Effects of TIMP1 rs4898 Gene Polymorphism on Early-Onset Preeclampsia Development and Placenta Weight
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. DNA Extraction
2.3. Genotyping
2.4. Statistical Analyses
3. Results
3.1. Clinical Characteristics of the Study Population
3.2. Association Analysis of MMP1, MMP9, TIMP1 and TIMP2 Polymorphisms
3.3. Haplotype and Gene-Gene Interaction Analysis
Haplotype Analysis of the MMP9 and TIMP2 Gene Polymorphisms
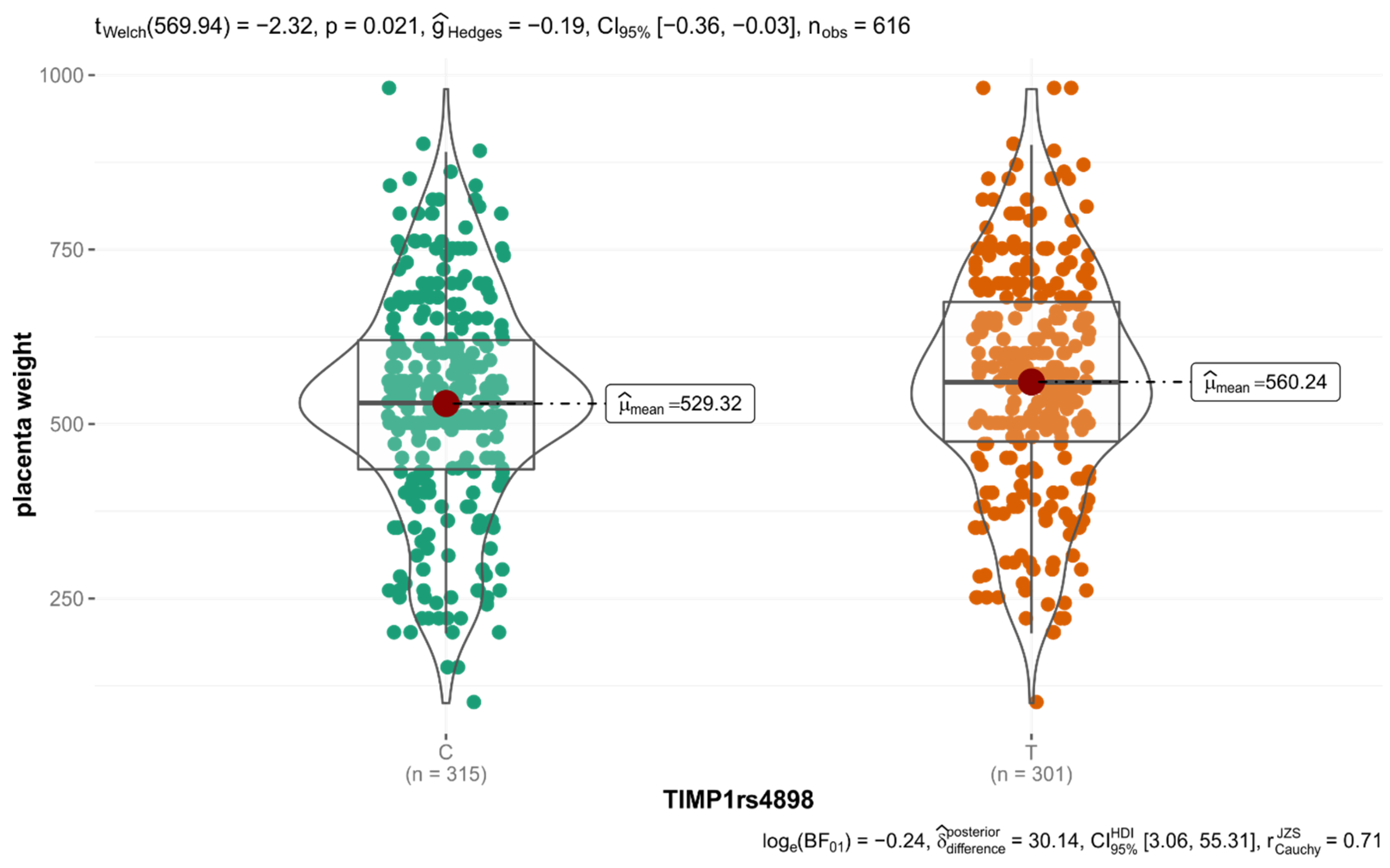
3.4. Association between Genotypes and Clinical Characteristics
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steegers, E.A.P.; von Dadelszen, P.; Duvekot, J.J.; Pijnenborg, R. Pre-eclampsia. Lancet 2010, 376, 631–644. [Google Scholar] [CrossRef]
- Nikolov, A.; Popovski, N. Role of gelatinases MMP-2 and MMP-9 in healthy and complicated pregnancy and their future potential as preeclampsia biomarkers. Diagnostics 2021, 11, 480. [Google Scholar] [CrossRef] [PubMed]
- Misra, G.A. Matrix metalloproteinases in neuroinflammation. Glia 2002, 39, 279–291. [Google Scholar]
- Misra, S.; Talwar, P.; Kumar, A.; Kumarb, P.; Sagara, R.; Vibhaa, D.; Pandita, A.K.; Gulatic, A.; Kushwahad, S.; Prasada, K. Association between matrix metalloproteinase family gene polymorphisms and risk of ischemic stroke: A systematic review and meta-analysis of 29 studies. Gene 2018, 672, 180–194. [Google Scholar] [CrossRef]
- Chen, J.; Khalil, R.A. Matrix metalloproteinases in normal pregnancy and preeclampsia. Prog. Mol. Biol. Transl. Sci. 2017, 148, 87–165. [Google Scholar] [PubMed]
- Yu, Y.; Wang, L.; Liu, T.; Guan, H. MicroRNA-204 suppresses trophoblast-like cell invasion by targeting matrix metalloproteinase-9. Biochem. Biophys. Res. Commun. 2015, 463, 285–291. [Google Scholar] [CrossRef]
- Borkakoti, N. Structural studies of matrix metalloproteinases. J. Mol. Med. 2000, 78, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Crocker, S.J.; Pagenstecher, A.; Campbell, I.L. The TIMPs tango with MMPs and more in the central nervous system. J. Neurosci. Res. 2004, 75, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Pereira, R.D.; De Long, N.E.; Wang, R.C.; Yazdi, F.T.; Holloway, A.C.; Raha, S. Angiogenesis in the placenta: The role of reactive oxygen species signaling. BioMed Res. Int. 2015, 2015, 814543. [Google Scholar] [CrossRef] [PubMed]
- Burton, G.J.; Woods, A.W.; Jauniaux, E.; Kingdom, J.C.P. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta 2009, 30, 473–482. [Google Scholar] [CrossRef]
- Lin, C.; He, H.; Cui, N.; Ren, Z.; Zhu, M.; Khalil, R.A. Decreased uterine vascularization and uterine arterial expansive remodeling with reduced matrix metalloproteinase-2 and -9 in hypertensive pregnancy. Am. J. Physiol. Heart Circ. 2020, 318, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Montagnana, M.; Lippi, G.; Albiero, A.; Scevarolli, S.; Salvagno, G.L.; Franchi, M.; Guidi, G.C. Evaluation of metalloproteinases 2 and 9 and their inhibitors in physiologic and pre-eclamptic pregnancy. J. Clin. Lab. Anal. 2009, 23, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Barišić, A.; Dević, P.S.; Ostojić, S.; Perezaa, N. Matrix metalloproteinase and tissue inhibitors of metalloproteinases gene polymorphisms in disorders that influence fertility and pregnancy complications: A systematic review and meta-analysis. Gene 2018, 647, 48–60. [Google Scholar]
