Appendiceal Signet Ring Cell Carcinoma: An Atypical Cause of Acute Appendicitis—A Case Study and Review of Current Knowledge
Abstract
1. Introduction
2. Case Presentation
3. Discussion
3.1. Signet Ring Cell Carcinoma: A Rare and Aggressive Form of Appendiceal Cancer
3.2. Demographic Patterns of ASRCC: Age, Sex, and Racial Disparities
3.3. Pathogenesis and Genetic Associations of ASRCC
3.4. Challenges in the Clinical Diagnosis of ASRCC: Overlapping Symptoms and Delayed Recognition
3.5. Imaging and Diagnostic Challenges in Preoperative Evaluation of Appendiceal Neoplasms: Distinguishing Malignant Lesions from Acute Appendicitis
3.6. Immunohistochemical Staining in the Diagnosis of ASRCC
3.7. Poor Prognosis of ASRCC: High Prevalence of Distant Metastases and Low Survival Rates
3.8. Appendiceal Signet Ring Cell Carcinoma: Heterogeneous Presentation, Management, and Outcomes—Insights from Case Reports and Studies
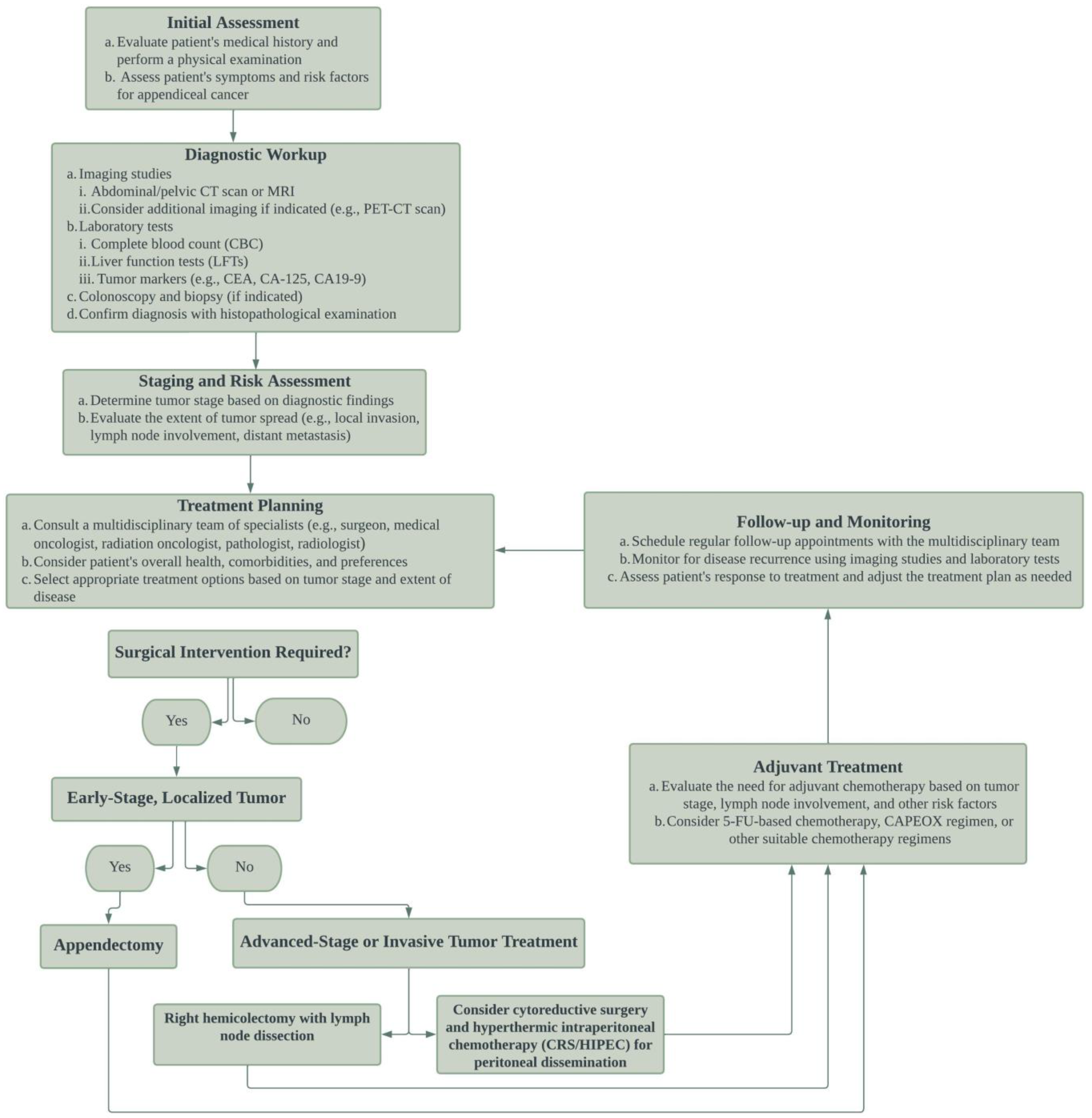
3.9. Individualized Management of ASRCC: Surgical Approaches, Adjuvant Therapy, and Controversies
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Enblad, M.; Egerszegi, P.P.; Birgisson, H.; Sjöblom, T.; Glimelius, B.; Folkesson, J. Signet Ring Cell Colorectal and Appendiceal Cancer: A Small Signet Ring Cell Component Is Also Associated with Poor Outcome. Cancers 2023, 15, 2497. [Google Scholar] [CrossRef]
- Cho, Y.J.; Kim, H.J.; Jang, S.K.; Yeon, J.W.; Kim, K.-H.; Paik, S.Y. Signet-ring cell carcinoma of the appendix: A case report with an emphasis on sonographic findings. Ultrasonography 2016, 35, 164–167. [Google Scholar] [CrossRef]
- Bu, Z.; Zheng, Z.; Li, Z.; Wu, X.; Zhang, L.; Wu, A.; Zong, X.; Ji, J. Clinicopathological and prognostic differences between mucinous gastric carcinoma and signet-ring cell carcinoma. Chin. J. Cancer Res. 2013, 25, 32–38. [Google Scholar] [CrossRef]
- Terada, T. An Immunohistochemical Study of Primary Signet-Ring Cell Carcinoma of the Stomach and Colorectum: Iii. Expressions of Ema, Cea, Ca19-9, Cdx-2, P53, Ki-67 Antigen, Ttf-1, Vimentin, and P63 in Normal Mucosa and in 42 Cases. Int. J. Clin. Exp. Pathol. 2013, 6, 630–638. [Google Scholar]
