Focus on the Most Common Paucisymptomatic Vasculopathic Population, from Diagnosis to Secondary Prevention of Complications
Abstract
:1. Introduction
2. Relevant Sections
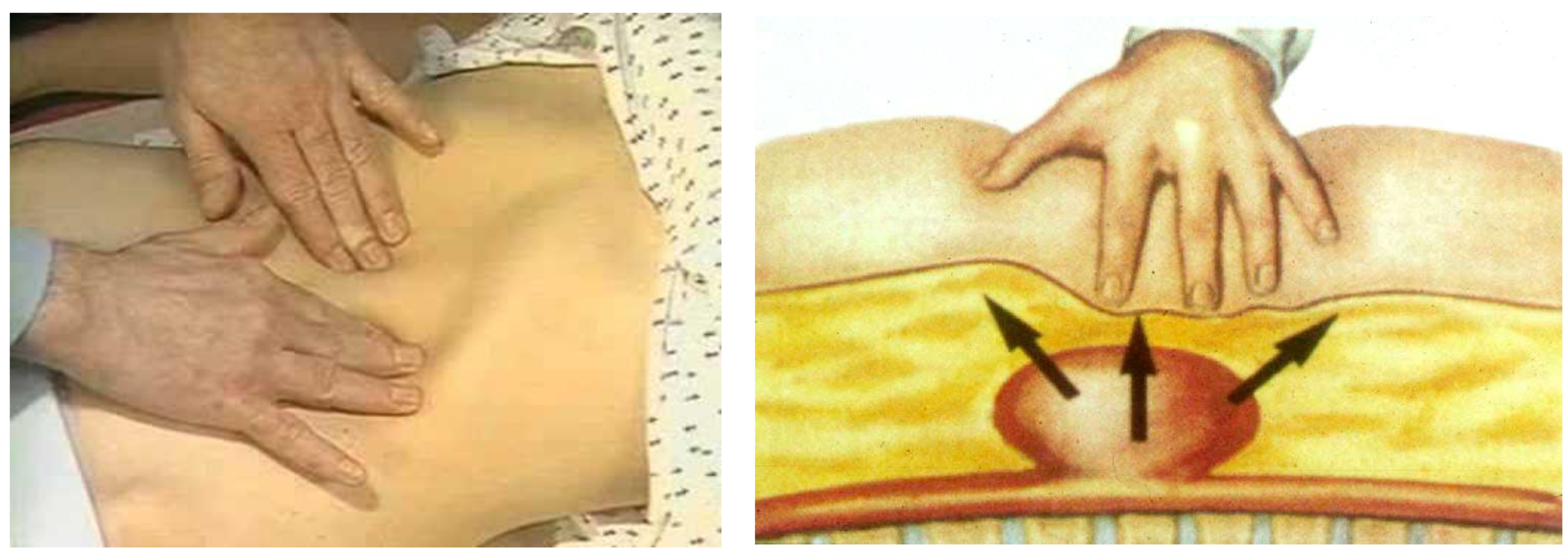
2.1. Abdominal Aortic Aneurysm (AAA)
- (1)
- Who to screen and how to screen for AAA?
- (2)
- How to prevent rAAAs?
2.2. Extracranial Internal Carotid Stenosis (EICS)
- (1)
- For whom and how to screen for EICS?
- (2)
- How to prevent an ischemic stroke of EICS origin?
2.3. Lower Extremity Arterial Disease (LEAD)
- (1)
- Who and how to screen for LEAD?
- -
- -
- The 30–50% of patients who have an atypical symptomatology due to the co-existence of other diseases, such as disc herniation, medullary stenosis, vertebral osteoarthritis, and peripheral neuropathy [52].
- (2)
- How to prevent MACE and MALE (CLTI, ALI, and amputation)?
2.4. Popliteal Artery Aneurysm (PAA)
- (1)
- Who and how to screen for PAA to?
- (2)
- How to prevent thromboembolism from PAA and rupture?
2.5. Renal Artery Stenosis (RAS)
- (1)
- Who and how to screen for RAS?
