Nephrogenic Systemic Fibrosis in Patients with Chronic Kidney Disease after the Use of Gadolinium-Based Contrast Agents: A Review for the Cardiovascular Imager
Abstract
:1. Introduction to Gadolinium-Based Contrast Agents
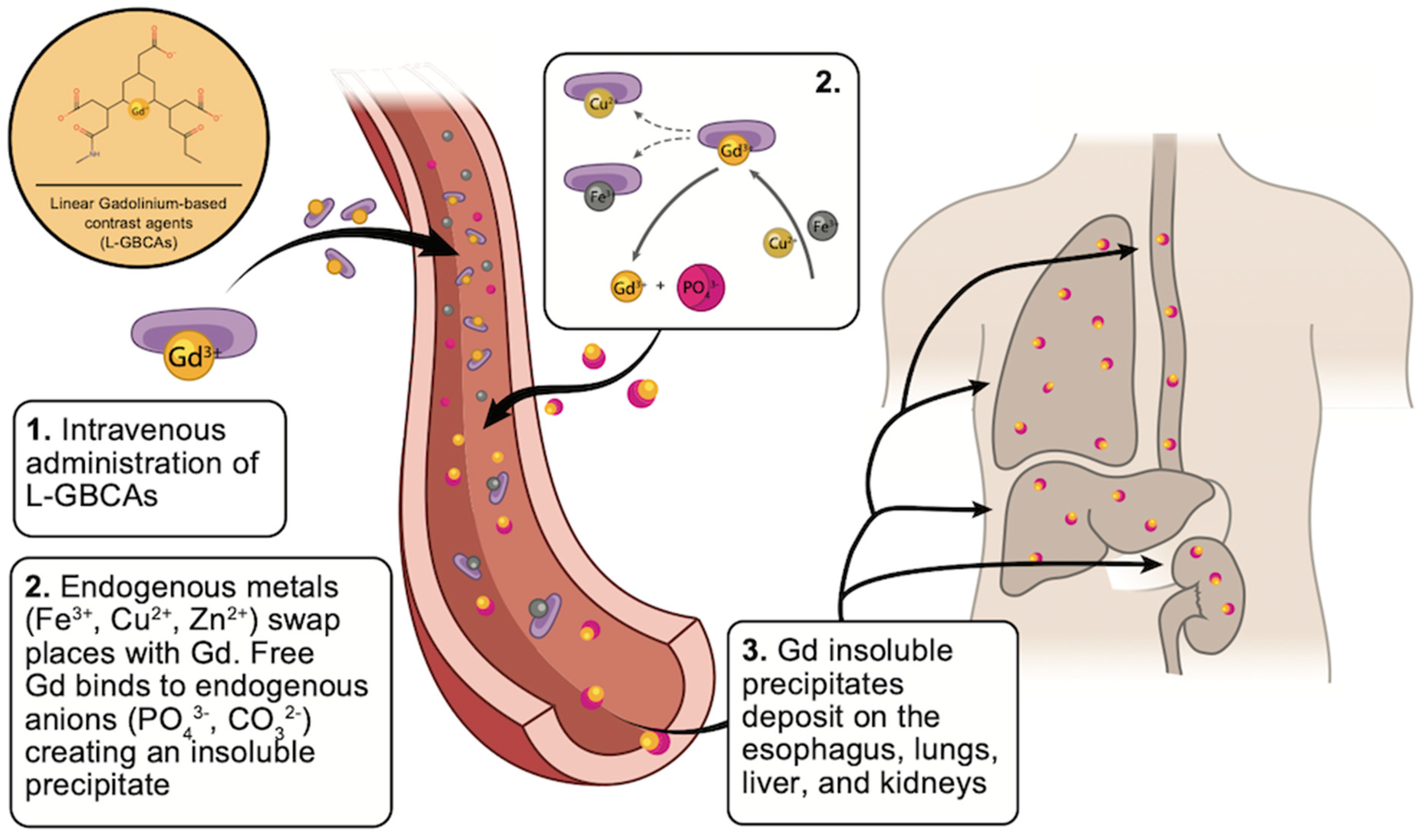
2. Linear vs. Macrocyclic GBCAs
3. Clinical Use of GBCAs in Cardiovascular Magnetic Resonance
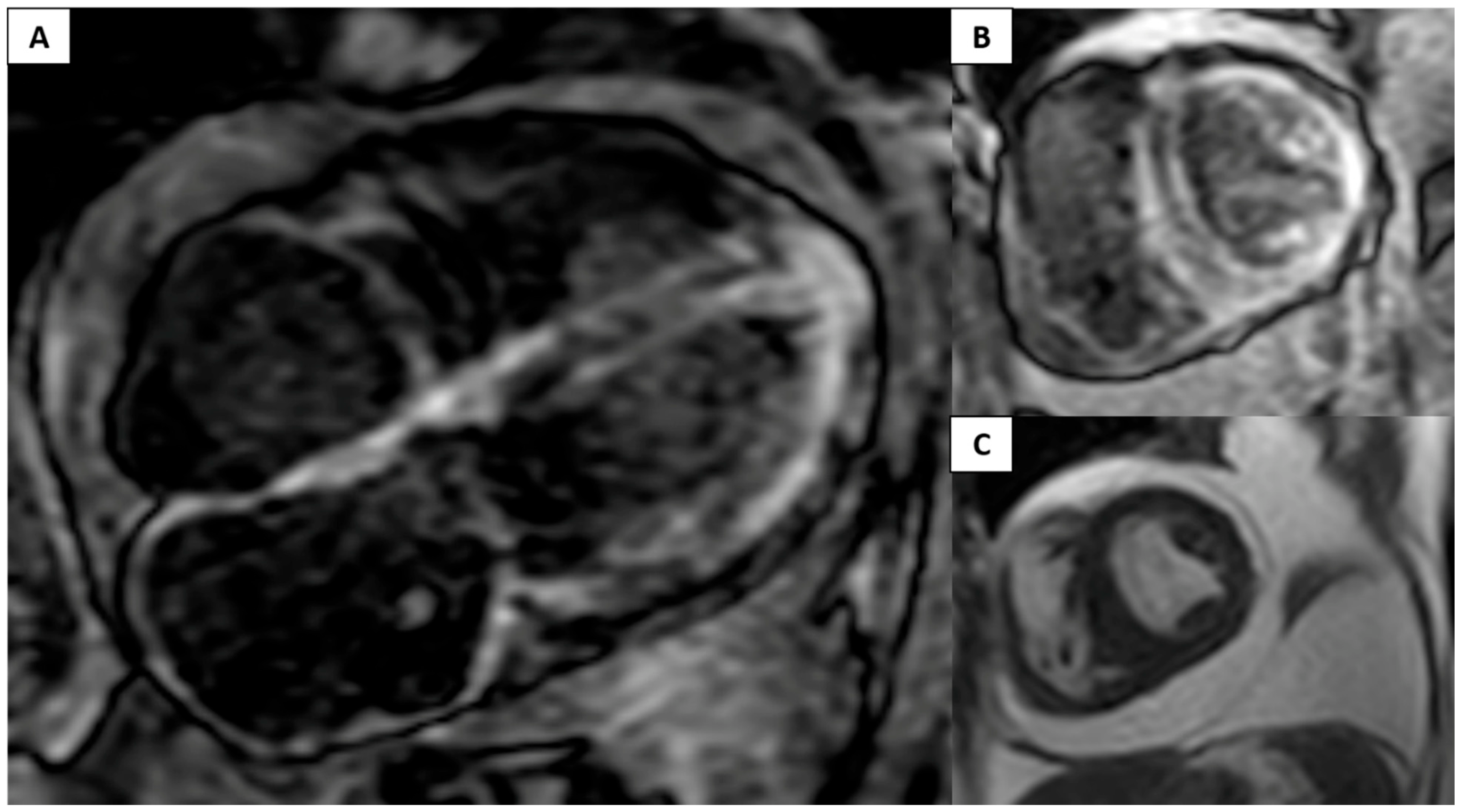
Clinical Case: Use of GBCAs in a Patient with Decreased Left Ventricular Ejection Fraction and Increased Thickness
4. Overview of Nephrogenic Systemic Fibrosis
5. General Risk Factors for NSF
6. Clinical Approach for the Diagnosis of NSF
7. Histopathologic Examination
8. GBCAs’ Differential Risk of NSF
9. Prevention and Treatment of NSF
10. Take-Home Messages and Clinical Applications
10.1. Estimation of the Glomerular Filtration Rate
- In the outpatient setting, eGFR should be estimated only in those patients with risk factors for CKD. Those patients with no risk factors or confirmed CKD should not undergo additional testing [25].
- A recent creatinine value should be used (<72 h) for eGFR estimation. However, there is no evidence regarding the most appropriate timing for eGFR estimation [49].
10.2. Patients at Risk for Chronic Kidney Disease
- Outpatients who may be receiving GBCAs should be screened for risk factors or conditions associated with CKD [25]. This assessment should include inquiring about a history of confirmed CKD or any kidney condition (dialysis, kidney transplant, glomerulopathies, single kidney, kidney surgery, or kidney neoplasm), hypertension (requiring medical therapy), cardiovascular disease (including heart failure or coronary disease), and diabetes mellitus on metformin. For those patients identified by screening with one or more risk factors, eGFR estimation with serum creatinine should be performed [25].
