Breath Volatile Organic Compounds in Surveillance of Gastric Cancer Patients following Radical Surgical Management
Abstract
:1. Introduction
2. Materials and Methods
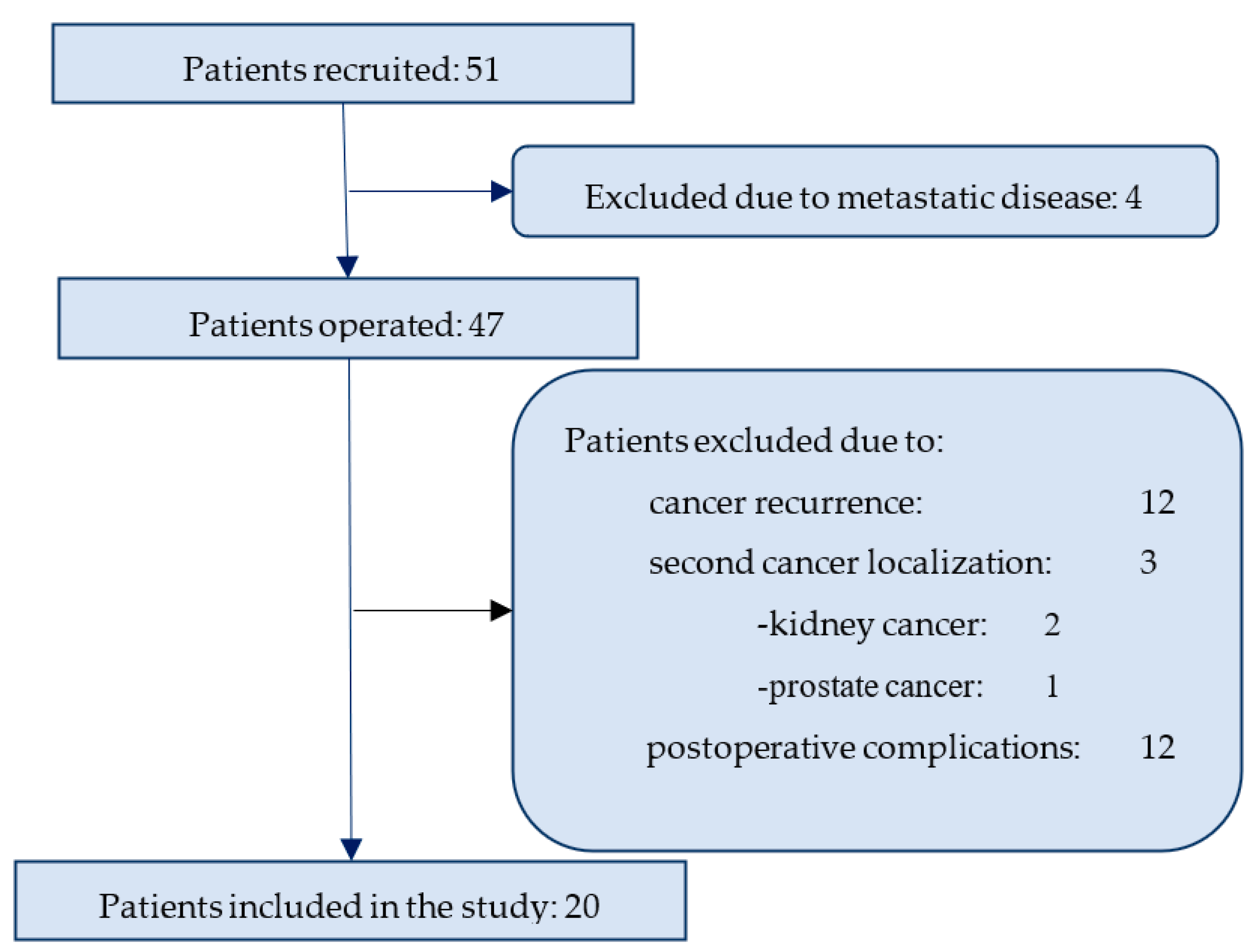
2.1. Study Population
2.2. Sampling Protocol
2.3. Breath Collection
2.4. Chemical Analysis
2.5. Statistical Analysis
3. Results
3.1. Chemical Analysis
3.2. Nanosensor Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Isobe, Y.; Nashimoto, A.; Akazawa, K.; Oda, I.; Hayashi, K.; Miyashiro, I.; Katai, H.; Tsujitani, S.; Kodera, Y.; Seto, Y.; et al. Gastric cancer treatment in Japan: 2008 annual report of the JGCA nationwide registry. Gastric Cancer 2011, 14, 301–316. [Google Scholar] [CrossRef] [PubMed]
- Bollschweiler, E.; Boettcher, K.; Hoelscher, A.H.; Sasako, M.; Kinoshita, T.; Maruyama, K.; Siewert, J.R. Is the prognosis for Japanese and German patients with gastric cancer really different? Cancer 1993, 71, 2918–2925. [Google Scholar] [CrossRef]
- Morgan, E.; Arnold, M.; Camargo, M.C.; Gini, A.; Kunzmann, A.T.; Matsuda, T.; Meheus, F.; Verhoeven, R.H.A.; Vignat, J.; Laversanne, M.; et al. The current and future incidence and mortality of gastric cancer in 185 countries, 2020–2040: A population-based modelling study. ClinicalMedicine 2022, 47, 101404. [Google Scholar] [CrossRef]
- Orditura, M.; Galizia, G.; Sforza, V.; Gambardella, V.; Fabozzi, A.; Laterza, M.M.; Andreozzi, F.; Ventriglia, J.; Savastano, B.; Mabilia, A.; et al. Treatment of gastric cancer. World J. Gastroenterol. 2014, 20, 1635–1649. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.X.; Moses, L.E.; Squires, M.H., 3rd; Poultsides, G.A.; Votanopoulos, K.; Weber, S.M.; Bloomston, M.; Pawlik, T.M.; Hawkins, W.G.; Linehan, D.C.; et al. Factors Associated With Recurrence and Survival in Lymph Node-negative Gastric Adenocarcinoma: A 7-Institution Study of the US Gastric Cancer Collaborative. Ann. Surg. 2015, 262, 999–1005. [Google Scholar] [CrossRef] [PubMed]
- Ajani, J.A.; D’Amico, T.A.; Almhanna, K.; Bentrem, D.J.; Chao, J.; Das, P.; Denlinger, C.S.; Fanta, P.; Farjah, F.; Fuchs, C.S.; et al. Gastric Cancer, Version 3.2016, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2016, 14, 1286–1312. [Google Scholar] [CrossRef] [PubMed]
- Aurello, P.; Petrucciani, N.; Antolino, L.; Giulitti, D.; D’Angelo, F.; Ramacciato, G. Follow-up after curative resection for gastric cancer: Is it time to tailor it? World J. Gastroenterol. 2017, 23, 3379–3387. [Google Scholar] [CrossRef] [PubMed]
