Using the Axial Oblique View of Computed Tomography (CT) in Evaluating Femoral Anteversion: A Comparative Cadaveric Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Digital Photographic Technique
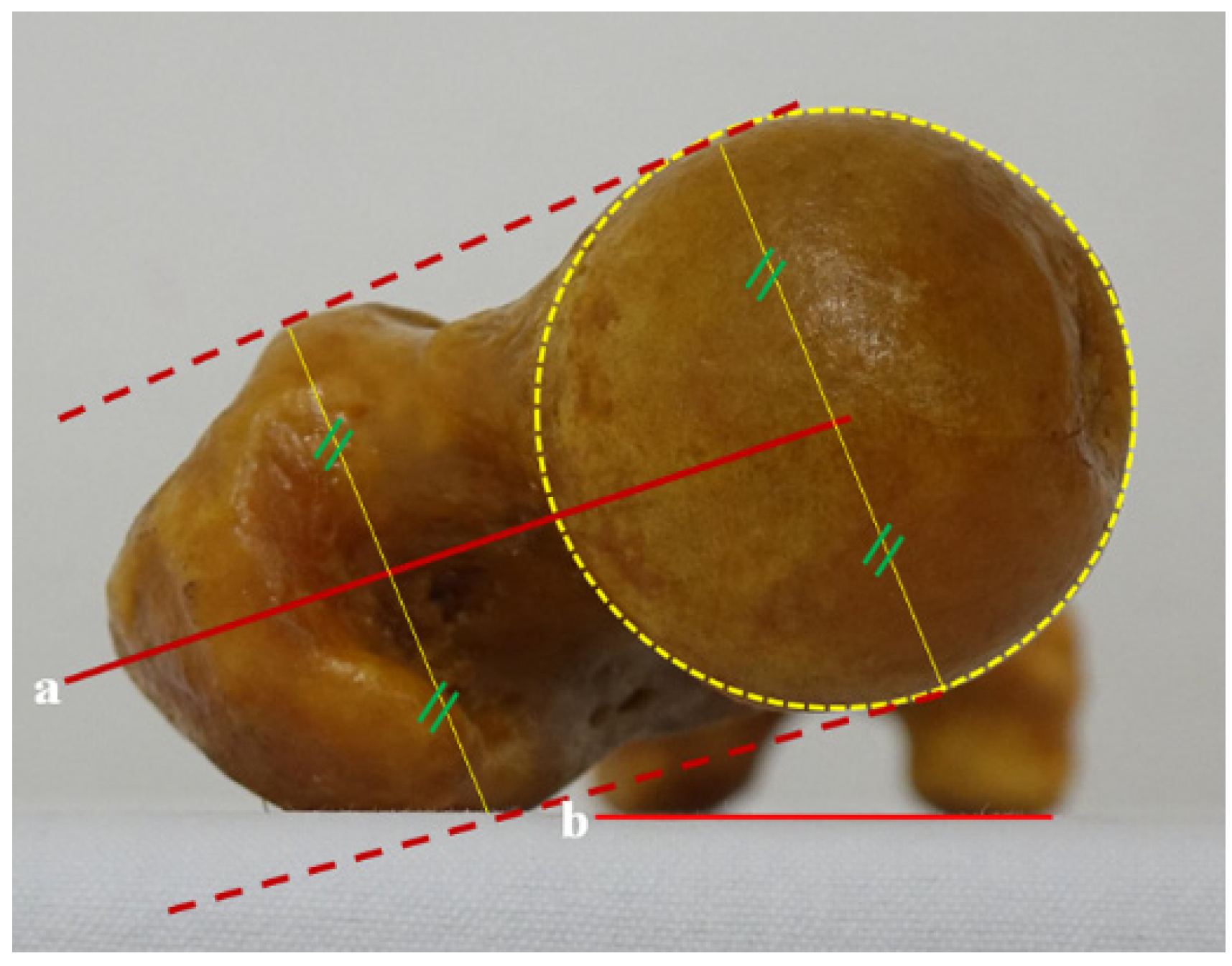
2.1.1. Head-Neck (H-N) Line
2.1.2. Head-Great Trochanter (H-G) Line
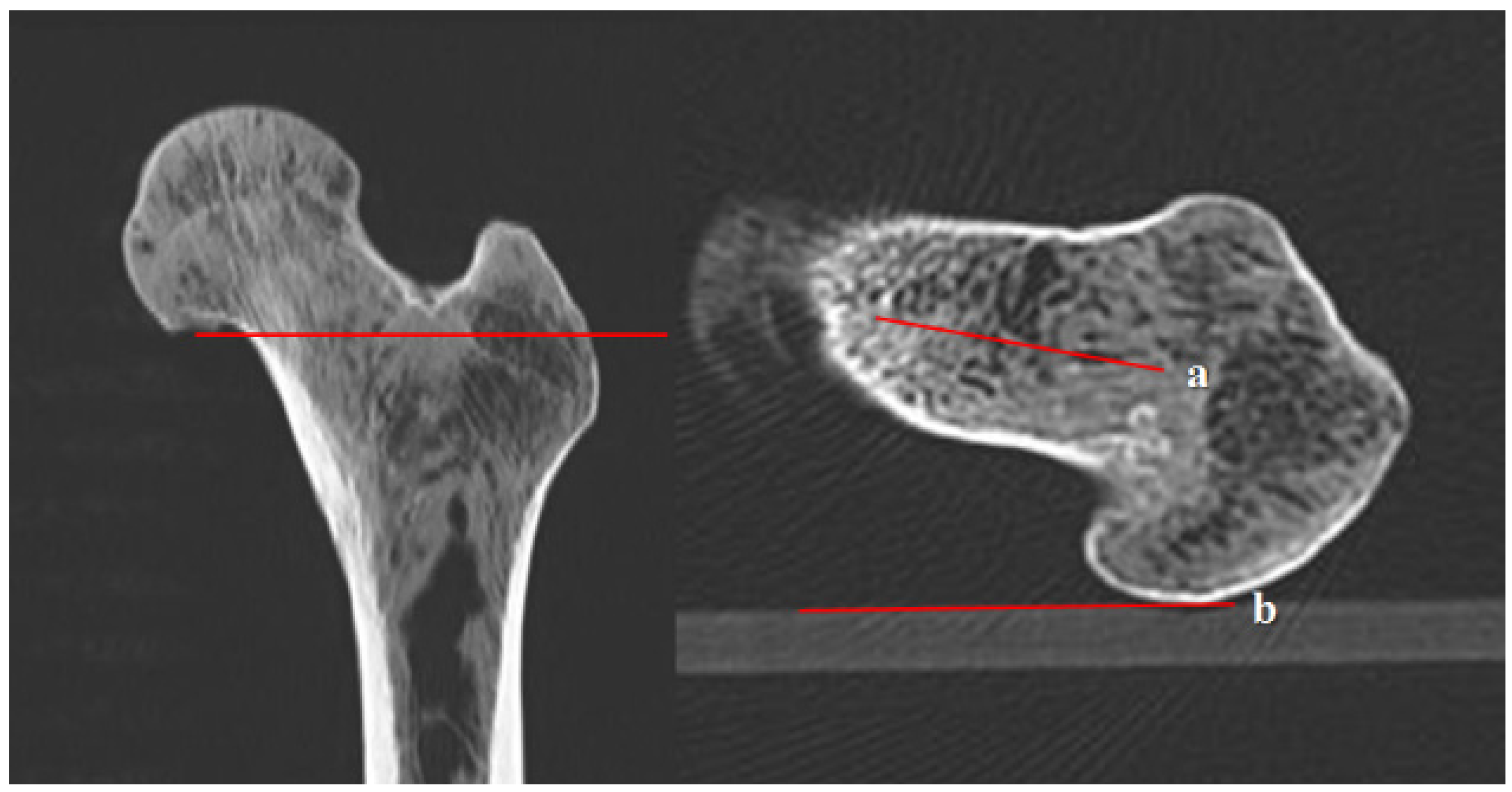
2.2. Computed Tomography (CT) Scans
2.2.1. A Line on a Conventional Transverse Section
2.2.2. B Line on a Conventional Transverse Section
2.2.3. C Line on an Axial Oblique Section
2.2.4. D Line on a 3D Conventional Reconstruction Section
2.2.5. E Line on a 3D Conventional Reconstruction Section
2.2.6. M Line on the 3D Volumetric Reconstruction Section
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sankar, W.N.; Neubuerger, C.O.; Moseley, C.F. Femoral anteversion in developmental dysplasia of the hip. J. Pediatr. Orthop. 2009, 29, 885–888. [Google Scholar] [CrossRef]
- Chung, C.Y.; Lee, K.M.; Park, M.S.; Lee, S.H.; Choi, I.H.; Cho, T.-J. Validity and reliability of measuring femoral anteversion and neck-shaft angle in patients with cerebral palsy. J. Bone Jt. Surg. Am. 2010, 92, 1195–1205. [Google Scholar] [CrossRef] [PubMed]
- Farhang, K.; Desai, R.; Wilber, J.H.; Cooperman, D.R.; Liu, R.W. An anatomical study of the entry point in the greater trochanter for intramedullary nailing. Bone Jt. J. 2014, 96, 1274–1281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winquist, R.A.; Hansen, S.T., Jr.; Clawson, D.K. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J. Bone Jt. Surg. Am. 1984, 66, 529–539. [Google Scholar] [CrossRef]
- Teo, P.C.; Kassim, A.Y.; Thevarajan, K. A 45-degree radiographic method for measuring the neck shaft angle and anteversion of the femur: A pilot study. J. Orthop. Surg. 2013, 21, 340–346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goyal, T.; Paul, S.; Choudhury, A.K.; Gupta, T. Assessment of acetabular component anteversion