1. Introduction
Sickle cell disease is a monogenic hematological disorder with varying clinical phenotypes. SCD is caused by a point mutation in the beta globin (HBB) gene found on chromosome 11. This single base pair substitution causes aberrant hemoglobin (HbS), which leads to the characteristic sickle form of the red blood cells (RBCs).
SCD is exceedingly prevalent in Sub-Saharan Africa, Southeast Asia, and the Middle East. According to the World Health Organization (WHO), approximately 300,000 infants are born with SCD in these countries every year [
1,
2]. Without treatment, many patients born with SCD die before the age of five [
3]. Early and efficient diagnosis of SCD would enable better management, alleviate morbidity, and reduce mortality. Molecular based screening specifying the genotype of SCD is crucial, not only for diagnosing patients, but also for genetic counseling to reduce the spread of SCD.
The cost and complexity of current standard diagnostic procedures impede the early detection of SCD in resource-limited settings across the world. Currently, methods such as isoelectric focusing (IEF), electrophoresis, and high-performance liquid chromatography (HPLC) are used to detect the wildtype (AA), sickle cell carrier (AS) and sickle cell disease (SS) genotypes. The above tests are expensive and require highly trained staff to interpret the results [
4]. Moreover, HPLC cannot stand alone as a diagnostic test and must be done along with a confirmatory test, such as sequencing-based DNA analysis, before a final diagnosis can be made [
4,
5]. Although different point-of-care assays are available commercially, most are antibody tests that cannot be applied in individuals who have undergone blood transfusions in the last 90 days, as it may result in misleading interpretations, due to presence of hemoglobin proteins from the donor blood. Antibody tests also prove inconclusive in cases where newborns undergo blood transfusion due to multiple reasons, including hemorrhagic shock and premature anemia, among other birth related complications [
6], requiring re-validation 90 days later, further delaying diagnosis and increasing cost. In addition, all newborns express basal level fetal hemoglobin in the first several months of life. As a result, in order to establish a definitive diagnosis, the levels of the different forms of hemoglobin must be compared at a later period [
7,
8].
Blood samples have long been utilized in clinical diagnosis and genetic investigations, including for newborn screening. However, blood samples are susceptible to clotting, smearing, and oversaturation [
9]. Hence, blood samples used for genetic screening must be collected very carefully, by trained professionals. In addition, blood collection is intrusive, especially for pediatric patients, and it may not be essential for molecular diagnosis, where easy-to-collect, less-expensive alternatives, such as the use of buccal swabs and saliva collection, can be attempted.
Allele-specific identification of disease mutation can provide classifications of genetic disease for precise diagnosis. Traditional techniques to identify point mutations are mainly dependent on methods such as gold-standard DNA sequencing [
10] and real-time PCR [
11], which are often time-consuming and require costly instruments and a clean environment. Isothermal DNA amplification approaches have similar sensitivity and specificity to a conventional PCR, can be set up at constant temperature, and requires only an inexpensive heating block.
