A Smartphone Application for Personalized Tooth Shade Determination
Abstract
:1. Introduction
2. Materials and Methods
2.1. Methodology: Design of the App, Developmental Environment, Smartphone, and Camera Settings
2.2. Tooth Color Measurement and Tooth Appearance Uniformity Evaluation
2.3. Data Analysis
2.4. Feasibility of the App for Personalized Tooth Shade Determination
2.5. Study Participants
3. Results
3.1. Evaluation of Tooth Appearance Uniformity in Photographs Obtained Using the App
3.2. Feasibility Check of the App for Personalized Tooth Shade Determination
3.2.1. In Vitro Tooth Shade Determination
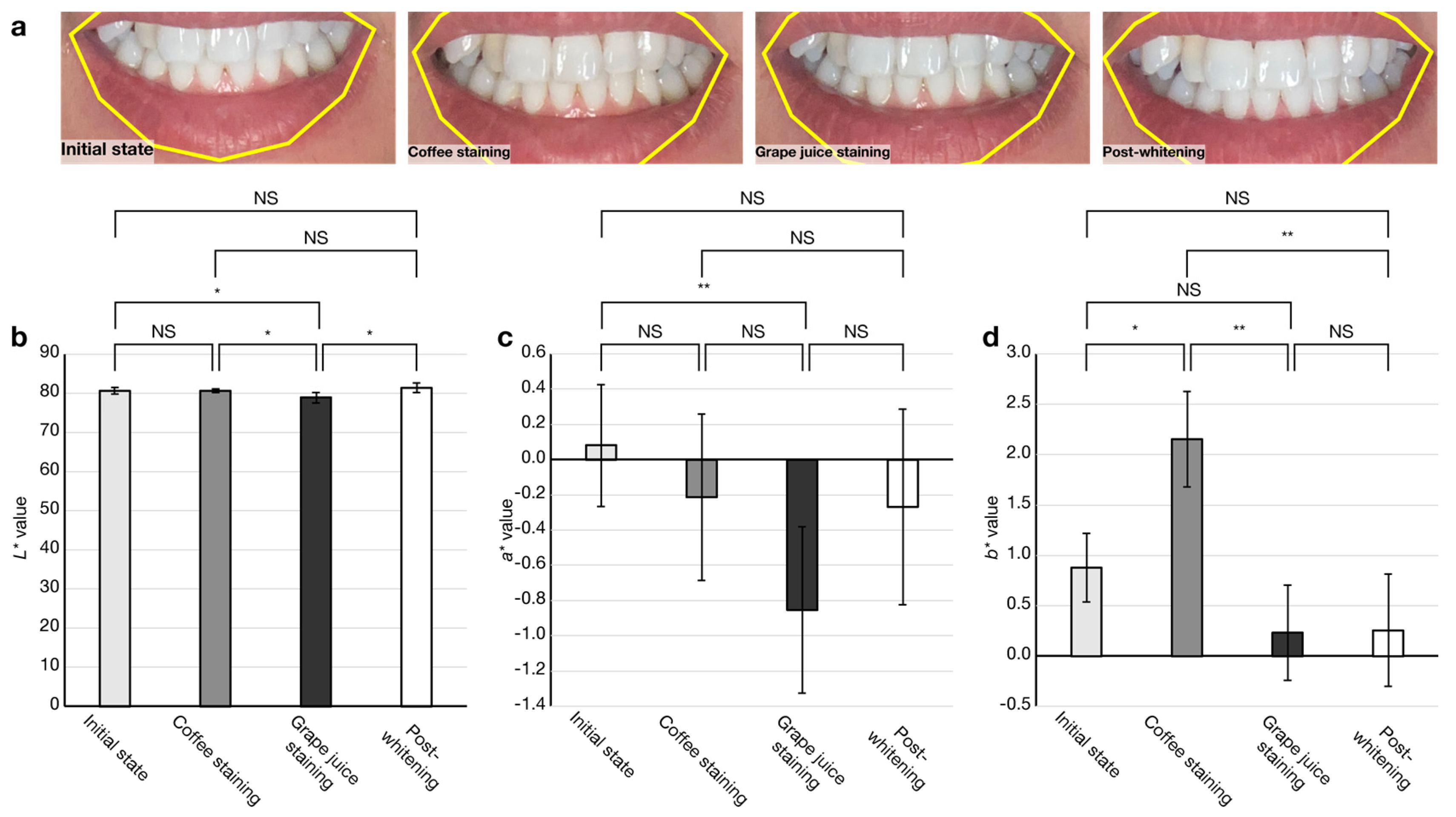
3.2.2. In Vivo Tooth Shade Determination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blanchard, D.; van Wissen, K. Home-based chemically induced whitening (bleaching) of teeth in adults: A summary of a systematic review. Public Health Nurs. 2020, 37, 626–627. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Martínez, J.; Valiente, M.; Sánchez-Martín, M.-J. Tooth whitening: From the established treatments to novel approaches to prevent side effects. J. Esthet. Restor. Dent. 2019, 31, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Tabatabaian, F.; Beyabanaki, E.; Alirezaei, P.; Epakchi, S. Visual and digital tooth shade selection methods, related effective factors and conditions, and their accuracy and precision: A literature review. J. Esthet. Restor. Dent. 2021, 33, 1084–1104. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Polo, C.; Gómez-Polo, M.; Martínez Vázquez de Parga, J.A.; Celemín-Viñuela, A. Clinical Study of the 3D-Master Color System among the Spanish Population. J. Prosthodont. 2018, 27, 708–715. [Google Scholar] [CrossRef]
- Gómez-Polo, C.; Gómez-Polo, M.; Quispe López, N.; Portillo Muñoz, M.; Montero, J. 3D Master Toothguide Is Adequate to Subjective Shade Selection? Medicina 2022, 58, 457. [Google Scholar] [CrossRef]
- Rao, D.; Joshi, S. Evaluation of natural tooth color space of the Indian population and its comparison to manufacturer’s shade systems. Contemp. Clin. Dent. 2018, 9, 395–399. [Google Scholar]
- Igiel, C.; Weyhrauch, M.; Wentaschek, S.; Scheller, H.; Lehmann, K.M. Dental color matching: A comparison between visual and instrumental methods. Dent. Mater. J. 2016, 35, 63–69. [Google Scholar] [CrossRef]
- Chang, J.-Y.; Chen, W.-C.; Huang, T.-K.; Wang, J.-C.; Fu, P.-S.; Chen, J.-H.; Hung, C.-C. Evaluating the accuracy of tooth color measurement by combining the Munsell color system and dental colorimeter. Kaohsiung J. Med. Sci. 2012, 28, 490–494. [Google Scholar] [CrossRef]
