Abstract
Objective: The aim of this systematic review was to determine whether rapid maxillary expansion (RME) allows favorable changes in the mandible during the treatment of class II malocclusion before the growth spurt. Methods: A search of Pubmed/Medline, the Science Direct, and the Google Scholar database was performed. The keywords used were: orthodontics, rapid maxillary expansion, class II, and growing patients. Relevant articles were assessed for quality according to Cochrane guidelines, and then changes in SNA, SNB, ANB, NL-NSL (or SN-SNP.SNA), and ML-NSL (or SN-Go-Gn) relationships were analyzed. Results: The selection process brought forth five articles, including 162 patients (91 females, 71 males) for detailed analysis. The quality of the evidence (GRADE) for comparisons and outcomes was assessed as moderate for SNB and ANB and as low or very low for other variables. Conclusions: The results of this systematic review showed that there is a small body of moderate-quality evidence for statistically and clinically favorable changes in SNB and ANB angles and a small body of low-quality evidence for changes in vertical parameters after RME.
1. Introduction and Objectives
Since Angell [1] introduced rapid maxillary expansion (RME) in 1860, regardless of continuous modification of the appliances used for this purpose, RME still involves separation of the maxillary midpalatal suture [2] in patients up to 15–18 years of age, who are prone to undergo this procedure [3,4,5]. As evidenced by meta-analyses, RME successfully corrects unilateral and bilateral crossbites and sagittal maxillary deficiencies, mainly in combination with maxillary protraction devices and/or a chin cap [6,7].
In addition to the objective evidence of RME effects on the maxilla [8], the literature also provides information about the beneficial RME effects on the mandible [9] (without overload of temporo-mandibular joints), which is expressed as a reduction in the facial vertical dimension and as a spontaneous class II correction [10,11].
Regardless of the scientific evidence for differences in RME achieved with bonded or banded hyrax screw [12], this issue is omitted in the literature, in either retrospective stud-ies [13], as well in systematic reviews [14] or meta-analyses [15].
Furthermore, notwithstanding a rigorous assessment of either the impartiality of the publications or correct reporting, the published evidence either omits the duration of an observation or admits the variety of additional (other than RME) interventions, which challenges the homogeneity of the study groups [16].
Considering new publications that have appeared in the literature since 2015 [17,18,19,20,21,22,23,24,25,26] including randomized clinical trials (RCTs) with potential evidence quality, as well as the previously published papers [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48] requiring adequate data analysis, we designed our systematic review to reject two null hypotheses: 1. RME applied in growing patients does not induce stable vertical and sagittal changes that favor class II treatment; 2. the achieved changes do not depend on banding or bonding of HS.
2. Material and Methods
This systematic review was registered at PROSPERO (CRD42020184895). By performing the PRISMA protocol and following recommendations from the Cochrane Handbook for Systematic Reviews of Interventions, we defined the main research questions in PICO format (Table 1).

Table 1.
PICO format.