after total hip arthroplasty: Comparison of anteroposterior and cross-table lateral radiographs with computed tomography scans. Clin. Orthop. Surg. 2021, 13, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Kaku, N.; Tagomori, H.; Tsumura, H. Comparison of cup setting angle accuracy between computed tomography-based and computed tomography-free navigation in the same patients with Crowe’s classification I or II hip dysplasia. Clin. Orthop. Surg. 2021, 13, 144–151. [Google Scholar] [CrossRef]
- Kim, J.S.; Park, T.S.; Park, S.B.; Kim, J.S.; Kim, I.Y.; Kim, S.I. Measurement of femoral neck anteversion in 3D. Part 1: 3D imaging method. Med. Biol. Eng. Comput. 2000, 38, 603–609. [Google Scholar] [CrossRef]
- Gose, S.; Sakai, T.; Shibata, T.; Murase, T.; Yoshikawa, H.; Sugamoto, K. Morphometric analysis of the femur in cerebral palsy: 3-dimensional CT study. J. Pediatr. Orthop. 2010, 30, 568–574. [Google Scholar] [CrossRef]
- Park, K.K.; Tsai, T.-Y.; Dimitriou, D.; Kwon, Y.-M. Utility of preoperative femoral neck geometry in predicting femoral stem anteversion. J. Arthroplasty 2015, 30, 1079–1084. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, D.Y.; Oliveira, A.M.; Zou, K.H.; Snyder, B.D.; Kleinman, P.K. Axial oblique CT to assess femoral anteversion. Am. J. Roentgenol. 2010, 194, 1230–1233. [Google Scholar] [CrossRef] [PubMed]
- Folinais, D.; Thelen, P.; Delin, C.; Radier, C.; Catonne, Y.; Lazennec, J.Y. Measuring femoral and rotational alignment: EOS system versus computed tomography. Orthop. Traumatol. Surg. Res. 2013, 99, 509–516. [Google Scholar] [CrossRef] [Green Version]
- Kuo, T.Y.; Skedros, J.G.; Bloebaum, R.D. Measurement of femoral anteversion by biplane radiography and computed tomography imaging: Comparison with an anatomic reference. Investig. Radiol. 