Thus far, the majority of the PCR-based genetic tests rely on the use of purified genomic DNA from clinical samples [
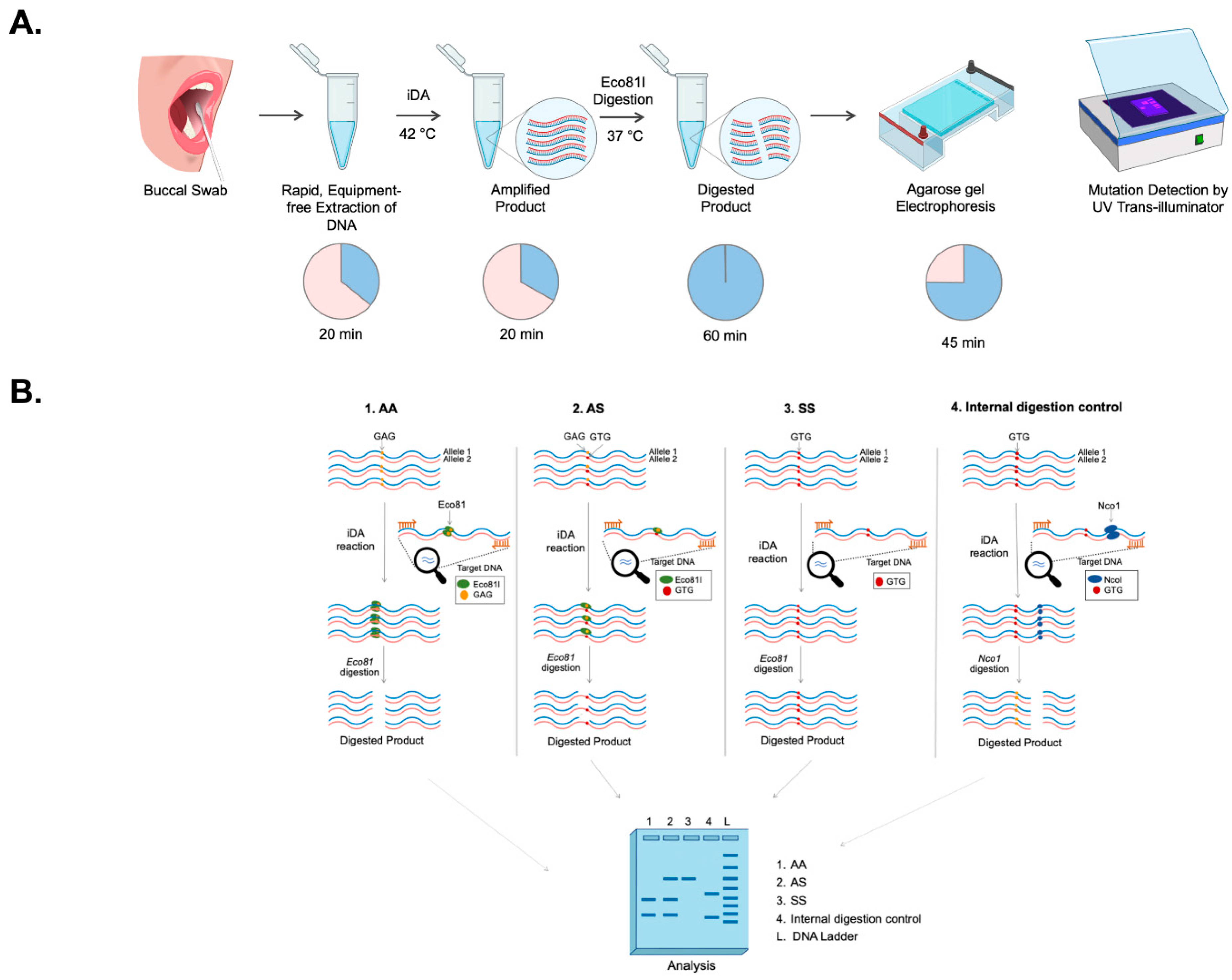
12], which constitutes a major bottleneck in molecular diagnosis. In the current pilot study, a unique strategy is demonstrated that allows specific discrimination of point mutation using
isothermal
DNA
Amplification coupled
Restrictase-mediated cleavage (iDAR). A simple non-invasive buccal swab specimen has been adopted, which is economical and can be used as a direct sample matrix without the need for a DNA extraction process. Moreover, the assay has been simplified to a one-pot single tube reaction of a complete sample-to-answer workflow which could facilitate the genetic analysis of the clinical sample in less than 150 min. As a proof-of-concept, the robustness of the iDAR assay in the detection of allele-specific SCD genotypes from extraction-free non-invasive crude lysates of buccal swab samples has been shown in patients, carriers, and wild-type samples.
