–626. [Google Scholar]
- Samartzis, D.; Shen, F.H.; Herman, J.; Mardjetko, S.M. Atlantoaxial rotatory fixation in the setting of associated congenital malformations: A modified classification system. Spine 2010, 35, E119–E127. [Google Scholar] [CrossRef] [PubMed]
- Been, H.D.; Kerkhoffs, G.M.; Maas, M. Suspected atlantoaxial rotatory fixation-subluxation: The value of multidetector computed tomography scanning under general anesthesia. Spine 2007, 32, E163–E167. [Google Scholar] [CrossRef] [PubMed]
- Sobolewski, B.A.; Mittiga, M.R.; Reed, J.L. Atlantoaxial rotary subluxation after minor trauma. Pediatr. Emerg. Care 2008, 24, 852–856. [Google Scholar] [CrossRef]
- Alanay, A.; Hicazi, A.; Acaroglu, E.; Yazici, M.; Aksoy, C.; Cila, A.; Akalan, N.; Sura, A. Reliability and necessity of dynamic computerized tomography in diagnosis of atlantoaxial rotatory subluxation. J. Pediatr. Orthop. 2002, 22, 763–765. [Google Scholar] [CrossRef]
- Hicazi, A.; Acaroglu, E.; Alanay, A.; Yazici, M.; Surat, A. Atlantoaxial rotatory fixation-subluxation revisited: A computed tomographic analysis of acute torticollis in pediatric patients. Spine 2002, 27, 2771–2775. [Google Scholar] [CrossRef]
- Landi, A.; Pietrantonio, A.; Marotta, N.; Mancarella, C.; Delfini, R. Atlantoaxial rotatory dislocation (AARD) in pediatric age: MRI study on conservative treatment with Philadelphia collar—experience of nine consecutive cases. Eur. Spine J. 2012, 21, S94–S99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abumi, K.; Shono, Y.; Taneichi, H.; Ito, M.; Kaneda, K. Correction of Cervical Kyphosis Using Pedicle Screw Fixation Systems. Spine 1999, 24, 2389–2396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Opoku-Darko, M.; Isaacs, A.; Du Plessis, S. Closed reduction of traumatic atlantoaxial rotatory subluxation with type II odontoid fracture. Interdiscip. Neurosurg. 2018, 11, 19–23. [Google Scholar] [CrossRef]
- Fath, L.; Cebula, H.; Santin, M.; Coca, A.; Debry, C.; Proust, F. The Grisel’s syndrome: A non-traumatic subluxation of the atlantoaxial joint. Neurochirurgie 2018, 64, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Pang, D. Atlantoaxial rotatory fixation. Neurosurgery 2010, 66, 161–183. [Google Scholar] [CrossRef] [PubMed]
- Subach, B.R.; McLaughlin, M.R.; Albright, A.L.; Pollack, I.F. Current Management of Pediatric Atlantoaxial Rotatory Subluxation. Spine 1998, 23, 2174–2179. [Google Scholar] [CrossRef] [PubMed]
- Ishii, K.; Matsumoto, M.; Momoshima, S.; Watanabe, K.; Tsuji, T.; Takaishi, H.; Nakamura, M.; Toyama, Y.; Chiba, K. Remodeling of C2 Facet Deformity Prevents Recurrent Subluxation in Patients With Chronic Atlantoaxial Rotatory Fixation. Spine 2011, 36, E256–E262. [Google Scholar] [CrossRef]
- Ishii, K.; Toyama, Y.; Nakamura, M.; Chiba, K.; Matsumoto, M. Management of Chronic Atlantoaxial Rotatory Fixation. Spine 2012, 37, E278–E285. [Google Scholar] [CrossRef]
- Graziano, G.P.; Herzenberg, J.E.; Hensinger, R.N. The halo-Ilizarov distraction cast for correction of cervical deformity. Report of six cases. J. Bone Jt. Surg. 1993, 75, 996–1003. [Google Scholar] [CrossRef]