- (2)
- How to prevent complications from RVH, end-stage renal failure, and kidney loss?
2.6. Prevertebral Subclavian Artery Stenosis (PSAS)
- (1)
- Who and how to screen for PSAS?
- (2)
- How to prevent complications from PSAS?
3. Conclusions
4. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johnston, K.W.; Rutherford, R.B.; Tilson, M.D.; Shah, D.M.; Hollier, L.; Stanley, J.C. Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. J. Vasc. Surg. 1991, 13, 452–458. [Google Scholar] [CrossRef] [Green Version]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reimerink, J.J.; van der Laan, M.J.; Koelemay, M.J.; Balm, R.; Legemate, D.A. Systematic review and meta-analysis of population-based mortality from ruptured abdominal aortic aneurysm. Br. J. Surg. 2013, 100, 1405–1413. [Google Scholar] [CrossRef] [PubMed]
- Kumar, Y.; Hooda, K.; Li, S.; Goyal, P.; Gupta, N.; Adeb, M. Abdominal aortic aneurysm: Pictorial review of common appearances and complications. Ann. Transl. Med. 2017, 5, 256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakalihasan, N.; Michel, J.B.; Katsargyris, A.; Kuivaniemi, H.; Defraigne, J.O.; Nchimi, A.; Powell, J.T.; Yoshimura, K.; Hultgren, R. Abdominal aortic aneurysms. Nat. Rev. Dis. Primers 2018, 4, 34. [Google Scholar] [CrossRef] [PubMed]
- Benson, R.A.; Meecham, L.; Fisher, O.; Loftus, I.M. Ultrasound screening for abdominal aortic aneurysm: Current practice, challenges and controversies. Br. J. Radiol. 2018, 91, 20170306. [Google Scholar] [CrossRef] [PubMed]
- Carino, D.; Sarac, T.P.; Ziganshin, B.A.; Elefteriades, J.A. Abdominal Aortic Aneurysm: Evolving Controversies and Uncertainties. Int. J. Angiol. 2018, 27, 58–80. [Google Scholar] [CrossRef]
- Wanhainen, A.; Verzini, F.; Van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Corrigendum to ‘European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms’ [European Journal of Vascular & Endovascular Surgery 57/1 (2019) 8-93]. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 494. [Google Scholar] [CrossRef] [Green Version]
- Guirguis-Blake, J.M.; Beil, T.L.; Senger, C.A.; Coppola, E.L. Primary Care Screening for Abdominal Aortic Aneurysm: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2019, 322, 2219–2238. [Google Scholar] [CrossRef] [Green Version]
- Bains, P.; Oliffe, J.L.; Mackay, M.H.; Kelly, M.T. Screening Older Adult Men for Abdominal Aortic Aneurysm: A Scoping Review. Am. J. Mens Health 2021, 15, 15579883211001204. [Google Scholar] [CrossRef]
- Lederle, F.A. The Last (Randomized) Word on Screening for Abdominal Aortic Aneurysms. JAMA Intern. Med. 2016, 176, 1767–1768. [Google Scholar] [CrossRef] [PubMed]
- Johansson, M.; Zahl, P.H.; Siersma, V.; Jørgensen, K.J.; Marklund, B.; Brodersen, J. Benefits and harms of screening men for abdominal aortic aneurysm in Sweden: A registry-based cohort study. Lancet 2018, 391, 2441–2447. [Google Scholar] [CrossRef] [PubMed]
- Olchanski, N.; Winn, A.; Cohen, J.T.; Neumann, P.J. Abdominal aortic aneurysm screening: How many life years lost from underuse of the medicare screening benefit? J. Gen. Intern. Med. 2014, 29, 1155–1161. [Google Scholar] [CrossRef] [Green Version]
- Kapila, V.; Jetty, P.; Wooster, D.; Vucemilo, V.; Dubois, L.; Canadian Society for Vascular Surgery. Screening for abdominal aortic aneurysms in Canada: 2020 review and position statement of the Canadian Society for Vascular Surgery. Can. J. Surg. 2021, 64, E461–E466. [Google Scholar] [CrossRef] [PubMed]
