Long COVID in Children: A Multidisciplinary Review
Abstract
:1. Introduction
2. Materials and Methods
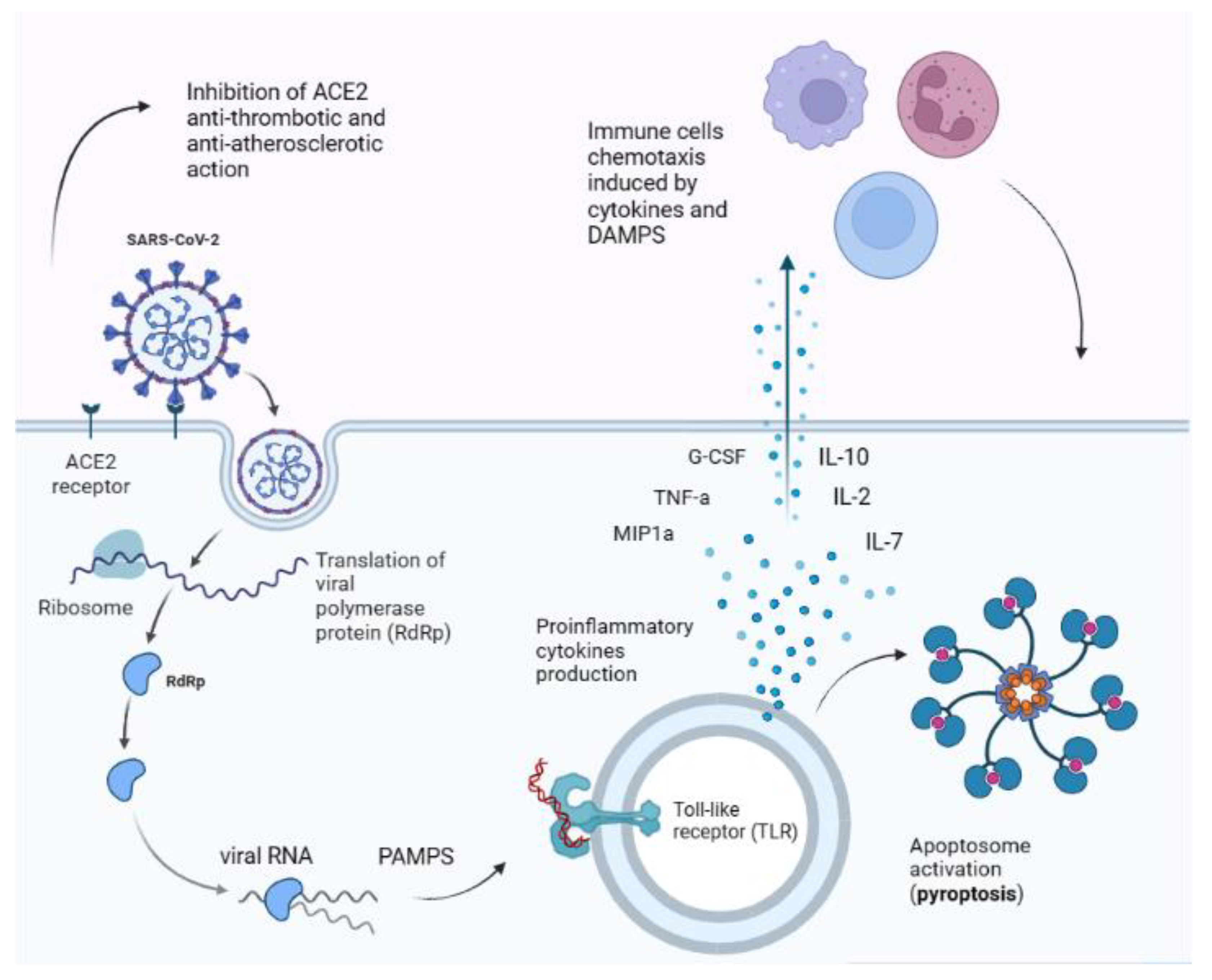
3. Pathophysiology
4. Long COVID in Children: Background and Definition
5. Long COVID Assessment in Children
5.1. Respiratory Assessment
5.1.1. Pulmonary Function Tests (PFTs)
5.1.2. Thoracic Imaging
5.2. Upper Airway Assessment
5.2.1. Olfactory Disfunction
5.2.2. Rhinological Symptoms
5.2.3. Otological Symptoms
5.2.4. Pharyngeal Symptoms
5.3. Gastrointestinal Assessment
5.4. Cardiologic Assessment
5.5. Common Motor Syndromes
5.6. Neurologic Assessment
5.6.1. Epidemiology, Clinical Phenotypes and Their Clinical Course
5.6.2. Putative Pathogenetic Mechanisms
5.6.3. The Strange Case of ME/CFS and What We Can Learn about Long COVID in Children
- i.
- a dysregulation of the 2-5A synthetase/ribonuclease L antiviral defence pathway [137];
- ii.
- an inhibition of the hypothalamus–pituitary–adrenal (HPA) axis, thus leading to hypocortisolism [138];
- iii.
- an altered sympathetic nervous activity, as demonstrated by orthostatic intolerance in these patients [139].
5.7. Psychological Aspects
6. Clinical Approach: From Diagnosis to Follow-Up
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Worldometer, C.C. Worldometer. Available online: https://www.worldometers.info/ (accessed on 10 December 2022).
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/?mapFilter=deaths (accessed on 10 December 2022).
- WHO Coronavirus Disease (COVID-19): Schools. Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-schools (accessed on 10 December 2022).
- American Academy of Pediatrics Children and COVID-19: State-Level Data Report (Aap.Org). Available online: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/ (accessed on 10 December 2022).
