The Impact of ACE Gene Variants on Acute-Phase Reactants in Children with Rheumatic Heart Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Laboratory Testing
2.2. Sample Preparation and Genotyping
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Association with RHD
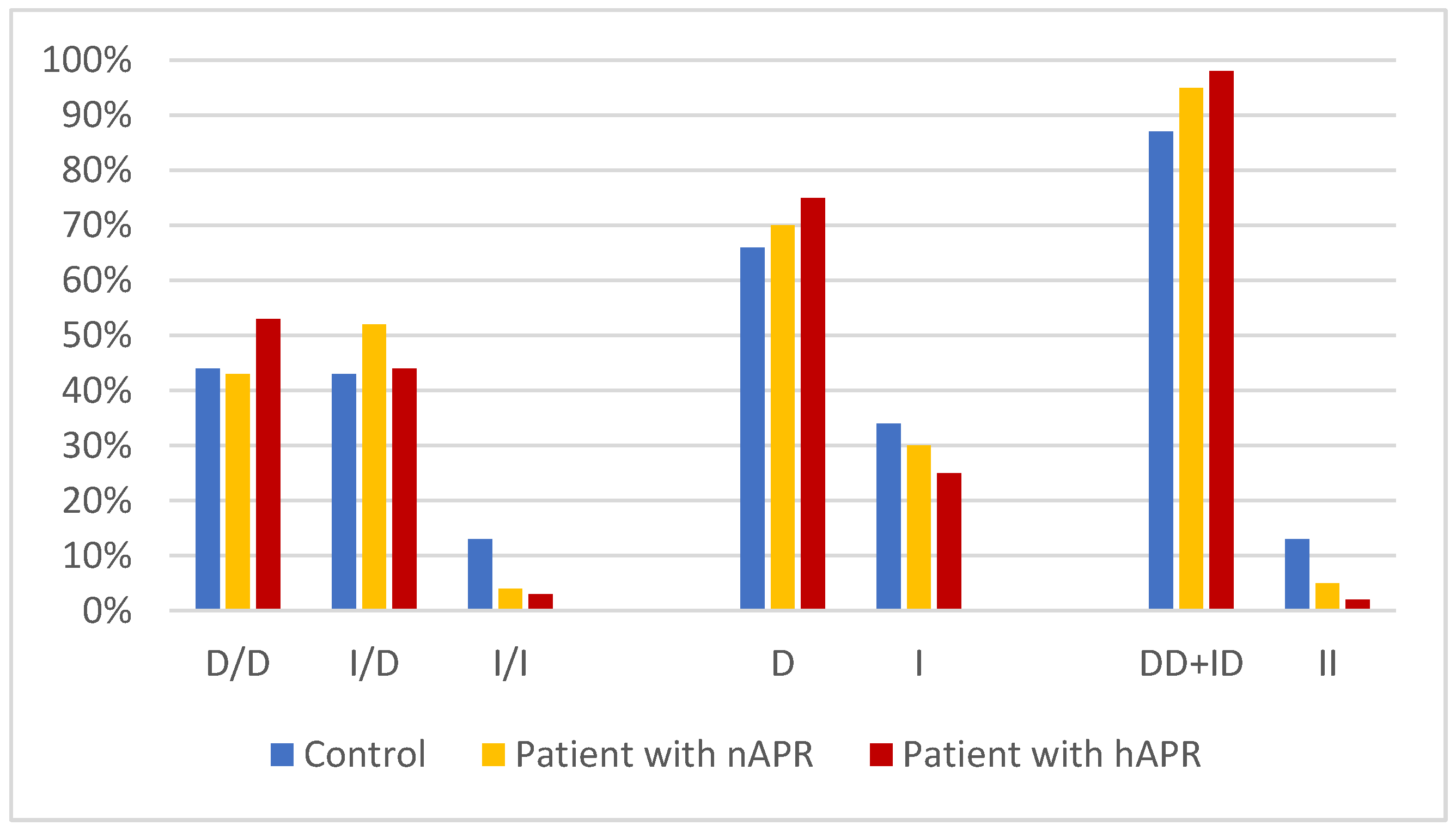
3.3. Association with ARP
3.4. Association with Disease Subtypes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marijon, E.; Mirabel, M.; Celermajer, D.S.; Jouven, X. Rheumatic heart disease. Lancet 2012, 379, 953–964. [Google Scholar] [CrossRef] [PubMed]
- Carapetis, J.R. Rheumatic Heart Disease in Asia. Circulation 2008, 118, 2748–2753. [Google Scholar] [CrossRef]
- Rwebembera, J.; Nascimento, B.R.; Minja, N.W.; de Loizaga, S.; Aliku, T.; dos Santos, L.P.A.; Galdino, B.F.; Corte, L.S.; Silva, V.R.; Chang, A.Y.; et al. Recent Advances in the Rheumatic Fever and Rheumatic Heart Disease Continuum. Pathogens 2022, 11, 179. [Google Scholar] [CrossRef] [PubMed]
- Bremner, J.; Frost, A.; Haub, C.; Mather, M.; Ringheim, K.; Zuehlke, E. World Population Highlights: Key Findings from PRB’s 2010 World Population Data Sheet. Popul. Bull. 2010, 65, 1–12. [Google Scholar]
- Abdallah, A.M.; Abu-Madi, M. The Genetic Control of the Rheumatic Heart: Closing the Genotype-Phenotype Gap. Front. Med. 2021, 8, 611036. [Google Scholar] [CrossRef] [PubMed]
- Muhamed, B.; Parks, T.; Sliwa, K. Genetics of rheumatic fever and rheumatic heart disease. Nat. Rev. Cardiol. 2020, 17, 145–154. [Google Scholar] [CrossRef]
- Abdallah, A.M.; Al-Mazroea, A.H.; Al-Harbi, W.N.; Al-Harbi, N.A.; Eldardear, A.E.; Almohammadi, Y.; Al-Harbi, K.M. Impact of MIF Gene Promoter Variations on Risk of Rheumatic Heart Disease and Its Age of Onset in Saudi Arabian Patients. Front. Immunol. 2016, 7, 98. [Google Scholar] [CrossRef] [PubMed]
- Burke, R.J.; Chang, C. Diagnostic criteria of acute rheumatic fever. Autoimmun. Rev. 2014, 13, 503–507. [Google Scholar] [CrossRef]
- Gewitz, M.H.; Baltimore, R.S.; Tani, L.Y.; Sable, C.A.; Shulman, S.T.; Carapetis, J.; Remenyi, B.; Taubert, K.A.; Bolger, A.F.; Beerman, L.; et al. Revision of the Jones Criteria for the Diagnosis of Acute Rheumatic Fever in the Era of Doppler Echocardiography: A Scientific Statement from the American Heart Association. Circulation 2015, 131, 1806–1818. [Google Scholar] [CrossRef]
- Gölbasi, Z.; Uçar, Ö.; Keles, T.; Sahin, A.; Çagli, K.; Çamsari, A.; Diker, E.; Aydogdu, S. Increased Levels of High Sensitive C-reactive Protein in Patients with Chronic Rheumatic Valve Disease: Evidence of Ongoing Inflammation. Eur. J. Heart Fail. 2002, 4, 593–595. [Google Scholar] [CrossRef]
- Archana, V.; Ambili, R.; Nisha, K.J.; Seba, A.; Preeja, C. Acute-phase reactants in periodontal disease: Current concepts and future implications. J. Investig. Clin. Dent. 2015, 6, 108–117. [Google Scholar] [CrossRef] [PubMed]