- Joergensen, T.M.; Christensen, K.; Lindholt, J.S.; Larsen, L.A.; Green, A.; Houlind, K. Editor’s Choice-High Heritability of Liability to Abdominal Aortic Aneurysms: A Population Based Twin Study. Eur. J. Vasc. Endovasc. Surg. 2016, 52, 41–46. [Google Scholar] [CrossRef] [Green Version]
- Wanhainen, A.; Lundkvist, J.; Bergqvist, D.; Björck, M. Cost-effectiveness of screening women for abdominal aortic aneurysm. J. Vasc. Surg. 2006, 43, 908–914. [Google Scholar] [CrossRef] [Green Version]
- Hultgren, R.; Fattahi, N.; Nilsson, O.; Svensjö, S.; Roy, J.; Linne, A. Evaluating feasibility of using national registries for identification, invitation, and ultrasound examination of persons with hereditary risk for aneurysm disease-detecting abdominal aortic aneurysms in first degree relatives (adult offspring) to AAA patients (DAAAD). Pilot Feasibility Stud. 2022, 8, 252. [Google Scholar] [CrossRef]
- Kristensen, J.S.S.; Obel, L.M.; Dahl, M.; Høgh, A.L.; Lindholt, J.S. Gender-specific predicted normal aortic size and its consequences of the population-based prevalence of abdominal aortic aneurysms. Ann. Vasc. Surg. 2023, 91, 127–134. [Google Scholar] [CrossRef]
- Phillips, A.R.; Andraska, E.A.; Reitz, K.M.; Habib, S.; Martinez-Meehan, D.; Dai, Y.; Johnson, A.E.; Liang, N.L. Association between neighborhood deprivation and presenting with a ruptured abdominal aortic aneurysm before screening age. J. Vasc. Surg. 2022, 76, 932–941.e2. [Google Scholar] [CrossRef]
- Savolainen, H.; Novak, J.; Dick, F.; Widmer, M.K.; Carrel, T.; Schmidli, J.; Meier, B. Prevention of rupture of abdominal aortic aneurysm. Scand. J. Surg. 2010, 99, 217–220. [Google Scholar] [CrossRef] [Green Version]
- Svensjö, S.; Björck, M.; Wanhainen, A. Editor’s choice: Five-year outcomes in men screened for abdominal aortic aneurysm at 65 years of age: A population-based cohort study. Eur. J. Vasc. Endovasc. Surg. 2014, 47, 37–44. [Google Scholar] [CrossRef] [Green Version]
- Ashton, H.A.; Buxton, M.J.; Day, N.E.; Kim, L.G.; Marteau, T.M.; Scott, R.A.; Thompson, S.G.; Walker, N.M.; Multicentre Aneurysm Screening Study Group. The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: A randomised controlled trial. Lancet 2002, 360, 1531–1539. [Google Scholar] [CrossRef]
- Wild, J.B.; Stather, P.W.; Biancari, F.; Choke, E.C.; Earnshaw, J.J.; Grant, S.W.; Hafez, H.; Holdsworth, R.; Juvonen, T.; Lindholt, J.; et al. A multicentre observational study of the outcomes of screening detected sub-aneurysmal aortic dilatation. Eur. J. Vasc. Endovasc. Surg. 2013, 45, 128–134. [Google Scholar] [CrossRef] [Green Version]
- Keisler, B.; Carter, C. Abdominal aortic aneurysm. Am. Fam. Physician 2015, 91, 538–543. [Google Scholar]
- Chun, K.C.; Anderson, R.C.; Smothers, H.C.; Sood, K.; Irwin, Z.T.; Wilson, M.D.; Lee, E.S. Risk of developing an abdominal aortic aneurysm after ectatic aorta detection from initial screening. J. Vasc. Surg. 2020, 71, 1913–1919. [Google Scholar] [CrossRef]
- Sweeting, M.J.; Thompson, S.G.; Brown, L.C.; Powell, J.T.; RESCAN Collaborators. Meta-analysis of individual patient data to examine factors affecting growth and rupture of small abdominal aortic aneurysms. Br. J. Surg. 2012, 99, 655–665. [Google Scholar] [CrossRef]