10.3. Contrast Selection
- In patients with normal kidney function (eGFR > 60 mL/min/1.73 m2) and no additional risk factors, the incidence of NSF after a GBCA infusion is negligible. As a result, any type of GBCAs can be safely used [43].
- In patients with stage 3 CKD (eGFR 30–50 mL/min/1.73 m2) and no additional risk factors, NSF’s risk is minimal. As a result, no additional actions are necessary.
- Acute kidney injury: the presence of AKI significantly increases the risk of NSF [36,39,47]. In addition, the incidence of AKI is significantly higher in patients with confirmed or suspected cardiovascular disease. As a result, additional precautions should be taken into account. In AKI, there is a lag between the serum creatinine values and the actual eGFR. As a result, the sole estimation of eGFR based on creatine values could be problematic. In this setting, the ACR group-I GBCA agents should be avoided in patients with confirmed or suspected AKI [25].
10.4. Dialysis: Specific Recommendation
- In those patients with terminal CKD already on RRT (hemodialysis or peritoneal dialysis), dialysis should continue after receiving a GBCA. GBCA infusion should be performed as closely before hemodialysis as is possible [25]. These patients should receive dialysis the same day of the procedure, ideally 2 to 3 h after the contrast infusion to minimize the possibility of transmetalation and NSF [25,49].