- Coolman, M.; de Maat, M.; Van Heerde, W.L.; Felida, L.; Schoormans, S.; Steegers, E.A.P.; Bertina, R.M.; de Groot, C.J.M. Matrix metalloproteinase-9 gene-1562C/T polymorphism mitigates preeclampsia. Placenta 2007, 28, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Palei, A.C.T.; Sandrim, V.C.; Duarte, G.; Cavallic, R.C.; Gerlachd, R.F.; Tanus-Santose, J.E. Matrix metalloproteinase (MMP)-9 genotypes and haplotypes in preeclampsia and gestational hypertension. Clin. Chim. Acta 2010, 411, 874–877. [Google Scholar] [CrossRef] [PubMed]
- Palei, A.C.T.; Sandrim, V.C.; Amaral, L.M.; Machado, J.S.R.; Cavalli, R.C.; Lacchini, R.; Duarte, G.; Tanus-Santos, J.E. Matrix metalloproteinase-9 polymorphisms affect plasma MMP-9 levels and antihypertensive therapy responsiveness in hypertensive disorders of pregnancy. Pharm. J. 2012, 12, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, Z.; Rahimi, Z.; Shahsavandi, M.O.; Bidoki, K.; Rezaei, M. MMP-9 (-1562 C:T) polymorphism as a biomarker of susceptibility to severe pre-eclampsia. Biomark. Med. 2013, 7, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Leonardo, D.P.; Albuquerque, D.M.; Lanaro, C.; Baptista, L.C.; Cecatti, J.G.; Surita, F.G.; Parpinelli, M.A.; Costa, F.F.; Franco-Penteado, C.F.; Fertrin, K.Y.; et al. Association of nitric oxide synthase and matrix metalloprotease single nucleotide polymorphisms with preeclampsia and its complications. PLOS ONE. 2015, 10, e0136693. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Zhang, Q.; Hu, B.; Zhang, K. Investigation of the association between matrix metalloproteinase-9 genetic polymorphisms and development of pre-eclampsia in Chinese pregnant women. Gen Mol. Res. 2016, 15, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Luizon, M.R.; Sandrim, V.C.; Palei, A.C.; Lacchini, R.; Cavalli, R.C.; Duarte, G.; Tanus-Santos, J.E. Epistasis among eNOS, MMP-9 and VEGF maternal genotypes in hypertensive disorders of pregnancy. Hypertens. Res. 2012, 35, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Cao, X.; Wang, Q.; Guo, C.; Cao, X.; Wang, Q.; Wang, G.; An, L.; Du, M.; Qiu, Y.; et al. Contribution of TIMP3 polymorphisms to the development of preeclampsia in Han Chinese women. J. Assist. Reprod. Genet. 2015, 32, 1525–1530. [Google Scholar] [CrossRef] [PubMed][Green Version]
- ACOG. ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet. Gynecol. 2019, 133, 1–25. [Google Scholar]
- R Core Team. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria; Available online: https://www.R-project.org/ (accessed on 30 September 2021).