- Fiolet, T.; Kherabi, Y.; MacDonald, C.J.; Ghosn, J.; Peiffer-Smadja, N. Comparing COVID-19 Vaccines for Their Characteristics, Efficacy and Effectiveness against SARS-CoV-2 and Variants of Concern: A Narrative Review. Clin. Microbiol. Infect. 2022, 28, 202–221. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-Acute COVID-19 Syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F. Case Report and Systematic Review Suggest That Children May Experience Similar Long-Term Effects to Adults after Clinical COVID-19. Acta Paediatr. Int. J. Paediatr. 2021, 110, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Buonsenso, D.; Munblit, D.; De Rose, C.; Sinatti, D.; Ricchiuto, A.; Carfi, A.V.P. Preliminary Evidence on Long COVID in Children. Acta Paediatr. 2021, 110, 2208–2211. [Google Scholar] [CrossRef] [PubMed]
- Say, D.; Crawford, N.; McNab, S.; Wurzel, D.; Steer, A.T.S. Post-Acute COVID-19 Outcomes in Children with Mild and Asymptomatic Disease. Lancet Child Adolesc. Health 2021, 5, e22–e23. [Google Scholar] [CrossRef]
- Jennings, G.; Monaghan, A.; Xue, F.; Mockler, D.; Romero-Ortuño, R. A Systematic Review of Persistent Symptoms and Residual Abnormal Functioning Following Acute COVID-19: Ongoing Symptomatic Phase vs. Post-COVID-19 Syndrome. J. Clin. Med. 2021, 10, 5913. [Google Scholar] [CrossRef]
- Huang, Q.; Wu, X.; Zheng, X.; Luo, S.; Xu, S.W.J. Targeting Inflammation and Cytokine Storm in COVID-19. Pharmacol. Res. 2020, 159, 105051. [Google Scholar] [CrossRef]
- Tay, M.Z.; Poh, C.M.; Rénia, L.; MacAry, P.A.; Ng, L.F.P. The Trinity of COVID-19: Immunity, Inflammation and Intervention. Nat. Rev. Immunol. 2020, 20, 363–374. [Google Scholar] [CrossRef]
- Weinstock, L.B.; Brook, J.B.; Walters, A.S.; Goris, A.; Afrin, L.B.; Molderings, G.J. Mast Cell Activation Symptoms Are Prevalent in Long-COVID. Int. J. Infect. Dis. 2021, 112, 217–226. [Google Scholar] [CrossRef]
- Biswas, S.; Thakur, V.; Kaur, P.; Khan, A.; Kulshrestha, S.K.P. Blood Clots in COVID-19 Patients: Simplifying the Curious Mystery. Med. Hypotheses 2021, 146, 110371. [Google Scholar] [CrossRef]
- Yonts, A.B. Pediatric Long-COVID: A Review of the Definition, Epidemiology, Presentation, and Pathophysiology. Pediatr. Ann. 2022, 51, e416–e420. [Google Scholar] [CrossRef]
- Huang, Y.; Yang, C.; Xu, X.-F.; Xu, W.; Liu, S.-W. Structural and Functional Properties of SARS-CoV-2 Spike Protein: Potential Antivirus Drug Development for COVID-19. Acta Pharmacol. Sin. 2020, 41, 1141–1149. [Google Scholar] [CrossRef] [PubMed]
- Gusev, E.; Sarapultsev, A.; Solomatina, L.; Chereshnev, V. SARS-CoV-2-Specific Immune Response and the Pathogenesis of COVID-19. Int. J. Mol. Sci. 2022, 23, 1716. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.B.; Farzan, M.; Chen, B.; Choe, H. Mechanisms of SARS-CoV-2 Entry into Cells. Nat. Rev. Mol. Cell Biol. 2022, 23, 3–20. [Google Scholar] [CrossRef]
- Alipoor, S.D.; Mirsaeidi, M. SARS-CoV-2 Cell Entry beyond the ACE2 Receptor. Mol. Biol. Rep. 2022, 49, 10715–10727. [Google Scholar] [CrossRef]
- Lim, S.; Zhang, M.; Chang, T.L. ACE2-Independent Alternative Receptors for SARS-CoV-2. Viruses 2022, 14, 2535. [Google Scholar] [CrossRef]
- Zheng, H.Y.; Zhang, M.; Yang, C.X.; Zhang, N.; Wang, X.C.; Yang, X.P.; Dong, X.Q.; Zheng, T.Y. Elevated Exhaustion Levels and Reduced Functional Diversity of T Cells in Peripheral Blood May Predict Severe Progression in COVID-19 Patients. Cell Mol. Immunol. 2020, 17, 541–543. [Google Scholar] [CrossRef]
- Lee, W.S.; Wheatley, A.K.; Kent, S.J.; Dekosky, B. Antibody-Dependent Enhancement and SARS-CoV-2 Vaccines and Therapies. Nat. Microbiol. 2020, 5, 1185–1191. [Google Scholar] [CrossRef]
- Tirado, S.M.; Yoon, K.J. Antibody-Dependent Enhancement of Virus Infection and Disease. Viral Immunol. 2003, 16, 69–86. [Google Scholar] [CrossRef]
- Sante, G.D.; De Rose, D.B.C.; Valentini, P.; Ria, F.; Sanguinetti, M. Immune Profile of Children with Post-Acute Sequelae of SARS-CoV-2 Infection (Long COVID). MedRxiv 2021. [Google Scholar] [CrossRef]
- Daher, A.; Balfanz, P.; Cornelissen, C.; Müller, A.; Bergs, I.; Marx, N.; Müller-Wieland, D.; Hartmann, B.; Dreher, M.; Müller, T. Follow up of Patients with Severe Coronavirus Disease 2019 (COVID-19): Pulmonary and Extrapulmonary Disease Sequelae. Respir. Med. 2020, 174, 106197. [Google Scholar] [CrossRef] [PubMed]
- Fainardi, V.; Meoli, A.; Chiopris, G.; Motta, M.; Skenderaj, K.; Grandinetti, R.; Bergomi, A.; Antodaro, F.; Zona, S.; Esposito, S. Long COVID in Children and Adolescents. Life 2022, 12, 285. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, T.; Shafran, R.; Ladhani, S.N. Long COVID (Post-COVID-19 Condition) in Children: A Modified Delphi Process. Arch. Dis. Child. 2022, 107, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Ayuzo del Valle, N.C.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. Long-COVID in Children and Adolescents: A Systematic Review and Meta-Analyses. Sci. Rep. 2022, 12, 9950. [Google Scholar] [CrossRef]
- Asadi-Pooya, A.A.; Nemati, H.; Shahisavandi, M.; Akbari, A.; Emami, A.; Lotfi, M.; Rostamihosseinkhani, M.; Barzegar, Z.; Kabiri, M.; Zeraatpisheh, Z.; et al. Long COVID in Children and Adolescents. World J. Pediatr. 2021, 17, 495–499. [Google Scholar] [CrossRef]