- Yeung, C.-Y.; Feng, C.-K. Halter Traction for the Treatment of Atlantoaxial Rotatory Fixation. J. Bone Jt. Surg. 2022, 104, 229–238. [Google Scholar] [CrossRef]
- Kia, C.; Mallozzi, S.; Moss, I. Chronic Atlantoaxial Rotatory Subluxation in an Adult Following a Traumatic Event: A Case Report. Int. J. Spine Surg. 2020, 14, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Fessler, R.G.; Sekhar, L.N. Atlas Neurosurgical Techniques: Spine and Peripheral Nerves; Thieme: New York, NY, USA, 2016. [Google Scholar]
- Vaccaro, A.R. Fractures of the Cervical, Thoracic, and Lumbar Spine, 1st ed.; CRC Press: Boca Raton, FL, USA, 2002. [Google Scholar] [CrossRef]
- Tauchi, R.; Imagama, S.; Ito, Z.; Ando, K.; Muramoto, A.; Matsui, H.; Matsumoto, T.; Yukawa, Y.; Kanemura, T.; Ishiguro, N. Surgical treatment for chronic atlantoaxial rotatory fixation in children. J. Pediatr. Orthop. B 2013, 22, 404–408. [Google Scholar] [CrossRef] [PubMed]
- Beier, A.D.; Vachhrajani, S.; Bayerl, S.H.; Aguilar, C.Y.D.; Lamberti-Pasculli, M.; Drake, J.M. Rotatory subluxation: Experience from the Hospital for Sick Children. J. Neurosurg. Pediatr. 2012, 9, 144–148. [Google Scholar] [CrossRef]
- Florensa, R. Indicaciones de la fijación posterior en columna cervical. Neurocir. XXI 1999, 5, 239–256. [Google Scholar]
- Huang, D.-G.; Hao, D.-J.; He, B.-R.; Wu, Q.-N.; Liu, T.-J.; Wang, X.-D.; Guo, H.; Fang, X.-Y. Posterior atlantoaxial fixation: A review of all techniques. Spine J. 2015, 15, 2271–2281. [Google Scholar] [CrossRef]
- Morales, L.C.; Alvarado, F.; Corredor, J.A.; Rodríguez, A. Bilateral C1 laminar hooks combined with C2 pedicle screw fixation in the treatment of atlantoaxial subluxation after Grisel syndrome. Spine J. 2016, 16, e755–e760. [Google Scholar] [CrossRef] [PubMed]
- Pereira, E.A.C.; Hempenstall, J.; Pretorius, P.M.; Kamat, A.A.; Cadoux-Hudson, T.A.D. La maladie de Grisel treated by combined C1-2 transarticular and C1 lateral mass screw fixation. Br. J. Neurosurg. 2010, 24, 499–501. [Google Scholar] [CrossRef]
- Unni, C.; Pettakkandy, V.; Jaleel, P.A.; Soren, S.K.; Vineeth, K.K. Atlantoaxial Stabilization by Posterior C1 and C2 Screw-Rod Fixation for Various Pathologies: Case Series and Comprehensive Review of Literature. J. Neurosci. Rural Pract. 2021, 12, 228–235. [Google Scholar] [CrossRef]
- Allen, B.L.; Ferguson, R.L.; Lehmann, T.R.; Oʼbrien, R.P. A Mechanistic Classification of Closed, Indirect Fractures and Dislocations of the Lower Cervical Spine. Spine 1982, 7, 1–27. [Google Scholar] [CrossRef]
- Vaccaro, A.R.; Hulbert, R.J.; Patel, A.A.; Fisher, C.; Dvorak, M.; Lehman, R.A.; Anderson, P.; Harrop, J.; Oner, F.C.; Arnold, P.; et al. The Subaxial Cervical Spine Injury Classification System. Spine 2007, 32, 2365–2374. [Google Scholar] [CrossRef] [Green Version]
- Mihara, H.; Cheng, B.C.; David, S.M.; Ohnari, K.; Zdeblick, T.A. Biomechanical Comparison of Posterior Cervical Fixation. Spine 2001, 26, 1662–1667. [Google Scholar] [CrossRef] [PubMed]
