The Role of Contrast-Enhanced Ultrasound in the Differential Diagnosis of Tuberous Vas Deferens Tuberculosis and Metastatic Inguinal Lymph Nodes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. US and CEUS Examination
2.3. Statistical Analyses
3. Results
3.1. Patients
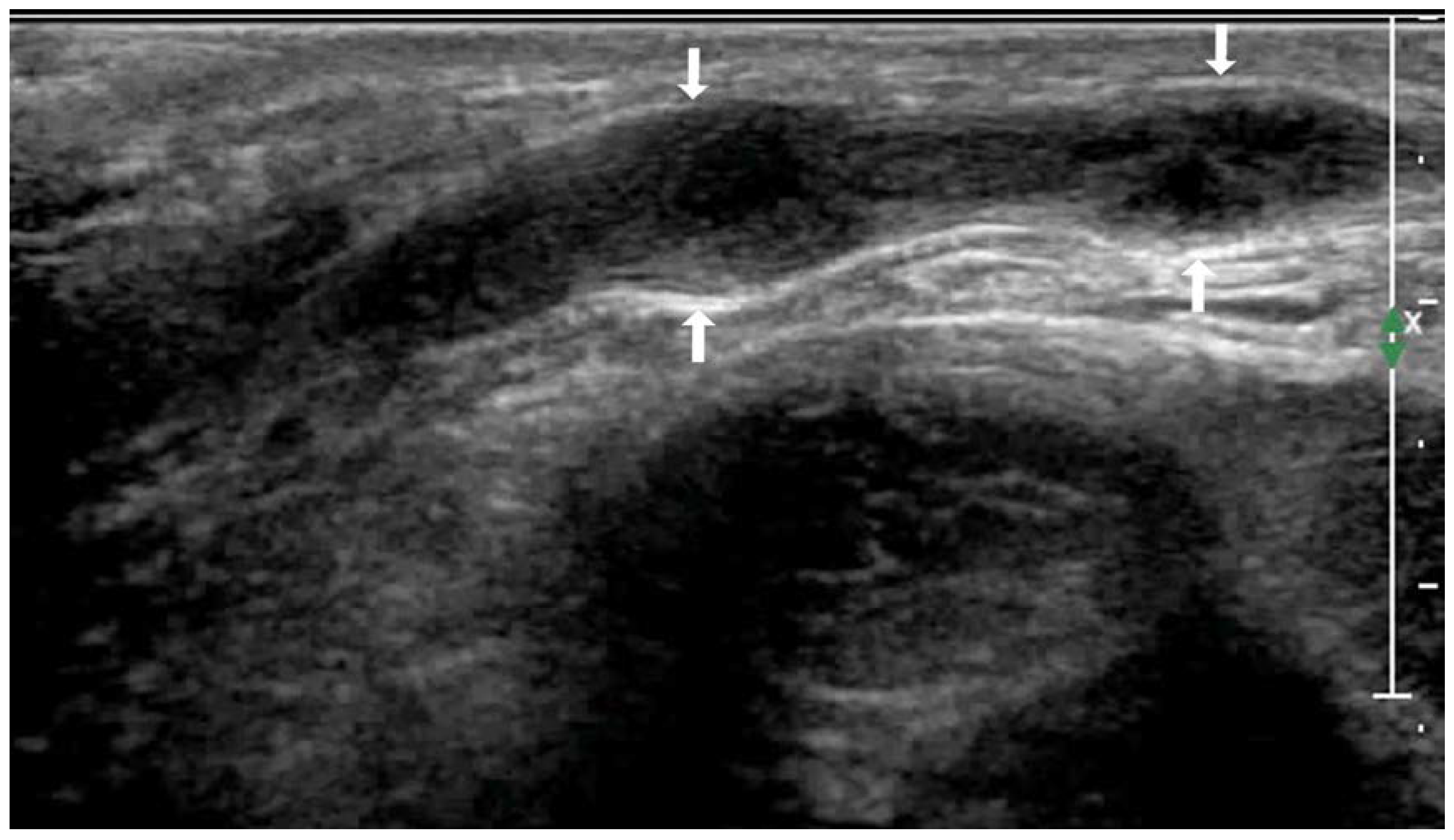
3.2. US Examination
3.3. CEUS Examination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhu, X.Y.; Jiang, Z.Q.; Wan, B.; Zhong, K.B.; Wen, L.J.; Zhou, Q.L.; Xu, S.Y. Routing reseach of vas deferens on anatomy and clinical application. Zhonghua Nan Ke Xue 2006, 12, 123–125. [Google Scholar] [PubMed]
- Jing, J.; Zhuang, H.; Luo, Y.; Chen, H.; Rao, Y. Vas deferens sonographic appearances of tuberculosis lesions of 19 cases of male genital systemic tuberculosis. Medicine 2019, 98, e14843. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, A.; Das, C.J.; Razik, A. Male genital tract tuberculosis: A comprehensive review of imaging findings and differential diagnosis. Abdom. Radiol. 2021, 46, 1677–1686. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Huang, L.; Zhang, X.; Ji, Q.; Shen, W. Multiparametric Magnetic Resonance Imaging Characteristics of Prostate Tuberculosis. Korean J. Radiol. 2015, 16, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Ravikanth, R.; Kamalasekar, K.; Patel, N. Extensive primary male genital tuberculosis. J. Hum. Reprod. Sci. 2019, 12, 258–261. [Google Scholar] [CrossRef]
- Bello, A.P.; Apatov, S.E.; Benfante, N.E.; Belenchón, I.R.; Brau, N.P.; Barrull, C.M.; Jenjitranant, P.; Vickers, A.J.; Fine, S.W.; Touijer, K.A. Prevalence of High-Risk Prostate Cancer Metastasis to Cloquet’s Ilioinguinal Lymph Node. J. Urol. 2022, 207, 1222–1226. [Google Scholar] [CrossRef]
- Bucknell, N.W.; E Gyorki, D.; Bressel, M.; Estall, V.; Webb, A.; Henderson, M.; Chua, M.S.; Rischin, D.; Tiong, A.; Hons, N.W.B.M.; et al. Cutaneous squamous cell carcinoma metastatic to the axilla and groin: Outcomes and prognostic factors. Australas. J. Dermatol. 2021, 63, 43–52. [Google Scholar] [CrossRef]
- Elsaqa, M.; Sharafeldeen, M.; Elabbady, A. Metastatic Prostate Cancer Presenting with Bilateral Inguinal Lymphadenopathy. Clin. Genitourin. Cancer 2019, 17, e1185–e1187. [Google Scholar] [CrossRef]
- de Gregorio, N.; Ebner, F.; Schwentner, L.; Friedl, T.W.; Deniz, M.; Látó, K.; Kreienberg, R.; Janni, W.; Varga, D. The role of preoperative ultrasound evaluation of inguinal lymph nodes in patients with vulvar malignancy. Gynecol. Oncol. 2013, 131, 113–117. [Google Scholar] [CrossRef]