- There is insufficient evidence to support changing patients from peritoneal dialysis to hemodialysis or altering dialysis prescription after the infusion of a GBCA. Peritoneal dialysis may be less effective than hemodialysis in clearing circulating GBCA; however, there is no evidence regarding the superiority of a specific type of RTT in order to decrease the risk of NSF [37,49].
10.5. Patients Who Require Multiple Studies
- NSF occurs most commonly in patients who received high doses of GBCA, either as a single dose or cumulatively after multiple administrations [25]. In some circumstances, patients may require multiple doses of a GBCA within a short time frame; thus, these patients are at a higher risk of developing NSF.
- In patients with preserved or moderately reduced kidney function (eGFR > 30 mL/min/1.73 m2), there is no contraindication if the examinations are determined to be necessary [25]. However, taking into account the elimination time of the GBCAs, it is advisable to wait at least 4 h between studies [37,49]. The usage of an ACR type-II GBCAs is advisable in this circumstance.
- In patients with residual kidney function who do not receive RRT, there should be at least 7 days between each study.
11. Limitations
- Even though current studies may not suggest NSF cases with the use of group II GBCAs, there is still epidemiological limitations to consider NSF risk as zero. There is a small number of patients with CKD stage 5 involved which underestimates the NSF incidence rate [48]. CKD patients should be assessed with a complete medical history and risk factors to determine GBCA use.
- We did not mention some other alternatives for CKD patients with eGFR < 30 mL/min/1.73 m2. For example, ferumoxytol is a vascular contrast agent for MR angiography with superparamagnetic properties useful to venous and arterial enhancement in stage 4 and 5 CKD patients [54].
12. Essentials
- Gadolinium-based contrast agents serve to improve diagnostic images’ sensitivity and specificity and characterize a wide array of cardiovascular pathologies.
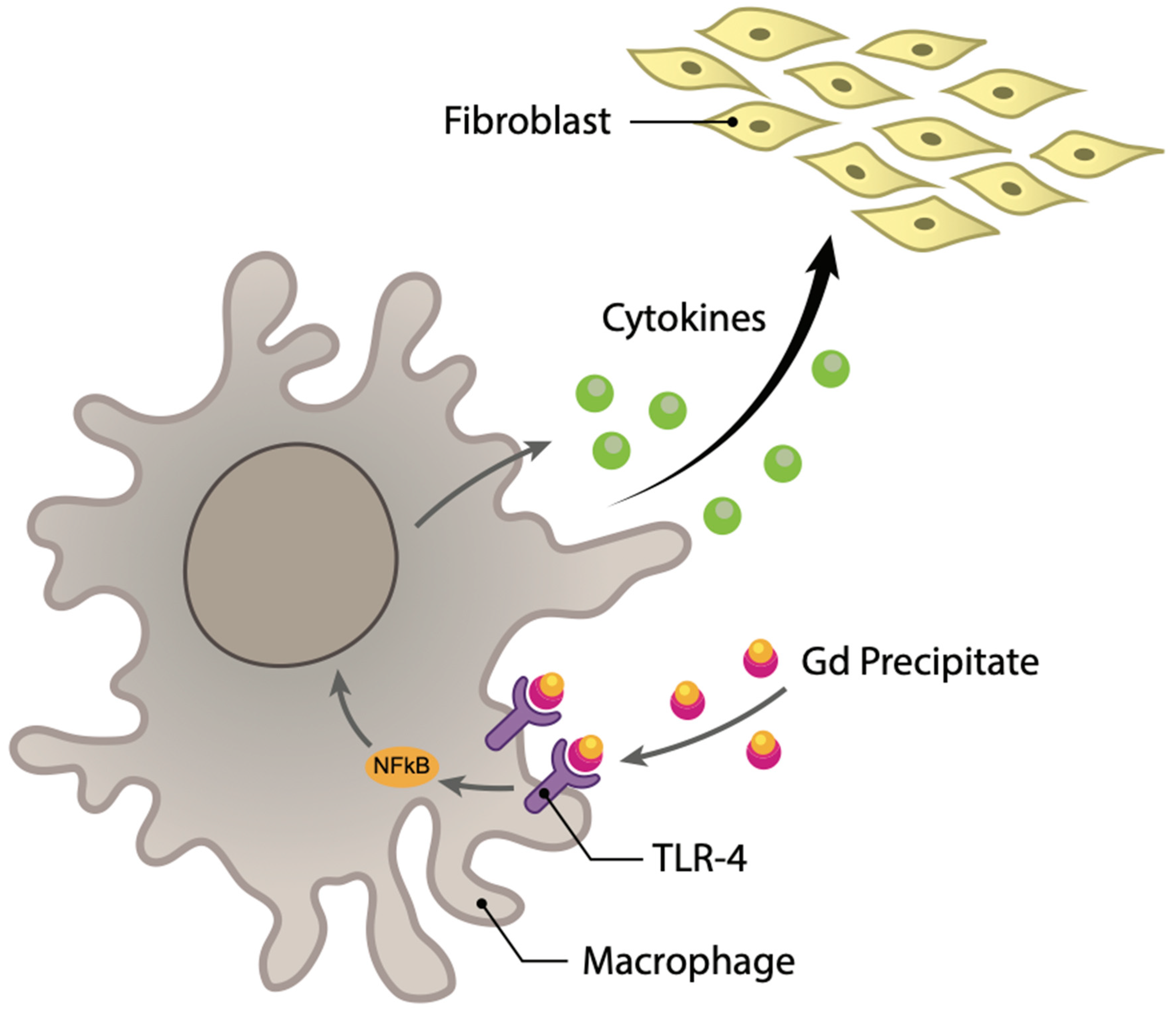
- NSF is a devastating, multisystemic fibrotic disease that affects the skin, muscle, and other organs (including lung, esophagus, and kidney) described in patients with severe renal impairment exposed to a gadolinium-based contrast agent.