- Patil, I. Visualizations with statistical details: The ‘ggstatsplot’ approach. J. Open Source Softw. 2021, 6, 1–5. [Google Scholar] [CrossRef]
- Gonzalez, J.R.; Moreno, V. SNPassoc: SNPs-Based Whole Genome Association Studies. R Package Version 2.0-1. Available online: https://CRAN.R-project.org/package=SNPassoc (accessed on 30 September 2021).
- Sinnwell, J.P.; Schaid, D. Haplo.stats: Statistical Analysis of Haplotypes with Traits and Covariates when Linkage Phase is Ambiguous. R Package Version 1.8.6. Available online: https://CRAN.R-project.org/package=haplo.stats (accessed on 30 September 2021).
- Gurdol, F.; Yurdum, L.M.; Ozturk, U.; Isbilen, E.; Cakmakoglu, B. Association of the CC chemokine receptor 5 (CCR5) polymorphisms with preeclampsia in Turkish women. Arch. Gynecol. Obstet. 2012, 286, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Magiełda-Stola, J.; Kurzawińska, G.; Ożarowski, M.; Karpiński, T.M.; Drews, K.; Seremak-Mrozikiewicz, A. The Significance of VDR Genetic Polymorphisms in the Etiology of Preeclampsia in Pregnant Polish Women. Diagnostics 2021, 11, 1698. [Google Scholar] [CrossRef]
- Magiełda-Stola, J.; Kurzawińska, G.; Ożarowski, M.; Bogacz, A.; Wolski, H.; Drews, K.; Karpiński, T.M.; Wolek, M.; Seremak-Mrozikiewicz, A. Placental mRNA and Protein Expression of VDR, CYP27B1 and CYP2R1 Genes Related to Vitamin D Metabolism in Preeclamptic Women. Appl. Sci. 2021, 11, 11880. [Google Scholar] [CrossRef]
- Tabatabaee, F.A.G.; Vasudevan, R.; Heidari, F.; Khazaei, S. Association of MMP-1, 9, 12 and TIMP-1 gene polymorphisms in Malaysian male hypertensive subjects. BioMed Res. Int. 2018, 29, 1734–1742. [Google Scholar]
- Rahimi, Z.; Kazemian, L.; Malek-Khosravi, S.; Najafi, F.; Rahimi, Z. Matrix metalloproteinase-7 A-181G and its interaction with matrix metalloproteinase-9 C-1562T polymorphism in preeclamptic patients: Association with malondialdehyde level and severe preeclampsia. Arch. Gynecol. Obstet. 2015, 291, 45–51. [Google Scholar] [CrossRef]
- Palei, A.C.T.; Sandrim, V.C.; Amaral, L.M.; Machado, J.S.R.; Cavalli, R.C.; Lacchini, R.; Duarte, G.; Tanus-Santos, J.E. Effects of matrix metalloproteinase (MMP)-2 polymorphisms on responsiveness to antihypertensive therapy of women with hypertensive disorders of pregnancy. Basic Clin. Pharmacol. Toxicol. 2012, 111, 262–267. [Google Scholar] [CrossRef]
- Fraser, R.; Walker, J.J.; Ekbote, U.V.; Martin, K.L.; McShane, P.; Orsi, N.M. Interleukin-4 -590 (C > T), toll-like receptor-2 + 2258 (G > A) and matrix metalloproteinase-9 -1562 (C > T) polymorphisms in pre-eclampsia. BJOG Int. J. Obstet. Gynaecol. 2008, 115, 1052–1056. [Google Scholar] [CrossRef]
- Jurajda, M.; Kanková, K.; Muzik, J.; Unzeitig, V.; Drábková, M.; Izakovičová-Hollá, L.; Vácha, J. Lack of an association of a single nucleotide polymorphism in the promoter of the matrix metalloproteinase-1 gene in Czech women with pregnancy-induced hypertension. Gynecol. Obstet. Investig. 2001, 52, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Atkinson, S.; Murphy, G. Identification of the Extracellular Matrix (ECM) binding motifs of tissue inhibitor of metalloproteinases (TIMP)-3 and effective transfer to TIMP-1. J. Biol. Chem. 2007, 282, 6887–6898. [Google Scholar] [CrossRef] [PubMed]