2. Materials and Methods
2.1. Construction of Recombinant HBB Plasmids Carrying HBB Wild-Type (AA), and Sickle Cell Mutation (SS) Sequence
The HBB gene was amplified from blood samples of a healthy individual/wild-type (AA) and SCD patients (SS) using genomic DNA with HBB primers (HBB-F: CTAGGGTTGGCCAATCTACTC and HBB-R: AGTAATGTACTAGGCAGACTGTG). The PCR amplicons were cloned into pJET plasmid (Fermentas, Waltham, MA, USA) following the manufacturer’s instructions. Subsequently, the ligated products were transformed into Escherichia coli DH5α, and colonies were screened using colony PCR. Recombinant plasmids were isolated and purified using Plasmid MiniPrep Kit (Thermo Fisher Scientific, Waltham, MA, USA). Results was further confirmed through Sanger sequencing. The recombinant HBB plasmids were termed pSR-βAA and pSR-βSS, and the concentrations of plasmid DNA were estimated using NanoDrop 2000 (Thermo Fisher Scientific, MA, USA).
2.2. Design of iDA Primers
iDA primers for the target gene HBB were designed as per manufacturer’s recommendations (TwistDx, Cambridge, UK). The primers were designed based on the following parameters: iDA product size between 250 to 300 bp, primer size between 30 to 35 nucleotides, and primer GC content 40–70% using the IDT OligoAnalyser tool. The iDA primers designed were HBB iDA forward primer: GTCAGGGCAGAGCCATCTATTGCTTACATT and HBB iDA reverse primer: ATAGACCAATAGGCAGAGAGAGTCAGTGCC. All the primers used in this study were synthesized from Sigma-Aldrich, Bangalore, India.
2.3. Sensitivity and Specificity Analysis
The HBB gene was amplified using HBB-F and HBB-R primer, and the concentration of the amplicon was determined using the Nanodrop 2000 (Thermo Fisher Scientific, MA, USA). The copy number of the amplified product was calculated using the formula: number of copies per µL = ((Amount of ds DNA) (6.0221023 molecules per mole))/((length of dsDNA) 109 ng (660 g/mole)). The PCR amplified product was serially diluted to obtain the copy number per µL in a range of 108–100. Each dilution was used for iDA. Simultaneously, real time quantitative PCR (qPCR) was also performed for each dilution using the Premix ExTaq Master Mix (Takara Bio Inc. Shiga, Japan), according to the manufacturer’s protocol.
2.4. Buccal Swab Samples Collection
The study was conducted after obtaining approval from the Institutional Ethics Committee at the CSIR-Institute of Genomics and Integrative Biology, New Delhi, and the All India Institute of Medical Sciences (AIIMS, New Delhi, India). Written informed consent was obtained for the study. Participants were requested to provide samples using nylon-flocked buccal swabs (Himedia, Mumbai, India) to swab each inner cheek at least 10–15 times. Buccal swab samples were collected and immediately placed in the lysis buffer.
2.5. Processing of Buccal Swab Specimens in Different Lysis Buffers
Four different lysis buffers, namely, buffer A (custom-made buffer), buffer B [
13], buffer C (custom-made buffer) and buffer D [
14], were attempted for the direct amplification of clinical buccal swab samples. The details of buffer compositions are given in
Table 1 Buccal swab samples collected in lysis buffer A, B, and C were directly used for performing iDA. For lysis buffer D, the samples were vortexed for 10 min and then incubated at 95 °C for 10 min, keeping buccal swabs in the tube itself. Samples were allowed to cool down at room temperature, and the buccal swabs were removed from the tube. Finally, 120 µL 1 M Tris-Cl (pH-8.0) was added. If the iDA was not performed immediately, buccal swab samples collected in respective lysis buffer were stored at 4 °C. The buccal swab samples which were collected and transported as dry swabs were processed in lysis buffer D on arrival and further processed in a similar manner to the processing of fresh buccal swabs.
