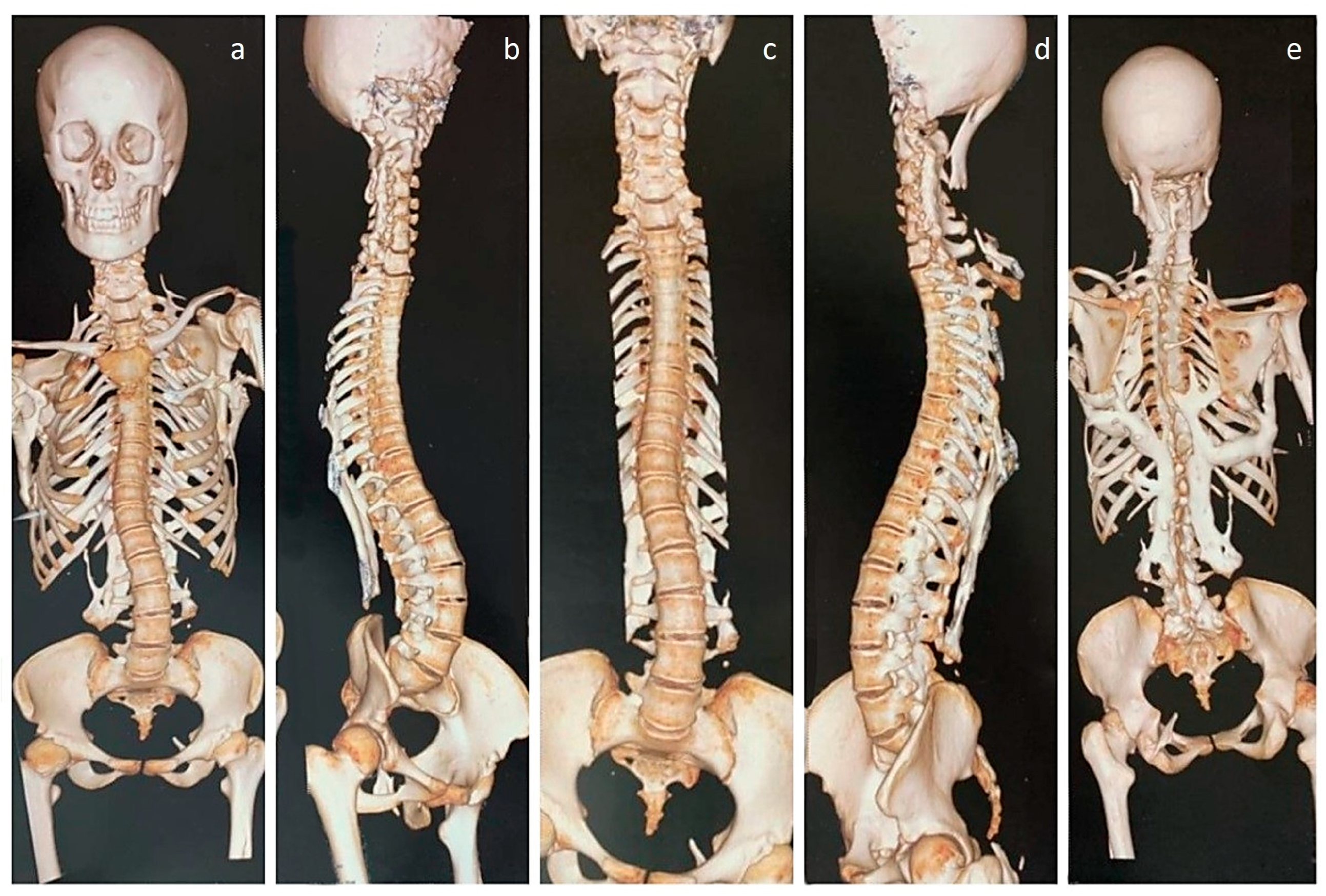
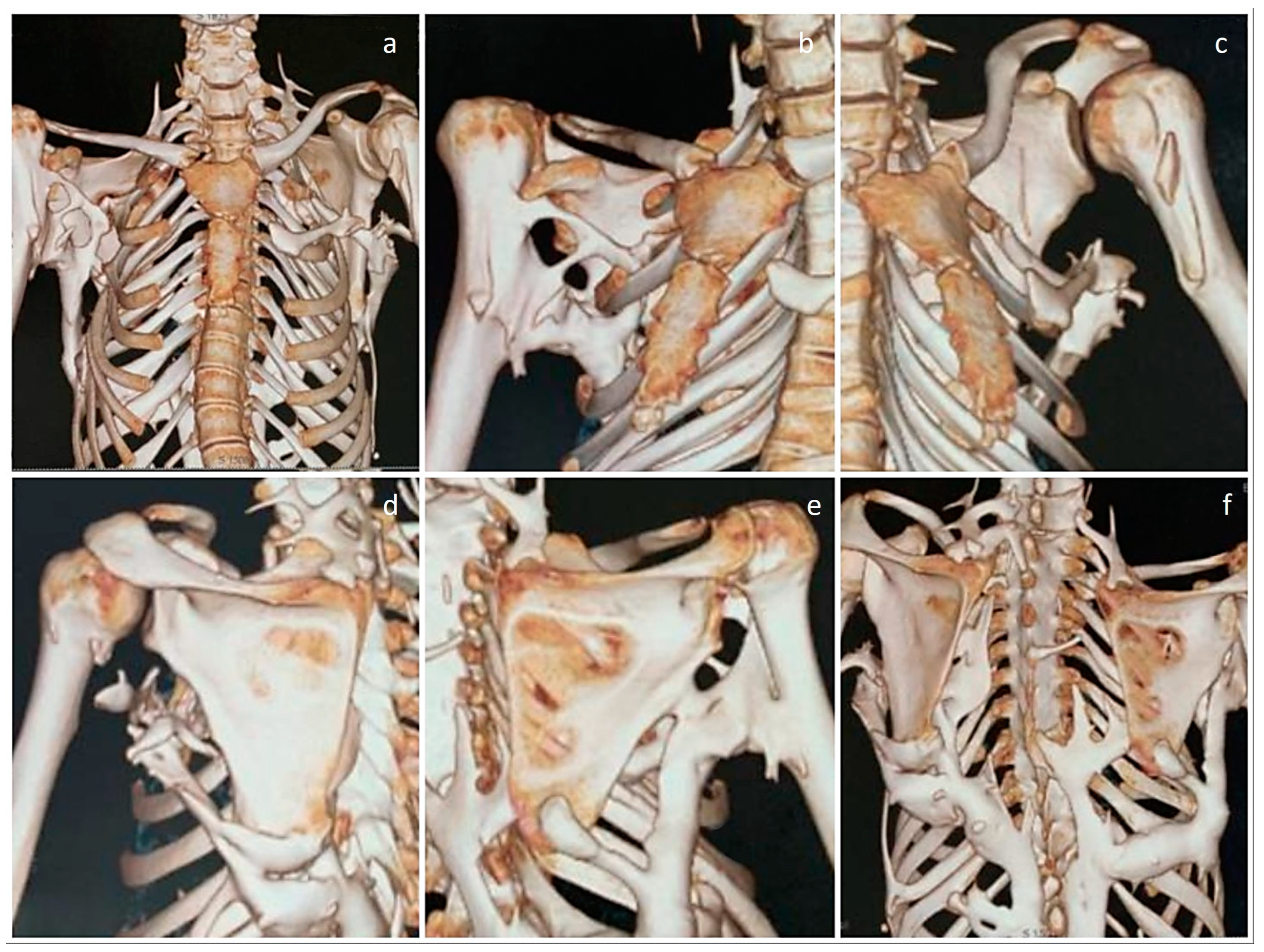
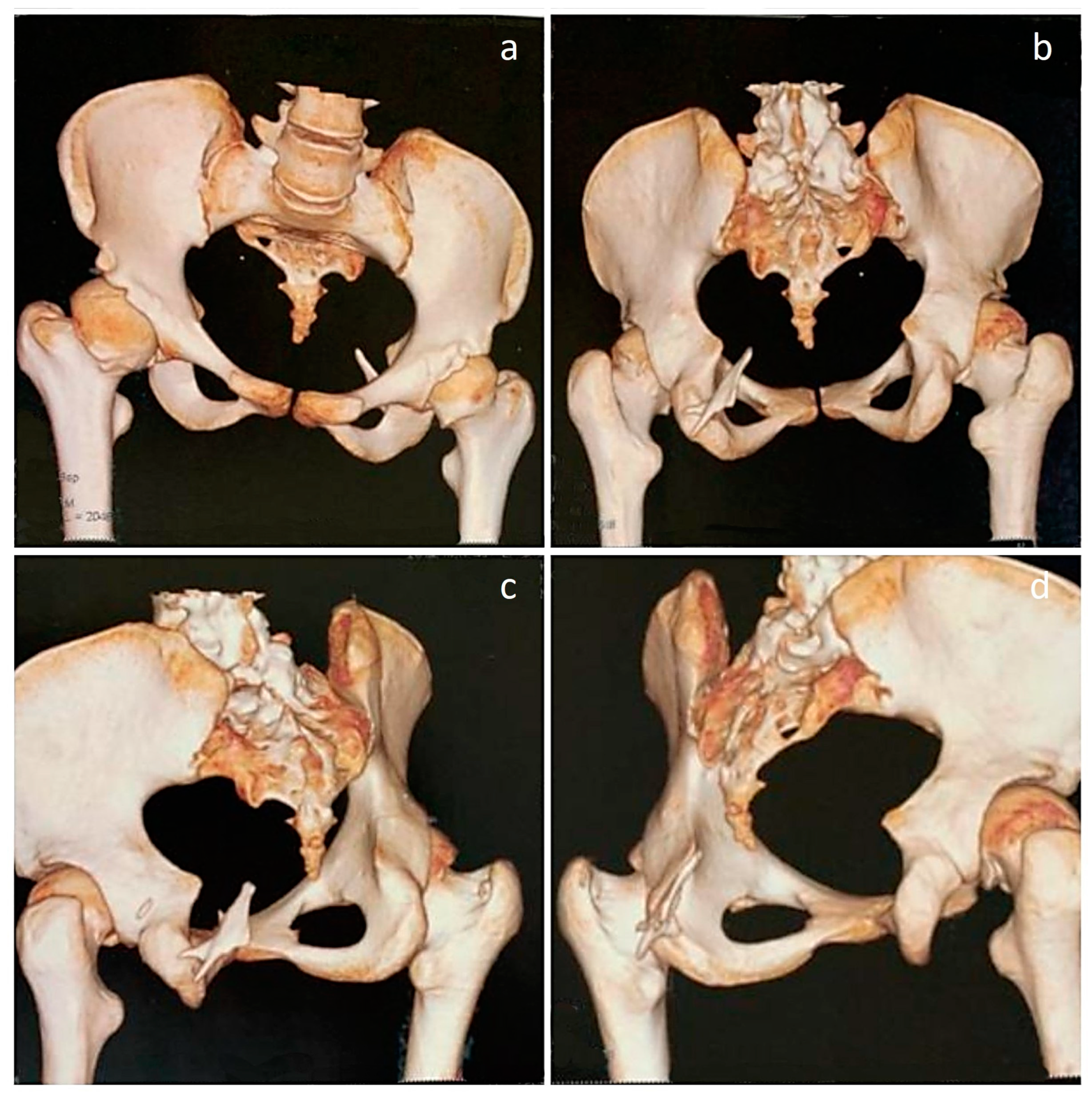
Living with Fibrodysplasia Ossificans Progressiva: Radiological Images of a Patient with Extensive Heterotopic Ossification
Abstract
:

Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Qi, Z.; Luan, J.; Zhou, X.; Cui, Y.; Han, J. Fibrodysplasia ossificans progressiva: Basic understanding and experimental models. Intractable Rare Dis. Res. 2017, 6, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Ravazzolo, R.; Bocciardi, R. Genomic Context and Mechanisms of the ACVR1 Mutation in Fibrodysplasia Ossificans Progressiva. Biomedicines 2021, 9, 154. [Google Scholar] [CrossRef] [PubMed]
- Meyers, C.; Lisiecki, J.; Miller, S.; Levin, A.; Fayad, L.; Ding, C.; Sono, T.; McCarthy, E.; Levi, B.; James, A.W. Heterotopic Ossification: A Comprehensive Review. JBMR Plus 2019, 3, e10172. [Google Scholar] [CrossRef] [PubMed]