- Löffek, S.; Schilling, O.; Franzke, C.W. Series “matrix metalloproteinases in lung health and disease”: Biological role of matrix metalloproteinases: A critical balance. Eur. Respr. J. 2011, 38, 191–208. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.X.; Yang, Q.D.; Liu, B.Q.; Zhang, L.; Ma, M.M.; Hu, Z.Y.; Xia, J.; Xu, H.W.; Du, X.P. TIMP-1 polymorphisms in a Chinese Han population with intracerebral hemorrhage. Int. J. Neurosci. 2014, 124, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Luizon, M.R.; Palei, A.C.; Sandrim, V.C.; Amaral, L.M.; Machado, J.S.R.; Lacchini, R.; Cavalli, R.C.; Duarte, G.; Tanus-Santos, J.E. Tissue inhibitor of matrix metalloproteinase-1 polymorphism, plasma TIMP-1 levels, and antihypertensive therapy responsiveness in hypertensive disorders of pregnancy. Pharm. J. 2014, 14, 535–541. [Google Scholar] [CrossRef]

| Gene | MMP1 | MMP9 | TIMP1 | TIMP2 | ||
|---|---|---|---|---|---|---|
| rs number | rs1799750 | rs17576 | rs17577 | rs4898 | rs2277698 | rs55743137 |
| Chromosome position (GRCh38.p12) | chr11:102799765-102799766 | chr20:46011586 | chr20:46014472 | chrX:47585586 | chr17:78870935 | chr17:78871103 |
| Traditional name | −1607 1G/2G | 836A > G | 2003G > A | 372T > C | 303C > T | — |
| Genomic positions * | NG_011740.2: g.3471del | NG_011468.1: g.7679A > G | NG_011468.1: g.10565G > A | NG_012533.1: g.8296T > C | NC_000017.11: g.78870935C > T | NC_000017.11: g.78871103G > T |
| Alleles | delC | A > G | G > A | T > C | C > T | G > T |
| Amino acid change | none | Q279R | R668Q | F124= | S101= | none |
| Location in gene | 2 KB Upstream Variant | Exon 6 | Exon 12 | Exon 5 | Exon 3 | Intron 2 |
| Gene rs Number | Primer Sequence | Amplicon Size | Restriction Enzyme | RFLP Product Size |
|---|---|---|---|---|
| MMP1 rs1799750 | 5′-TGACTTTTAAAACATAGTCTATGTTCA-3′ 5′-TCTTGGATTGATTTGAGATAAGTCATAGC-3′ | 269 bp | AluI | 1G 241, 28 bz 2G 269 bz |
| MMP9 rs17576 | 5′-GAGAGATGGGATGAACTG-3′ 5′-GTGGTGGAAATGTGGTGT-3′ | 439 bp | MspI | A 252, 187 bz G 187, 129, 123 bz |
| MMP9 rs17577 | 5′-ACACGCACGACGTCTTCCAGTATC-3′ 5′-GGGGCATTTGTTTCCATTTCCA-3′ | 138 bp | TaqI | G 115, 23 bz A 138 bz |
| TIMP1 rs4898 | 5′-GCACATCACTACCTGCAGTCT-3′ 5′-GAA ACA AGC CCA CGA TTT AG-3′ | 175 bz | BauI (BssSI) | T 175 bz C 153, 22 bz |
| TIMP2 rs2277698 | 5′-CCAGGAAATTGGCAGGTAGT-3′ 5′-GAATTCACCAACTGTGTGGC-3′ | 369 bz | BsrI | C 369 bz T 231, 138 bz |
| TIMP2 rs55743137 | 5′-CCTTTGAACATCTGGAAAGACAA-3′ 5′-TAACCCATGTATTTGCACTTCCT-3′ | 160 bz | AluI | T 160 pz G 108, 52 bz |
| Variables | PE (n = 115) | Controls (n = 193) | p | EOPE (n = 55) | LOPE (n = 60) | p |
|---|---|---|---|---|---|---|