- Kilicarslan, A.; Uysal, A.; Roach, E.C. Acute Phase Reactants. Acta Med. 2013, 2, 2–7. [Google Scholar]
- Markanday, A. Acute Phase Reactants in Infections: Evidence-Based Review and a Guide for Clinicians. Open Forum Infect. Dis. 2015, 2, ofv098. [Google Scholar] [CrossRef]
- Manzo, C.; Milchert, M.; Venditti, C.; Castagna, A.; Nune, A.; Natale, M.; Brzosko, M. Fever Correlation with Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) Concentrations in Patients with Isolated Polymyalgia Rheumatica (PMR): A Retrospective Comparison Study between Hospital and Out-of-Hospital Local Registries. Life 2022, 12, 985. [Google Scholar] [CrossRef] [PubMed]
- Pathak, A.; Agrawal, A. Evolution of C-Reactive Protein. Front. Immunol. 2019, 10, 943. [Google Scholar] [CrossRef] [PubMed]
- Osei-Bimpong, A.; Meek, J.H.; Lewis, S.M. ESR or CRP? A comparison of their clinical utility. Hematology 2007, 12, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Song, S.; Ning, Q.; Zhu, D.; Jia, J.; Zhang, H.; Zhao, J.; Hao, S.; Liu, F.; Chu, C.; et al. Prediction for Intravenous Immunoglobulin Resistance Combining Genetic Risk Loci Identified from Next Generation Sequencing and Laboratory Data in Kawasaki Disease. Front. Pediatr. 2020, 8, 462367. [Google Scholar] [CrossRef]
- Rhodes, B.; Fuernrohr, B.G.; Vyse, T.J. C-reactive protein in rheumatology: Biology and genetics. Nat. Rev. Rheumatol. 2011, 7, 282–289. [Google Scholar] [CrossRef]
- Kullo, I.J.; Ding, K.; Shameer, K.; McCarty, C.A.; Jarvik, G.P.; Denny, J.C.; Ritchie, M.D.; Ye, Z.; Crosslin, D.R.; Chisholm, R.L.; et al. Complement Receptor 1 Gene Variants Are Associated with Erythrocyte Sedimentation Rate. Am. J. Hum. Genet. 2011, 89, 131–138. [Google Scholar] [CrossRef]
- Bluett, J.; Ibrahim, I.; Plant, D.; Hyrich, K.L.; Morgan, A.W.; Wilson, A.G.; Isaacs, J.D.; BRAGGSS; Barton, A. Association of a complement receptor 1 gene variant with baseline erythrocyte sedimentation rate levels in patients starting anti-TNF therapy in a UK rheumatoid arthritis cohort: Results from the Biologics in Rheumatoid Arthritis Genetics and Genomics Study Syndicate cohort. Pharm. J. 2013, 14, 171–175. [Google Scholar] [CrossRef]
- Bulatov, E.; Khaiboullina, S.; dos Reis, H.J.; Palotás, A.; Venkataraman, K.; Vijayalakshmi, M.; Rizvanov, A. Ubiquitin-Proteasome System: Promising Therapeutic Targets in Autoimmune and Neurodegenerative Diseases. Bionanoscience 2016, 6, 341–344. [Google Scholar] [CrossRef]