2.1. Search Strategy
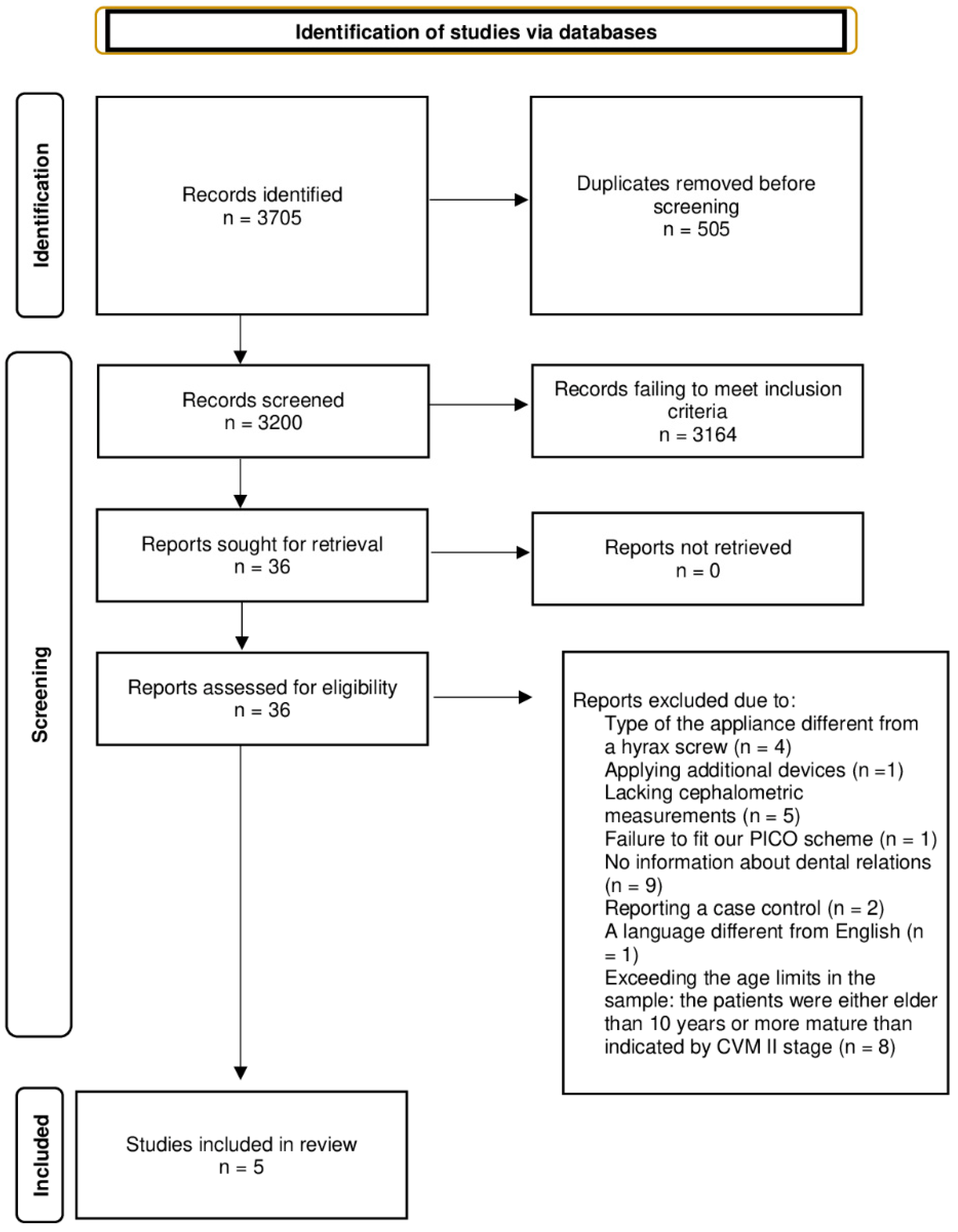
The search strategy of electronic databases Pubmed/Medline, Science Direct, and Google Scholar (1970 to December 2019) is shown in Table 2. The entire selection process is presented in the PRISMA diagram (Figure 1).

Table 2.
Search strategy.
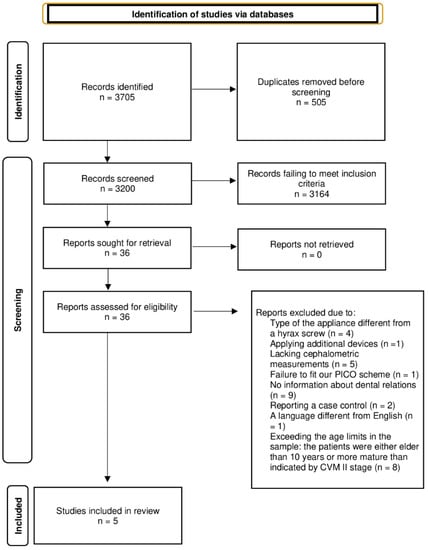
Figure 1.
PRISMA diagram.