- Kawahara, Y.; Togawa, Y.; Yamamoto, Y.; Wakabayashi, S.; Matsue, H.; Inafuku, K. Usefulness of 2-D shear wave elastography for the diagnosis of inguinal lymph node metastasis of malignant melanoma and squamous cell carcinoma. J. Dermatol. 2020, 47, 1312–1316. [Google Scholar] [CrossRef]
- Garganese, G.; Fragomeni, S.M.; Pasciuto, T.; Leombroni, M.; Moro, F.; Evangelista, M.T.; Bove, S.; Gentileschi, S.; Tagliaferri, L.; Paris, I.; et al. Ultrasound morphometric and cytologic preoperative assessment of inguinal lymph-node status in women with vulvar cancer: MorphoNode study. Ultrasound Obstet. Gynecol. 2019, 55, 401–410. [Google Scholar] [CrossRef]
- Tranquart, F.; Mercier, L.; Frinking, P.; Gaud, E.; Arditi, M. Perfusion Quantification in Contrast-Enhanced Ultrasound (CEUS)—Ready for Research Projects and Routine Clinical Use. Ultraschall der Med. Eur. J. Ultrasound 2012, 33 (Suppl. S1), S31–S38. [Google Scholar] [CrossRef]
- Tufano, A.; Drudi, F.M.; Angelini, F.; Polito, E.; Martino, M.; Granata, A.; Di Pierro, G.B.; Kutrolli, E.; Sampalmieri, M.; Canale, V.; et al. Contrast-Enhanced Ultrasound (CEUS) in the Evaluation of Renal Masses with Histopathological Validation—Results from a Prospective Single-Center Study. Diagnostics 2022, 12, 1209. [Google Scholar] [CrossRef]
- Trimboli, P.; Castellana, M.; Virili, C.; Havre, R.F.; Bini, F.; Marinozzi, F.; D’ambrosio, F.; Giorgino, F.; Giovanella, L.; Prosch, H.; et al. Performance of contrast-enhanced ultrasound (CEUS) in assessing thyroid nodules: A systematic review and meta-analysis using histological standard of reference. Radiol. Med. 2020, 125, 406–415. [Google Scholar] [CrossRef]
- Aggarwal, A.; Das, C.J.; Manchanda, S. Imaging Spectrum of Female Genital Tuberculosis: A Comprehensive Review. Curr. Probl. Diagn. Radiol. 2022, 51, 617–627. [Google Scholar] [CrossRef]
- Tjahyadi, D.; Ropii, B.; Tjandraprawira, K.D.; Parwati, I.; Djuwantono, T.; Permadi, W.; Li, T. Female Genital Tuberculosis: Clinical Presentation, Current Diagnosis, and Treatment. Infect. Dis. Obstet. Gynecol. 2022, 2022, 3548190. [Google Scholar] [CrossRef]
- Kulchavenya, E.; Kim, C.-S.; Bulanova, O.; Zhukova, I. Male genital tuberculosis: Epidemiology and diagnostic. World J. Urol. 2011, 30, 15–21. [Google Scholar] [CrossRef]
- Lin, Z.; Chen, J.; Lin, Q.; Chen, J.; Yan, Y. Magnetic resonance imaging-guided transperineal prostate biopsy. J. Cancer Res. Ther. 2019, 15, 394. [Google Scholar] [CrossRef]
- Basaraba, R.J.; Hunter, R.L. Pathology of Tuberculosis: How the Pathology of Human Tuberculosis Informs and Directs Animal Models. Microbiol. Spectr. 2017, 5, 117–129. [Google Scholar] [CrossRef]