- Baiocchi, G.L.; Marrelli, D.; Verlato, G.; Morgagni, P.; Giacopuzzi, S.; Coniglio, A.; Marchet, A.; Rosa, F.; Capponi, M.G.; Di Leo, A.; et al. Follow-up after gastrectomy for cancer: An appraisal of the Italian research group for gastric cancer. Ann. Surg. Oncol. 2014, 21, 2005–2011. [Google Scholar] [CrossRef]
- Lordick, F.; Carneiro, F.; Cascinu, S.; Fleitas, T.; Haustermans, K.; Piessen, G.; Vogel, A.; Smyth, E.C. on behalf of the ESMO Guidelines Committee. Gastric cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2022, 33, 1005–1020. [Google Scholar] [CrossRef] [PubMed]
- Koppula, B.R.; Fine, G.C.; Salem, A.E.; Covington, M.F.; Wiggins, R.H.; Hoffman, J.M.; Morton, K.A. PET-CT in Clinical Adult Oncology: III. Gastrointestinal Malignancies. Cancers 2022, 14, 2668. [Google Scholar] [CrossRef] [PubMed]
- Pleil, J.D.; Stiegel, M.A.; Risby, T.H. Clinical breath analysis: Discriminating between human endogenous compounds and exogenous (environmental) chemical confounders. J. Breath Res. 2013, 7, 017107. [Google Scholar] [CrossRef] [PubMed]
- Krilaviciute, A.; Heiss, J.A.; Leja, M.; Kupcinskas, J.; Haick, H.; Brenner, H. Detection of cancer through exhaled breath: A systematic review. Oncotarget 2015, 6, 38643–38657. [Google Scholar] [CrossRef] [PubMed]
- Sola Martinez, R.A.; Pastor Hernandez, J.M.; Yanes Torrado, O.; Canovas Diaz, M.; de Diego Puente, T.; Vinaixa Crevillent, M. Exhaled volatile organic compounds analysis in clinical pediatrics: A systematic review. Pediatr. Res. 2021, 89, 1352–1363. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, W.M.; Lawal, O.; Nijsen, T.M.; Goodacre, R.; Fowler, S.J. Exhaled Volatile Organic Compounds of Infection: A Systematic Review. ACS Infect. Dis. 2017, 3, 695–710. [Google Scholar] [CrossRef]
- Sun, X.; Shao, K.; Wang, T. Detection of volatile organic compounds (VOCs) from exhaled breath as noninvasive methods for cancer diagnosis. Anal. Bioanal. Chem. 2016, 408, 2759–2780. [Google Scholar] [CrossRef]
- Amal, H.; Leja, M.; Funka, K.; Skapars, R.; Sivins, A.; Ancans, G.; Liepniece-Karele, I.; Kikuste, I.; Lasina, I.; Haick, H. Detection of precancerous gastric lesions and gastric cancer through exhaled breath. Gut 2016, 65, 400–407. [Google Scholar] [CrossRef]
- Xu, Z.Q.; Broza, Y.Y.; Ionsecu, R.; Tisch, U.; Ding, L.; Liu, H.; Song, Q.; Pan, Y.Y.; Xiong, F.X.; Gu, K.S.; et al. A nanomaterial-based breath test for distinguishing gastric cancer from benign gastric conditions. Br. J. Cancer 2013, 108, 941–950. [Google Scholar] [CrossRef]
- Shehada, N.; Bronstrup, G.; Funka, K.; Christiansen, S.; Leja, M.; Haick, H. Ultrasensitive silicon nanowire for real-world gas sensing: Noninvasive diagnosis of cancer from breath volatolome. Nano Lett. 2015, 15, 1288–1295. [Google Scholar] [CrossRef]