| Maternal age (years) | 30.32 ± 5.32 | 31.06 ± 3.89 | 0.2019 | 30.11 ± 5.22 | 30.53 ± 5.45 | 0.6782 |
| Gestational age (weeks) | 33.69 ± 3.58 | 38.97 ± 1.09 | <0.001 | 30.56 ± 2.10 | 36.61 ± 1.71 | <0.001 |
| Systolic blood pressure (mmHg) | 171.71 ± 18.63 | 104.56 ± 10.85 | <0.001 | 175.64 ± 19.51 | 168.05 ± 17.15 | 0.0335 |
| Diastolic blood pressure (mmHg) | 106.80 ± 12.81 | 66.01 ± 7.77 | <0.001 | 107.34 ± 13.53 | 106.20 ± 12.18 | 0.6157 |
| Pre-pregnancy BMI (kg/m2) | 25.17 ± 5.83 | 21.00 ± 2.50 | <0.001 | 24.99 ± 4.67 | 25.34 ± 6.74 | 0.7534 |
| Post-pregnancy BMI (kg/m2) | 30.48 ± 5.27 | 26.17 ± 2.94 | <0.001 | 30.16 ± 4.12 | 30.78 ± 6.16 | 0.5225 |
| Caesarean section, N (%) | 104 (90.43) | 65 (33.68) | <0.001 * | 54 (98.18) | 50 (83.33) | 0.009 # |
| Primipara, N (%) | 69 (60.00) | 22 (11.40) | <0.001 * | 33 (60.00) | 36 (60.00) | 1.000 * |
| Infant sex—girl N (%) | 59 (51.30) | 81 (41.97) | 0.1117 * | 28 (50.91) | 31 (51.67) | 0.9203 * |
| Infant birthweight (g) | 1892.97 ± 857.63 | 3467.46 ± 409.17 | <0.001 | 1323.15 ± 426.30 | 2442.81 ± 809.98 | <0.001 |
| Apgar score at 1 min | 7.35 ± 2.70 | 9.87 ± 0.47 | <0.001 | 6.11 ± 2.62 | 8.54 ± 2.21 | <0.001 |
| Apgar score at 5 min | 8.58 ± 1.54 | 9.98 ± 0.13 | <0.001 | 7.85 ± 1.63 | 9.29 ± 1.06 | <0.001 |
| Placenta weight (g) | 423.53 ± 162.68 | 611.30 ± 113.43 | <0.001 | 325.64 ± 100.41 | 517.65 ± 155.88 | <0.001 |
| Variables | All PE Women (n = 115) | EOPE (n = 55) | LOPE (n = 60) | p EOPE vs. LOPE |
|---|---|---|---|---|
| Urea (mg/dL) | 30.23 ± 13.62 | 32.11 ± 13.58 | 28.45 ± 13.52 | 0.1577 |
| Uremic acid (mg/dL) | 6.49 ± 1.33 | 6.74 ± 1.50 | 6.26 ± 1.10 | 0.0593 |
| Total protein (g/dL) | 5.67 ± 0.71 | 5.47 ± 0.57 | 5.85 ± 0.78 | 0.0049 |
| Creatinine (mg/dL) | 0.75 ± 0.21 | 0.81 ± 0.26 | 0.69 ± 0.11 | 0.0919 |
| Proteinuria (mg/dL) | 279.79 ± 193.69 | 369.96 ± 181.79 | 194.37 ± 164.78 | <0.001 |
| ALT, U/L | 35.33 ± 43.42 | 50.69 ± 56.75 | 20.99 ± 17.98 | 0.0803 |
| AST, IU/L | 36.07 ± 38.62 | 48.46 ± 50.81 | 24.51 ± 17.01 | 0.1131 |
| Proteinuria, g/24 h | 3.72 ± 3.27 | 4.86 ± 2.77 | 2.49 ± 3.42 | 0.0499 |
| SNP | Alleles | HWE p | OR (95%CI) | p | Allele Frequency in European Population * | |
|---|---|---|---|---|---|---|
| MMP1 rs1799750 | 1G | 2G | ||||
| PE | 113 (0.491) | 117 (0.508) | 0.960 | 1.274 (0.919–1.768) | 0.145 | 1G = 0.4960 2G = 0.5040 |
| control | 213 (0.551) | 173 (0.448) | 0.997 | |||
| MMP9 rs17576 | A | G | ||||
| PE | 143 (0.621) | 87 (0.378) | 0.622 | 1.157 (0.824–1.624) | 0.398 | A = 0.6193 G = 0.3807 |
| control | 253 (0.655) | 133 (0.344) | 0.616 | |||
| MMP9 rs17577 | G | A | ||||
| PE | 289 (0.821) | 41 (0.178) | 0.103 | 1.305 (0.839–2.031) | 0.236 | G = 0.8250 A = 0.1750 |
| control | 331 (0.857) | 55 (0.142) | 0.471 | |||
| TIMP1 rs4898 | T | C | ||||
| PE | 108 (0.469) | 122 (0.531) | 0.971 | 1.129 (0.814–1.566) | 0.464 | T = 0.535 C = 0.465 |
| control | 193 (0.500) | 193 (0.500) | 0.319 | |||
| TIMP2 rs2277698 | C | T | ||||