- Arboix, A.; Oliveres, M.; Massons, J.; Pujades, R.; Garcia-Eroles, L. Early differentiation of cardioembolic from atherothrombotic cerebral infarction: A multivariate analysis. Eur. J. Neurol. 1999, 6, 677–683. [Google Scholar] [CrossRef]
- Chaturvedi, S.; Bruno, A.; Feasby, T.; Holloway, R.; Benavente, O.; Cohen, S.N.; Cote, R.; Hess, D.; Saver, J.; Spence, J.D.; et al. Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Carotid endarterectomy–An evidence-based review: Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2005, 65, 794–801. [Google Scholar] [CrossRef] [Green Version]
- de Weerd, M.; Greving, J.P.; Hedblad, B.; Lorenz, M.W.; Mathiesen, E.B.; O’Leary, D.H.; Rosvall, M.; Sitzer, M.; Buskens, E.; Bots, M.L. Prevalence of asymptomatic carotid artery stenosis in the general population: An individual participant data meta-analysis. Stroke 2010, 41, 1294–1297. [Google Scholar] [CrossRef] [Green Version]
- AbuRahma, A.F.; Avgerinos, E.D.; Chang, R.W.; Darling, R.C., 3rd; Duncan, A.A.; Forbes, T.L.; Malas, M.B.; Murad, M.H.; Perler, B.A.; Powell, R.J.; et al. Society for Vascular Surgery clinical practice guidelines for management of extracranial cerebrovascular disease. J. Vasc. Surg. 2022, 75, 4S–22S. [Google Scholar] [CrossRef]
- Stroke Prevention and Educational Awareness Diffusion (SPREAD). Available online: http://www.iso-spread.it/capitoli/LINEE_GUIDA_SPREAD_8a_EDIZIONE.pdf (accessed on 30 May 2022).
- Wu, C.M.; McLaughlin, K.; Lorenzetti, D.L.; Hill, M.D.; Manns, B.J.; Ghali, W.A. Early risk of stroke after transient ischemic attack: A systematic review and meta-analysis. Arch. Intern. Med. 2007, 167, 2417–2422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hui, W.; Wu, C.; Zhao, W.; Sun, H.; Hao, J.; Liang, H.; Wang, X.; Li, M.; Jadhav, A.P.; Han, Y.; et al. Efficacy and Safety of Recanalization Therapy for Acute Ischemic Stroke with Large Vessel Occlusion: A Systematic Review. Stroke 2020, 51, 2026–2035. [Google Scholar] [CrossRef]
- Sharifpour, M.; Moore, L.E.; Shanks, A.M.; Didier, T.J.; Kheterpal, S.; Mashour, G.A. Incidence, predictors, and outcomes of perioperative stroke in noncarotid major vascular surgery. Anesth. Analg. 2013, 116, 424–434. [Google Scholar] [CrossRef]
- National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar]
- Dobs, A.S.; Nieto, F.J.; Szklo, M.; Barnes, R.; Sharrett, A.R.; Ko, W.J. Risk factors for popliteal and carotid wall thicknesses in the Atherosclerosis Risk in Communities (ARIC) Study. Am. J. Epidemiol. 1999, 150, 1055–1067. [Google Scholar] [CrossRef]
- Smith, N.L.; Barzilay, J.I.; Shaffer, D.; Savage, P.J.; Heckbert, S.R.; Kuller, L.H.; Kronmal, R.A.; Resnick, H.E.; Psaty, B.M. Fasting and 2-hour postchallenge serum glucose measures and risk of incident cardiovascular events in the elderly: The Cardiovascular Health Study. Arch. Intern. Med. 2002, 162, 209–216. [Google Scholar] [CrossRef] [Green Version]
- Wolff, T.; Miller, T.; Ko, S. Aspirin for the primary prevention of cardiovascular events: An update of the evidence for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2009, 150, 405–410. [Google Scholar] [CrossRef]