- There is not a specific treatment or prophylaxis regimen to treat or prevent the onset of NSF.
- Even though the newer macrocyclic agents have proven to be much safer in patients with chronic kidney disease and end-stage renal failure, clinicians must fully understand the clinical characteristics and risk factors of this devastating pathology and maintain a high degree of suspicion to prevent and recognize it. Cardiac MRI with late gadolinium enhancement (LGE) has significantly impacted the management, decision making, and diagnosis of various cardiomyopathy or interstitial heart disease. However, the over-concerned about nephrogenic systemic fibrosis may make cardiac MRI with LGE be avoided inappropriately. The risk and benefits of this imaging study should be balanced.
Author Contributions
Funding
Conflicts of Interest
References
- Wermuth, P.J.; Jimenez, S.A. Gadolinium compounds signaling through TLR 4 and TLR 7 in normal human macrophages: Establishment of a proinflammatory phenotype and implications for the pathogenesis of nephrogenic systemic fibrosis. J. Immunol. 2012, 189, 318–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caravan, P. Strategies for increasing the sensitivity of gadolinium based MRI contrast agents. Chem. Soc. Rev. 2006, 35, 512. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, H.S.; Morcos, S.K.; Almén, T.; Bellin, M.-F.; Bertolotto, M.; Bongartz, G.; Clement, O.; Leander, P.; Heinz-Peer, G.; Reimer, P.; et al. Nephrogenic systemic fibrosis and gadolinium-based contrast media: Updated ESUR contrast medium safety committee guidelines. Eur. Radiol. 2013, 23, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.C.C.; Reed, E.; Sheppard, M.N.; Elkington, A.G.; Ho, S.; Burke, M.; Petrou, M.; Pennell, D.J. The histologic basis of late gadolinium enhancement cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2004, 43, 2260–2264. [Google Scholar] [CrossRef]
- Vogler, H.; Platzek, J.; Schuhmann-Giampieri, G.; Frenzel, T.; Weinmann, H.-J.; Radüchel, B.; Press, W.-R. Pre-clinical evaluation of gadobutrol: A new, neutral, extracellular contrast agent for magnetic resonance imaging. Eur. J. Radiol. 1995, 21, 1–10. [Google Scholar] [CrossRef]
- Scott, L.J. Gadobutrol: A review of its use for contrast-enhanced magnetic resonance imaging in adults and children. Clin. Drug Investig. 2013, 33, 303–314. [Google Scholar] [CrossRef]
- FDA. DOTAREM (Gadoterate Meglumine) Injection for Intravenous Use; FDA: Silver Spring, MD, USA, 2013; pp. 1–13. [Google Scholar]
- Tombach, B.; Bremer, C.; Reimer, P.; Schaefer, R.M.; Ebert, W.; Geens, V.; Heindel, W. Pharmacokinetics of 1M Gadobutrol in Patients with Chronic Renal Failure. Investig. Radiol. 2000, 35, 35. [Google Scholar] [CrossRef]
- European Medicines Agency. Gadovist 1.0 mmol/Ml Solution for Injection; European Medicines Agency: Amsterdam, The Netherlands, 2012; pp. 1–9. [Google Scholar]
- European Medicines Agency (EMA) Gadolinium-Containing Contrast Agents; European Medicines Agency: Amsterdam, The Netherlands, 2010.