- Klotz, A.-L.; Habibi, Y.; Corcodel, N.; Rammelsberg, P.; Hassel, A.J.; Zenthöfer, A. Laboratory and clinical reliability of two spectrophotometers. J. Esthet. Restor. Dent. 2022, 34, 369–373. [Google Scholar] [CrossRef]
- Witkowski, S.; Yajima, N.-D.; Wolkewitz, M.; Strub, J.R. Reliability of shade selection using an intraoral spectrophotometer. Clin. Oral Investig. 2012, 16, 945–949. [Google Scholar] [CrossRef]
- McLaren, E.A.; Figueira, J.; Goldstein, R.E. A Technique Using Calibrated Photography and Photoshop for Accurate Shade Analysis and Communication. Compend. Contin. Educ. Dent. 2017, 38, 106–113. [Google Scholar] [PubMed]
- Hein, S.; Zangl, M. The use of a standardized gray reference card in dental photography to correct the effects of five commonly used diffusers on the color of 40 extracted human teeth. Int. J. Esthet. Dent. 2016, 11, 246–259. [Google Scholar] [PubMed]
- Tam, W.K.; Lee, H.J. Accurate shade image matching by using a smartphone camera. J. Prosthodont. Res. 2017, 61, 168–176. [Google Scholar] [CrossRef]
- Sirintawat, N.; Leelaratrungruang, T.; Poovarodom, P.; Kiattavorncharoen, S.; Amornsettachai, P. The accuracy and reliability of tooth shade selection using different instrumental techniques: An in vitro study. Sensors 2021, 21, 7490. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, A.; Bakhtiari, Z.; Mighani, F.; Bakhtiari, F. Validity and reliability of tooth color selection by smartphone photography and software applications. J. Indian Prosthodont. Soc. 2021, 21, 281–286. [Google Scholar]
- Jorquera, G.J.; Atria, P.J.; Galán, M.; Feureisen, J.; Imbarak, M.; Kernitsky, J.; Cacciuttolo, F.; Hirata, R.; Sampaio, C.S. A comparison of ceramic crown color difference between different shade selection methods: Visual, digital camera, and smartphone. J. Prosthet. Dent. 2022, 128, 784–792. [Google Scholar] [CrossRef]
- Khabarlak, K.; Koriashkina, L. Fast Facial Landmark Detection and Applications: A Survey. J. Comput. Sci. Technol. 2022, 22, e02. [Google Scholar] [CrossRef]
- Ishikawa-Nagai, S.; Yoshida, A.; Sakai, M.; Kristiansen, J.; Da Silva, J.D. Clinical evaluation of perceptibility of color differences between natural teeth and all-ceramic crowns. J. Dent. 2009, 37, 57–63. [Google Scholar] [CrossRef]
- Thoma, D.; Ioannidis, A.; Fehmer, V.; Michelotti, G.; Jung, R.; Sailer, I. Threshold Values for the Perception of Color Changes in Human Teeth. Int. J. Periodontics Restor. Dent. 2016, 36, 777–783. [Google Scholar] [CrossRef]
- Paolone, G. Direct composites in anteriors: A matter of substrate. Int. J. Esthet. Dent. 2017, 12, 468–481. [Google Scholar]
- Paolone, G.; Mandurino, M.; De Palma, F.; Mazzitelli, C.; Scotti, N.; Breschi, L.; Gherlone, E.; Cantatore, G.; Vichi, A. Color Stability of Polymer-Based Composite CAD/CAM Blocks: A Systematic Review. Polymers 2023, 15, 464. [Google Scholar] [CrossRef] [PubMed]