2.2. Data Extraction
The remaining work was analyzed for suitability purposes within our study by two independent researchers (MK, KR). They downloaded the selected articles and contacted the authors of the papers if the data essential for our PICO format were missing. A lack of feedback either weakened a given article’s total score or excluded such a paper from our study. Experienced researchers (JL, BK, NK, and MS) independently verified the selection, and then the extracted data were compiled in a Microsoft Office Excel 2013 spreadsheet (Microsoft Corporation, Redmond, Washington, DC, USA); the level agreement was statistically evaluated with unweighted Cohen kappa statistics.
2.3. Quality Assessment
2.3.1. Risk of Bias
The Cochrane Collaboration tool for assessing risk of bias in RCTs as low, unclear, or high enabled us to evaluate random sequence generation, allocation concealment, blinding of participants and personnel, blinding of assessors, incomplete outcome data, and selective reporting of outcomes.
The quality of the CCTs was assessed with a modified Newcastle–Ottawa Scale, composed of three sections:
- Selection, evaluation of case definitions, representativeness of cases, control selection, and definition of controls. Each aspect was assigned 1 point, giving 4 points in total.
- Comparability, appraising SNA, SNB, ANB, NL-NSL (or SN-SNP.SNA), and ML-NSL (or SN-Go-Gn) as the main parameters and observation time as an additional parameter, giving 2 points in total.
- Outcome assessment, evaluation of outcome measures, duration of the follow-up, and blinding of assessors, giving 3 points in total.
2.3.2. Evidence
We used the scale of the GRADE Working Group; thus, we evaluated the analyzed papers as high, moderate, low, or very low quality in terms of supporting the confidence in the estimate.
3. Results
The demographic structure of the pooled patient sample extracted from the articles, together with the ranges of sagittal and vertical changes in the mandible after RME application, is shown in Table 3.

Table 3.
The composition of the study material.
3.1. Quality Assessment
3.1.1. Risk of Bias
The results of the risk of bias analysis in RCTs and in CCTs are presented in Table 4 and Table 5, respectively.

Table 4.
Assessment of the risk of bias in RCTs.

Table 5.
Assessment of the risk of bias in the CCTs.
3.1.2. Evidence
The quality of the evidence (GRADE) for comparisons and outcomes was moderate for SNB and ANB angles due to their statistically significant changes
Since an overall GRADE quality rating can be applied to a body of evidence across outcomes, usually by taking the lowest quality of evidence from all of the outcomes that are critical to decision making, we assessed our evidence as very low quality.
3.1.3. Outcomes
Changes in the sagittal and vertical parameters, and their dependence on a different mode of HS mounting, are shown in Table 6. For the papers encompassing control groups, an inter-group comparison was carried out. The synthesis of results was in turn impossible due to the small sample sizes, insufficient data provided, or discrepancies between the results in the analyzed papers.

Table 6.
Characteristics of post-RME changes in the sagittal and the vertical parameter values.
4. Discussion
There are reports in the literature regarding the rationale for using RME as an additional utility in class II treatment [33,42,49]. This rationale is based either on studies evaluating the morphology of the maxilla and the mandible, which turned out to be different in normal, distal, and mesial occlusions [50,51], or on reports regarding the lack of “self-correction” of distal occlusion during growth [52]. Improvements in the transverse dimension of the maxilla, which is narrowed in patients with class II [53,54,55,56], should facilitate both the protrusion and growth of the mandible, which fundamentally realizes the “foot to the shoe” concept [57]. This spontaneous class II correction, which is most often presented in studies evaluating dental relationships [33,58], is not supported by changes in the skeletal parameters analyzed in our study. Regarding the SNA angle, the body of evidence for all comparisons and outcomes was rated as very low quality. We found moderate-quality evidence for an increase in the SNB angle after 6 months of observation [30], suggesting the protrusion of the mandible, which follows the RME protocol. This study, however, involved children in whom changes in skeletal parameters resulted from growth; thus, a lack of comparison of the achieved changes with a control group challenges the reliability of the outcome. In turn, the comparable value of the SNB angle in the treated and control groups after a 4-year follow-up [34] may be related to the patients’ further development, namely, the CMS III phase, which is characterized by a significant increase in the mandible. A reduction in the ANB angle, also defined as a moderate quality of evidence, suggests both statistical and clinical improvements in class II malocclusion; nonetheless, it is the result of SNA changes and should also be treated with caution.