- Aime, S.; Caravan, P. Biodistribution of gadolinium-based contrast agents, including gadolinium deposition. J. Magn. Reson. Imaging 2009, 30, 1259–1267. [Google Scholar] [CrossRef] [Green Version]
- Clough, T.J.; Jiang, L.; Wong, K.-L.; Long, N.J. Ligand design strategies to increase stability of gadolinium-based magnetic resonance imaging contrast agents. Nat. Commun. 2019, 10, 1420. [Google Scholar] [CrossRef] [Green Version]
- Sieber, M.A.; Lengsfeld, P.; Frenzel, T.; Golfier, S.; Schmitt-Willich, H.; Siegmund, F.; Walter, J.; Weinmann, H.-J.; Pietsch, H. Preclinical investigation to compare different gadolinium-based contrast agents regarding their propensity to release gadolinium in vivo and to trigger nephrogenic systemic fibrosis-like lesions. Eur. Radiol. 2008, 18, 2164–2173. [Google Scholar] [CrossRef] [Green Version]
- FDA. Gadovist (Gadobutrol) Injection, for Intravenous Use: US Prescribing Information; FDA: Silver Spring, MD, USA, 2011. [Google Scholar]
- Bussi, S.; Coppo, A.; Celeste, R.; Fanizzi, A.; Fringuello Mingo, A.; Ferraris, A.; Botteron, C.; Kirchin, M.A.; Tedoldi, F.; Maisano, F. Macrocyclic MR contrast agents: Evaluation of multiple-organ gadolinium retention in healthy rats. Insights Into Imaging 2020, 11, 11. [Google Scholar] [CrossRef]
- Hazelton, J.M.; Chiu, M.K.; Abujudeh, H.H. Nephrogenic systemic fibrosis: A review of history, pathophysiology, and current guidelines. Curr. Radiol. Rep. 2019, 7, 5. [Google Scholar] [CrossRef]
- Tóth, É.; Helm, L.; Merbach, A.E. Relaxivity of MRI Contrast Agents; Springer: Berlin/Heidelberg, Germany, 2002; pp. 61–101. [Google Scholar]
- Brücher, E. Kinetic Stabilities of Gadolinium(III) Chelates Used as MRI Contrast Agents; Springer: Berlin/Heidelberg, Germany, 2002; pp. 103–122. [Google Scholar]
- Woolen, S.A.; Shankar, P.R.; Gagnier, J.J.; MacEachern, M.P.; Singer, L.; Davenport, M.S. Risk of nephrogenic systemic fibrosis in patients with stage 4 or 5 chronic kidney disease receiving a group II gadolinium-based contrast agent. JAMA Intern. Med. 2020, 180, 223. [Google Scholar] [CrossRef]
- Tombach, B.; Bremer, C.; Reimer, P.; Matzkies, F.; Schaefer, R.M.; Ebert, W.; Geens, V.; Eisele, J.; Heindel, W. Using highly concentrated gadobutrol as an MR contrast agent in patients also requiring hemodialysis. Am. J. Roentgenol. 2002, 178, 105–109. [Google Scholar] [CrossRef]
- Von Knobelsdorff-Brenkenhoff, F.; Schüler, J.; Dogangüzel, S.; Dieringer, M.A.; Rudolph, A.; Greiser, A.; Kellman, P.; Schulz-Menger, J. Detection and monitoring of acute myocarditis applying quantitative cardiovascular magnetic resonance. Circ. Cardiovasc. Imaging 2017, 10, e005242. [Google Scholar] [CrossRef] [Green Version]
- Minutoli, F.; Bella, G.D.; Mazzeo, A.; Donato, R.; Russo, M.; Scribano, E.; Baldari, S. Comparison between 99m Tc-Diphosphonate Imaging and MRI with late gadolinium enhancement in evaluating cardiac involvement in patients with transthyretin familial amyloid polyneuropathy. Am. J. Roentgenol. 2013, 200, W256–W265. [Google Scholar] [CrossRef]
- Hussain, S.T.; Paul, M.; Plein, S.; McCann, G.P.; Shah, A.M.; Marber, M.S.; Chiribiri, A.; Morton, G.; Redwood, S.; MacCarthy, P.; et al. Design and rationale of the MR-INFORM study: Stress perfusion cardiovascular magnetic resonance imaging to guide the management of patients with stable coronary artery disease. J. Cardiovasc. Magn. Reson. 2012, 14, 65. [Google Scholar] [CrossRef] [Green Version]
- Nacif, M.S.; Arai, A.A.; Lima, J.A.; Bluemke, D.A. Gadolinium-enhanced cardiovascular magnetic resonance: Administered dose in relationship to United States Food and Drug Administration (FDA) guidelines. J. Cardiovasc. Magn. Reson. 2012, 14, 18. [Google Scholar] [CrossRef] [Green Version]
- ACR Committee on Drugs and Contrast Media. ACR Manual on Contrast Media Version; ACR: Silver Spring, MD, USA, 2022; ISBN 978-1-55903-012-0. [Google Scholar]
- Cowper, S.E.; Bucala, R.; Leboit, P.E. Nephrogenic fibrosing dermopathy/nephrogenic systemic fibrosis—setting the record straight. Semin. Arthritis Rheum. 2006, 35, 208–210. [Google Scholar] [CrossRef]
- Cowper, S.E. Nephrogenic Systemic Fibrosis: An Overview. J. Am. Coll Radiol. 2008, 5, 23–28. [Google Scholar] [CrossRef]
- Reiter, T.; Ritter, O.; Prince, M.R.; Nordbeck, P.; Wanner, C.; Nagel, E.; Bauer, W.R. Minimizing risk of nephrogenic systemic fibrosis in cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2012, 14, 31. [Google Scholar] [CrossRef] [Green Version]