- Miller, F.; Nguyen, V.; Navaratnam, A.M.D.; Shrotri, M.; Kovar, J.; Hayward, A.C.; Fragaszy, E.; Aldridge, R.W.; Hardelid, P. Prevalence of Persistent Symptoms in Children during the COVID-19 Pandemic: Evidence from a Household Cohort Study in England and Wales. MedRxiv 2021, 41, 979–984. [Google Scholar] [CrossRef]
- Osmanov, I.M.; Spiridonova, E.; Bobkova, P.; Gamirova, A.; Shikhaleva, A.; Andreeva, M.; Blyuss, O.; El-Taravi, Y.; DunnGalvin, A.; Comberiati, P.; et al. Risk Factors for Long COVID in Previously Hospitalised Children Using the ISARIC Global Follow-up Protocol: A Prospective Cohort Study. Eur. Respir. J. 2022, 59, 2101341. [Google Scholar] [CrossRef]
- Molteni, E.; Absoud, M.; Duncan, E.L. Assessing the Impact of the Pandemic in Children and Adolescents: SARS-CoV-2 Infection and Beyond. Lancet Child Adolesc. Health 2022, 6, 216–217. [Google Scholar] [CrossRef]
- Borch, L.; Holm, M.; Knudsen, M.; Ellermann-Eriksen, S.; Hagstroem, S. Long COVID Symptoms and Duration in SARS-CoV-2 Positive Children—A Nationwide Cohort Study. Eur. J. Pediatr. 2022, 181, 1597–1607. [Google Scholar] [CrossRef]
- Torres-Castro, R.; Vasconcello-Castillo, L.; Alsina-Restoy, X.; Solis-Navarro, L.; Burgos, F.; Puppo, H.; Vilaró, J. Respiratory Function in Patients Post-Infection by COVID-19: A Systematic Review and Meta-Analysis. Pulmonology 2021, 27, 328–337. [Google Scholar] [CrossRef]
- Ng, C.K. Six Month Radiological and Physiological Outcomes in Severe Acute Respiratory Syndrome (SARS) Survivors. Thorax 2004, 59, 889–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leftin Dobkin, S.C.; Collaco, J.M.; McGrath-Morrow, S.A. Protracted Respiratory Findings in Children Post-SARS-CoV-2 Infection. Pediatr. Pulmonol. 2021, 56, 3682–3687. [Google Scholar] [CrossRef] [PubMed]
- Doležalová, K.; Tuková, J.; Pohunek, P. The Respiratory Consequences of COVID-19 Lasted for a Median of 4 Months in a Cohort of Children Aged 2–18 Years of Age. Acta Paediatr. Int. J. Paediatr. 2022, 111, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazi-Hoffnung, L.; Shmueli, E.; Ehrlich, S.; Ziv, A.; Bar-On, O.; Birk, E.; Lowenthal, A.; Prais, D. Long COVID in Children: Observations from a Designated Pediatric Clinic. Pediatr. Infect. Dis. J. 2021, 40, E509–E511. [Google Scholar] [CrossRef] [PubMed]
- La Regina, D.P.; Pepino, D.; Nenna, R.; Iovine, E.; Mancino, E.; Andreoli, G.; Zicari, A.M.; Spalice, A.; Midulla, F. Pediatric COVID-19 Follow-Up with Lung Ultrasound: A Prospective Cohort Study. Diagnostics 2022, 12, 2202. [Google Scholar] [CrossRef] [PubMed]
- Heiss, R.; Tan, L.; Schmidt, S.; Regensburger, A.P.; Ewert, F.; Mammadova, D.; Buehler, A.; Vogel-Claussen, J.; Voskrebenzev, A.; Rauh, M.; et al. Pulmonary Dysfunction after Pediatric COVID-19. Radiology 2022, 306, 221250. [Google Scholar] [CrossRef]
- Rinaldo, R.F.; Mondoni, M.; Parazzini, E.M.; Pitari, F.; Brambilla, E.; Luraschi, S.; Balbi, M.; Papa, G.F.S.; Sotgiu, G.; Guazzi, M.; et al. Deconditioning as Main Mechanism of Impaired Exercise in COVID-19 Survivors. Eur. Respir. J. 2021, 58, 2100870. [Google Scholar] [CrossRef]
- Esmaeilzadeh, H.; Sanaei Dashti, A.; Mortazavi, N.; Fatemian, H.; Vali, M. Persistent Cough and Asthma-like Symptoms Post COVID-19 Hospitalization in Children. BMC Infect. Dis. 2022, 22, 244. [Google Scholar] [CrossRef]
- Mikhail, I.; Grayson, M.H. Asthma and Viral Infections. Ann. Allergy Asthma Immunol. 2019, 123, 352–358. [Google Scholar] [CrossRef] [Green Version]
- Soldati, G.; Demi, M. What Is COVID 19 Teaching Us about Pulmonary Ultrasound? Diagnostics 2022, 12, 838. [Google Scholar] [CrossRef]
- Musolino, A.M.; Supino, M.C.; Buonsenso, D.; Ferro, V.; Valentini, P.; Magistrelli, A.; Lombardi, M.H.; Romani, L.; D’Argenio, P.; Campana, A. Lung Ultrasound in Children with COVID-19: Preliminary Findings. Ultrasound Med. Biol. 2020, 46, 2094–2098. [Google Scholar] [CrossRef] [PubMed]
- Caroselli, C.; Blaivas, M.; Falzetti, S. Diagnostic Imaging in Newborns, Children and Adolescents Infected with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Is There a Realistic Alternative to Lung High-Resolution Computed Tomography (HRCT) and Chest X-Rays? A Systematic Review of the Literature. Ultrasound Med. Biol. 2021, 47, 3034–3040. [Google Scholar] [CrossRef] [PubMed]
- Sferrazza Papa, G.F.; Pellegrino, G.M.; Volpicelli, G.; Sferrazza Papa, S.; di Marco, F.; Mondoni, M.; Centanni, S. Lung Ultrasound B Lines: Etiologies and Evolution with Age. Respiration 2017, 94, 313–314. [Google Scholar] [CrossRef]
- Hau Ng, B.; Nuratiqah Nik Abeed, N.; Ban Yu-Lin, A.; Faisal Abdul Hamid, M.; Ian Soo, C.; Kori, N.; Azura Mohamed Mukari, S.; Azzaki Zainal, I.; Kamaruzaman, L.; Yusuf Abu Shamsi, M.; et al. Lung Computed Tomography Patterns of a Cluster of Asymptomatic Young Males with COVID-19 Admitted to a Teaching Hospital in Kuala Lumpur. Med. J. Malays. 2020, 75, 368–371. [Google Scholar]
- Denina, M.; Pruccoli, G.; Scolfaro, C.; Mignone, F.; Zoppo, M.; Giraudo, I.; Silvestro, E.; Bertolotti, L.; Rosati, S.; Ramenghi, U.; et al. Sequelae of COVID-19 in Hospitalized Children: A 4-Months Follow-Up. Pediatr. Infect. Dis. J. 2020, 39, E458–E459. [Google Scholar] [CrossRef]
- Geiger, J.; Zeimpekis, K.G.; Jung, A.; Moeller, A.; Kellenberger, C.J. Clinical Application of Ultrashort Echo-Time MRI for Lung Pathologies in Children. Clin. Radiol. 2021, 76, 708.e9–708.e17. [Google Scholar] [CrossRef]