- Tian, Y.; Ge, Z.; Xing, Y.; Sun, Y.; Ying, J. Correlation of angiotensin I-converting enzyme gene insertion/deletion polymorphism with rheumatic heart disease: A meta-analysis. Biosci. Rep. 2016, 36, e00412. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Dvir, N.; Jacques, M.; Cavalcante, L.; Papadimitriou, I.D.; Munson, F.; Kuang, J.; Garnham, A.; Landen, S.; Li, J. ACE I/D Gene Variant Predicts ACE Enzyme Content in Blood but Not the ACE, UCP2, and UCP3 Protein Content in Human Skeletal Muscle in the Gene SMART Study. J. Appl. Physiol. 2018, 125, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Al-Harbi, K.M.; Almuzaini, I.S.; Morsy, M.M.; Abdelaziz, N.A.; Al-Balawi, A.M.; Abdallah, A.M. Angiotensin-converting enzyme gene insertion/deletion polymorphism in Saudi patients with rheumatic heart disease. Saudi Med. J. 2015, 36, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Morsy, M.-M.F.; Abdelaziz, N.A.M.; Boghdady, A.M.; Ahmed, H.; Abu Elfadl, E.M.; Ismail, M.A. Angiotensin converting enzyme DD genotype is associated with development of rheumatic heart disease in Egyptian children. Rheumatol. Int. 2011, 31, 17–21. [Google Scholar] [CrossRef]
- Davutoglu, V.; Nacak, M. Influence of angiotensin-converting enzyme gene insertion/deletion polymorphism on rheumatic valve involvement, valve severity and subsequent valve calcification. J. Heart Valve Dis. 2005, 14, 277–281. [Google Scholar]
- Abdallah, A.M.; Alnuzha, A.; Al-Mazroea, A.H.; Eldardear, A.E.; Alsamman, A.Y.; Almohammadi, Y.; Al-Harbi, K.M. IL10 Promoter Polymorphisms are Associated with Rheumatic Heart Disease in Saudi Arabian Patients. Pediatr. Cardiol. 2016, 37, 99–105. [Google Scholar] [CrossRef]
- Saracevic, A.; Simundic, A.-M.; Celap, I.; Luzanic, V. Angiotensin-converting enzyme insertion/deletion polymorphism genotyping error: The cause and a possible solution to the problem. Mol. Biol. Rep. 2013, 40, 4459–4463. [Google Scholar] [CrossRef]
- Soubrier, F. From an ACE polymorphism to genome-wide searches for eQTL. J. Clin. Investig. 2013, 123, 111–112. [Google Scholar] [CrossRef]
- Tkacova, R.; Joppa, P. Angiotensin-converting enzyme genotype and C-reactive protein in patients with COPD. Eur. Respir. J. 2007, 29, 816–817. [Google Scholar] [CrossRef]
- Awad, K.; Zaki, M.M.; Mohammed, M.; Lewek, J.; Lavie, C.J.; Banach, M. Effect of the Renin-Angiotensin System Inhibitors on Inflammatory Markers: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Mayo Clin. Proc. 2022, 97, 1808–1823. [Google Scholar] [CrossRef] [PubMed]
- Peng, N.; Liu, J.-T.; Gao, D.-F.; Lin, R.; Li, R. Angiotensin II-induced C-reactive protein generation: Inflammatory role of vascular smooth muscle cells in atherosclerosis. Atherosclerosis 2007, 193, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Liu, J.; Liu, X.; Li, M. Angiotensin II induces C-reactive protein expression through ERK1/2 and JNK signaling in human aortic endothelial cells. Atherosclerosis 2010, 212, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Ichikawa, J.; Giuroiu, I.; Laino, A.S.; Hao, Y.; Krogsgaard, M.; Vassallo, M.; Woods, D.M.; Stephen Hodi, F.; Weber, J. C reactive protein impairs adaptive immunity in immune cells of patients with melanoma. J. Immunother. Cancer 2020, 8, e000234. [Google Scholar] [CrossRef]