- Leja, M.; Kortelainen, J.M.; Polaka, I.; Turppa, E.; Mitrovics, J.; Padilla, M.; Mochalski, P.; Shuster, G.; Pohle, R.; Kashanin, D.; et al. Sensing gastric cancer via point-of-care sensor breath analyzer. Cancer 2021, 127, 1286–1292. [Google Scholar] [CrossRef]
- Markar, S.R.; Wiggins, T.; Antonowicz, S.; Chin, S.T.; Romano, A.; Nikolic, K.; Evans, B.; Cunningham, D.; Mughal, M.; Lagergren, J.; et al. Assessment of a Noninvasive Exhaled Breath Test for the Diagnosis of Oesophagogastric Cancer. JAMA Oncol. 2018, 4, 970–976. [Google Scholar] [CrossRef]
- Zhang, J.; Tian, Y.; Luo, Z.; Qian, C.; Li, W.; Duan, Y. Breath volatile organic compound analysis: An emerging method for gastric cancer detection. J. Breath Res. 2021, 15, 044002. [Google Scholar] [CrossRef] [PubMed]
- Duran-Acevedo, C.M.; Jaimes-Mogollon, A.L.; Gualdron-Guerrero, O.E.; Welearegay, T.G.; Martinez-Marin, J.D.; Caceres-Tarazona, J.M.; Sanchez-Acevedo, Z.C.; Beleno-Saenz, K.J.; Cindemir, U.; Osterlund, L.; et al. Exhaled breath analysis for gastric cancer diagnosis in Colombian patients. Oncotarget 2018, 9, 28805–28817. [Google Scholar] [CrossRef] [PubMed]
- Gasenko, E.; Leja, M.; Polaka, I.; Hegmane, A.; Murillo, R.; Bordin, D.; Link, A.; Kulju, M.; Mochalski, P.; Shani, G.; et al. How do international gastric cancer prevention guidelines influence clinical practice globally? Eur. J. Cancer Prev. 2020, 29, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Baiocchi, G.L.; D’Ugo, D.; Coit, D.; Hardwick, R.; Kassab, P.; Nashimoto, A.; Marrelli, D.; Allum, W.; Berruti, A.; Chandramohan, S.M.; et al. Follow-up after gastrectomy for cancer: The Charter Scaligero Consensus Conference. Gastric Cancer 2016, 19, 15–20. [Google Scholar] [CrossRef]
- Japanese Gastric Cancer Asscociation. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer 2021, 24, 1–21. [Google Scholar] [CrossRef]
- Henry, N.L.; Hayes, D.F. Cancer biomarkers. Mol. Oncol. 2012, 6, 140–146. [Google Scholar] [CrossRef]
- Gion, M.; Trevisiol, C.; Fabricio, A.S.C. State of the art and trends of circulating cancer biomarkers. Int. J. Biol. Markers 2020, 35 (Suppl. 1), 12–15. [Google Scholar] [CrossRef]
- Leja, M.; Line, A. Early detection of gastric cancer beyond endoscopy-new methods. Best Pract. Res. Clin. Gastroenterol. 2021, 50–51, 101731. [Google Scholar] [CrossRef]
- Leja, M.; Amal, H.; Lasina, I.; Skapars, R.; Sivins, A.; Ancans, G.; Tolmanis, I.; Vanags, A.; Kupcinskas, J.; Ramonaite, R.; et al. Analysis of the effects of microbiome-related confounding factors on the reproducibility of the volatolomic test. J. Breath Res. 2016, 10, 037101. [Google Scholar] [CrossRef]