| PE | 196 (0.852) | 34 (0.147) | 0.545 | 0.980 (0.62–1.552) | 0.999 | C = 0.8748 T = 0.1252 |
| control | 328 (0.849) | 58 (0.151) | 0.651 | |||
| TIMP2 rs55743137 | T | G | ||||
| PE | 181 (0.786) | 49 (0.213) | 0.992 | 1.222 (0.812–1.838) | 0.343 | T = 0.8002 G = 0.1998 |
| control | 316 (0.818) | 70 (0.181) | 0.523 | |||
| SNP | Genotypes | PE (n = 115) | Control (n = 193) | OR (95%CI) | p-Value | * p-Value |
|---|---|---|---|---|---|---|
| MMP1 rs1799750 | 1G/1G | 27 (0.235) | 59 (0.305) | 1.00 | 0.3332 | 0.3455 |
| 1G/2G | 59 (0.513) | 95 (0.492) | 0.74 (0.42–1.29) | |||
| 2G/2G | 29 (0.252) | 39 (0.202) | 0.62 (0.32–1.19) | |||
| Dominant | 88 (0.765) | 134 (0.694) | 0.70 (0.41–1.18) | 0.1762 | 0.1548 | |
| Recessive | 86 (0.748) | 154 (0.798) | 0.75 (0.43–1.30) | 0.3080 | 0.4482 | |
| MMP9 rs17576 | AA | 42 (0.365) | 86 (0.446) | 1.00 | 0.2731 | 0.7135 |
| AG | 59 (0.513) | 81 (0.420) | 0.67 (0.41–1.10) | |||
| GG | 14 (0.122) | 26 (0.134) | 0.91 (0.43–1.91) | |||
| Dominant | 73 (0.635) | 107 (0.554) | 0.72 (0.45–1.15) | 0.1649 | 0.4127 | |
| Recessive | 101 (0.878) | 167 (0.865) | 1.12 (0.56–2.25) | 0.7422 | 0.8464 | |
| MMP9 rs17577 | GG | 81 (0.704) | 144 (0.746) | 1.00 | 0.4329 | 0.2268 |
| GA | 27 (0.235) | 43 (0.223) | 0.90 (0.52–1.56) | |||
| AA | 7 (0.061) | 6 (0.031) | 0.48 (0.16–1.48) | |||
| Dominant | 34 (0.296) | 49 (0.254) | 0.81 (0.48–1.36) | 0.4260 | 0.1754 | |
| Recessive | 108 (0.939) | 187 (0.969) | 0.50 (0.16–1.51) | 0.2171 | 0.1495 | |
| TIMP1 rs4898 | CC | 33 (0.287) | 43 (0.223) | 1.00 | 0.4046 | 0.7358 |
| TC | 56 (0.487) | 107 (0.554) | 1.47 (0.84–2.56) | |||
| TT | 26 (0.226) | 43 (0.223) | 1.27 (0.65–2.47) | |||
| Dominant | 82 (0.713) | 150 (0.777) | 1.40 (0.83–2.38) | 0.2093 | 0.4965 | |
| Recessive | 89 (0.774) | 150 (0.777) | 0.98 (0.56–1.71) | 0.9466 | 0.8806 | |
| TIMP2 rs2277698 | CC | 85 (0.739) | 141 (0.731) | 1.00 | 0.9590 | 0.8303 |
| CT | 26 (0.226) | 46 (0.238) | 1.07 (0.61–1.85) | |||
| TT | 4 (0.035) | 6 (0.031) | 0.90 (0.25–3.30) | |||
| Dominant | 30 (0.261) | 52 (0.269) | 1.04 (0.62–1.76) | 0.8693 | 0.8443 | |
| Recessive | 111 (0.965) | 187 (0.969) | 0.89 (0.25–3.22) | 0.8602 | 0.6292 | |
| TIMP2 rs55743137 | TT | 71 (0.617) | 127 (0.658) | 1.00 | 0.4767 | 0.5195 |
| TG | 39 (0.339) | 62 (0.321) | 0.89 (0.54–1.46) | |||
| GG | 5 (0.043) | 4 (0.021) | 0.45 (0.12–1.72) | |||
| Dominant | 44 (0.383) | 66 (0.342) | 0.84 (0.52–1.35) | 0.4724 | 0.3917 | |
| Recessive | 110 (0.957) | 189 (0.979) | 0.47 (0.12–1.77) | 0.2609 | 0.3510 |
| SNP | Genotypes/Models | Controls (n = 193) n (%) | EOPE (n = 55) n (%) | LOPE (n = 60) n (%) | EOPE vs. Control | LOPE vs. Control | EOPE vs. LOPE | |||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | p | OR (95%CI) | p | OR (95%CI) | p | |||||
| MMP1 rs1799750 | 1G/1G | 59 (0.305) | 12 (0.218) | 15 (0.250) | 1.00 | 0.4297 | 1.00 | 0.5095 | 1.00 | 0.8007 |
| 1G/2G | 95 (0.492) | 30 (0.545) | 29 (0.483) | 0.64 (0.31–1.36) | 0.83 (0.41–1.68) | 1.29 (0.52–3.23) | ||||