- Antithrombotic Trialists’ (ATT) Collaboration; Baigent, C.; Blackwell, L.; Collins, R.; Emberson, J.; Godwin, J.; Peto, R.; Buring, J.; Hennekens, C.; Kearney, P.; et al. Aspirin in the primary and secondary prevention of vascular disease: Collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009, 373, 1849–1860. [Google Scholar] [CrossRef] [Green Version]
- Abbott, A.L. Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: Results of a systematic review and analysis. Stroke 2009, 40, e573–e583. [Google Scholar] [CrossRef] [Green Version]
- Silvennoinen, H.M.; Ikonen, S.; Soinne, L.; Railo, M.; Valanne, L. CT angiographic analysis of carotid artery stenosis: Comparison of manual assessment, semiautomatic vessel analysis, and digital subtraction angiography. Am. J. Neuroradiol. 2007, 28, 97–103. [Google Scholar]
- Adla, T.; Adlova, R. Multimodality imaging of carotid stenosis. Int. J. Angiol. 2015, 24, 179–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bir, S.C.; Kelley, R.E. Carotid atherosclerotic disease: A systematic review of pathogenesis and management. Brain Circ. 2022, 8, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Saxena, A.; Ng, E.Y.; Lim, S.T. Imaging modalities to diagnose carotid artery stenosis: Progress and prospect. Biomed. Eng. Online 2019, 18, 66. [Google Scholar] [CrossRef] [Green Version]
- Kolodgie, F.D.; Yahagi, K.; Mori, H.; Romero, M.E.; Trout HHRd Finn, A.V.; Virmani, R. High-risk carotid plaque: Lessons learned from histopathology. Semin. Vasc. Surg. 2017, 30, 31–43. [Google Scholar] [CrossRef]
- Kamtchum-Tatuene, J.; Noubiap, J.J.; Wilman, A.H.; Saqqur, M.; Shuaib, A.; Jickling, G.C. Prevalence of high-risk plaques and risk of stroke in patients with asymptomatic carotid stenosis: A meta-analysis. JAMA Neurol. 2020, 77, 1524–1535. [Google Scholar] [CrossRef]
- Heart Protection Study Collaborative Group. Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20,536 high-risk individuals: A randomised controlled trial. Lancet 2011, 378, 2013–2020. [Google Scholar] [CrossRef] [Green Version]
- Gabel, J.; Jabo, B.; Patel, S.; Kiang, S.; Bianchi, C.; Chiriano, J.; Teruya, T.; Abou-Zamzam, A.M., Jr. Vascular Quality Initiative. Analysis of Patients Undergoing Major Lower Extremity Amputation in the Vascular Quality Initiative. Ann. Vasc. Surg. 2018, 46, 75–82. [Google Scholar] [CrossRef]
- Fowkes, F.G.; Rudan, D.; Rudan, I.; Aboyans, V.; Denenberg, J.O.; McDermott, M.M.; Norman, P.E.; Sampson, U.K.; Williams, L.J.; Mensah, G.A.; et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 2013, 382, 1329–1340. [Google Scholar] [CrossRef]
- Grøndal, N.; Søgaard, R.; Lindholt, J.S. Baseline prevalence of abdominal aortic aneurysm, peripheral arterial disease and hypertension in men aged 65-74 years from a population screening study (VIVA trial). Br. J. Surg. 2015, 102, 902–906. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.B.; Bartelink, M.E.L.; Björck, M.; Brodmann, M.; Cohnert, T.; Collet, J.P.; Czerny, M.; De Carlo, M. ESC Scientific Document Group. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: The European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur. Heart J. 2018, 39, 763–816. [Google Scholar] [CrossRef] [Green Version]
- Frank, U.; Nikol, S.; Belch, J.; Boc, V.; Brodmann, M.; Carpentier, P.H.; Chraim, A.; Canning, C.; Dimakakos, E.; Gottsäter, A. ESVM Guideline on peripheral arterial disease. VASA 2019, 48 (Suppl. 102), 1–79. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care 2003, 26, 3333–3341. [Google Scholar] [CrossRef] [Green Version]