- Zou, Z.; Zhang, H.L.; Roditi, G.H.; Leiner, T.; Kucharczyk, W.; Prince, M.R. Nephrogenic systemic fibrosis. JACC Cardiovasc. Imaging 2011, 4, 1206–1216. [Google Scholar] [CrossRef]
- Prince, M.R.; Zhang, H.; Morris, M.; MacGregor, J.L.; Grossman, M.E.; Silberzweig, J.; DeLapaz, R.L.; Lee, H.J.; Magro, C.M.; Valeri, A.M. Incidence of nephrogenic systemic fibrosis at two large medical centers. Radiology 2008, 248, 807–816. [Google Scholar] [CrossRef]
- Cowper, S.E.; Robin, H.S.; Steinberg, S.M.; Su, L.D.; Gupta, S.; LeBoit, P.E. Scleromyxoedema-like cutaneous diseases in renal-dialysis patients. Lancet 2000, 356, 1000–1001. [Google Scholar] [CrossRef]
- Cowper, S.E. Nephrogenic Systemic Fibrosis: The nosological and conceptual evolution of nephrogenic fibrosing dermopathy. Am. J. Kidney Dis. 2005, 46, 763–765. [Google Scholar] [CrossRef]
- Grobner, T. Gadolinium—A specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol. Dial. Transplant. 2006, 21, 1104–1108. [Google Scholar] [CrossRef] [Green Version]
- Girardi, M.; Kay, J.; Elston, D.M.; LeBoit, P.E.; Abu-Alfa, A.; Cowper, S.E. Nephrogenic systemic fibrosis: Clinicopathological definition and workup recommendations. J. Am. Acad. Dermatol. 2011, 65, 1095–1106.e7. [Google Scholar] [CrossRef]
- Yee, J. Prophylactic hemodialysis for protection against gadolinium-induced nephrogenic systemic fibrosis: A doll’s house. Adv. Chronic Kidney Dis. 2017, 24, 133–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaewlai, R.; Abujudeh, H. Nephrogenic systemic fibrosis. Am. J. Roentgenol. 2012, 199, W17–W23. [Google Scholar] [CrossRef] [PubMed]
- Mathur, M.; Jones, J.R.; Weinreb, J.C. Gadolinium deposition and nephrogenic systemic fibrosis: A radiologist’s primer. RadioGraphics 2020, 40, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, H.S. Nephrogenic systemic fibrosis: A serious adverse reaction to Gadolinium—1997–2006–2016. Part 1. Acta Radiol. 2016, 57, 515–520. [Google Scholar] [CrossRef]
- Deo, A.; Fogel, M.; Cowper, S.E. Nephrogenic systemic fibrosis: A population study examining the relationship of disease development to gadolinium exposure. Clin. J. Am. Soc. Nephrol. 2007, 2, 264–267. [Google Scholar] [CrossRef]
- Wang, Y.; Alkasab, T.K.; Narin, O.; Nazarian, R.M.; Kaewlai, R.; Kay, J.; Abujudeh, H.H. Incidence of nephrogenic systemic fibrosis after adoption of restrictive gadolinium-based contrast agent guidelines. Radiology 2011, 260, 105–111. [Google Scholar] [CrossRef] [Green Version]
- Prince, M.R.; Lee, H.G.; Lee, C.-H.; Youn, S.W.; Lee, I.H.; Yoon, W.; Yang, B.; Wang, H.; Wang, J.; Shih, T.T.; et al. Safety of Gadobutrol in over 23,000 patients: The GARDIAN Study, a global multicentre, prospective, non-interventional study. Eur. Radiol. 2017, 27, 286–295. [Google Scholar] [CrossRef] [Green Version]
- Soyer, P.; Dohan, A.; Patkar, D.; Gottschalk, A. Observational study on the safety profile of gadoterate meglumine in 35,499 patients: The SECURE Study. J. Magn. Reson. Imaging 2017, 45, 988–997. [Google Scholar] [CrossRef] [Green Version]
- Michaely, H.J.; Aschauer, M.; Deutschmann, H.; Bongartz, G.; Gutberlet, M.; Woitek, R.; Ertl-Wagner, B.; Kucharczyk, W.; Hammerstingl, R.; de Cobelli, F.; et al. Gadobutrol in renally impaired patients. Investig. Radiol. 2017, 52, 55–60. [Google Scholar] [CrossRef] [Green Version]
- Tsushima, Y.; Awai, K.; Shinoda, G.; Miyoshi, H.; Chosa, M.; Sunaya, T.; Endrikat, J. Post-marketing surveillance of Gadobutrol for contrast-enhanced magnetic resonance imaging in Japan. Jpn. J. Radiol. 2018, 36, 676–685. [Google Scholar] [CrossRef]
- Young, L.K.; Matthew, S.Z.; Houston, J.G. Absence of potential gadolinium toxicity symptoms following 22,897 Gadoteric Acid (Dotarem®) examinations, including 3,209 performed on renally insufficient individuals. Eur. Radiol. 2019, 29, 1922–1930. [Google Scholar] [CrossRef] [Green Version]
- McWilliams, R.G.; Frabizzio, J.V.; de Backer, A.I.; Grinberg, A.; Maes, B.D.; Zobel, B.B.; Gottschalk, A. Observational study on the incidence of nephrogenic systemic fibrosis in patients with renal impairment following gadoterate meglumine administration: The NSsaFe Study. J. Magn. Reson. Imaging 2020, 51, 607–614. [Google Scholar] [CrossRef]