- Kuriakose, T.; Kanneganti, T.-D. Is Inflammasome a Potential Target of Prophylaxis in Rheumatic Heart Disease? Circulation 2018, 138, 2662–2665. [Google Scholar] [CrossRef]
- Lagrand, W.K.; Niessen, H.W.M.; Wolbink, G.-J.; Jaspars, L.H.; Visser, C.A.; Verheugt, F.W.A.; Meijer, C.J.L.M.; Hack, C.E. C-Reactive Protein Colocalizes With Complement in Human Hearts During Acute Myocardial Infarction. Circulation 1997, 95, 97–103. [Google Scholar] [CrossRef]
- Bahramali, E.; Firouzabadi, N.; Jonaidi-Jafari, N.; Shafiei, M. Renin–angiotensin system genetic polymorphisms: Lack of association with CRP levels in patients with coronary artery disease. J. Renin-Angiotensin-Aldosterone Syst. 2014, 15, 559–565. [Google Scholar] [CrossRef]
- Dai, S.; Ding, M.; Liang, N.; Li, Z.; Li, D.; Guan, L.; Liu, H. Associations of ACE I/D polymorphism with the levels of ACE, kallikrein, angiotensin II and interleukin-6 in STEMI patients. Sci. Rep. 2019, 9, 19719. [Google Scholar] [CrossRef]
- Avila-Vanzzini, N.; Posadas-Romero, C.; Gonzalez-Salazar, M.D.C.; Maass-Iturbide, C.; Melendez-Ramirez, G.; Perez-Mendez, O.; Del Valle-Mondragon, L.; Masso-Rojas, F.; Lopez, E.V.; Herrera-Bello, H.; et al. The ACE I/D polymorphism is associated with nitric oxide metabolite and blood pressure levels in healthy Mexican men. Arch. De Cardiol. De México 2015, 85, 105–110. [Google Scholar] [CrossRef]
- Eisenmann, J.C.; Sarzynski, M.A.; Glenn, K.; Rothschild, M.; Heelan, K.A. ACE I/D genotype, adiposity, and blood pressure in children. Cardiovasc. Diabetol. 2009, 8, 14–18. [Google Scholar] [CrossRef]
- Fiorentino, G.; Benincasa, G.; Coppola, A.; Franzese, M.; Annunziata, A.; Affinito, O.; Viglietti, M.; Napoli, C. Targeted genetic analysis unveils novel associations between ACE I/D and APO T158C polymorphisms with D-dimer levels in severe COVID-19 patients with pulmonary embolism. J. Thromb. Thrombolysis 2022, 55, 51–59. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed Marei, Y.; Abdallah Bayoumy, A.; Mohamed Abulazm Nassar, H.; Mansour, B.; Bakeir Hamady, A. The Relation between ACE Gene Polymorphism and the Severity of COVID-19 Infection. Int. J. Microbiol. 2023, 2023, 4540287. [Google Scholar] [CrossRef] [PubMed]
- Montes-De-Oca-García, A.; Perez-Bey, A.; Velázquez-Díaz, D.; Corral-Pérez, J.; Opazo-Díaz, E.; Rebollo-Ramos, M.; Gómez-Gallego, F.; Cuenca-García, M.; Casals, C.; Ponce-González, J.G. Influence of ACE Gene I/D Polymorphism on Cardiometabolic Risk, Maximal Fat Oxidation, Cardiorespiratory Fitness, Diet and Physical Activity in Young Adults. Int. J. Environ. Res. Public Health 2021, 18, 3443. [Google Scholar] [CrossRef]