- Rossi, E.C.; Kowalski, L.D.; Scalici, J.; Cantrell, L.; Schuler, K.; Hanna, R.K.; Method, M.; Ade, M.; Ivanova, A.; Boggess, J.F. A comparison of sentinel lymph node biopsy to lymphadenectomy for endometrial cancer staging (FIRES trial): A multicentre, prospective, cohort study. Lancet Oncol. 2017, 18, 384–392. [Google Scholar] [CrossRef]
- Mathevet, P.; Lécuru, F.; Uzan, C.; Boutitie, F.; Magaud, L.; Guyon, F.; Querleu, D.; Fourchotte, V.; Baron, M.; Bats, A.-S.; et al. Sentinel lymph node biopsy and morbidity outcomes in early cervical cancer: Results of a multicentre randomised trial (SENTICOL-2). Eur. J. Cancer 2021, 148, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Tamura, T.; Kurishima, K.; Nakazawa, K.; Kagohashi, K.; Ishikawa, H.; Satoh, H.; Hizawa, N. Specific organ metastases and survival in metastatic non-small-cell lung cancer. Mol. Clin. Oncol. 2014, 3, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Akrivos, N.; Rodolakis, A.; Vlachos, G.; Sotiropoulou, M.; Papantoniou, V.; Biliatis, I.; Haidopoulos, D.; Thomakos, N.; Simou, M.; Antsaklis, A. Detection and credibility of sentinel node in vulvar cancer: A single institutional study and short review of literature. Arch. Gynecol. Obstet. 2011, 284, 1551–1556. [Google Scholar] [CrossRef] [PubMed]
- Klar, M.; Bossart, M.; Stickeler, E.; Brink, I.; Orlowska-Volk, M.; Denschlag, D. Sentinel lymph node detection in patients with vulvar carcinoma; Feasibility of intra-operative mapping with technetium-99m-labeled nanocolloid. Eur. J. Surg. Oncol. (EJSO) 2011, 37, 818–823. [Google Scholar] [CrossRef] [PubMed]
- Cui, Q.; Dai, L.; Li, J.; Xue, J. Accuracy of CEUS-guided sentinel lymph node biopsy in early-stage breast cancer: A study review and meta-analysis. World J. Surg. Oncol. 2020, 18, 112. [Google Scholar] [CrossRef]
- Moody, A.N.; Bull, J.; Culpan, A.-M.; Munyombwe, T.; Sharma, N.; Whitaker, M.; Wolstenhulme, S. Preoperative sentinel lymph node identification, biopsy and localisation using contrast enhanced ultrasound (CEUS) in patients with breast cancer: A systematic review and meta-analysis. Clin. Radiol. 2017, 72, 959–971. [Google Scholar] [CrossRef]
- Ling, W.; Nie, J.; Zhang, D.; Yang, Q.; Jin, H.; Ou, X.; Ma, X.; Luo, Y. Role of Contrast-Enhanced Ultrasound (CEUS) in the Diagnosis of Cervical Lymph Node Metastasis in Nasopharyngeal Carcinoma (NPC) Patients. Front. Oncol. 2020, 10, 972. [Google Scholar] [CrossRef]
- Zhan, J.; Diao, X.; Chen, Y.; Wang, W.; Ding, H. Predicting cervical lymph node metastasis in patients with papillary thyroid cancer (PTC)—Why contrast-enhanced ultrasound (CEUS) was performed before thyroidectomy. Clin. Hemorheol. Microcirc. 2019, 72, 61–73. [Google Scholar] [CrossRef]