A statistically significant increase in the NL-NSL (or SN-SNP.SNA) angle, which is beneficial to the treatment of a class II open bite, occurred in one study [30], but had low-quality evidence caused by either the lack of a control group (fundamental in any research on growing patients) or the inability to compare the results with those of other studies. A statistically insignificant decrease in the ML-NSL (or SN-Go.Gn) angle in the one-year observation [20], clinically demonstrated as a counter-clockwise rotation of the mandible, regardless of a comparison with the control group, was assessed as evidence of a very low quality due to both the small number of patients and the discrepancies between the results.
A minor distal displacement of the mandible was the immediate effect of the banded RME. A decrease in the SNB angle may be related not only to the retraction of the mandible, but also to its clockwise rotation. In particular, a transverse overcorrection, i.e., raising the occlusion through contact of the palatal cusps of the maxillary teeth with the buccal cusps of their antagonists, resulted in a statistically significant increase in the ML-NSL (or SN-Go.Gn) angle in 28 patients [9]. This result, due to the occurrence in a single work and the small number of patients, was rated as very low quality evidence. On the other hand, the 6-month observation [30] theoretically allows us to conclude that the forward movement of the mandible is stable due to a statistically significant increase in the SNB angle and decrease in the ANB angle, regardless of the increase in the ML-NSL (or SN-Go.Gn) angle proving clockwise mandibular rotation. Nevertheless, due to the lack of comparison with the control group and due to the small number of studies and the patients analyzed, this information was considered as low-quality evidence.
There were discrepancies in the annual observations of the bonded HS effects [20,43]. Due to the minor changes in the SNA angle, the position of the maxilla was considered stable. A minor increase (comparing to control group) in the SNB angle allowed diagnosing a stable, statistically insignificant forward movement of the mandible. A statistically significant decrease in the ML-NSL (or SN-Go.Gn) angle, opposite to the increase recorded in the control group, allowed us to evaluate a clinically favorable counterclockwise rotation of the mandible [20]. Those outcomes were different to those reported by De Rossi et al. [43]; therefore, they were considered as very low quality evidence. A four-year follow-up [34] of the patients showed an insignificant decrease in the SNA angle after treatment, and its insignificant increase when compared with the control group. It brought low-quality evidence for a forward movement of the maxilla after RME application, compared to untreated patients. The lack of homogeneity of both the control and the intervention groups could have resulted in a comparable, but not statistically significant, increase in the SNB angle in the group treated with bonded HSs, as well as in the control group. It should be emphasized that the initial anterior–posterior position of the mandible was more favorable in the study group than in the control group, both at T1 and T3. The decrease in the ANB angle was twice as high in the study group than in the control group, but this change was statistically significant only in comparison with the initial situation.
As for the comparison of bonded and banded HS on the mandible, the differences in follow-ups presented do not allow for reliable evaluation, especially of the vertical changes. To do so, morphological changes in the mandible occurring post-RME treatment should be provided and thoroughly analyzed.
The body of evidence identified did not allow for an unequivocal determination of the skeletal changes after RME. Even if they were reproducible, these changes were assessed mainly on the basis of studies that were burdened with a medium risk of bias and involved only a few patients. Not all changes in the analyzed parameters could be compared with those in the control group, which made it difficult to draw conclusions. The works identified in this review also did not clearly determine the effect of the RME type on the mandible.
5. Potential Biases in the Review Process and Limitations
Any possible bias that could result from qualifying CCTs for this review was overcome using all possible methods for the objective selection of studies. An independent search, qualification for review, and risk of bias assessment were performed by two authors, and the dispute was resolved by an experienced researcher. Therefore, the main limitation of this work was the small number of qualified studies and the lack of representativeness of the groups. This is most likely due to the difficulty of achieving a homogeneous group of patients with only one form of intervention who were observed for an extended period of time during their growth.