- Penfield, J.G.; Reilly, R.F. NSF: What we know and what we need to know: Nephrogenic systemic fibrosis risk: Is there a difference between gadolinium-based contrast agents? Semin. Dial. 2008, 21, 129–134. [Google Scholar] [CrossRef]
- Rudnick, M.R.; Wahba, I.M.; Leonberg-Yoo, A.K.; Miskulin, D.; Litt, H.I. Risks and options with gadolinium-based contrast agents in patients With CKD: A review. Am. J. Kidney Dis. 2020, 77, 517–528. [Google Scholar] [CrossRef]
- Schieda, N.; Blaichman, J.I.; Costa, A.F.; Glikstein, R.; Hurrell, C.; James, M.; Jabehdar Maralani, P.; Shabana, W.; Tang, A.; Tsampalieros, A.; et al. Gadolinium-based contrast agents in kidney disease: Comprehensive review and clinical practice guideline issued by the Canadian Association of Radiologists. Can. Assoc. Radiol. J. 2018, 69, 136–150. [Google Scholar] [CrossRef] [Green Version]
- Murashima, M.; Drott, H.R.; Carlow, D.; Shaw, L.M.; Milone, M.; Bachman, M.; Tsai, D.E.; Yang, S.L.; Bloom, R.D. Removal of Gadolinium by peritoneal dialysis. Clin. Nephrol. 2008, 69, 368–373. [Google Scholar] [CrossRef]
- Basak, P.; Jesmajian, S. Nephrogenic systemic fibrosis: Current concepts. Indian J. Dermatol. 2011, 56, 59. [Google Scholar] [CrossRef]
- Guo, B.J.; Yang, Z.L.; Zhang, L.J. Gadolinium deposition in brain: Current scientific evidence and future perspectives. Front. Mol. Neurosci. 2018, 11, 335. [Google Scholar] [CrossRef] [Green Version]
- Gulani, V.; Calamante, F.; Shellock, F.G.; Kanal, E.; Reeder, S.B. Gadolinium deposition in the brain: Summary of evidence and recommendations. Lancet Neurol. 2017, 16, 564–570. [Google Scholar] [CrossRef]
- Stoumpos, S.; Hennessy, M.; Vesey, A.T.; Radjenovic, A.; Kasthuri, R.; Kingsmore, D.B.; Mark, P.B.; Roditi, G. Ferumoxytol magnetic resonance angiography: A dose-finding study in patients with chronic kidney disease. Eur. Radiol. 2019, 29, 3543–3552. [Google Scholar] [CrossRef] [Green Version]
| Molecule, Trade Name, and (Vendor) | Type | Osmolality (mOsm/kg H2O) * | Viscosity (mPa•) * | Thermodynamic Complex Stability (log Keq) | Relaxivities r1/r2 in Plasma (mmol/L) at 1.5 T * | Concentration (mol/L) | Approved Intravenous Dose (mmol/kg) | Comments |
|---|---|---|---|---|---|---|---|---|
| Gadobutrol, Gadavist (Bayer Healthcare) | Macrocyclic Non-ionic | 1603 | 4.96 | 21.8 | 5.2/6.1 | 1 | 0.1–0.3 | Highest viscosity. It is marketed as Gadovist outside the United States. |
| Gadoterate meglumine, Dotarem (Guerbet) | Macrocyclic Ionic | 1350 | 2.4 | 25.6 | 3.6/4.3 | 0.5 | 0.1–0.2 | In 2019, a generic version of Dotarem was introduced (Clariscan, GE Healthcare). Some animal studies have shown slightly higher levels of gadolinium deposition with Clariscan compared to Dotarem [15]. |
| Gadoteridol, ProHance (Bracco) | Macrocyclic Non-ionic | 630 | 1.3 | 23.8 | 4.1/5 | 0.5 | 0.1–0.2 | Lowest viscosity and osmolality. Below average viscosity. |
| Gadopentetate dimeglumine, Magnevist (Bayer Healthcare) | Linear Ionic | 1960 | 1.9 | 22.1 | 4.1/4.6 | 0.5 | 0.1–0.3 | Oldest approved agent. Below average relaxivity. High risk of NSF. |
| Gadodiamide, Omniscan (GE Healthcare) | Linear Non-ionic | 783 | 1.4 | 16.9 | 4.3/5.2 | 0.5 | 0.1–0.3 | Low thermodynamic stability; very high risk of NSF. Use suspended in the European Union. |
| Gadobenate dimeglumine, MultiHance (Bracco) | Linear Ionic | 1970 | 5.3 | 22.6 | 6.3/8.7 | 0.5 | 0.05–0.1 | Highest relaxivity of extracellular GBCAs. EMA restricted to hepatobiliary imaging. |
| Gadoxetate disodium, Eovist/Primovist (Bayer Healthcare) | Linear Ionic | 688 | 1.19 | 23.5 | 6.9/8.7 | 0.25 | 0.025 | Designed for liver imaging. Renal and biliary excretion. Very high relaxivity. EMA restricted to hepatobiliary imaging. |
| High Risk | Intermediate Risk | Low Risk |
|---|---|---|
| Gadodiamide | Gadobenate dimeglumine | Gadobutrol |
| Gadoversetamide | Gadoxetate disodium | Gadoteridol |
| Gadopentetate dimeglumine | Gadofosvest | Gadoterate meglumine |
| ACR Group I * | ACR Group II ** | ACR Group III *** |
|---|---|---|
| Gadodiamide Gadoversetamide Gadopentetate dimeglumine | Gadobenate dimeglumine | Gadoxetate disodium |
| Gadobutrol | ||
| Gadoteric acid | ||
| Gadoteridol |
| Clinical History | Signs | Symptoms |
|---|---|---|