2.6. iDA Assay Setup and Electrophoresis
iDA reactions were performed using the TwistAmp Basic kit (TwistDx Limited, Cambridge, UK, TABAS03KIT), according to the manufacturer’s instructions. For a 50 µL reaction, 37.5 µL of master mix containing 29.5 µL of rehydration buffer, 2.4 µL of 10 µM HBB iDA forward primer, 2.4 µL of 10 µM HBB iDA reverse primer (all together, called HBB iDA mix); 5–10 ng of recombinant plasmid, or 5–20% of buccal swab lysate, was sequentially added to a reagent pellet and the solution was pipetted up and down 6 to 8 times to mix. Subsequently, 2.4 µL of magnesium acetate (MgOAc) was added to the lid, and the tubes were closed and mixed by brief vortexing. After brief centrifugation, the reaction was immediately initiated by incubation in a heat block, with a constant temperature (either 42 °C or 37 °C) for 20 min. The iDA products were analyzed using 2% agarose gel electrophoresis and documented using a UV transilluminator or gel documentation system.
2.7. Targeted Cleavage of iDA Products
Eco81I-mediated cleavage of iDA products were performed in 30 µL of reaction volume containing 4–8 µL of direct iDA product, 1 Tango buffer, and 15 U of Eco81I (Thermo Scientific, MA, USA). Alternatively, DdeI enzyme can also be used for iDAR. The reaction was incubated at 37 °C for 1 h under shaking conditions (180 rpm) in an incubator, and the cleaved products were analyzed using 2.5% agarose gel electrophoresis. To ensure the purity of the SCD iDA product, Nco1 enzyme (New England BioLabs, Ipswich, UK) was used as an internal digestion control.
2.8. PCR Amplification and Sanger Sequencing
Clinical buccal swab samples were used for HBB gene amplification using primer HBB-F (seq): GCTGTCATCACTTAGACCTCAC and HBB-R (seq): CATAGACTCACCCTGAAGTTCTCA, which covers SCD mutation using standard PCR with OneTaq DNA polymerase (New England BioLabs, MA, USA)). The PCR products were column purified using a PCR purification kit (Genetix Biotech, Delhi, India) and were subjected to Sanger sequencing. Sequencing was carried out at AgriGenome Labs Pvt. Ltd., Kochi, India
2.9. One-Pot-Reaction
For the one-pot synthesis, 1 reaction of HBB iDA mix was divided into 5 reactions, each containing 8 µL of HBB iDA mix and 5–20% of buccal swab sample. The reaction was activated by addition of 0.8 µL MgOAc and subsequently amplified at 37 °C for 10 min and inactivated at 85 °C for 5 min in the heat block. The digestion premix for the 30 µL reaction was made with 1 Tango buffer and 15U Eco81I, added to the respective tubes for mutation screening. As an internal control, a digestion premix containing 1 Cutsmart buffer and 15 U of NcoI was prepared for 30 µL reaction. One-pot products were analyzed using 2.5% agarose gel electrophoresis and documented using a UV transilluminator or gel documentation system.
4. Discussion
Sickle cell disease has emerged as a significant global health burden and to combat it, early diagnosis using genetic confirmation is vital. One way of doing it this is by enabling simple and accurate diagnostic screening in a limited resource setting, leading to early diagnosis, expeditious management in affected newborns, as well as aid in the identification of carriers and subsequent genetic counseling [
15].
Currently, in order to make a conclusive diagnosis, there are a series of tests that are performed, including a full blood panel, followed by HPLC and further confirmation of the genetic mutation through Sanger sequencing. Although the latter ensures an accurate diagnosis, it is not quick nor easily deployable, requiring specialized instruments and trained professionals. Hence, developing simple and efficient strategies of diagnosis is crucial.
SCD screening can also be achieved by several point-of-care tests, such as assays based on hemoglobin solubility [
16] and monoclonal antibody-based detection of hemoglobin AA or SS [
17], which are becoming accessible, reducing the challenges regarding necessary infrastructure and costs. However, any assay based on monoclonal antibodies, such as HemoTypeSC [
17], that identifies hemoglobin proteins cannot be utilized in patients who have been transfused recently, since blood transfusions contain globin proteins from the donor, and this leads to misinterpretation of the results [
4]. Solubility testing cannot differentiate between SCD and a carrier; hence, it is not recommended due to these limitations, and it is less ideal for SCD screening [
16].