- Mohammed, D.A.; Uberoi, R.; Lopes, A.D.B.; Monaghan, J. Inguinal Node Status by Ultrasound in Vulva Cancer. Gynecol. Oncol. 2000, 77, 93–96. [Google Scholar] [CrossRef]
- Krishna, R.P.; Sistla, S.C.; Smile, R.; Krishnan, R. Sonography: An underutilized diagnostic tool in the assessment of metastatic groin nodes. J. Clin. Ultrasound 2007, 36, 212–217. [Google Scholar] [CrossRef]
- Lam, W.; Kaul, A.; Ayres, B.; Corbishley, C.; Perry, M.; Sharma, D.; Pilcher, J.; Watkin, N. 56 The role of ultrasound in the detection of inguinal nodal metastasis in patients with primary squamous cell carcinoma of the penis: A prospective cohort analysis of 726 inguinal basins assessed in a single institution. Eur. Urol. Suppl. 2014, 13, e56. [Google Scholar] [CrossRef]
- Kanchustambham, V.; Saladi, S. Adenocarcinoma of the Lung with Inguinal Lymph Node Metastasis. Cureus 2021, 13, e13658. [Google Scholar] [CrossRef]
- Mehralivand, S.; van der Poel, H.; Winter, A.; Choyke, P.L.; Pinto, P.A.; Turkbey, B. Sentinel lymph node imaging in urologic oncology. Transl. Androl. Urol. 2018, 7, 887–902. [Google Scholar] [CrossRef]
- Lützen, U.; Zuhayra, M.; Marx, M.; Zhao, Y.; Colberg, C.; Knüpfer, S.; Baumann, R.; Kähler, K.C.; Jünemann, K.-P.; Naumann, C.M. Value and efficiency of sentinel lymph node diagnostics in patients with penile carcinoma with palpable inguinal lymph nodes as a new multimodal, minimally invasive approach. Eur. J. Nucl. Med. 2016, 43, 2313–2323. [Google Scholar] [CrossRef]
- Lam, W.; Alnajjar, H.M.; La-Touche, S.; Perry, M.; Sharma, D.; Corbishley, C.; Pilcher, J.; Heenan, S.; Watkin, N. Dynamic Sentinel Lymph Node Biopsy in Patients with Invasive Squamous Cell Carcinoma of the Penis: A Prospective Study of the Long-Term Outcome of 500 Inguinal Basins Assessed at a Single Institution. Eur. Urol. 2013, 63, 657–663. [Google Scholar] [CrossRef]
- Wang, A.; Lu, L.; Fan, J.; Wang, S.; Chen, X. Lymph node metastatic patterns and its clinical significance for thoracic superficial esophageal squamous cell carcinoma. J. Cardiothorac. Surg. 2020, 15, 262. [Google Scholar] [CrossRef]
- Arun, I.; Maity, N.; Hameed, S.; Jain, P.V.; Manikantan, K.; Sharan, R.; Arun, P. Lymph node characteristics and their prognostic significance in oral squamous cell carcinoma. Head Neck 2020, 43, 520–533. [Google Scholar] [CrossRef]




| Routine Ultrasound Manifestations | VD TB (17 Cases) | Metastatic Lymph Nodes (28 Cases) | χ2 | p | |
|---|---|---|---|---|---|