6. Conclusions
Conclusions presented due to their insufficient value should be treated with caution. Based on this systematic review, the following can be suspected:
- As there is a small body of moderate-quality evidence for changes in the SNB angle caused by the RME, regardless of its type, and because those changes are similar to the spontaneous ones occurring in untreated patients after a 4-year follow-up, the first null hypothesis is sustained.
- Despite the fact that the effects of RME varied: counter-clockwise and clockwise rotation of the mandible following bonded and banded HS treatment, respectively, there is a small body of low-quality evidence; thus, the second null hypothesis is also sustained. Nevertheless, this systematic review could not include parameters demonstrating a changing morphology of the mandible, which are necessary for a reliable analysis and evaluation of the effect of bonded versus banded HSs on the mandible.
- The lowest and close to the lowest grades of studies according to GRADE highly suggest the necessity of conducting thoroughly planned and reported studies of not only angular, but also morphological parameters in order to reject our null hypotheses. Due to ethical contraindications for creating and observing a control group, we suggest using control groups selected from existing growth studies.
Author Contributions
Conceptualization, M.K., J.L.; methodology, M.K., J.L.; software, M.K.; validation, M.K., K.R. and N.K.; formal analysis, M.K.; investigation, M.K., K.R.; resources, M.K.; data curation, M.K., J.L.; writing—original draft preparation, M.K.; writing—review and editing, J.L., M.S.; visualization, M.K.; supervision, J.L., B.K. and M.S.; project administration, M.K.; funding acquisition, J.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Angel, E. Treatment of irregulatic of the permanent or adult teeth. Dent. C 1860, 1, 540–544. [Google Scholar]
- Haas, A.J. The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965, 16, 200–217. [Google Scholar]
- Wertz, R.A. Rapid expansion of the maxillary dental arch and nasal cavity by opening the mid-palatal suture. Angle Orthod. 1961, 31, 73–90. [Google Scholar]
- Haas, A.J. Palatal expansion: Just the beginning of dentofacial ortho- pedics. Am. J. Orthod. 1970, 57, 219–255. [Google Scholar] [CrossRef]
- Bishara, S.E.; Stale, R.N. Maxillary expansions: Clinical implications. Am. J. Orthod. Dentofacial. Orthop. 1987, 91, 3–14. [Google Scholar] [CrossRef]
- Zuccati, G.; Casci, S.; Doldo, T.; Clauser, C. Expansion of maxillary arches with crossbite: A systematic review of RCTs in the last 12 years. Eur. J. Orthod. 2013, 35, 29–37. [Google Scholar] [CrossRef]
- Rongo, R.; D’Anto, V.; Bucci, R.; Polito, I.; Martina, R.; Michelotti, A. Skeletal and dental effects of Class III orthopedic treatment: A systematic review and meta-analysis. J. Oral Rehabil. 2017, 44, 545–562. [Google Scholar] [CrossRef]
- Zhou, Y.; Long, H.; Ye, N.; Xue, J.; Yang, X.; Liao, L.; Lai, W. The effectiveness of non-surgical maxillary expansion: A meta-analysis. Eur. J. Orthod. 2014, 36, 233–242. [Google Scholar] [CrossRef]
- Abate, A.; Cavagnetto, D.; Rusconi, F.M.E.; Cressoni, P.; Esposito, L. Safety and Effects of the Rapid Maxillary Expander on Temporomandibular Joint in Subjects Affected by Juvenile Idiopathic Arthritis: A Retrospective Study. Children 2021, 8, 33. [Google Scholar] [CrossRef]
- Baccetti, T.; Franchi, L.; McNamara, J.; Tollaro, I. Early dentofacial features of Class II malocclusion: A longitudial study from the deciduous through the mixed dentition. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 502–509. [Google Scholar] [CrossRef]