In recent years, lateral flow assays (LFAs) have been broadly used as portable molecular diagnostic methods. In 2015, Kanter et al. developed a sickle SCAN scan based on lateral flow immunoassay to detect SCD [
8]. However, the assay has several limitations, such as misinterpretation due to visual reading, polyclonal antibody cross-reactivity, inconsistency in the band’s intensity, and false-positive results in identifying HbAS with HbSS. Hence, the authors suggested further confirmatory validation. Another study by Natoli et al. reported a strategy for allele-specific detection of the sickle cell mutation using blood samples [
18]. In their assay, two separate reactions for each sample are required to detect AA and SS genotypes, which is the major limitation of the above study.
Isothermal DNA amplification-based molecular diagnosis is an emerging strategy that has been successfully employed for the screening of infectious diseases such as Ebola virus disease (EVD) and COVID-19 [
19,
20]. Current studies focus on developing an isothermal DNA amplification-based strategy for the screening of SCD. There are, however, certain challenges that had to be addressed in order to develop this assay, such as the nature of sample collected and the quickest way to process the samples without compromising the efficiency and accuracy of the test.
Our iDAR assay system is very simple and easily deployable in a resource limited setting, as it only requires a heat block and a tube prefilled with a mixture containing the essential reagents for amplification and subsequently treated with restrictase in the same tube for screening. Notably, the addition of direct buccal swab samples does not significantly affect the sensitivity of the iDA. It was noted that the sensitivity of iDA was compromised when more than 20% of the buccal swab lysates make up the reaction volume. The present study has demonstrated the sensitivity of iDA to be 91.5%; however, the sensitivity of the assay can be increased by changing the concentration of buccal swab lysate in the reaction volume. Moreover, we were able to achieve 100% amplification by modulating the buccal swab lysate concentration. In addition, we also observed that iDA assay detected the genotype correctly, even in patients who had undergone blood transfusion within a few weeks before sample collection. Hence, the current study has shown 100% specificity in discriminating AA, AS, and SS genotypes. Moreover, the chances of false positive results are highly unlikely using the iDAR assay system, since the enzyme site is lost in SS genotype. It is noteworthy that if digestion is not kept under recommended conditions, the AA genotype can be falsely diagnosed as the AS genotype.
In this study, a single test reaction is required to differentiate all the three genotypes, the SS, AS and AA alleles, which brings down the assay cost. By leveraging Eco81I-mediated sequence-specific cleavage, our iDAR assay system shows a more consistent and precise outcome for heterozygous (AS) and homozygous (SS) samples. The iDAR assay offers an alternative to DNA sequencing or real-time PCR for rapid SCD genotyping, while retaining the advantages of simplicity, affordability, and a faster qualitative readout.
Traditionally, blood samples have been used for clinical diagnostics and genetic studies. However, blood collection is an invasive procedure, and is both expensive and requires trained professionals. Even though blood is the preferred sample for running most of the molecular tests, using it for DNA amplification is not suitable, for multiple reasons [
21,
22]. The nucleic acid isolated from blood or blood containing samples is usually low; therefore, the sensitivity of isothermal amplification is reduced. A more suitable and less invasive alternative to blood is taking saliva for use in molecular diagnosis. However, certain study participants have difficulty in spitting into a tube, while others struggle to produce enough saliva for genetic testing [
23] Dry mouth is a typical medication side effect that can make saliva collection difficult [
23]. However, buccal swab sample collection is quick, non-invasive, and inexpensive. Taking all of this into account, this study sought to explore the feasibility of performing SCD genotyping. This type of testing also makes it easy for patients and their family members to collect samples at clinics or at their homes. Biological samples, such as stool, serum, plasma, vaginal, and nasal, have been used for isothermal amplification [
24]; however, this is the first report where buccal swab specimens have directly been used for iDA, especially in the molecular diagnosis of a genetic disease.