| Bilateral incidence | 10/17 (58.82%) | 16/28 (57.14%) | 0.120 | 0.912 | |
| Unilateral onset | 7/17 (41.17%) | 12/28 (42.85%) | |||
| Number of lesions | <3 | 6/17 (35.29%) | 15/28 (53.57%) | 0.947 | 0.331 |
| >3 | 11/17 (64.70%) | 13/28 (46.42%) | |||
| Maximum lesion size | <1 cm | 5/17 (29.41%) | 9/28 (32.14%) | NA | 0.917 |
| 1–3 cm | 10/17 (58.82%) | 14/28 (50.00%) | |||
| >3 cm | 2/17 (11.76%) | 5/28 (17.85%) | |||
| Internal echogenicity | Hypoechoic | 10/17 (58.82%) | 18/28 (64.28%) | NA | 0.080 |
| Isoechoic | 1/17 (5.88%) | 7/28 (25.00%) | |||
| Mixed echogenicity | 6/17 (35.29%) | 3/28 (10.71%) | |||
| Internal calcification foci | + | 3/17 (17.64%) | 1/28 (3.57%) | NA | 0.144 |
| − | 14/17 (82.35%) | 27/28 (96.42%) | |||
| Lesions conglomeration | + | 10/17 (58.82%) | 6/28 (21.42%) | 6.455 | 0.023 |
| − | 7/17 (41.17%) | 22/28 (78.57%) | |||
| Sinus canal, skin rupture | + | 0 | 2/28 (7.14%) | NA | 0.519 |
| − | 17/17 (100%) | 26/28 (92.85%) | |||
| CEUS Enhanced Mode, Degree and Intensity | VD TB (17 Cases) | Metastatic Lymph Nodes (28 Cases) | χ2 | p | |
|---|---|---|---|---|---|
| CEUS degree | 18.865 | 0.000 | |||
| Homogeneous enhancement | 3/17 (17.64%) | 23/28 (82.14%) | |||
| Heterogeneous enhancement | septal enhancement | 4/17 (23.52%) | 0 | ||
| Annular enhancement | 4/17 (23.52%) | 5/28 (17.85%) | |||
| Nodule-in-nodule enhancement | 3/17 (17.64%) | 0 | |||
| non-enhancement | 3/17 (17.64%) | 0 | |||
| Enhanced intensity | 17.455 | 0.000 | |||
| Low enhancement | 5/17 (29.41%) | 0 | |||
| Equal enhancement | 4/17 (23.52%) | 0 | |||
| High enhancement | 8/17 (47.05%) | 28/28 (100%) | |||
| CEUS mode | 15.074 | 0.000 | |||
| Centripetal enhancement | 0 | 16/28 (57.14%) | |||
| Noncentripetal enhancement | 17/17 (100%) | 12/28 (42.85%) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, W.; Ni, T.; Tang, W.; Yang, G. The Role of Contrast-Enhanced Ultrasound in the Differential Diagnosis of Tuberous Vas Deferens Tuberculosis and Metastatic Inguinal Lymph Nodes. Diagnostics 2023, 13, 1762. https://doi.org/10.3390/diagnostics13101762
Zhang W, Ni T, Tang W, Yang G. The Role of Contrast-Enhanced Ultrasound in the Differential Diagnosis of Tuberous Vas Deferens Tuberculosis and Metastatic Inguinal Lymph Nodes. Diagnostics. 2023; 13(10):1762. https://doi.org/10.3390/diagnostics13101762
Chicago/Turabian StyleZhang, Wenzhi, Tu Ni, Wei Tang, and Gaoyi Yang. 2023. "The Role of Contrast-Enhanced Ultrasound in the Differential Diagnosis of Tuberous Vas Deferens Tuberculosis and Metastatic Inguinal Lymph Nodes" Diagnostics 13, no. 10: 1762. https://doi.org/10.3390/diagnostics13101762