- Hirsch, W.; Sorge, I.; Krohmer, S.; Weber, D.; Meier, K.; Till, H. MRI of the Lungs in Children. Eur. J. Radiol. 2008, 68, 278–288. [Google Scholar] [CrossRef]
- Ley-Zaporozhan, J.; Ley, S.; Sommerburg, O.; Komm, N.; Müller, F.-M.; Schenk, J. Clinical Application of MRI in Children for the Assessment of Pulmonary Diseases. RöFo Fortschr. Geb. Röntgenstrahlen Bildgeb. Verfahr. 2009, 181, 419–432. [Google Scholar] [CrossRef]
- Bhatia, A.; Sodhi, K.S.; Gauba, R.; Mathew, J.L.; Bal, A. Pediatric Lung MRI in Pulmonary Alveolar Proteinosis: An Alternative to CT as a Radiation-Free Modality. Indian J. Pediatr. 2022, 89, 616–617. [Google Scholar] [CrossRef]
- Sodhi, K.S.; Gauba, R.; Bhatia, A.; Saxena, A.K.; Mathew, J.L. Lung MRI- Changing Paradigms in Evaluation of Chronic Granulomatous Disease in Children. J. Clin. Immunol. 2022, 42, 898–900. [Google Scholar] [CrossRef]
- Sodhi, K.S.; Sharma, M.; Lee, E.Y.; Saxena, A.K.; Mathew, J.L.; Singh, M.; Khandelwal, N. Diagnostic Utility of 3T Lung MRI in Children with Interstitial Lung Disease. Acad. Radiol. 2018, 25, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Liszewski, M.C.; Görkem, S.; Sodhi, K.S.; Lee, E.Y. Lung Magnetic Resonance Imaging for Pneumonia in Children. Pediatr. Radiol. 2017, 47, 1420–1430. [Google Scholar] [CrossRef]
- Renz, D.M.; Herrmann, K.-H.; Kraemer, M.; Boettcher, J.; Waginger, M.; Krueger, P.-C.; Pfeil, A.; Streitparth, F.; Kentouche, K.; Gruhn, B.; et al. Ultrashort Echo Time MRI of the Lung in Children and Adolescents: Comparison with Non-Enhanced Computed Tomography and Standard Post-Contrast T1w MRI Sequences. Eur. Radiol. 2022, 32, 1833–1842. [Google Scholar] [CrossRef] [PubMed]
- Serai, S.D.; Rapp, J.B.; States, L.J.; Andronikou, S.; Ciet, P.; Lee, E.Y. Pediatric Lung MRI: Currently Available and Emerging Techniques. Am. J. Roentgenol. 2021, 216, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Wielpütz, M.O.; von Stackelberg, O.; Stahl, M.; Jobst, B.J.; Eichinger, M.; Puderbach, M.U.; Nährlich, L.; Barth, S.; Schneider, C.; Kopp, M.V.; et al. Multicentre Standardisation of Chest MRI as Radiation-Free Outcome Measure of Lung Disease in Young Children with Cystic Fibrosis. J. Cyst. Fibros. 2018, 17, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Yucel, S.; Aycicek, T.; Ceyhan Bilgici, M.; Dincer, O.S.; Tomak, L. 3 Tesla MRI in Diagnosis and Follow up of Children with Pneumonia. Clin. Imaging 2021, 79, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Sansone, F.; Attanasi, M.; di Filippo, P.; Sferrazza Papa, G.F.; di Pillo, S.; Chiarelli, F. Usefulness of Lung Ultrasound in Paediatric Respiratory Diseases. Diagnostics 2021, 11, 1783. [Google Scholar] [CrossRef]
- Meliante, P.G.; Marcellino, A.; Altomari, R.; Testa, A.; Gallo, A.; Ralli, M.; de Vincentiis, M.; Lubrano, R. Smell and Taste in Children with COVID-19. Allergy Rhinol. 2022, 13, 215265752211449. [Google Scholar] [CrossRef]
- Rusetsky, Y.; Meytel, I.; Mokoyan, Z.; Fisenko, A.; Babayan, A.; Malyavina, U. Smell Status in Children Infected with SARS-CoV-2. Laryngoscope 2021, 131, E2475–E2480. [Google Scholar] [CrossRef]
- Roge, I.; Smane, L.; Kivite-Urtane, A.; Pucuka, Z.; Racko, I.; Klavina, L.; Pavare, J. Comparison of Persistent Symptoms after COVID-19 and Other Non-SARS-CoV-2 Infections in Children. Front. Pediatr. 2021, 9, 752385. [Google Scholar] [CrossRef]
- Raad, N.; Ghorbani, J.; Mikaniki, N.; Haseli, S.; Karimi-Galougahi, M. Otitis Media in Coronavirus Disease 2019: A Case Series. J. Laryngol. Otol. 2021, 135, 10–13. [Google Scholar] [CrossRef] [PubMed]
- Götzinger, F.; Santiago-García, B.; Noguera-Julián, A.; Lanaspa, M.; Lancella, L.; Calò Carducci, F.I.; Gabrovska, N.; Velizarova, S.; Prunk, P.; Osterman, V.; et al. COVID-19 in Children and Adolescents in Europe: A Multinational, Multicentre Cohort Study. Lancet Child Adolesc. Health 2020, 4, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Zavala, M.; Ireland, G.; Amin-Chowdhury, Z.; Ramsay, M.E.; Ladhani, S.N. Acute and Persistent Symptoms in Children with Polymerase Chain Reaction (PCR)–Confirmed Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection Compared with Test-Negative Children in England: Active, Prospective, National Surveillance. Clin. Infect. Dis. 2022, 75, e191–e200. [Google Scholar] [CrossRef] [PubMed]
- Cooper, S.; Tobar, A.; Konen, O.; Orenstein, N.; Kropach Gilad, N.; Landau, Y.E.; Mozer-Glassberg, Y.; Bar-Lev, M.R.; Shaoul, R.; Shamir, R.; et al. Long COVID-19 Liver Manifestation in Children. J. Pediatr. Gastroenterol. Nutr. 2022, 75, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Meringer, H.; Mehandru, S. Gastrointestinal Post-Acute COVID-19 Syndrome. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 345–346. [Google Scholar] [CrossRef]
- Mohamed, D.Z.; Ghoneim, M.E.-S.; Abu-Risha, S.E.-S.; Abdelsalam, R.A.; Farag, M.A. Gastrointestinal and Hepatic Diseases during the COVID-19 Pandemic: Manifestations, Mechanism and Management. World J. Gastroenterol. 2021, 27, 4504–4535. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major Findings, Mechanisms and Recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Yeoh, Y.K.; Zuo, T.; Lui, G.C.-Y.; Zhang, F.; Liu, Q.; Li, A.Y.; Chung, A.C.; Cheung, C.P.; Tso, E.Y.; Fung, K.S.; et al. Gut Microbiota Composition Reflects Disease Severity and Dysfunctional Immune Responses in Patients with COVID-19. Gut 2021, 70, 698–706. [Google Scholar] [CrossRef]