- McNamara, J.A., Jr.; Brudon, W.L. Orthodontic and Orthopedic Treatment in the Mixed Dentition; Needham Press: Needham, MA, USA, 1993. [Google Scholar]
- Asanza, S.; Cisneros, G.J.; Nieberg, L.G. Comparison of Hyrax and bonded expansion appliances. Angle Orthod. 1997, 67, 15–22. [Google Scholar] [PubMed]
- Lanteri, V.; Abate, A.; Cavagnetto, D.; Ugolini, A.; Gaffuri, F.; Gianolio, A.; Maspero, C. Cephalometric Changes Following Maxillary Expansion with Ni-Ti Leaf Springs Palatal Expander and Rapid Maxillary Expander: A Retrospective Study. Appl. Sci. 2021, 11, 5748. [Google Scholar] [CrossRef]
- Lagravere, M.O.; Major, P.W.; Flores-Mir, C. Long-term Skeletal Changes with Rapid Maxillary Expansion: A Systematic Review. Angle Orthod. 2005, 75, 1046–1052. [Google Scholar]
- Lagravere, M.O.; Heo, G.; Major, P.W.; Flores-Mir, C. Meta-analysis of immediate changes with rapid maxillary expansion treatment. J. Am. Dent. Assoc. 2006, 137, 44–53. [Google Scholar] [CrossRef]
- Fernando, M.; Feres, M.F.N.; Hasnain, R.; Alhadlaq, A.; El-Bialy, T. Rapid maxillary expansion effects in Class II malocclusion: A systematic review. Angle Orthod. 2015, 85, 1070–1079. [Google Scholar]
- Pereira, J.; Jacob, B.H.; Locks, A.; Brunetto, M.; Ribeiro, G.L.U. Evaluation of the rapid and slow maxillary expansion using cone-beam computed tomography: A randomized clinical trial. Prog. Orthod. 2017, 22, 61–68. [Google Scholar] [CrossRef]
- Caprioglio, A.; Bergamini, C.; Franchi, L.; Vercellini, N.; Zecca, P.A.; Nucera, R.; Fastuca, R. Prediction of Class II improvement after rapid maxillary expansion in early mixed dentition. Prog. Orthod. 2017, 18, 9. [Google Scholar] [CrossRef]
- Conroy-Piskai, C.; Galang-Boquiren, M.T.; Obraz, A.; Costa Viana, M.G.; Oppermann, N.; Sanchez, F.; Edgren, B.; Kusnoto, B. Assessment of vertical changes during palatal expansion using quad helix or bonded rapid palatal expander. Angle Orthod. 2016, 86, 925–933. [Google Scholar] [CrossRef]
- Lione, R.; Brunelli, V.; Franchi, L.; Pavoni, C.; Souki, B.Q.; Cozza, P. Mandibular response after rapid maxillary expansion in class II growing patients: A pilot randomized controlled trial. Prog. Orthod. 2017, 18, 36. [Google Scholar] [CrossRef]
- Maspero, C.; Galbiati, G.; Giannini, L.; Farronato, G. Sagittal and vertical effects of transverse sagittal maxillary expander (TSME) in three different malocclusion groups. Prog. Orthod. 2015, 16, 6. [Google Scholar] [CrossRef]
- Giancotti, A.; Maselli, A.; Di Girolamo, R. Rapid Palatal Expansion in Treatment of Class II Malocclusions. Br. J. Orthod. 1999, 26, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Ugolini, A.; Cerruto, C.; Di Vece, L.; Ghislanzoni, L.H.; Sforza, C.; Doldo, T.; Silvestrini-Biavati, A.; Caprioglio, A. Dental arch response to Haas-type rapid maxillary expansion anchored to deciduous vs permanent molars: A multicentric randomized controlled trial. Angle Orthod. 2015, 85, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.N.; Chen, S.; Huang, C.Y.; Zhong, C.; Jin, J.; Yu, F.Y.; Zhang, Z.Z.; Lu, H.P. Comparison of the effects of rapid maxillary expansion versus Twin Block appliance on mandibular growth in skeletal Class II patients. Oral Health 2020, 20, 350. [Google Scholar] [CrossRef]
- Maspero, C.; Begnoni, G.; Magnani, A.; Farronato, M.; Khomchyna, N.; Dellavia, C. Rapid Maxillary Expander and Eruption Guidance Appliance therapy in skeletal Class II: Cephalometric considerations. Eur. J. Paediatr. Dent. 2019, 20, 4. [Google Scholar]