2003, 38, 221–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pomerantz, M.L.; Glaser, D.; Doan, J.; Kumar, S.; Edmonds, E.W. Three-dimensional biplanar radiography as a new means of accessing femoral version: A comparative study of EOS three-dimensional radiography versus computed tomography. Skelet. Radiol. 2015, 44, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Delin, C.; Silvera, S.; Bassinet, C.; Thelen, P.; Rehel, J.-L.; Legmann, P.; Folinais, D. Ionizing radiation doses during lower limb torsion and anteversion measurements by EOS stereoradiography and computed tomography. Eur. J. Radiol. 2014, 83, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Davids, J.R.; Marshall, A.D.; Blocker, E.R.; Frick, S.L.; Blackhurst, D.W.; Skewes, E. Femoral anteversion in children with cerebral palsy. Assessment with two and three-dimensional computed tomography scans. J. Bone Jt. Surg. Am. 2003, 85, 481–488. [Google Scholar] [CrossRef]
- Parikh, S.; Noyes, F.R. Patellofemoral disorders: Role of computed tomography and magnetic resonance imaging in defining abnormal rotational lower limb alignment. Sports Health 2011, 3, 158–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, C.; Cho, T.-J.; Shin, C.H.; Choi, I.H.; Yoo, W.J. Functional outcomes of hip arthroscopy for pediatric and adolescent hip disorders. Clin. Orthop. Surg. 2020, 12, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Rosskopf, A.B.; Ramseier, L.E.; Sutter, R.; Pfirrmann, C.W.A.; Buck, F.M. Femoral and tibial torsion measurement in children and adolescents: Comparison of 3D models based on low-dose biplanar radiography and low-dose CT. Am. J. Roentgenol. 2014, 202, W285–W291. [Google Scholar] [CrossRef] [PubMed]
- Buck, F.M.; Guggenberger, R.; Koch, P.P.; Pfirrmann, C.W.A. Femoral and tibial torsion measurements with 3D models based on low-dose biplanar radiographs in comparison with standard CT measurements. Am. J. Roentgenol. 2012, 199, W607–W612. [Google Scholar] [CrossRef]
- Adamczyk, E.; Sibiński, M.; Synder, M. The value of femoral anteversion angle measured clinically and on radiographs. Chir. Narzadow Ruchu Ortop. Pol. 2010, 75, 344–347. [Google Scholar] [PubMed]