- Natarajan, A.; Zlitni, S.; Brooks, E.F.; Vance, S.E.; Dahlen, A.; Hedlin, H.; Park, R.M.; Han, A.; Schmidtke, D.T.; Verma, R.; et al. Gastrointestinal Symptoms and Fecal Shedding of SARS-CoV-2 RNA Suggest Prolonged Gastrointestinal Infection. Med 2022, 3, 371–387.e9. [Google Scholar] [CrossRef]
- Zollner, A.; Koch, R.; Jukic, A.; Pfister, A.; Meyer, M.; Rössler, A.; Kimpel, J.; Adolph, T.E.; Tilg, H. Postacute COVID-19 Is Characterized by Gut Viral Antigen Persistence in Inflammatory Bowel Diseases. Gastroenterology 2022, 163, 495–506.e8. [Google Scholar] [CrossRef]
- De Almeida, V.M.; Engel, D.F.; Ricci, M.F.; Cruz, C.S.; Lopes, I.S.; Alves, D.A.; Auriol, M.; Magalhães, J.; Zuccoli, G.S.; Smith, B.J.; et al. Gut Microbiota from Patients with Mild COVID-19 Cause Alterations in Mice That Resemble Post-COVID Syndrome. Res. Sq. 2022; preprint. [Google Scholar] [CrossRef]
- Morello, R.; de Rose, C.; Cardinali, S.; Valentini, P.; Buonsenso, D. Lactoferrin as Possible Treatment for Chronic Gastrointestinal Symptoms in Children with Long COVID: Case Series and Literature Review. Children 2022, 9, 1446. [Google Scholar] [CrossRef] [PubMed]
- Buonsenso, D.; di Gennaro, L.; de Rose, C.; Morello, R.; D’Ilario, F.; Zampino, G.; Piazza, M.; Boner, A.L.; Iraci, C.; O’Connell, S.; et al. Long-Term Outcomes of Pediatric Infections: From Traditional Infectious Diseases to Long COVID. Future Microbiol. 2022, 17, 551–571. [Google Scholar] [CrossRef] [PubMed]
- Evans, S.S.; Repasky, E.A.; Fisher, D.T. Fever and the Thermal Regulation of Immunity: The Immune System Feels the Heat. Nat. Rev. Immunol. 2015, 15, 335–349. [Google Scholar] [CrossRef] [PubMed]
- Barizien, N.; le Guen, M.; Russel, S.; Touche, P.; Huang, F.; Vallée, A. Clinical Characterization of Dysautonomia in Long COVID-19 Patients. Sci. Rep. 2021, 11, 14042. [Google Scholar] [CrossRef] [PubMed]
- Boris, J.R.; Moak, J.P. Pediatric Postural Orthostatic Tachycardia Syndrome: Where We Stand. Pediatrics 2022, 150, e2021054945. [Google Scholar] [CrossRef]
- Yong, S.J. Long COVID or Post-COVID-19 Syndrome: Putative Pathophysiology, Risk Factors, and Treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef]
- Buchhorn, R. Dysautonomia in Children with Post-Acute Sequelae of Coronavirus 2019 Disease and/or Vaccination. Vaccines 2022, 10, 1686. [Google Scholar] [CrossRef] [PubMed]
- Kokorelis, C.; Malone, L.; Byrne, K.; Morrow, A.; Rowe, P.C. Onset of Postural Orthostatic Tachycardia Syndrome (POTS) Following COVID-19 Infection: A Pediatric Case Report. Clin. Pediatr. 2023, 62, 92–95. [Google Scholar] [CrossRef]
- Shechter, A.; Yelin, D.; Margalit, I.; Abitbol, M.; Morelli, O.; Hamdan, A.; Vaturi, M.; Eisen, A.; Sagie, A.; Kornowski, R.; et al. Assessment of Adult Patients with Long COVID Manifestations Suspected as Cardiovascular: A Single-Center Experience. J. Clin. Med. 2022, 11, 6123. [Google Scholar] [CrossRef]
- Bocci, T.; Bertini, A.; Campiglio, L.; Botta, S.; Libelli, G.; Guidetti, M.; Priori, A. Not Myopathic, but Autonomic Changes in Patients with Long-COVID Syndrome: A Case Series. Neurol. Sci. 2023, 44, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Safavi, F.; Gustafson, L.; Walitt, B.; Lehky, T.; Dehbashi, S.; Wiebold, A.; Mina, Y.; Shin, S.; Pan, B.; Polydefkis, M.; et al. Neuropathic Symptoms with SARS-CoV-2 Vaccination. MedRxiv, 2022; preprint. [Google Scholar] [CrossRef]
- Oaklander, A.L.; Mills, A.J.; Kelley, M.; Toran, L.S.; Smith, B.; Dalakas, M.C.; Nath, A. Peripheral Neuropathy Evaluations of Patients with Prolonged Long COVID. Neurol. Neuroimmunol. Neuroinflammation 2022, 9, e1146. [Google Scholar] [CrossRef] [PubMed]
- Abrams, R.M.C.; Simpson, D.M.; Navis, A.; Jette, N.; Zhou, L.; Shin, S.C. Small Fiber Neuropathy Associated with SARS-CoV-2 Infection. Muscle Nerve 2022, 65, 440–443. [Google Scholar] [CrossRef]
- Bitirgen, G.; Korkmaz, C.; Zamani, A.; Ozkagnici, A.; Zengin, N.; Ponirakis, G.; Malik, R.A. Corneal Confocal Microscopy Identifies Corneal Nerve Fibre Loss and Increased Dendritic Cells in Patients with Long COVID. Br. J. Ophthalmol. 2022, 106, 1635–1641. [Google Scholar] [CrossRef]
- Morello, R.; Martino, L.; Buonsenso, D. Diagnosis and Management of Post-COVID (Long COVID) in Children: A Moving Target. Curr. Opin. Pediatr. 2023, 35, 184–192. [Google Scholar] [CrossRef]
- Pellegrino, R.; Chiappini, E.; Licari, A.; Galli, L.; Marseglia, G.L. Prevalence and Clinical Presentation of Long COVID in Children: A Systematic Review. Eur. J. Pediatr. 2022, 181, 3995–4009. [Google Scholar] [CrossRef]
- Hickie, I.; Davenport, T.; Wakefield, D.; Vollmer-Conna, U.; Cameron, B.; Vernon, S.D.; Reeves, W.C.; Lloyd, A. Post-Infective and Chronic Fatigue Syndromes Precipitated by Viral and Non-Viral Pathogens: Prospective Cohort Study. BMJ 2006, 16, 7568. [Google Scholar] [CrossRef] [Green Version]
- Ariza, M.E. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: The Human Herpesviruses Are Back! Biomolecules 2021, 11, 185. [Google Scholar] [CrossRef]
- Montani, D.; Savale, L.; Noel, N.; Meyrignac, O.; Colle, R.; Gasnier, M.; Corruble, E.; Beurnier, A.; Jutant, E.-M.; Pham, T.; et al. Post-Acute COVID-19 Syndrome. Eur. Respir. Rev. 2022, 31, 210185. [Google Scholar] [CrossRef]