- Baldini, A.; Nota, A.; Santariello, C.; Caruso, S.; Assi, V.; Ballanti, F.; Gatto, R.; Cozza, P. Sagittal dentoskeletal modifications associated with different activation protocols of rapid maxillary expansion. Eur. J. Paediatr. Dent. 2018, 19, 151–155. [Google Scholar]
- Velazquez, P.; Benito, E.; Bravo, L.A. Rapid maxillary expansion. A study of the long-term effects. Am. J. Orthod. Dentofac. Orthop. 1996, 109, 361–367. [Google Scholar] [CrossRef]
- Chang, J.Y.; McNamara, J.A.; Herberger, T.A. A longitudinal study of skeletal side effects induced by rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 330–337. [Google Scholar] [CrossRef]
- Farronato, G.; Maspero, C.; Esposito, L.; Briguglio, E.; Farronato, D.; Giannini, L. Rapid maxillary expansion in growing patients. Hyrax versus transverse sagittal maxillary expander: A cephalometric investigation. Eur. J. Orthod. 2011, 33, 185–189. [Google Scholar] [CrossRef][Green Version]
- Farronato, G.; Giannini, L.; Galbiati, G.; Maspero, C. Sagittal and vertical effects of rapid maxillary expansion in Class I, II and III occlusions. Angle Orthod. 2011, 81, 298–303. [Google Scholar] [CrossRef]
- Baratieri, C.; Alves, M.; Sant’anna, E.F.; Nojima, M.C.G.; Nojima, L.I. 3D Mandibular Positioning After Rapid Rapid Maxillary Expansion in Class II Malocclusion. Braz. Dent. J. 2011, 22, 428–434. [Google Scholar] [CrossRef]
- Volk, T.; Sadowsky, C.; BeGole, E.; Boice, P. Rapid palatal expansion for spontaneous Class II correction. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 310–315. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A.; Sigler, L.; Franchi, L.; Guest, S.S.; Baccetti, T. Changes in Occlusal Relationships in Mixed Dentition Patients Treated with Rapid Maxillary Expansion. A Prospective Clinical Study. Angle Orthod. 2010, 80, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Guest, S.; McNamara, J.A.; Baccetti, T.; Franchi, L. Improving Class II malocclusion as a side-effect of rapid maxillary expansion: A prospective clinical study. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 582–591. [Google Scholar] [CrossRef]
- Lima Filho, R.M.A.; de Oliveira Ruellas, A.C. Long-term maxillary changes in patients with skeletal Class II malocclusion treated with slow and rapid palatal expansion. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Lambot, T.; Van Steenberghe, P.R.; Vanmuylder, N.; De Maertelaer, V.; Glineur, R. Traitement précoce d'expansion transversale par disjoncteur palatin et par 3D Quad Action mandibular appliance: Évaluation d'une approche globale sur 22 patients. Orthod Fr. 2008, 79, 107–114. [Google Scholar] [CrossRef]
- Lagravere, M.O.; Carey, J.; Heo, G.; Toogood, R.W.; Major, P.W. Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: A randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 304.e1–304.e12. [Google Scholar] [CrossRef]
- Cozza, P.; Giancotti, A.; Petrosino, A. Rapid Palatal Expansion in Mixed Dentition Using a Modified Expander: A Cephalometric Investigation. J. Orthod. 2001, 28, 129–134. [Google Scholar] [CrossRef]
- Ballanti, F.; Lione, R.; Fanucci, E.; Franchi, L.; Baccetti, T.; Cozza, P. Immediate and Post-Retention Effects of Rapid Maxillary Expansion Investigated by Computed Tomography in Growing Patients. Angle Orthod. 2009, 79, 24–29. [Google Scholar] [CrossRef]
- Da Silva Filho, O.G.; Boas, M.C.; Filho, L.C. Rapid maxillary expansion in the primary and mixed dentitions: A cephalometric evaluation. Am. J. Orthod. Dentofac. Orthop. 1991, 100, 171–181. [Google Scholar]
- Garib, D.G.; Henriques, J.C.; Carvalho, P.E.G.; Gomes, S.C. Longitudinal Effects of Rapid Maxillary Expansion. A Retrospective Cephalometric Study. Angle Orthod. 2007, 77, 3. [Google Scholar] [CrossRef]