| Authors | Smartphone | External Light Source | Filter | Capture Mode | Potential Target Application and Its User |
|---|---|---|---|---|---|
| Tam et al. [13] | iPhone 6 Plus | None | None | Portrait | Clinical use by dentists |
| Sirintawat et al. [14] | Galaxy Note 20 Ultra 5G | Light correcting device | Polarization | Portrait | Clinical use by dentists |
| Mohammadi et al. [15] | iPhone 7 | Light correcting device | Polarization | Portrait | Clinical use by dentists |
| Jorquera et al. [16] | iPhone XS | Light correcting device | Polarization | Portrait | Clinical use by dentists |
| Kusayanagi et al. [current study] | iPhone 11 | None | None | Selfie | Home use by whitening product customers |
| 95% CI | |||||
|---|---|---|---|---|---|
| Group | Average 1 | SEM | Lower Bound | Upper Bound | |
| CV of L* value | With | 0.0256 | 0.0042 | 0.0173 | 0.0338 |
| Without | 0.0459 | 0.0222 | 0.0023 | 0.0894 | |
| CV of a* value | With | 0.2748 | 0.0588 | 0.1596 | 0.3899 |
| Without | 0.3279 | 0.0996 | 0.1327 | 0.5230 | |
| CV of b* value | With | 0.1053 | 0.0497 | 0.0078 | 0.2028 |
| Without | 0.1717 | 0.0681 | 0.0383 | 0.3051 | |
| 95% CI | ||||
|---|---|---|---|---|
| Average 1 | SEM | Lower Bound | Upper Bound | |
| CV of L* value | 0.0052 | 0.0006 | 0.0040 | 0.0063 |
| CV of a* value | 0.0322 | 0.0028 | 0.0268 | 0.0376 |
| CV of b* value | 0.0116 | 0.0035 | 0.0048 | 0.0048 |
| ΔEab 1 | Initial State | Coffee Staining | Grape Juice Staining | Post-Whitening |
|---|---|---|---|---|
| Initial state | − | 1.3 | 2.0 | 0 |
| Coffee staining | 1.3 | − | 2.6 | 1.9 |
| Grape juice staining | 2.0 | 2.6 | − | 2.5 |
| Post-whitening | 0 | 1.9 | 2.5 | − |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kusayanagi, T.; Maegawa, S.; Terauchi, S.; Hashimoto, W.; Kaneda, S. A Smartphone Application for Personalized Tooth Shade Determination. Diagnostics 2023, 13, 1969. https://doi.org/10.3390/diagnostics13111969
Kusayanagi T, Maegawa S, Terauchi S, Hashimoto W, Kaneda S. A Smartphone Application for Personalized Tooth Shade Determination. Diagnostics. 2023; 13(11):1969. https://doi.org/10.3390/diagnostics13111969
Chicago/Turabian StyleKusayanagi, Tomoya, Sota Maegawa, Shuya Terauchi, Wataru Hashimoto, and Shohei Kaneda. 2023. "A Smartphone Application for Personalized Tooth Shade Determination" Diagnostics 13, no. 11: 1969. https://doi.org/10.3390/diagnostics13111969
APA StyleKusayanagi, T., Maegawa, S., Terauchi, S., Hashimoto, W., & Kaneda, S. (2023). A Smartphone Application for Personalized Tooth Shade Determination. Diagnostics, 13(11), 1969. https://doi.org/10.3390/diagnostics13111969