- Araja, D.; Berkis, U.; Lunga, A.; Murovska, M. Shadow Burden of Undiagnosed Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) on Society: Retrospective and Prospective-In Light of COVID-19. J. Clin. Med. 2021, 10, 3017. [Google Scholar] [CrossRef] [PubMed]
- Komaroff, A.L.; Lipkin, W.I. Insights from Myalgic Encephalomyelitis/Chronic Fatigue Syndrome May Help Unravel the Pathogenesis of Postacute COVID-19 Syndrome. Trends Mol. Med. 2021, 27, 895–906. [Google Scholar] [CrossRef] [PubMed]
- Tarantino, S.; Graziano, S.; Carducci, C.; Giampaolo, R.; Grimaldi Capitello, T. Cognitive Difficulties, Psychological Symptoms, and Long Lasting Somatic Complaints in Adolescents with Previous SARS-CoV-2 Infection: A Telehealth Cross-Sectional Pilot Study. Brain Sci. 2022, 12, 969. [Google Scholar] [CrossRef]
- Morrow, A.K.; Ng, R.; Vargas, G.; Jashar, D.T.; Henning, E.; Stinson, N.; Malone, L.A. Postacute/Long COVID in Pediatrics: Development of a Multidisciplinary Rehabilitation Clinic and Preliminary Case Series. Am. J. Phys. Med. Rehabil. 2021, 100, 1140–1147. [Google Scholar] [CrossRef]
- Hernández-Sampelayo, T.; Gómez-Pavón, J.; González del Castillo, J.; Martín-Delgado, M.C.; Martín-Sánchez, F.J.; Martínez-Sellés, M.; Molero García, J.M.; Moreno Guillén, S.; Rodríguez-Artalejo, F.; Ruiz-Galiana, J.; et al. COVID in Pediatric Age: An Opinion Paper. Rev. Española Quimioter. 2022, 35, 333–343. [Google Scholar] [CrossRef]
- Mizrahi, B.; Sudry, T.; Flaks-Manov, N.; Yehezkelli, Y.; Kalkstein, N.; Akiva, P.; Ekka-Zohar, A.; ben David, S.S.; Lerner, U.; Bivas-Benita, M.; et al. Long COVID Outcomes at One Year after Mild SARS-CoV-2 Infection: Nationwide Cohort Study. BMJ 2023, 380, e072529. [Google Scholar] [CrossRef]
- Hicks, S.D. Comparison of Symptom Duration Between Children With SARS-CoV-2 and Peers With Other Viral Illnesses During the COVID-19 Pandemic. Clin. Pediatr. 2023, 00099228231152840. [Google Scholar] [CrossRef] [PubMed]
- Parisi, G.F.; Diaferio, L.; Brindisi, G.; Indolfi, C.; Umano, G.R.; Klain, A.; Marchese, G.; Ghiglioni, D.G.; Zicari, A.M.; Marseglia, G.L.; et al. Cross-Sectional Survey on Long Term Sequelae of Pediatric COVID-19 among Italian Pediatricians. Children 2021, 8, 769. [Google Scholar] [CrossRef]
- Bocci, T.; Campiglio, L.; Priori, A. Disorders of Cranial and Spinal Nerves; Milano University Press: Milan, Italy, 2021; ISBN 9791280325372. [Google Scholar]
- Chou, S.H.-Y.; Beghi, E.; Helbok, R.; Moro, E.; Sampson, J.; Altamirano, V.; Mainali, S.; Bassetti, C.; Suarez, J.I.; McNett, M.; et al. Global Incidence of Neurological Manifestations among Patients Hospitalized with COVID-19—A Report for the GCS-NeuroCOVID Consortium and the ENERGY Consortium. JAMA Netw. Open 2021, 4, e2112131. [Google Scholar] [CrossRef]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683. [Google Scholar] [CrossRef] [Green Version]
- Piazza, M.; di Cicco, M.; Pecoraro, L.; Ghezzi, M.; Peroni, D.; Comberiati, P. Long COVID-19 in Children: From the Pathogenesis to the Biologically Plausible Roots of the Syndrome. Biomolecules 2022, 12, 556. [Google Scholar] [CrossRef]
- Troitskaya, L.A.; Plotnikova, I.A.; Avakyan, G.G.; Erokhina, V.A.; Badalyan, O.L.; Muraveva, A.V.; Zelentsova, V.L.; Khodko, O.K.; Safarova, S.T.; Shirokova, E.I.; et al. Neuropsychological Evaluation of Cognitive Disorders in Children after COVID-19. Eur. J. Transl. Myol. 2022, 32. [Google Scholar] [CrossRef]
- Ferrucci, R.; Dini, M.; Rosci, C.; Capozza, A.; Groppo, E.; Reitano, M.R.; Allocco, E.; Poletti, B.; Brugnera, A.; Bai, F.; et al. One-year Cognitive Follow-up of COVID-19 Hospitalized Patients. Eur. J. Neurol. 2022, 29, 2006–2014. [Google Scholar] [CrossRef] [PubMed]
- Gentile, F.; Bocci, T.; Coppola, S.; Pozzi, T.; Modafferi, L.; Priori, A.; Chiumello, D. Putative Role of the Lung–Brain Axis in the Pathogenesis of COVID-19-Associated Respiratory Failure: A Systematic Review. Biomedicines 2022, 10, 729. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.E.; Asfour, A.; Sewell, T.B.; Hooe, B.; Pryce, P.; Earley, C.; Shen, M.Y.; Kerner-Rossi, M.; Thakur, K.T.; Vargas, W.S.; et al. Neurological Issues in Children with COVID-19. Neurosci. Lett. 2021, 743, 135567. [Google Scholar] [CrossRef]
- Dufort, E.M.; Koumans, E.H.; Chow, E.J.; Rosenthal, E.M.; Muse, A.; Rowlands, J.; Barranco, M.A.; Maxted, A.M.; Rosenberg, E.S.; Easton, D.; et al. Multisystem Inflammatory Syndrome in Children in New York State. N. Engl. J. Med. 2020, 383, 347–358. [Google Scholar] [CrossRef]
- Feldstein, L.R.; Rose, E.B.; Horwitz, S.M.; Collins, J.P.; Newhams, M.M.; Son, M.B.F.; Newburger, J.W.; Kleinman, L.C.; Heidemann, S.M.; Martin, A.A.; et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N. Engl. J. Med. 2020, 383, 334–346. [Google Scholar] [CrossRef]
- Abdel-Mannan, O.; Eyre, M.; Löbel, U.; Bamford, A.; Eltze, C.; Hameed, B.; Hemingway, C.; Hacohen, Y. Neurologic and Radiographic Findings Associated with COVID-19 Infection in Children. JAMA Neurol. 2020, 77, 1440. [Google Scholar] [CrossRef] [PubMed]
- Dugue, R.; Cay-Martínez, K.C.; Thakur, K.T.; Garcia, J.A.; Chauhan, L.V.; Williams, S.H.; Briese, T.; Jain, K.; Foca, M.; McBrian, D.K.; et al. Neurologic Manifestations in an Infant with COVID-19. Neurology 2020, 94, 1100–1102. [Google Scholar] [CrossRef] [Green Version]
- Abel, D.; Shen, M.Y.; Abid, Z.; Hennigan, C.; Boneparth, A.; Miller, E.H.; Uhlemann, A.-C.; McBrian, D.K.; Thakur, K.; Silver, W.; et al. Encephalopathy and Bilateral Thalamic Lesions in a Child with MIS-C Associated with COVID-19. Neurology 2020, 95, 745–748. [Google Scholar] [CrossRef]