- Scheepers, M.; Al-Difaie, Z.; Brandts, L.; Peeters, A.; van Grinsven, B.; Bouvy, N.D. Diagnostic Performance of Electronic Noses in Cancer Diagnoses Using Exhaled Breath: A Systematic Review and Meta-analysis. JAMA Netw. Open 2022, 5, e2219372. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Li, J.; Xiong, X.; Hao, T.; Zhang, C.; Gao, Z.; Zhong, L.; Zhao, Y. Volatile organic compounds as a potential screening tool for neoplasm of the digestive system: A meta-analysis. Sci. Rep. 2021, 11, 23716. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Mou, Y.; Hu, B. Diagnostic Ability of Volatile Organic Compounds in Digestive Cancer: A Systematic Review With Meta-Analysis. Clin. Med. Insights Oncol. 2022, 16, 11795549221105027. [Google Scholar] [CrossRef]
- Broza, Y.Y.; Kremer, R.; Tisch, U.; Gevorkyan, A.; Shiban, A.; Best, L.A.; Haick, H. A nanomaterial-based breath test for short-term follow-up after lung tumor resection. Nanomedicine 2013, 9, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Poli, D.; Carbognani, P.; Corradi, M.; Goldoni, M.; Acampa, O.; Balbi, B.; Bianchi, L.; Rusca, M.; Mutti, A. Exhaled volatile organic compounds in patients with non-small cell lung cancer: Cross sectional and nested short-term follow-up study. Respir. Res. 2005, 6, 71. [Google Scholar] [CrossRef]
- Poli, D.; Goldoni, M.; Caglieri, A.; Ceresa, G.; Acampa, O.; Carbognani, P.; Rusca, M.; Corradi, M. Breath analysis in non small cell lung cancer patients after surgical tumour resection. Acta Biomed. 2008, 79 (Suppl. 1), 64–72. [Google Scholar]
- Aslam, M.A.; Xue, C.; Chen, Y.; Zhang, A.; Liu, M.; Wang, K.; Cui, D. Breath analysis based early gastric cancer classification from deep stacked sparse autoencoder neural network. Sci. Rep. 2021, 11, 4014. [Google Scholar] [CrossRef] [PubMed]
- Polaka, I.; Bhandari, M.P.; Mezmale, L.; Anarkulova, L.; Veliks, V.; Sivins, A.; Lescinska, A.M.; Tolmanis, I.; Vilkoite, I.; Ivanovs, I.; et al. Modular Point-of-Care Breath Analyzer and Shape Taxonomy-Based Machine Learning for Gastric Cancer Detection. Diagnostics 2022, 12, 491. [Google Scholar] [CrossRef]
- Siddikov, D.R.; Bobakulov, K.M.; Nishanbaev, S.Z.; Abdullaev, N.D. Secondary Metabolites from Aerial Parts of Several Geranium Species Growing in Uzbekistan and their Adaptive Role. Chem. Nat. Compd. 2015, 51, 793–796. [Google Scholar] [CrossRef]
- Tanod, W.A.; Yanuhar, U.; Maftuch; Putra, M.Y.; Risjani, Y. Screening of NO Inhibitor Release Activity from Soft Coral Extracts Origin Palu Bay, Central Sulawesi, Indonesia. Antiinflamm. Antiallergy Agents Med. Chem. 2019, 18, 126–141. [Google Scholar] [CrossRef]