- Kehr, P.; Weidner, A. Cervical Spine I, 1st ed.; Springer: Strasbourg, France, 1987. [Google Scholar]
- Abumi, K.; Itoh, H.; Taneichi, H.; Kaneda, K. Transpedicular Screw Fixation for Traumatic Lesions of the Middle and Lower Cervical Spine. J. Spinal Disord. 1994, 7, 19–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lapsiwala, S.B.; Anderson, P.A.; Oza, A.; Resnick, D.K. Biomechanical Comparison of Four C1 to C2 Rigid Fixative Techniques: Anterior Transarticular, Posterior Transarticular, C1 to C2 Pedicle, and C1 to C2 Intralaminar Screws. Neurosurgery 2006, 58, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Menendez, J.A.; Wright, N.M. Techniques of Posterior C1–C2 Stabilization. Neurosurgery 2007, 60, S103–S111. [Google Scholar] [CrossRef] [PubMed]
- Vender, J.R.; Rekito, A.J.; Harrison, S.J.; McDonnell, D.E. Evolution of posterior cervical and occipitocervical fusion and instrumentation. Neurosurg. Focus 2004, 16, E9. [Google Scholar] [CrossRef]
- Chen, Q.; Brahimaj, B.C.; Khanna, R.; Kerolus, M.G.; Tan, L.A.; David, B.T.; Fessler, R.G. Posterior atlantoaxial fusion: A comprehensive review of surgical techniques and relevant vascular anomalies. J. Spine Surg. 2020, 6, 164–180. [Google Scholar] [CrossRef]
- Bhimani, A.D.; Chiu, R.G.; Esfahani, D.R.; Patel, A.S.; Denyer, S.; Hobbs, J.G.; Mehta, A.I. C1-C2 Fusion Versus Occipito-Cervical Fusion for High Cervical Fractures: A Multi-Institutional Database Analysis and Review of the Literature. World Neurosurg. 2018, 119, e459–e466. [Google Scholar] [CrossRef]
- Ashafai, N.S.; Visocchi, M.; Wąsik, N. Occipitocervical Fusion: An Updated Review. Acta Neurochir. Suppl. 2019, 125, 247–252. [Google Scholar] [CrossRef]
- Mixter, S.J.; Osgood, R.B. Traumatic Lesions of the Atlas and Axis. Ann. Surg. 1910, 51, 193–207. [Google Scholar] [CrossRef]
- Harms, J.; Melcher, R.P. Posterior C1–C2 Fusion with Polyaxial Screw and Rod Fixation. Spine 2001, 26, 2467–2471. [Google Scholar] [CrossRef]
- Mummaneni, P.V.; Haid, R.W. Atlantoaxial fixation: Overview of all techniques. Neurol. India 2005, 53, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Coyne, T.J.; Fehlings, M.G.; Wallace, M.C.; Bernstein, M.; Tator, C.H. C1-C2 Posterior Cervical Fusion. Neurosurgery 1995, 37, 688–693. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Desai, K.I.; Muzumdar, D.P. Atlantoaxial fixation using plate and screw method: A report of 160 treated patients. Neurosurgery 2002, 51, 1351–1357. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Laheri, V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir. 1994, 129, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Hitchon, P.W.; Rengachary, S.S.; Traynelis, V.C. Techniques in Spinal Fusion and Stabilization; Thieme: New York, NY, USA, 1995. [Google Scholar]
- Xu, J.; Yin, Q.; Xia, H.; Wu, Z.; Ma, X.; Zhang, K.; Wang, Z.; Yang, J.; Ai, F.; Wang, J.; et al. New Clinical Classification System for Atlantoaxial Dislocation. Orthopedics 2013, 36, e95–e100. [Google Scholar] [CrossRef] [Green Version]