- Sominsky, L.; de Luca, S.; Spencer, S.J. Microglia: Key Players in Neurodevelopment and Neuronal Plasticity. Int. J. Biochem. Cell Biol. 2018, 94, 56–60. [Google Scholar] [CrossRef]
- Muccigrosso, M.M.; Ford, J.; Benner, B.; Moussa, D.; Burnsides, C.; Fenn, A.M.; Popovich, P.G.; Lifshitz, J.; Walker, F.R.; Eiferman, D.S.; et al. Cognitive Deficits Develop 1 Month after Diffuse Brain Injury and Are Exaggerated by Microglia-Associated Reactivity to Peripheral Immune Challenge. Brain Behav. Immun. 2016, 54, 95–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galatro, T.F.; Holtman, I.R.; Lerario, A.M.; Vainchtein, I.D.; Brouwer, N.; Sola, P.R.; Veras, M.M.; Pereira, T.F.; Leite, R.E.P.; Möller, T.; et al. Transcriptomic Analysis of Purified Human Cortical Microglia Reveals Age-Associated Changes. Nat. Neurosci. 2017, 20, 1162–1171. [Google Scholar] [CrossRef]
- Yang, Q.; Hughes, T.A.; Kelkar, A.; Yu, X.; Cheng, K.; Park, S.; Huang, W.-C.; Lovell, J.F.; Neelamegham, S. Inhibition of SARS-CoV-2 Viral Entry upon Blocking N- and O-Glycan Elaboration. Elife 2020, 9, e61552. [Google Scholar] [CrossRef]
- Han, T.; Kang, J.; Li, G.; Ge, J.; Gu, J. Analysis of 2019-NCoV Receptor ACE2 Expression in Different Tissues and Its Significance Study. Ann. Transl. Med. 2020, 8, 1077. [Google Scholar] [CrossRef] [PubMed]
- Baig, A.M.; Khaleeq, A.; Ali, U.; Syeda, H. Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chem. Neurosci. 2020, 11, 995–998. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Bai, W.; Hashikawa, T. The Neuroinvasive Potential of SARS-CoV2 May Play a Role in the Respiratory Failure of COVID-19 Patients. J. Med. Virol. 2020, 92, 552–555. [Google Scholar] [CrossRef] [PubMed]
- Emmi, A.; Rizzo, S.; Barzon, L.; Sandre, M.; Carturan, E.; Sinigaglia, A.; Riccetti, S.; della Barbera, M.; Boscolo-Berto, R.; Cocco, P.; et al. Detection of SARS-CoV-2 Viral Proteins and Genomic Sequences in Human Brainstem Nuclei. NPJ Park. Dis. 2023, 9, 25. [Google Scholar] [CrossRef]
- Bocci, T.; Bulfamante, G.; Campiglio, L.; Coppola, S.; Falleni, M.; Chiumello, D.; Priori, A. Brainstem Clinical and Neurophysiological Involvement in COVID-19. J. Neurol. 2021, 268, 3598–3600. [Google Scholar] [CrossRef]
- Bulfamante, G.; Bocci, T.; Falleni, M.; Campiglio, L.; Coppola, S.; Tosi, D.; Chiumello, D.; Priori, A. Brainstem Neuropathology in Two Cases of COVID-19: SARS-CoV-2 Trafficking between Brain and Lung. J. Neurol. 2021, 268, 4486–4491. [Google Scholar] [CrossRef]
- Emmi, A.; Boura, I.; Raeder, V.; Mathew, D.; Sulzer, D.; Goldman, J.E.; Leta, V. COVID-19, Nervous System Pathology, and Parkinson’s Disease: Bench to Bedside. Int. Rev. Neurobiol. 2022, 165, 17–34. [Google Scholar]
- Emmi, A.; Sandre, M.; Porzionato, A.; Antonini, A. Smell Deficits in COVID-19 and Possible Links with Parkinson’s Disease. Int. Rev. Neurobiol. 2022, 165, 91–102. [Google Scholar] [PubMed]
- Horner, O.; Hedderly, T.; Malik, O. The Changing Landscape of Childhood Tic Disorders Following COVID-19. Paediatr. Child. Health 2022, 32, 363–367. [Google Scholar] [CrossRef]
- Bateman, L.; Bested, A.C.; Bonilla, H.F.; Chheda, B.V.; Chu, L.; Curtin, J.M.; Dempsey, T.T.; Dimmock, M.E.; Dowell, T.G.; Felsenstein, D.; et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of Diagnosis and Management. Mayo Clin. Proc. 2021, 96, 2861–2878. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Hernandez, O.-D.; Shoenfeld, Y. Infection, Vaccination, and Autoantibodies in Chronic Fatigue Syndrome, Cause or Coincidence? Ann. N. Y Acad. Sci. 2009, 1173, 600–609. [Google Scholar] [CrossRef]
- Wong, T.L.; Weitzer, D.J. Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)—A Systemic Review and Comparison of Clinical Presentation and Symptomatology. Medicina 2021, 57, 418. [Google Scholar] [CrossRef] [PubMed]
- Friedman, K.J.; Murovska, M.; Pheby, D.F.H.; Zalewski, P. Our Evolving Understanding of ME/CFS. Medicina 2021, 57, 200. [Google Scholar] [CrossRef]
- Komaroff, A.L.; Bateman, L. Will COVID-19 Lead to Myalgic Encephalomyelitis/Chronic Fatigue Syndrome? Front. Med. 2021, 7, 606824. [Google Scholar] [CrossRef]
- Katz, B.Z.; Shiraishi, Y.; Mears, C.J.; Binns, H.J.; Taylor, R. Chronic Fatigue Syndrome after Infectious Mononucleosis in Adolescents. Pediatrics 2009, 124, 189–193. [Google Scholar] [CrossRef] [Green Version]
- Jordan, K.M.; Huang, C.-F.; Jason, L.A.; Richman, J.; Mears, C.J.; McCready, W.; Katz, B.Z.; Ayers, P.M.; Rademaker, A.; Taylor, K.K. Prevalence of Pediatric Chronic Fatigue Syndrome in a Community-Based Sample. J. Chronic Fatigue Syndr. 2006, 13, 75–78. [Google Scholar] [CrossRef]
- Chu, L.; Valencia, I.J.; Garvert, D.W.; Montoya, J.G. Onset Patterns and Course of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Front. Pediatr. 2019, 7, 12. [Google Scholar] [CrossRef]
- Marshall-Gradisnik, S.; Huth, T.; Chacko, A.; Smith, P.; Staines, D.; Johnston, S. Natural Killer Cells and Single Nucleotide Polymorphisms of Specific Ion Channels and Receptor Genes in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Appl. Clin. Genet. 2016, 9, 39–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nijhof, S.L.; Rutten, J.M.T.M.; Uiterwaal, C.S.P.M.; Bleijenberg, G.; Kimpen, J.L.L.; van de Putte, E.M. The Role of Hypocortisolism in Chronic Fatigue Syndrome. Psychoneuroendocrinology 2014, 42, 199–206. [Google Scholar] [CrossRef]