- Chao, C.-H.; Wen, Z.-H.; Su, J.-H.; Chen, I.M.; Huang, H.-C.; Dai, C.-F.; Sheu, J.-H. Further study on anti-inflammatory oxygenated steroids from the octocoral Dendronephthya griffini. Steroids 2008, 73, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Orabi, S.H.; Al-Sabbagh, E.S.; Khalifa, H.K.; Mohamed, M.A.E.; Elhamouly, M.; Gad-Allah, S.M.; Abdel-Daim, M.M.; Eldaim, M.A.A. Commiphora myrrha Resin Alcoholic Extract Ameliorates High Fat Diet Induced Obesity via Regulation of UCP1 and Adiponectin Proteins Expression in Rats. Nutrients 2020, 12, 803. [Google Scholar] [CrossRef] [PubMed]
- Degirmenci, H.; Erkurt, H. Relationship between volatile components, antimicrobial and antioxidant properties of the essential oil, hydrosol and extracts of Citrus aurantium L. flowers. J. Infect. Public Health 2020, 13, 58–67. [Google Scholar] [CrossRef]
- Rogers, W.R.; McCullough, B.; Caton, J.E. Cigarette smoking by baboons: In vivo assessment of particulate inhalation using bronchoalveolar lavage to recover [14C]dotriacontane. Toxicology 1981, 20, 309–321. [Google Scholar] [CrossRef]
- Peng, G.; Hakim, M.; Broza, Y.Y.; Billan, S.; Abdah-Bortnyak, R.; Kuten, A.; Tisch, U.; Haick, H. Detection of lung, breast, colorectal, and prostate cancers from exhaled breath using a single array of nanosensors. Br. J. Cancer 2010, 103, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Peng, G.; Tisch, U.; Adams, O.; Hakim, M.; Shehada, N.; Broza, Y.Y.; Billan, S.; Abdah-Bortnyak, R.; Kuten, A.; Haick, H. Diagnosing lung cancer in exhaled breath using gold nanoparticles. Nat. Nanotechnol. 2009, 4, 669–673. [Google Scholar] [CrossRef]
- Helmig, D.; Vierling, L. Water adsorption capacity of the solid adsorbents Tenax TA, Tenax GR, Carbotrap, Carbotrap C, Carbosieve SIII, and Carboxen 569 and water management techniques for the atmospheric sampling of volatile organic trace gases. Anal. Chem. 1995, 67, 4380–4386. [Google Scholar] [CrossRef]
- Broza, Y.Y.; Haick, H. Nanomaterial-based sensors for detection of disease by volatile organic compounds. Nanomedicine 2013, 8, 785–806. [Google Scholar] [CrossRef]
- Konvalina, G.; Haick, H. Effect of humidity on nanoparticle-based chemiresistors: A comparison between synthetic and real-world samples. ACS. Appl. Mater. Interf. 2011, 4, 317–325. [Google Scholar] [CrossRef]
- Konvalina, G.; Haick, H. Sensors for breath testing: From nanomaterials to comprehensive disease detection. Acc. Chem. Res. 2014, 47, 66–76. [Google Scholar] [CrossRef]