- Wendling, L.K.; McNamara, J.A., Jr.; Franchi, L.; Baccetti, T. A Prospective Study of the Short-term Treatment Effects of the Acrylic-splint Rapid Maxillary Expander Combined with the Lower Schwarz Appliance. Angle Orthod. 2004, 75, 7–14. [Google Scholar]
- DeRossi, M.; DeRossi, A.; Abrao, J. Skeletal Alternations Associated with the Use of Bonded Rapid Maxillary Expansion Appliance. Braz. Dent. J. 2011, 22, 334–339. [Google Scholar]
- Perillo, L.; De Rossa, A.; Iaselli, F.; D’Apuzzo, F.; Grassia, V.; Cappabianca, S. Comparison between rapid and mixed maxillary expansion through an assessment of dento-skeletal effects on posteroanterior cephalometry. Prog. Orthod. 2014, 18, 46. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gianolio, A.; Cherchi, C.; Lanteri, V. Rapid and slow maxillary expansion: A posteroanterior cephalometric study. Eur. J. Paediatr. Dent. 2014, 15, 415–418. [Google Scholar]
- Wissheimer, A.; de Menezes, L.M.; Mezomo, M.; Dias, D.M.; de Lima, E.M.S.; Rizzatoo, S.M.D. Immediate effects of rapid maxillary expansion with Haas-type and hyrax-type expanders: A randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 366–376. [Google Scholar] [CrossRef]
- Akkaya, S.; Lorenzon, S.; Ucem, T.T. A comparison of sagittal and vertical effects between bonded rapid and slow maxillary expansion procedures. Eur. J. Orthod. 1999, 21, 175–180. [Google Scholar] [CrossRef]
- Sandlk, M.; Hazar, S. Skeletal and dental changes after maxillary expansion in the mixed dentition. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 321–327. [Google Scholar]
- Lima Filho, R.M.A.; Lima, A.C.; De Oliveira Ruellas, A.C.O. Spontaneous correction of Class II malocclusion after rapid palatal expansion. Angle Orthod. 2003, 73, 745–752. [Google Scholar]
- Franchi, L.; Baccetti, T. Transverse maxillary deficiency in Class II and Class III malocclusions: A cephalometric and morphometric study on postero-anterior films. Orthod. Craniofac. Res. 2005, 8, 21–28. [Google Scholar] [CrossRef]
- Pancherz, H.; Zieber, K.; Hoyer, B. Cephalometric characteristics of Class II division 1 and Class II division 2 malocclusions: A comparative study in children. Angle Orthod. 1997, 67, 111–120. [Google Scholar]
- Bishara, S.E.; Bayati, P.; Jakobsen, J.R. Longitudinal comparisons of dental arch changes in normal and untreated Class II, division 1 subjects and their clinical implications. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 483–489. [Google Scholar] [CrossRef]
- Will, L.A. Transverse maxillary deformities: Diagnosis and treatment. Oral Maxillofac. Surg. 1996, 5, 1–28. [Google Scholar]
- Tollaro, I.; Baccetti, T.; Franchi, L.; Tanasescu, C.D. Role of posterior transverse interarch discrepancy in Class II, division 1 malocclusion during the mixed dentition phase. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 417–422. [Google Scholar] [CrossRef]
- Buschang, P.H.; Stroud, J.; Alexander, R.G. Differences in dental arch morphology among adult females with untreated Class I and Class II malocclusion. Eur. J. Orthod. 1994, 16, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Varrela, J. Longitudinal assessment of Class II occlusal and skeletal development in the deciduous dentition. Eur. J. Orthod. 1993, 15, 34. [Google Scholar]
- McNamara, J.A. Early intervention in the transverse dimension: Is it worth the effort? Am. J. Orthod. Dentofac. Orthop. 2002, 121, 572–574. [Google Scholar] [CrossRef]
- McNamara, J.A. Long-term adaptations to changes in the transverse dimension in children and adolescents: An overview. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 71–74. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).