- Wang, J.; Sun, Z.; Yang, Y.; Wu, J.; Quan, W.; Chen, X.; Ni, P.; Li, D. Association of laboratory parameters and genetic polymorphisms with ischemic stroke in Chinese Han population. Exp. Ther. Med. 2021, 21, 490. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.; Abbas, S.; Bilal, A.; Aslam, M.N.; Awan, F.R. Association of ACE I/D Polymorphism with Risk of Diabetes in Cardiovascular Disease Patients. Exp. Clin. Endocrinol. Diabetes 2020, 128, 82–88. [Google Scholar] [CrossRef]
- Kosan, C.; Cayir, A.; Turan, M.I. Relationship between genetic mutation variations and acute-phase reactants in the attack-free period of children diagnosed with familial Mediterranean fever. Braz. J. Med. Biol. Res. 2013, 46, 904–908. [Google Scholar] [CrossRef]
- Salehi, R.; Motaghi, M.; Salehi, A.; Karimzadeh, H.; Pakzad, B. Impact of Single Nucleotide Polymorphism in the ANKRD55 Gene on Occurrence and Clinical Characteristics of Rheumatoid Arthritis. Avicenna J. Med. Biotechnol. 2022, 14, 259–263. [Google Scholar] [CrossRef]
- Newburger, J.W.; Takahashi, M.; Gerber, M.A.; Gewitz, M.H.; Tani, L.Y.; Burns, J.C.; Shulman, S.T.; Bolger, A.F.; Ferrieri, P.; Baltimore, R.S.; et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 2004, 114, 1708–1733. [Google Scholar] [CrossRef]
- Huang, M.-Y.; Gupta-Malhotra, M.; Huang, J.-J.; Syu, F.-K.; Huang, T.-Y. Acute-Phase Reactants and a Supplemental Diagnostic Aid for Kawasaki Disease. Pediatr. Cardiol. 2010, 31, 1209–1213. [Google Scholar] [CrossRef]
- Korean Kawasaki Disease Genetics Consortium; Kim, J.-J.; Yun, S.W.; Yu, J.J.; Yoon, K.L.; Lee, K.-Y.; Kil, H.-R.; Kim, G.B.; Han, M.K.; Song, M.S.; et al. Common Variants in the CRP Promoter are Associated with a High C-Reactive Protein Level in Kawasaki Disease. Pediatr. Cardiol. 2015, 36, 438–444. [Google Scholar] [CrossRef]
- Conboy, J.G. Developmental regulation of RNA processing by Rbfox proteins: Rbfox Regulation of RNA Processing. Wiley Interdiscip. Rev. RNA 2017, 8, e1398. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Maggadottir, S.M.; Hakonarson, H. Are genetic tests informative in predicting food allergy? Curr. Opin. Allergy Clin. Immunol. 2016, 16, 257–264. [Google Scholar] [CrossRef]
- Bill, B.R.; Lowe, J.K.; DyBuncio, C.T.; Fogel, B.L. Orchestration of Neurodevelopmental Programs by RBFOX1: Implications for Autism Spectrum Disorder. Int. Rev. Neurobiol. 2013, 113, 251–267. [Google Scholar] [CrossRef] [PubMed]
- Fernàndez-Castillo, N.; Gan, G.; van Donkelaar, M.M.; Vaht, M.; Weber, H.; Retz, W.; Meyer-Lindenberg, A.; Franke, B.; Harro, J.; Reif, A.; et al. RBFOX1, encoding a splicing regulator, is a candidate gene for aggressive behavior. Eur. Neuropsychopharmacol. 2020, 30, 44–55. [Google Scholar] [CrossRef]
- Fransén, K.; Pettersson, C.; Hurtig-Wennlöf, A. CRP levels are significantly associated with CRP genotype and estrogen use in The Lifestyle, Biomarker and Atherosclerosis (LBA) study. BMC Cardiovasc. Disord. 2022, 22, 170. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.T. Quantile-dependent expressivity of serum C-reactive protein concentrations in family sets. PeerJ 2021, 9, e10914. [Google Scholar] [CrossRef]