- Sinigaglia, R.; Bundy, A.; Monterumici, D.A. Traumatic atlantoaxial rotatory dislocation in adults. Chir. Narzadow Ruchu Ortop. Pol. 2008, 73, 149–154. [Google Scholar]
- Isik, H.S.; Sandal, E.; Cagli, S. Clinical outcomes of posterior c1 and c2 screw-rod fixation for atlantoaxial instability. Turk. Neurosurg. 2017, 2, 17–22. [Google Scholar] [CrossRef]
- Kim, B.; Iwata, K.; Sugimoto, K.; Suzuki, S.; Ema, Y.; Tsunobuchi, H.; Nishiwaki, K. Significance of prevention and early treatment of a postoperative twisted neck: Atlantoaxial rotatory subluxation after head and neck surgery. J. Anesth. 2010, 24, 598–602. [Google Scholar] [CrossRef]
- Van Holsbeeck, E.; Mackay, N. Diagnosis of acute atlanto-axial rotatory fixation. J. Bone Jt. Surg. Br. Vol. 1989, 71, 90–91. [Google Scholar] [CrossRef]



|
| Fielding–Hawkins Classification | Description | Therapeutic Strategy |
|---|---|---|
| Type I | Pure rotation of the atlas in relation to the axis without anterior displacement | Conservative treatment: soft collar, non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants. |
| Type II | Rotated atlas with anterior displacement of 3 to 5 mm | Conservative treatment, reduction, Philadelphia brace |
| Type III | Atlas rotated with anterior displacement greater than 5 mm | Surgical treatment, open reduction, fusion of C1-C2 |
|
| Author. | Etiology | Mainly Symptom | Complications | Treatment |
|---|---|---|---|---|
| Xu et al. [71] | Varied | Varied | No | Surgery |
| Sinigaglia et al. [72] | Traumatic | Pain Deformity | Residual pain at follow-up | Halo |
| Isik et al. [73] | Rheumatoid arthritis | Pain Myelopathy | No | Surgery |
| Kim et al. [74] | Iatrogenic-postsurgery | Pain Deformity | No | Conservative Traction Surgery |
| Graziano et al. [41] | Rheumatoid arthritis Traumatic Ankylosing spondylitis | Deformity Renal and cardiopulmonary problems | Cast sores Pin infection | External fixator (50% recurrence) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González, D.C.N.; Ardura Aragón, F.; Sanjuan, J.C.; Maniega, S.S.; Andrino, A.L.; García Fraile, R.; Labrador Hernández, G.; Calabia-Campo, J.; Caballero-García, A.; Córdova-Martínez, A. C1-C2 Rotatory Subluxation in Adults “A Narrative Review”. Diagnostics 2022, 12, 1615. https://doi.org/10.3390/diagnostics12071615
González DCN, Ardura Aragón F, Sanjuan JC, Maniega SS, Andrino AL, García Fraile R, Labrador Hernández G, Calabia-Campo J, Caballero-García A, Córdova-Martínez A. C1-C2 Rotatory Subluxation in Adults “A Narrative Review”. Diagnostics. 2022; 12(7):1615. https://doi.org/10.3390/diagnostics12071615
Chicago/Turabian StyleGonzález, David C. Noriega, Francisco Ardura Aragón, Jesús Crespo Sanjuan, Silvia Santiago Maniega, Alejandro León Andrino, Rubén García Fraile, Gregorio Labrador Hernández, Juan Calabia-Campo, Alberto Caballero-García, and Alfredo Córdova-Martínez. 2022. "C1-C2 Rotatory Subluxation in Adults “A Narrative Review”" Diagnostics 12, no. 7: 1615. https://doi.org/10.3390/diagnostics12071615