- Wyller, V.B.; Vitelli, V.; Sulheim, D.; Fagermoen, E.; Winger, A.; Godang, K.; Bollerslev, J. Altered Neuroendocrine Control and Association to Clinical Symptoms in Adolescent Chronic Fatigue Syndrome: A Cross-Sectional Study. J. Transl. Med. 2016, 14, 121. [Google Scholar] [CrossRef] [Green Version]
- Sotzny, F.; Blanco, J.; Capelli, E.; Castro-Marrero, J.; Steiner, S.; Murovska, M.; Scheibenbogen, C. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome–Evidence for an Autoimmune Disease. Autoimmun. Rev. 2018, 17, 601–609. [Google Scholar] [CrossRef]
- Rowe, K. Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME) in Adolescents: Practical Guidance and Management Challenges. Adolesc. Health Med. Ther. 2023, 14, 13–26. [Google Scholar] [CrossRef] [PubMed]
- Hiremath, S.; Doukrou, M.; Flannery, H.; Carey, C.; Gregorowski, A.; Ward, J.; Hargreaves, D.; Segal, T.Y. Key Features of a Multi-Disciplinary Hospital-Based Rehabilitation Program for Children and Adolescents with Moderate to Severe Myalgic Encephalomyelitis/Chronic Fatigue Syndrome ME/CFS. Int. J. Environ. Res. Public Health 2022, 19, 13608. [Google Scholar] [CrossRef]
- White, P.; Goldsmith, K.; Johnson, A.; Potts, L.; Walwyn, R.; DeCesare, J.; Baber, H.; Burgess, M.; Clark, L.; Cox, D.; et al. Comparison of Adaptive Pacing Therapy, Cognitive Behaviour Therapy, Graded Exercise Therapy, and Specialist Medical Care for Chronic Fatigue Syndrome (PACE): A Randomised Trial. Lancet 2011, 377, 823–836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rowe, K.S. Double-Blind Randomized Controlled Trial to Assess the Efficacy of Intravenous Gammaglobulin for the Management of Chronic Fatigue Syndrome in Adolescents. J. Psychiatr. Res. 1997, 31, 133–147. [Google Scholar] [CrossRef] [PubMed]
- Fluge, Ø.; Risa, K.; Lunde, S.; Alme, K.; Rekeland, I.G.; Sapkota, D.; Kristoffersen, E.K.; Sørland, K.; Bruland, O.; Dahl, O.; et al. B-Lymphocyte Depletion in Myalgic Encephalopathy/ Chronic Fatigue Syndrome. An Open-Label Phase II Study with Rituximab Maintenance Treatment. PLoS ONE 2015, 10, e0129898. [Google Scholar] [CrossRef] [PubMed]
- Arora, T.; Grey, I.; Östlundh, L.; Lam, K.B.H.; Omar, O.M.; Arnone, D. The Prevalence of Psychological Consequences of COVID-19: A Systematic Review and Meta-Analysis of Observational Studies. J. Health Psychol. 2022, 27, 805–824. [Google Scholar] [CrossRef] [PubMed]
- Di Filippo, P.; Attanasi, M.; Dodi, G.; Porreca, A.; Raso, M.; di Pillo, S.; Chiarelli, F. Evaluation of Sleep Quality and Anxiety in Italian Pediatric Healthcare Workers during the First Wave of COVID-19 Pandemic. BMC Res. Notes 2021, 14, 219. [Google Scholar] [CrossRef] [PubMed]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An Investigation of Mental Health Status of Children and Adolescents in China during the Outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112–118. [Google Scholar] [CrossRef]
- Laura, V.-S.; Javier, F.; Miguel, A.V. Psychological Wellbeing of Vulnerable Children during the COVID-19 Pandemic. Psicothema 2020, 32, 501–507. [Google Scholar]
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lu, L. Mental Health Considerations for Children Quarantined Because of COVID-19. Lancet Child. Adolesc. Health 2020, 4, 347–349. [Google Scholar] [CrossRef] [Green Version]
- Pisano, L.; Galimi, G.; Cerniglia, L. A Qualitative Report on Exploratory Data on the Possible Emotional/Behavioral Correlates of COVID-19 Lockdown in 4-10 Years Children in Italy. Psychology, 2020; preprint. [Google Scholar] [CrossRef]
- Hughes, S.E.; Haroon, S.; Subramanian, A.; McMullan, C.; Aiyegbusi, O.L.; Turner, G.M.; Jackson, L.; Davies, E.H.; Frost, C.; McNamara, G.; et al. Development and Validation of the Symptom Burden Questionnaire for Long COVID (SBQ-LC): Rasch Analysis. BMJ 2022, 37, e070230. [Google Scholar] [CrossRef]
- O’Connor, R.J.; Preston, N.; Parkin, A.; Makower, S.; Ross, D.; Gee, J.; Halpin, S.J.; Horton, M.; Sivan, M. The COVID-19 Yorkshire Rehabilitation Scale (C19-YRS): Application and Psychometric Analysis in a Post-COVID-19 Syndrome Cohort. J. Med. Virol. 2022, 94, 1027–1034. [Google Scholar] [CrossRef]
- Liu, K.; Zhang, W.; Yang, Y.; Zhang, J.; Li, Y.; Chen, Y. Respiratory Rehabilitation in Elderly Patients with COVID-19: A Randomized Controlled Study. Complement. Ther. Clin. Pract. 2020, 39, 101166. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sansone, F.; Pellegrino, G.M.; Caronni, A.; Bonazza, F.; Vegni, E.; Lué, A.; Bocci, T.; Pipolo, C.; Giusti, G.; Di Filippo, P.; et al. Long COVID in Children: A Multidisciplinary Review. Diagnostics 2023, 13, 1990. https://doi.org/10.3390/diagnostics13121990
Sansone F, Pellegrino GM, Caronni A, Bonazza F, Vegni E, Lué A, Bocci T, Pipolo C, Giusti G, Di Filippo P, et al. Long COVID in Children: A Multidisciplinary Review. Diagnostics. 2023; 13(12):1990. https://doi.org/10.3390/diagnostics13121990
Chicago/Turabian StyleSansone, Francesco, Giulia Michela Pellegrino, Antonio Caronni, Federica Bonazza, Elena Vegni, Alberto Lué, Tommaso Bocci, Carlotta Pipolo, Giuliano Giusti, Paola Di Filippo, and et al. 2023. "Long COVID in Children: A Multidisciplinary Review" Diagnostics 13, no. 12: 1990. https://doi.org/10.3390/diagnostics13121990