- Ma, J.; Lv, Z.; Wang, J.; Lu, J. Relationship Between IL-10 Gene Polymorphism and Spinal Tuberculosis. Med. Sci. Monit. 2019, 25, 4901–4906. [Google Scholar] [CrossRef] [PubMed]
- Nasef, S.I.; Ellawindy, A.; Askar, A.M.; Hashem, A.A.; Omar, H.H. Assessment of Angiopoietin-2 Single Nucleotide Polymorphism in Patients with Rheumatoid Arthritis. Inflammation 2022. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, A.M.; Carlus, S.J.; Al-Mazroea, A.H.; Alluqmani, M.; Almohammadi, Y.; Bhuiyan, Z.A.; Al-Harbi, K.M. Digenic Inheritance of LAMA4 and MYH7 Mutations in Patient with Infantile Dilated Cardiomyopathy. Medicina 2019, 55, 17. [Google Scholar] [CrossRef]
- Hatmal, M.M.; Al-Hatamleh, M.A.I.; Olaimat, A.N.; Mohamud, R.; Fawaz, M.; Kateeb, E.T.; Alkhairy, O.K.; Tayyem, R.; Lounis, M.; Al-Raeei, M.; et al. Reported Adverse Effects and Attitudes among Arab Populations Following COVID-19 Vaccination: A Large-Scale Multinational Study Implementing Machine Learning Tools in Predicting Post-Vaccination Adverse Effects Based on Predisposing Factors. Vaccines 2022, 10, 366. [Google Scholar] [CrossRef]
- Pakzad, B.; Moghadammanesh, H.; Salesi, M.; Salehi, R. Strong Association of Polymorphism in SPRED2 Gene with Disease Susceptibility and Clinical Characteristics of Rheumatoid Arthritis in the Iranian Population. Avicenna J. Med. Biotechnol. 2022, 14, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, S.-Y.; Liu, H.-H.; Yin, X.-D.; Cao, L.-T.; Xu, J.-H.; Li, X.-M.; Ye, D.-Q.; Wang, J. Associations of Vitamin D Receptor Single Nucleotide Polymorphisms with Susceptibility to Systemic Sclerosis. Arch. Med. Res. 2019, 50, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Vaquero, C.; Fiter, J.; Enjuanes, A.; Nogués, X.; Díez-Pérez, A.; Nolla, J.M. Influence of the BsmI Polymorphism of the Vitamin D Receptor Gene on Rheumatoid Arthritis Clinical Activity. J. Rheumatol. 2007, 34, 1823–1826. [Google Scholar] [PubMed]

| Parameter | Value | ||
|---|---|---|---|
| Age (mean ± SD years): | |||
| Controls | 20.5 (4.2) | ||
| Patients | 19 (5) | ||
| Gender (male/female %): | |||
| Controls | 49.6/50.4 | ||
| Patients | 56/44 | ||
| Clinical presentation (n (%)): | |||
| Valvular lesion: | |||
| Mitral valve lesion (MVL) | 67 (54) | ||
| Combined valve lesion (CVL) | 57 (46) | ||
| Carditis | 79 (64) | ||
| Arthritis | 71 (57) | ||
| Chorea | 6 (8) | ||
| Skin rash | 3 (4) | ||
| Subcutaneous nodules | 2 (2.7) | ||
| Recurrence | NA | ||
| Laboratory findings (n (%)): | |||
| Elevated acute-phase reactants (CRP/ESR) | 75 (75.7) | ||
| Prolonged PR interval | 38 (50.7) | ||
| Genotype | Control (n = 198) | Patients (n = 123) | |||||