| L-GBCA exposure (2–8 weeks—10 years after gadolinium uptake) Family history of NSF Renal: AKI, history of chronic kidney disease, kidney transplantation, or hemodialysis | Eye: Whitish-yellow plaques with vascular ectasia Skin changes: Hyperpigmentation, symmetrical lesions, rash-patterned plaques (red to violaceous lesions), superficial papules (beefy lesions in upper extremities), macules, nodules, skin thickening (cobble stoning or peau d’orange appearance) Renal: Volume overload, uremia Extremities: Limited range motion, joint contractures (finger, elbows, toes, and ankles), symmetric edema (inferior limbs) | Eye: Vision impairment, conjunctival injection, and white-yellow scleral plaques Skin: Pruritus, burning pain, new skin lesion, induration, and swelling Extremities: Edema, pain, and decreased mobility of the joints Urinary findings: Anuria, oliguria |
| Authors, Study Name | Year | Study Type | Total Number of Patients | GBCA | Number of Patients with Renal Impairment | NSF Cases at Maximum Follow-Up | Estimated NSF Incidence |
|---|---|---|---|---|---|---|---|
| Aneet et al. [39] | 2007 | Retrospective cohort | 467 (87 with gadolinium exposure) | Gadopentetate diglumine (L) and gadodiamide (L) | 87 patients with end-stage renal disease (patients in dialysis) | 3 | 4.3 cases per 1000 patients-year (overall NSF incidence) |
| Wang Y et al. [40] | 2011 | Retrospective cohort | 52,954 (after the 2007 Restrictive GBCA guidelines were implemented) | Gadopentetate diglumine (L) and gadobenate diglumine (L) | 6454 patients with GFR between 30–59 mL/min/m2; 36 patients with GFR lower than 30 mL/min/m2 | 0 | - |
| Prince MR et al. GARDIAN study [41] | 2016 | Prospective cohort | 23,708 | Gadobutrol (M) | 100 patients with moderate renal impairment (GFR: 30–59 mL/min/1.73 m2) and 31 patients with severe renal impairment (<30 mL/min/1.73 m2) | 0 | - |
| Soyer P et al. SECURE study [42] | 2017 | Prospective cohort | 35,499 | Gadorate meglumine (M) | 417 patients with moderate renal impairment (GFR: 30–59 mL/min/1.73 m2); 58 patients with severe renal impairment (GFR: 15–39 mL/min/1.73 m2); 7 patients with end-stage renal impairment (GFR: <15 mL/min/1.73 m2) or dialysis. | 0 | - |
| Michaely HJ et al. GRIP study [43] | 2017 | Prospective cohort | 908 | Gadobutrol (M) | 586 with moderate (GFR: 30–59 mL/min/1.73 m2) and 284 with severe renal impairment (<30 mL/min/1.73 m2) | 0 | - |
| Tsushima Y et al. [44] | 2018 | Prospective cohort | 3337 | Gadobutrol (M) | 356 patients with GFR between 45–59 mL/min/m2; 71 patients with GFR between 30–44 mL/min/m2; 4 patients with GFR between 15–29 mL/min/m2; 1 patient with GFR < 15 mL/min/m2 | 0 | - |
| Young LK [45] | 2019 | Retrospective cohort | 22,897 | Gadorate meglumine (M) | 2570 patients with moderate renal impairment (GFR: 30–59 mL/min/1.73 m2); 464 patients with severe renal impairment (GFR: 15–39 mL/min/1.73 m2); 123 patients with end-stage renal impairment (GFR: <15 mL/min/1.73 m2) or dialysis. | 0 | - |
| McWilliams RG et al. NSsaFe study [46] | 2020 | Prospective cohort | 540 | Gadorate meglumine (M) | 226 patients with moderate renal impairment (GFR: 30–59 mL/min/1.73 m2); 59 patients with severe renal impairment (GFR: 15–39 mL/min/1.73 m2); 58 patients with end-stage renal impairment (GFR: <15 mL/min/1.73 m2) or dialysis. | 0 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallo-Bernal, S.; Patino-Jaramillo, N.; Calixto, C.A.; Higuera, S.A.; Forero, J.F.; Lara Fernandes, J.; Góngora, C.; Gee, M.S.; Ghoshhajra, B.; Medina, H.M. Nephrogenic Systemic Fibrosis in Patients with Chronic Kidney Disease after the Use of Gadolinium-Based Contrast Agents: A Review for the Cardiovascular Imager. Diagnostics 2022, 12, 1816. https://doi.org/10.3390/diagnostics12081816
Gallo-Bernal S, Patino-Jaramillo N, Calixto CA, Higuera SA, Forero JF, Lara Fernandes J, Góngora C, Gee MS, Ghoshhajra B, Medina HM. Nephrogenic Systemic Fibrosis in Patients with Chronic Kidney Disease after the Use of Gadolinium-Based Contrast Agents: A Review for the Cardiovascular Imager. Diagnostics. 2022; 12(8):1816. https://doi.org/10.3390/diagnostics12081816
Chicago/Turabian StyleGallo-Bernal, Sebastian, Nasly Patino-Jaramillo, Camilo A. Calixto, Sergio A. Higuera, Julian F. Forero, Juliano Lara Fernandes, Carlos Góngora, Michael S. Gee, Brian Ghoshhajra, and Hector M. Medina. 2022. "Nephrogenic Systemic Fibrosis in Patients with Chronic Kidney Disease after the Use of Gadolinium-Based Contrast Agents: A Review for the Cardiovascular Imager" Diagnostics 12, no. 8: 1816. https://doi.org/10.3390/diagnostics12081816