| 2G/2G | 39 (0.202) | 13 (0.236) | 16 (0.267) | 0.61 (0.25–1.48) | 0.62 (0.28–1.40) | 1.02 (0.35–2.92) | ||||
| Dominant | 134 (0.694) | 43 (0.782) | 45 (0.750) | 0.63 (0.31–1.29) | 0.1963 | 0.76 (0.39–1.46) | 0.4024 | 1.19 (0.50–2.84) | 0.6873 | |
| Recessive | 154 (0.798) | 42 (0.764) | 44 (0.733) | 0.82 (0.40–1.67) | 0.5855 | 0.70 (0.36–1.36) | 0.2974 | 0.85 (0.37–1.98) | 0.7083 | |
| MMP9 rs17576 | AA | 86 (0.446) | 21 (0.382) | 21 (0.350) | 1.00 | 0.1841 | 1.00 | 0.4137 | 1.00 | 0.2929 |
| AG | 81 (0.420) | 30 (0.545) | 29 (0.483) | 0.66 (0.35–1.24) | 0.68 (0.36–1.29) | 0.97 (0.44–2.13) | ||||
| GG | 26 (0.134) | 4 (0.073) | 10 (0.167) | 1.59 (0.50–5.04) | 0.63 (0.27–1.52) | 2.50 (0.68–9.25) | ||||
| Dominant | 107 (0.554) | 34 (0.618) | 39 (0.650) | 0.77 (0.42–1.42) | 0.3976 | 0.67 (0.37–1.22) | 0.1874 | 1.15 (0.54–2.45) | 0.7234 | |
| Recessive | 167 (0.865) | 51 (0.927) | 50 (0.833) | 1.99 (0.66–5.95) | 0.1908 | 0.78 (0.35–1.72) | 0.5422 | 2.55 (0.75–8.67) | 0.1176 | |
| MMP9 rs17577 | GG | 144 (0.746) | 40 (0.727) | 41 (0.683) | 1.00 | 0.7361 | 1.00 | 0.4283 | 1.00 | 0.8727 |
| GA | 43 (0.223) | 12 (0.218) | 15 (0.250) | 1.00 (0.48–2.06) | 0.82 (0.41–1.62) | 1.22 (0.51–2.93) | ||||
| AA | 6 (0.031) | 3 (0.055) | 4 (0.067) | 0.56 (0.13–2.32) | 0.43 (0.12–1.59) | 1.30 (0.27–6.18) | ||||
| Dominant | 49 (0.254) | 15 (0.273) | 19 (0.317) | 0.91 (0.46–1.78) | 0.7791 | 0.73 (0.39–1.38) | 0.3436 | 1.24 (0.55–2.76) | 0.6056 | |
| Recessive | 187 (0.969) | 52 (0.945) | 56 (0.933) | 0.56 (0.13–2.30) | 0.4338 | 0.45 (0.12–1.65) | 0.2433 | 1.24 (0.26–5.80) | 0.7855 | |
| TIMP1 rs4898 | CC | 43 (0.223) | 19 (0.345) | 14 (0.233) | 1.00 | 0.1426 | 1.00 | 0.4109 | 1.00 | 0.1059 |
| TC | 107 (0.554) | 28 (0.509) | 28 (0.467) | 1.69 (0.85–3.34) | 1.24 (0.60–2.59) | 1.36 (0.57–3.23) | ||||
| TT | 43 (0.223) | 8 (0.145) | 18 (0.300) | 2.38 (0.94–6.01) | 0.78 (0.34–1.76) | 3.05 (1.04–9.01) | ||||
| Dominant | 150 (0.777) | 36 (0.655) | 46 (0.767) | 1.84 (0.96–3.53) | 0.0706 | 1.06 (0.53–2.11) | 0.8645 | 1.73 (0.77–3.92) | 0.1839 | |
| Recessive | 150 (0.777) | 47 (0.855) | 42 (0.700) | 1.68 (0.74–3.83) | 0.1968 | 1.50 (0.78–2.86) | 0.2298 | 2.52 (0.99–6.39) | 0.0452 | |
| TIMP2 rs2277698 | CC | 141 (0.731) | 39 (0.709) | 46 (0.767) | 1.00 | 0.7759 | 1.00 | 0.5628 | 1.00 | |
| CT | 46 (0.238) | 15 (0.273) | 11 (0.183) | 0.85 (0.43–1.68) | 1.36 (0.65–2.85) | 0.62 (0.26–1.51) | 0.3635 | |||
| TT | 6 (0.031) | 1 (0.018) | 3 (0.050) | 1.66 (0.19–14.20) | 0.65 (0.16–2.71) | 2.54 (0.25–25.45) | ||||
| Dominant | 52 (0.269) | 16 (0.291) | 14 (0.233) | 0.90 (0.46–1.74) | 0.7538 | 1.21 (0.62–2.39) | 0.5749 | 0.74 (0.32–1.71) | 0.4825 | |
| Recessive | 187 (0.969) | 54 (0.982) | 57 (0.950) | 1.73 (0.20–14.70) | 0.5923 | 0.61 (0.15–2.52) | 0.5059 | 2.84 (0.29–28.17) | 0.3401 | |
| TIMP2 rs55743137 | TT | 127 (0.658) | 32 (0.582) | 39 (0.650) | 1.00 | 0.5588 | 1.00 | 0.2457 | 1.00 | |