- Leng, G.C.; Lee, A.J.; Fowkes, F.G.; Lowe, G.D.; Housley, E. The relationship between cigarette smoking and cardiovascular risk factors in peripheral arterial disease compared with ischaemic heart disease. The Edinburgh Artery Study. Eur. Heart J. 1995, 16, 1542–1548. [Google Scholar] [CrossRef]
- Howard, D.P.; Banerjee, A.; Fairhead, J.F.; Hands, L.; Silver, L.E.; Rothwell, P.M.; Oxford Vascular Study. Population-Based Study of Incidence, Risk Factors, Outcome, and Prognosis of Ischemic Peripheral Arterial Events: Implications for Prevention. Circulation 2015, 132, 1805–1815. [Google Scholar] [CrossRef]
- Tsimikas, S.; Karwatowska-Prokopczuk, E.; Gouni-Berthold, I.; Tardif, J.C.; Baum, S.J.; Steinhagen-Thiessen, E.; Shapiro, M.D.; Stroes, E.S.; Moriarty, P.M.; Nordestgaard, B.G.; et al. Lipoprotein(a) Reduction in Persons with Cardiovascular Disease. N. Engl. J. Med. 2020, 382, 244–255. [Google Scholar] [CrossRef]
- Wassel, C.L.; Loomba, R.; Ix, J.H.; Allison, M.A.; Denenberg, J.O.; Criqui, M.H. Family history of peripheral artery disease is associated with prevalence and severity of peripheral artery disease: The San Diego population study. J. Am. Coll. Cardiol. 2011, 58, 1386–1392. [Google Scholar] [CrossRef] [Green Version]
- Surma, S.; Banach, M. Fibrinogen and Atherosclerotic Cardiovascular Diseases-Review of the Literature and Clinical Studies. Int. J. Mol. Sci. 2021, 23, 193. [Google Scholar] [CrossRef]
- Serra, R.; Bracale, U.M.; Ielapi, N.; Del Guercio, L.; Di Taranto, M.D.; Sodo, M.; Michael, A.; Faga, T.; Bevacqua, E.; Jiritano, F.; et al. The Impact of Chronic Kidney Disease on Peripheral Artery Disease and Peripheral Revascularization. Int. J. Gen. Med. 2021, 14, 3749–3759. [Google Scholar] [CrossRef]
- Criqui, M.H.; Matsushita, K.; Aboyans, V.; Hess, C.N.; Hicks, C.W.; Kwan, T.W.; McDermott, M.M.; Misra, S.; Ujueta, F.; American Heart Association Council on Epidemiology and Prevention; et al. Lower Extremity Peripheral Artery Disease: Contemporary Epidemiology, Management Gaps, and Future Directions: A Scientific Statement from the American Heart Association. Circulation 2021, 144, e171–e191. [Google Scholar] [CrossRef]
- Amirhamzeh, M.M.; Chant, H.J.; Rees, J.L.; Hands, L.J.; Powell, R.J.; Campbell, W.B. A comparative study of treadmill tests and heel raising exercise for peripheral arterial disease. Eur. J. Vasc. Endovasc. Surg. 1997, 13, 301–305. [Google Scholar] [CrossRef] [Green Version]
- Chung, W.K.; Erion, K.; Florez, J.C.; Hattersley, A.T.; Hivert, M.F.; Lee, C.G.; McCarthy, M.I.; Nolan, J.J.; Norris, J.M.; Pearson, E.R. Precision Medicine in Diabetes: A Consensus Report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2020, 43, 1617–1635. [Google Scholar] [CrossRef] [PubMed]
- Oyama, K.; Giugliano, R.P.; Blazing, M.A.; Park, J.G.; Tershakovec, A.M.; Sabatine, M.S.; Cannon, C.P.; Braunwald, E. Baseline Low-Density Lipoprotein Cholesterol and Clinical Outcomes of Combining Ezetimibe with Statin Therapy in IMPROVE-IT. J. Am. Coll. Cardiol. 2021, 78, 1499–1507. [Google Scholar] [CrossRef] [PubMed]