- Fusari, M.; Sorrentino, N.; Bottazzi, E.C.; Del Vecchio, W.; Cozzolino, I.; Maurea, S.; Salvatore, M.; Imbriaco, M. Primary signet ring cell carcinoma of the appendix mimicking acute appendicitis. Acta Radiol. Short Rep. 2012, 1, 1–3. [Google Scholar] [CrossRef]
- Sato, A.; Sato, Y.; Hiruta, N.; Oshiro, T.; Yoshida, Y.; Urita, T.; Kitahara, T.; Kadoya, K.; Nabekura, T.; Moriyama, Y.; et al. Signet-Ring Cell Carcinoma of the Appendix with Ganglioneuromatosis: A Case Report. Surg. Case Rep. 2022, 8, 151. [Google Scholar] [CrossRef]
- Benesch, M.G.; Mathieson, A. Epidemiology of Signet Ring Cell Adenocarcinomas. Cancers 2020, 12, 1544. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a popula-tion-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- Vincenti, L.; Andriola, V.; Cazzato, G.; Colagrande, A.; Fiore, F. Goblet Cell Carcinoma of the Appendix with Synchronous Adenocarcinoma of the Cecum: Distinct or Related Entities? Diseases 2022, 10, 77. [Google Scholar] [CrossRef]
- Hoehn, R.S.; Caroline, J.; Rieser, M.; Choudry, H.; Melnitchouk, N.; Hechtman, J.; Bahary, N. Current Management of Appendiceal Neoplasms. Am. Soc. Clin. Oncol. Educ. Book 2021, 41, 118–132. [Google Scholar] [CrossRef]
- Kelly, K.J. Management of Appendix Cancer. Clin. Colon Rectal Surg. 2015, 28, 247–255. [Google Scholar] [CrossRef]
- Chen, G.; Chen, K.; Sahyoun, L.; Zaman, S.; Protiva, P. Appendiceal adenocarcinoma is associated with better prognosis than cecal adenocarcinoma: A population-based comparative survival study. BMJ Open Gastroenterol. 2023, 10, e001045. [Google Scholar] [CrossRef] [PubMed]
- McCusker, M.E.; Coté, T.R.; Clegg, L.X.; Sobin, L.H. Primary Malignant Neoplasms of the Appendix: A Popula-tion-Based Study from the Surveillance, Epidemiology and End-Results Program, 1973–1998. Cancer 2002, 94, 3307–3312. [Google Scholar] [CrossRef] [PubMed]
- Petras, R.E.; Frankel, W.L. Chapter 23—Large Intestine (Colon). In Modern Surgical Pathology, 2nd ed.; Weidner, N., Richard, J., Cote, S.S., Weiss, L.M., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2009; pp. 755–836. [Google Scholar]