| TG | 62 (0.321) | 22 (0.400) | 17 (0.283) | 0.71 (0.38–1.32) | 1.12 (0.59–2.14) | 0.63 (0.29–1.39) | 0.2183 | |||
| GG | 4 (0.021) | 1 (0.018) | 4 (0.067) | 1.01 (0.11–9.33) | 0.31 (0.07–1.29) | 3.28 (0.35–30.85) | ||||
| Dominant | 66 (0.342) | 23 (0.418) | 21 (0.350) | 0.72 (0.39–1.33) | 0.3022 | 0.97 (0.53–1.77) | 0.9090 | 0.75 (0.35–1.59) | 0.4524 | |
| Recessive | 189 (0.979) | 54 (0.982) | 56 (0.933) | 1.14 (0.13–10.44) | 0.9046 | 0.30 (0.07–1.22) | 0.1011 | 3.86 (0.42-35.62) | 0.1863 | |
| Frequencies | PE vs. Controls | EOPE vs. Controls | LOPE vs. Controls | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Haplotype | Controls | PE | EOPE | LOPE | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| MMP9 loci rs17576 and rs17577 | ||||||||||
| AG | 0.652 | 0.608 | 0.645 | 0.575 | 0.827 (0.59–1.159) | 0.270 | 0.968 (0.621–1.508) | 0.885 | 0.719 (0.473–1.092) | 0.121 |
| GG | 0.204 | 0.213 | 0.190 | 0.233 | 1.052 (0.704–1.57) | 0.804 | 0.916 (0.536–1.567) | 0.751 | 1.182 (0.724–1.93) | 0.501 |
| GA | 0.139 | 0.165 | 0.154 | 0.175 | 1.216 (0.774–1.911) | 0.393 | 1.123 (0.621–2.03) | 0.698 | 1.304 (0.751–2.264) | 0.334 |
| TIMP2 loci rs2277698 and rs55743137 | ||||||||||
| CT | 0.803 | 0.786 | 0.781 | 0.791 | 0.905 (0.605–1.355) | 0.629 | 0.878 (0.523–1.473) | 0.623 | 0.931 (0.561–1.546) | 0.784 |
| TG | 0.134 | 0.147 | 0.154 | 0.141 | 1.114 (0.698–1.777) | 0.649 | 1.174 (0.648–2.126) | 0.595 | 1.06 (0.587–1.913) | 0.846 |
| CG | 0.046 | 0.065 | 0.063 | 0.066 | 1.426 (0.704–2.888) | 0.321 | 1.389 (0.564–3.417) | 0.472 | 1.46 (0.618–3.448) | 0.385 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mrozikiewicz, A.E.; Kurzawińska, G.; Goździewicz-Szpera, A.; Potograbski, M.; Ożarowski, M.; Karpiński, T.M.; Barlik, M.; Jędrzejczak, P.; Drews, K. Effects of TIMP1 rs4898 Gene Polymorphism on Early-Onset Preeclampsia Development and Placenta Weight. Diagnostics 2022, 12, 1637. https://doi.org/10.3390/diagnostics12071637
Mrozikiewicz AE, Kurzawińska G, Goździewicz-Szpera A, Potograbski M, Ożarowski M, Karpiński TM, Barlik M, Jędrzejczak P, Drews K. Effects of TIMP1 rs4898 Gene Polymorphism on Early-Onset Preeclampsia Development and Placenta Weight. Diagnostics. 2022; 12(7):1637. https://doi.org/10.3390/diagnostics12071637
Chicago/Turabian StyleMrozikiewicz, Aleksandra E., Grażyna Kurzawińska, Agata Goździewicz-Szpera, Michał Potograbski, Marcin Ożarowski, Tomasz M. Karpiński, Magdalena Barlik, Piotr Jędrzejczak, and Krzysztof Drews. 2022. "Effects of TIMP1 rs4898 Gene Polymorphism on Early-Onset Preeclampsia Development and Placenta Weight" Diagnostics 12, no. 7: 1637. https://doi.org/10.3390/diagnostics12071637
APA StyleMrozikiewicz, A. E., Kurzawińska, G., Goździewicz-Szpera, A., Potograbski, M., Ożarowski, M., Karpiński, T. M., Barlik, M., Jędrzejczak, P., & Drews, K. (2022). Effects of TIMP1 rs4898 Gene Polymorphism on Early-Onset Preeclampsia Development and Placenta Weight. Diagnostics, 12(7), 1637. https://doi.org/10.3390/diagnostics12071637