Developing a molecular diagnostic test that does not require DNA isolation is difficult, since existing genotyping strategies based on DNA amplification necessitate relatively high DNA purity [
25,
26]. Hence, developing a genetic test that analyzes the samples without DNA isolation and purification has remained elusive. The current study aimed to establish an inexpensive, low-complexity buffer system with routine laboratory chemicals that make direct iDA feasible by utilizing a simple procedure that allows for the efficient release of DNA from buccal swab specimens.
Previously, to aid the release of nucleic acids from human cells, various procedures have been applied, such as using complex solvents and expensive unique materials [
27,
28]. In the iDAR assay system, we leveraged NaOH to lyse the cell membrane for releasing DNA and Tris-Cl as a crucial pH control agent, providing an appropriate environment for iDA reaction. Thus, the iDAR assay system proposed in this study is capable of genotyping target genes without undertaking the laborious, time-consuming and expensive nucleic acid isolation and purification step, avoiding the possibility of cross contamination.
To date, no information is available on the stability of DNA in “dry swab” for storage and transport at various temperatures and its impact, specifically on the iDA for genetic testing. The storage of biological samples is a major challenge during sample collection at a remote place, as sample integrity is a factor of great importance. Ideally, biological samples must be kept in temperature-controlled, adequately qualified storage [
29], and processed as soon as possible after collection. However, in a realistic scenario, the vast majority are stored and transported some distances before processing. In this study, the viability of dry swabs without any transport reagent was tested for storage and transport at various incubation times and temperatures. It was observed that dry swabs can be transported at a maximum of 42 °C and held for up to 72 h without affecting iDA. These findings are significant for low- and middle-income nations that have limited access to rapid refrigerated transport and storage of samples, providing a cost-effective option. Finally, this study reveals the practical and financial benefits of employing dry swabs without a transportation reagent.
In the iDAR assay system, reagents account for the majority of the overall per-test cost. Thus, it was hypothesized that lowering the per-test reaction volume can significantly reduce the assay’s cost. Thus, different reaction volumes were experimented with, and it was observed that amplification using direct buccal swab specimens as templates in all volumes worked efficiently without compromising assay sensitivity and performance. Hence, this brings down the amplification cost by one-fifth and also significantly lowers the overall assay cost to USD 5.
However, we have not shown whether the iDAR assay system can discriminate among AA, hemoglobin type C genotypes AC, CC (HbC), and SC (compound heterozygous for HbC and HbS). Principally, the iDAR assay tool can discriminate between HbC genotypes if the Hpy188III enzyme is used instead of Eco81I. Hpy188III recognises TCNNGA in the AA genotype, whereas in HbC, glutamate (GAG) is changed to lysine (AAG) in the sixth codon of HBB gene. This results in the loss of enzyme recognition site (TCNNAA), and hence, no digestion would be expected with Hpy188II in the CC genotype. Therefore, if the digestion pattern of a study subject shows heterozygosity with both Eco81I and Hpy188III restriction enzymes, it suggests the SC genotype.
One of the limitation of the iDAR assay tool is the differentiation of SS from Sβ thalassemia, which is recognized as the heterozygous AS genotype. Since β thalassemia is caused due to more than 200 mutations and these mutations are spread across the HBB gene, so it becomes difficult to integrate β thalassemia mutations in the iDAR assay.
In summary, the iDAR assay platform has considerable advantages. The results show that iDAR is an efficient assay capable of detecting all three genotypes, SS, AS, and AA. Existing genetic diagnostic tests based on PCR, such as DNA sequencing and qPCR, typically require a complicated operational procedure, as well as expensive and sophisticated instruments that may not be available in many laboratories, whereas the iDAR assay can be done with less complex instruments and provides reliable, inexpensive, easy-to-use, and affordable genetic diagnostics for SCD, facilitating the expansion of SCD screening in low-resource settings.