- Tisch, U.; Haick, H. Sensors Based on Monolayer-Capped Metal Nanoparticles. In Nanstructured Materials; Volme 2, Momentum Press, LLC: New York, NY, USA, 2010; Chapter 4; pp. 141–202. [Google Scholar]
- Amann, A.; Spanel, P.; Smith, D. Breath analysis: The approach towards clinical applications. Mini-Rev. Med. Chem. 2007, 7, 115–129. [Google Scholar] [CrossRef] [PubMed]
- Amann, A.; Miekisch, W.; Pleil, J.; Risby, T.; Schubert, J. Methodological issues of sample collection and analysis of exhaled breath. Eur. Resp. Soc. Monogr. 2010, 49, 96–114. [Google Scholar]
- Hakim, M.; Broza, Y.Y.; Barash, O.; Peled, N.; Phillips, M.; Amann, A.; Haick, H. Volatile organic compounds of lung cancer and possible biochemical pathways. Chem. Rev. 2012, 112, 5949–5966. [Google Scholar] [CrossRef] [PubMed]
- Filipiak, W.; Sponring, A.; Filipiak, A.; Ager, C.; Schubert, J.; Miekisch, W.; Amann, A.; Troppmair, A. TD-GC-MS analysis of volatile metabolites of human lung cancer and normal cells in vitro. Cancer. Epidemiol. Biomarkers. Prev. 2010, 19, 182–195. [Google Scholar] [CrossRef] [PubMed]
- Tisch, U.; Haick, H. Nanomaterials for cross-reactive sensor arrays. Bull. MRS 2010, 35, 797–803. [Google Scholar] [CrossRef]
- Dovgolevsky, E.; Haick, H. Direct observation of the transition point between quasi-spherical and cubic nanoparticles in a two-step seed-mediated growth method. Small 2008, 4, 2059–2066. [Google Scholar] [CrossRef]
- Dovgolevsky, E.; Tisch, U.; Haick, H. Chemically sensitive resistors based on monolayer-capped cubic nanoparticles: Towards configurable nanoporous sensors. Small 2009, 5, 1158–1161. [Google Scholar] [CrossRef]
- Dovgolevsky, E.; Konvalina, G.; Tisch, U.; Haick, H. Monolayer-capped cubic platinum nanoparticles for sensing nonpolar analytes in highly humid atmospheres. J. Phys. Chem. C. 2010, 114, 14042–14049. [Google Scholar] [CrossRef]
- Zilberman, Y.; Ionescu, R.; Feng, X.; Müllen, K.; Haick, H. Nanoarray of polycyclic aromatic hydrocarbons and carbon nanotubes for accurate and predictive detection in real-world environmental humidity. ACS Nano 2011, 5, 6743–6753. [Google Scholar] [CrossRef]
- Zilberman, Y.; Tisch, U.; Pisula, W.; Feng, X.; Müllen, K.; Haick, H. Spongelike structures of hexa-peri-hexabenzocoronene derivatives enhance the sensitivity of chemiresistive carbon nanotubes to nonpolar volatile organic compounds of cancer. Langmuir 2009, 25, 5411–5416. [Google Scholar] [CrossRef]
- Peng, G.; Trock, E.; Haick, H. Detecting simulated patterns of lung cancer biomarkers by random network of single-walled carbon nanotubes coated with nonpolymeric organic materials. Nano Lett. 2008, 8, 3631–3635. [Google Scholar] [CrossRef] [PubMed]