|---|---|---|---|---|---|---|---|
| Count | Frequency | Count | Frequency | X2 | p-Value | OR (95%CI) | |
| DD | 88 | 0.44 | 60 | 0.49 | 5.2 | 0.07 | |
| ID | 85 | 0.43 | 57 | 0.46 | |||
| II | 25 | 0.13 | 6 | 0.05 | |||
| D | 261 | 0.66 | 177 | 0.72 | 3.8 | 0.06 | |
| I | 135 | 0.34 | 63 | 0.28 | |||
| DD+ID | 173 | 0.87 | 117 | 0.95 | 4.4 | 0.04 | 2.9 (1.1–7.6) |
| II | 25 | 0.13 | 6 | 0.05 | |||
| II+ID | 110 | 0.56 | 63 | 0.51 | 0.5 | ||
| DD | 88 | 0.44 | 60 | 0.49 | |||
| Genotype | Control (n = 198) | RHD with High APR (n = 75) | RHD with Normal APR (n = 48) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Count | Frequency | Count | Frequency | Count | Frequency | p-Value 1 | p-Value 2 | p-Value 3 | |
| D/D | 88 | 0.44 | 40 | 0.53 | 20 | 0.43 | 0.04 | 0.2 | 0.5 |
| I/D | 85 | 0.43 | 33 | 0.44 | 24 | 0.52 | |||
| I/I | 25 | 0.13 | 2 | 0.03 | 2 | 0.04 | |||
| D | 261 | 0.66 | 113 | 0.75 | 64 | 0.70 | 0.04 | 0.5 | 0.4 |
| I | 135 | 0.34 | 37 | 0.25 | 28 | 0.30 | |||
| DD+ID | 173 | 0.87 | 73 | 0.97 | 44 | 0.96 | 0.02 | 0.2 | 1 |
| II | 25 | 0.13 | 2 | 0.03 | 2 | 0.04 | |||
| II+ID | 110 | 0.56 | 35 | 0.47 | 26 | 0.57 | 0.2 | 1 | 0.4 |
| DD | 88 | 0.44 | 40 | 0.53 | 20 | 0.43 | |||
| Genotype | Control (n = 198) | Patients (n = 75) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MVL (n = 33) | CVL (n = 42) | p-Value 1 | p-Value 2 | p-Value 3 | |||||
| Count | Frequency | Count | Frequency | Count | Frequency | ||||
| D/D | 88 | 0.44 | 18 | 0.55 | 22 | 0.52 | 0.06 * | 0.3 * | 0.4 * |
| I/D | 85 | 0.43 | 15 | 0.45 | 18 | 0.43 | |||
| I/I | 25 | 0.13 | 0 | 0 | 2 | 0.05 | |||
| D | 261 | 0.66 | 51 | 0.77 | 62 | 0.74 | 0.09 | 0.2 | 0.8 |
| I | 135 | 0.34 | 15 | 0.23 | 22 | 0.26 | |||
| D/D+I/D | 173 | 0.87 | 33 | 1.0 | 40 | 0.95 | 0.02 * | 0.1 * | 0.3 * |
| I/I | 25 | 0.13 | 0 | 0 | 2 | 0.05 | |||
| II+ID | 110 | 0.56 | 15 | 0.45 | 20 | 0.48 | 0.2 | 0.2 | 0.5 |
| DD | 88 | 0.44 | 18 | 0.55 | 22 | 0.52 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almazroea, A.H.; Yousef, S.; Ahmad, S.M.S.; AlHiraky, H.N.; Al-Haidose, A.; Abdallah, A.M. The Impact of ACE Gene Variants on Acute-Phase Reactants in Children with Rheumatic Heart Disease. Diagnostics 2023, 13, 1672. https://doi.org/10.3390/diagnostics13101672
Almazroea AH, Yousef S, Ahmad SMS, AlHiraky HN, Al-Haidose A, Abdallah AM. The Impact of ACE Gene Variants on Acute-Phase Reactants in Children with Rheumatic Heart Disease. Diagnostics. 2023; 13(10):1672. https://doi.org/10.3390/diagnostics13101672
Chicago/Turabian StyleAlmazroea, Abdulhadi H., Sondos Yousef, Salma M. S. Ahmad, Hanin N. AlHiraky, Amal Al-Haidose, and Atiyeh M. Abdallah. 2023. "The Impact of ACE Gene Variants on Acute-Phase Reactants in Children with Rheumatic Heart Disease" Diagnostics 13, no. 10: 1672. https://doi.org/10.3390/diagnostics13101672