- Anand, S.S.; Bosch, J.; Eikelboom, J.W.; Connolly, S.J.; Diaz, R.; Widimsky, P.; Aboyans, V.; Alings, M.; Kakkar, A.K.; Keltai, K.; et al. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: An international, randomised, double-blind, placebo-controlled trial. Lancet 2018, 391, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Aboyans, V.; Bauersachs, R.; Mazzolai, L.; Brodmann, M.; Palomares, J.F.R.; Debus, S.; Collet, J.P.; Drexel, H.; Espinola-Klein, C.; Lewis, B.S.; et al. Antithrombotic therapies in aortic and peripheral arterial diseases in 2021: A consensus document from the ESC working group on aorta and peripheral vascular diseases, the ESC working group on thrombosis, and the ESC working group on cardiovascular pharmacotherapy. Eur. Heart J. 2021, 42, 4013–4024. [Google Scholar] [CrossRef] [PubMed]
- Martelli, E.; Ippoliti, A.; Ventoruzzo, G.; De Vivo, G.; Ascoli Marchetti, A.; Pistolese, G.R. Popliteal artery aneurysms. Factors associated with thromboembolism and graft failure. Int. Angiol. 2004, 23, 54–65. [Google Scholar]
- Kropman, R.H.; Schrijver, A.M.; Kelder, J.C.; Moll, F.L.; de Vries, J.P. Clinical outcome of acute leg ischaemia due to thrombosed popliteal artery aneurysm: Systematic review of 895 cases. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 452–457. [Google Scholar] [CrossRef] [Green Version]
- Farber, A.; Angle, N.; Avgerinos, E.; Dubois, L.; Eslami, M.; Geraghty, P.; Haurani, M.; Jim, J.; Ketteler, E.; Pulli, R.; et al. The Society for Vascular Surgery clinical practice guidelines on popliteal artery aneurysms. J. Vasc. Surg. 2022, 75, 109S–120S. [Google Scholar] [CrossRef]
- Tuveson, V.; Löfdahl, H.E.; Hultgren, R. Patients with abdominal aortic aneurysm have a high prevalence of popliteal artery aneurysms. Vasc. Med. 2016, 21, 369–375. [Google Scholar] [CrossRef] [Green Version]
- Tsilimparis, N.; Dayama, A.; Ricotta, J.J., 2nd. Open and endovascular repair of popliteal artery aneurysms: Tabular review of the literature. Ann. Vasc. Surg. 2013, 27, 259–265. [Google Scholar] [CrossRef]
- Vrijenhoek, J.E.; Mackaay, A.J.; Moll, F.L. Small popliteal artery aneurysms: Important clinical consequences and contralateral survey in daily vascular surgery practice. Ann. Vasc. Surg. 2013, 27, 454–458. [Google Scholar] [CrossRef]
- Magee, R.; Quigley, F.; McCann, M.; Buttner, P.; Golledge, J. Growth and risk factors for expansion of dilated popliteal arteries. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 606–611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartz, C.J.; White, T.A. Stenosis of renal artery: An unselected necropsy study. Br. Med. J. 1964, 2, 1415–1421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Safian, R.D.; Textor, S.C. Renal-artery stenosis. N. Engl. J. Med. 2001, 344, 431–442. [Google Scholar] [CrossRef]
- Messerli, F.H.; Bangalore, S.; Makani, H.; Rimoldi, S.F.; Allemann, Y.; White, C.J.; Textor, S.; Sleight, P. Flash pulmonary oedema and bilateral renal artery stenosis: The Pickering syndrome. Eur. Heart J. 2011, 32, 2231–2235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zierler, R.E.; Bergelin, R.O.; Davidson, R.C.; Cantwell-Gab, K.; Polissar, N.L.; Strandness, D.E., Jr. A prospective study of disease progression in patients with atherosclerotic renal artery stenosis. Am. J. Hypertens. 1996, 9, 1055–1061. [Google Scholar] [CrossRef]
- Dai, Z.; Zhang, X. Pathophysiology and Clinical Impacts of Chronic Kidney Disease on Coronary Artery Calcification. J. Cardiovasc. Dev. Dis. 2023, 10, 207. [Google Scholar] [CrossRef]