- Botser, I.B.; Ozoude, G.C.; Martin, D.E.; Siddiqi, A.J.; Kuppuswami, S.; Domb, B.G. Femoral anteversion in the hip: Comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy 2012, 28, 619–627. [Google Scholar] [CrossRef]
- Gulan, G.; Matovinović, D.; Nemec, B.; Rubinić, D.; Ravlić-Gulan, J. Femoral neck anteversion: Values, development, measurement, common problems. Coll. Antropol. 2000, 24, 521–527. [Google Scholar] [PubMed]
- Günther, K.P.; Kessler, S.; Tomczak, R.; Pfeifer, P.; Puhl, W. Femoral anteversion: Significance of clinical methods and imaging techniques in the diagnosis in children and adolescents. Z. Orthop. Ihre Grenzgeb. 1996, 134, 295–301. [Google Scholar] [CrossRef]
- Koenig, J.K.; Pring, M.E.; Dwek, J.R. MR evaluation of femoral neck version and tibial torsion. Pediatr. Radiol. 2012, 42, 113–115. [Google Scholar] [CrossRef] [PubMed]
- Muhamad, A.R.; Freitas, J.M.; Bomar, J.D.; Dwek, J.; Hosalkar, H.S. CT and MRI lower extremity torsional profile studies: Measurement reproducibility. J. Child. Orthop. 2012, 6, 391–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stübig, T.; Min, W.; Arvani, M.; Hawi, N.; Krettek, C.; Citak, M. Accuracy of measurement of femoral anteversion in femoral shaft fractures using a computer imaging software: A cadaveric study. Arch. Orthop. Trauma Surg. 2012, 132, 613–616. [Google Scholar] [CrossRef] [PubMed]
- Yun, H.H.; Yoon, J.R.; Yang, J.-H.; Song, S.Y.; Park, S.B.; Lee, J.W. A validation study for estimation of femoral anteversion using the posterior lesser trochanter line: An analysis of computed tomography measurement. J. Arthroplast. 2013, 28, 1776–1780. [Google Scholar] [CrossRef] [PubMed]
- Lausten, G.S.; Jørgensen, F.; Boesen, J. Measurement of anteversion of the femoral neck. Ultrasound and computerised tomography compared. J. Bone Jt. Surg. Br. 1989, 71, 237–239. [Google Scholar] [CrossRef] [PubMed]