| T0 Preop | T1 (3 mo) | T2 (6 mo) | T3 (9 mo) | T4 (12 mo) | T5 (18 mo) | T6 (24 mo) | T7 (30 mo) | T8 (36 mo) | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| nanosensors | 18 | 14 | 15 | 10 | 11 | 10 | 7 | 7 | 6 | 98 |
| GC-MS | 19 | 14 | 16 | 10 | 11 | 10 | 7 | 7 | 6 | 100 |
| Patients involved | 20 | 14 | 17 | 10 | 11 | 11 | 7 | 7 | 7 | 104 |
| Number or Mean (Standard Deviation) | % | |
|---|---|---|
| Total Number of Patients | 20 | |
| Sex, n | ||
| Male | 16 | 80 |
| Female | 4 | 20 |
| Mean age, y | 61.5 ± 9.9 | |
| Smoking, n | ||
| Smoker | 7 | 35 |
| Ex-smoker | 8 | 40 |
| Non-smoker | 5 | 25 |
| Cancer stage, n | ||
| Stage I | 7 | 35 |
| Stage II | 8 | 40 |
| Stage III | 5 | 25 |
| Cancer type, n | ||
| Intestinal | 5 | 25 |
| Diffuse | 6 | 30 |
| Mixed | 9 | 45 |
| Cancer differentiation grade, n | ||
| Well-differentiated | 1 | 5 |
| Moderately differentiated | 11 | 55 |
| Poorly differentiated | 7 | 35 |
| Undifferentiated | 1 | 5 |
| The operation type, n | ||
| Total gastrectomy | 14 | 70 |
| Distal gastrectomy | 6 | 30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Škapars, R.; Gašenko, E.; Broza, Y.Y.; Sīviņš, A.; Poļaka, I.; Bogdanova, I.; Pčolkins, A.; Veliks, V.; Folkmanis, V.; Lesčinska, A.; et al. Breath Volatile Organic Compounds in Surveillance of Gastric Cancer Patients following Radical Surgical Management. Diagnostics 2023, 13, 1670. https://doi.org/10.3390/diagnostics13101670
Škapars R, Gašenko E, Broza YY, Sīviņš A, Poļaka I, Bogdanova I, Pčolkins A, Veliks V, Folkmanis V, Lesčinska A, et al. Breath Volatile Organic Compounds in Surveillance of Gastric Cancer Patients following Radical Surgical Management. Diagnostics. 2023; 13(10):1670. https://doi.org/10.3390/diagnostics13101670
Chicago/Turabian StyleŠkapars, Roberts, Evita Gašenko, Yoav Y. Broza, Armands Sīviņš, Inese Poļaka, Inga Bogdanova, Andrejs Pčolkins, Viktors Veliks, Valdis Folkmanis, Anna Lesčinska, and et al. 2023. "Breath Volatile Organic Compounds in Surveillance of Gastric Cancer Patients following Radical Surgical Management" Diagnostics 13, no. 10: 1670. https://doi.org/10.3390/diagnostics13101670
APA StyleŠkapars, R., Gašenko, E., Broza, Y. Y., Sīviņš, A., Poļaka, I., Bogdanova, I., Pčolkins, A., Veliks, V., Folkmanis, V., Lesčinska, A., Liepniece-Karele, I., Haick, H., Rumba-Rozenfelde, I., & Leja, M. (2023). Breath Volatile Organic Compounds in Surveillance of Gastric Cancer Patients following Radical Surgical Management. Diagnostics, 13(10), 1670. https://doi.org/10.3390/diagnostics13101670