- Mousa, A.Y.; AbuRahma, A.F.; Bozzay, J.; Broce, M.; Bates, M. Update on intervention versus medical therapy for atherosclerotic renal artery stenosis. J. Vasc. Surg. 2015, 61, 1613–1623. [Google Scholar] [CrossRef] [Green Version]
- Cooper, C.J.; Murphy, T.P.; Cutlip, D.E.; Jamerson, K.; Henrich, W.; Reid, D.M.; Cohen, D.J.; Matsumoto, A.H.; Steffes, M.; Jaff, M.R.; et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N. Engl. J. Med. 2014, 370, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Chrysochou, C.; Foley, R.N.; Young, J.F.; Khavandi, K.; Cheung, C.M.; Kalra, P.A. Dispelling the myth: The use of renin-angiotensin blockade in atheromatous renovascular disease. Nephrol. Dial. Transpl. 2012, 27, 1403–1409. [Google Scholar] [CrossRef] [Green Version]
- English, J.A.; Carell, E.S.; Guidera, S.A.; Tripp, H.F. Angiographic prevalence and clinical predictors of left subclavian stenosis in patients undergoing diagnostic cardiac catheterization. Catheter Cardiovasc. Interv. 2001, 54, 8–11. [Google Scholar] [CrossRef]
- Przewlocki, T.; Kablak-Ziembicka, A.; Pieniazek, P.; Musialek, P.; Kadzielski, A.; Zalewski, J.; Kozanecki, A.; Tracz, W. Determinants of immediate and long-term results of subclavian and innominate artery angioplasty. Catheter Cardiovasc. Interv. 2006, 67, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Aboyans, V.; Criqui, M.H.; McDermott, M.M.; Allison, M.A.; Denenberg, J.O.; Shadman, R.; Fronek, A. The vital prognosis of subclavian stenosis. J. Am. Coll. Cardiol. 2007, 49, 1540–1545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osborn, L.A.; Vernon, S.M.; Reynolds, B.; Timm, T.C.; Allen, K. Screening for subclavian artery stenosis in patients who are candidates for coronary bypass surgery. Catheter Cardiovasc. Interv. 2002, 56, 162–165. [Google Scholar] [CrossRef] [PubMed]















Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martelli, E.; Enea, I.; Zamboni, M.; Federici, M.; Bracale, U.M.; Sangiorgi, G.; Martelli, A.R.; Messina, T.; Settembrini, A.M. Focus on the Most Common Paucisymptomatic Vasculopathic Population, from Diagnosis to Secondary Prevention of Complications. Diagnostics 2023, 13, 2356. https://doi.org/10.3390/diagnostics13142356
Martelli E, Enea I, Zamboni M, Federici M, Bracale UM, Sangiorgi G, Martelli AR, Messina T, Settembrini AM. Focus on the Most Common Paucisymptomatic Vasculopathic Population, from Diagnosis to Secondary Prevention of Complications. Diagnostics. 2023; 13(14):2356. https://doi.org/10.3390/diagnostics13142356
Chicago/Turabian StyleMartelli, Eugenio, Iolanda Enea, Matilde Zamboni, Massimo Federici, Umberto M. Bracale, Giuseppe Sangiorgi, Allegra R. Martelli, Teresa Messina, and Alberto M. Settembrini. 2023. "Focus on the Most Common Paucisymptomatic Vasculopathic Population, from Diagnosis to Secondary Prevention of Complications" Diagnostics 13, no. 14: 2356. https://doi.org/10.3390/diagnostics13142356
APA StyleMartelli, E., Enea, I., Zamboni, M., Federici, M., Bracale, U. M., Sangiorgi, G., Martelli, A. R., Messina, T., & Settembrini, A. M. (2023). Focus on the Most Common Paucisymptomatic Vasculopathic Population, from Diagnosis to Secondary Prevention of Complications. Diagnostics, 13(14), 2356. https://doi.org/10.3390/diagnostics13142356