- Smilde, B.J.; Botman, E.; de Ruiter, R.D.; Smit, J.M.; Teunissen, B.P.; Lubbers, W.D.; Schwarte, L.A.; Schober, P.; Eekhoff, E.M.W. Monitoring and Management of Fibrodysplasia Ossificans Progressiva: Current Perspectives. Orthop. Res. Rev. 2022, 14, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Kitoh, H. Clinical Aspects and Current Therapeutic Approaches for FOP. Biomedicines 2020, 8, 325. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, F.S.; Mukaddam, M.A.; Baujat, G.; Brown, M.; Cali, A.; Cho, T.J.; Crowe, C.; De Cunto, C.L.; Delai, P.; Diecidue, R.J.; et al. The medical management of fibrodysplasia ossificans progressiva: Current treatment considerations. Proc. Intl. Clin. Council FOP 2021, 2, 1–127. [Google Scholar]
- Pignolo, R.J.; Shore, E.M.; Kaplan, F.S. Fibrodysplasia ossificans progressiva: Diagnosis, management, and therapeutic horizons. Pediatr. Endocrinol. Rev. 2013, 10 (Suppl. S2), 437–448. [Google Scholar] [PubMed]
- Ortiz-Agapito, F.; Colmenares-Bonilla, D. Quality of life of patients with fibrodysplasia ossificans progressiva. J. Child. Orthop. 2015, 9, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Towler, O.W.; Kaplan, F.S.; Shore, E.M. The Developmental Phenotype of the Great Toe in Fibrodysplasia Ossificans Progressiva. Front. Cell Dev. Biol. 2020, 8, 612853. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, F.S.; Lounev, V.Y.; Wang, H.; Pignolo, R.J.; Shore, E.M. Fibrodysplasia ossificans progressiva: A blueprint for metamorphosis. Ann. N. Y. Acad. Sci. 2011, 1237, 5–10. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotb, M.M.; Omar, U.F.; Kaliya-Perumal, A.-K. Living with Fibrodysplasia Ossificans Progressiva: Radiological Images of a Patient with Extensive Heterotopic Ossification. Diagnostics 2023, 13, 1711. https://doi.org/10.3390/diagnostics13101711
Kotb MM, Omar UF, Kaliya-Perumal A-K. Living with Fibrodysplasia Ossificans Progressiva: Radiological Images of a Patient with Extensive Heterotopic Ossification. Diagnostics. 2023; 13(10):1711. https://doi.org/10.3390/diagnostics13101711
Chicago/Turabian StyleKotb, Mohammed Mostafa, Usama Farghaly Omar, and Arun-Kumar Kaliya-Perumal. 2023. "Living with Fibrodysplasia Ossificans Progressiva: Radiological Images of a Patient with Extensive Heterotopic Ossification" Diagnostics 13, no. 10: 1711. https://doi.org/10.3390/diagnostics13101711
APA StyleKotb, M. M., Omar, U. F., & Kaliya-Perumal, A.-K. (2023). Living with Fibrodysplasia Ossificans Progressiva: Radiological Images of a Patient with Extensive Heterotopic Ossification. Diagnostics, 13(10), 1711. https://doi.org/10.3390/diagnostics13101711