- Unnanuntana, A.; Toogood, P.; Hart, D.; Cooperman, D.; Grant, R.E. Evaluation of proximal femoral geometry using digital photographs. J. Orthop. Res. 2010, 28, 1399–1404. [Google Scholar] [CrossRef]








| Line | ICC |
|---|---|
| H-N | 0.956 |
| H-G | 0.982 |
| A | 0.994 |
| B | 0.996 |
| C | 0.986 |
| D | 0.965 |
| Actual Gross Anteversion | CT Anteversion | p-Value |
|---|---|---|
| Reference Line (Mean ± SE) | Reference Line (Mean ± SE) | |
| H-N line (10.43 ± 1.12) | A line (16.12 ± 1.94) | 0.000 * |
| B line (10.34 ± 1.86) | 0.925 | |
| C line (17.47 ± 1.46) | 0.000 * | |
| D line (22.80 ± 1.66) | 0.000 * | |
| E line (21.31 ± 1.66) | 0.000 * | |
| M line (8.59 ± 1.31) | 0.122 | |
| H-G line (19.50 ± 1.00) | A line (16.12 ± 1.94) | 0.021 * |
| B line (10.34 ± 1.86) | 0.000 * | |
| C line (17.47 ± 1.46) | 0.065 | |
| D line (22.80 ± 1.66) | 0.010 * | |
| E line (21.31 ± 1.66) | 0.021 * | |
| M line (8.59 ± 1.31) | 0.000 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, K.-S.; Yon, C.-J.; Heo, Y.-R.; Lee, J.-H.; Lee, S.-B.; Ko, Y.-K.; Lee, K.-J.; Lee, S.-W. Using the Axial Oblique View of Computed Tomography (CT) in Evaluating Femoral Anteversion: A Comparative Cadaveric Study. Diagnostics 2022, 12, 1820. https://doi.org/10.3390/diagnostics12081820
Song K-S, Yon C-J, Heo Y-R, Lee J-H, Lee S-B, Ko Y-K, Lee K-J, Lee S-W. Using the Axial Oblique View of Computed Tomography (CT) in Evaluating Femoral Anteversion: A Comparative Cadaveric Study. Diagnostics. 2022; 12(8):1820. https://doi.org/10.3390/diagnostics12081820
Chicago/Turabian StyleSong, Kwang-Soon, Chang-Jin Yon, Yu-Ran Heo, Jae-Ho Lee, Seung-Bo Lee, Yeon-Kyoung Ko, Kyung-Jae Lee, and Si-Wook Lee. 2022. "Using the Axial Oblique View of Computed Tomography (CT) in Evaluating Femoral Anteversion: A Comparative Cadaveric Study" Diagnostics 12, no. 8: 1820. https://doi.org/10.3390/diagnostics12081820