- Ko, Y.H.; Jung, C.-K.; Oh, S.N.; Kim, T.H.; Won, H.S.; Kang, J.H.; Kim, H.J.; Kang, W.K.; Oh, S.T.; Hong, Y.S. Primary signet ring cell carcinoma of the appendix: A rare case report and our 18-year experience. World J. Gastroenterol. 2008, 14, 5763–5768. [Google Scholar] [CrossRef]
- Caesar-Peterson, S.; Tulla, K.; Southall, C.; Lin, Y.; Genelus-Dominique, E. A rare case of signet ring cell carcinoma of the appendix. J. Surg. Case Rep. 2020, 2020, rjaa139. [Google Scholar] [CrossRef]
- Wei, Q.; Wang, X.; Gao, J.; Li, J.; Li, J.; Qi, C.; Li, Y.; Li, Z.; Shen, L. Clinicopathologic and Molecular Features of Colorectal Adenocarcinoma with Signet-Ring Cell Component. PLoS ONE 2016, 11, e0156659. [Google Scholar] [CrossRef]
- Heinen, C.D. Mismatch repair defects and Lynch syndrome: The role of the basic scientist in the battle against cancer. DNA Repair 2016, 38, 127–134. [Google Scholar] [CrossRef]
- Hatch, Q.M.; Gilbert, E.W. Appendiceal Neoplasms. Clin. Colon Rectal Surg. 2018, 31, 278–287. [Google Scholar] [CrossRef]
- Stein, S.; Raymond, D.O.B. Appendiceal Adenocarcinoma Presenting as Perforated Appendicitis. Cureus 2021, 13, e13578. [Google Scholar] [CrossRef]
- Zhou, M.-L.; Yan, F.-H.; Xu, P.-J.; Zhang, L.-J.; Li, Q.-H.; Ji, Y. Mucinous cystadenoma of the appendix: CT findings. Chin. Med. J. 2006, 119, 1300–1303. [Google Scholar] [CrossRef]
- Madwed, D.; Mindelzun, R.; Jeffrey, R.B.; Madwed, R.M.A.R.B.J.D.; Wang, H.; Chen, Y.-Q.; Wei, R.; Wang, Q.-B.; Song, B.; Wang, C.-Y.; et al. Mucocele of the appendix: Imaging findings. Am. J. Roentgenol. 1992, 159, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.; Park, H.; Lee, Y.R.; Kook, S.H.; Kim, S.K.; Kwag, H.J.; Chung, E.C. The Most Useful Findings for Diagnosing Acute Appendicitis on Contrast-Enhanced Helical Ct. Acta Radiol. 2003, 44, 574–582. [Google Scholar] [CrossRef]
- Pickhardt, P.J.; Levy, A.D.; Rohrmann, C.A., Jr.; Kende, A.I. Primary Neoplasms of the Appendix Manifesting as Acute Appendicitis: Ct Findings with Pathologic Comparison. Radiology 2002, 224, 775–781. [Google Scholar] [CrossRef] [PubMed]
- El Hussein, S.; Khader, S.N. Primary signet ring cell carcinoma of the pancreas: Cytopathology review of a rare entity. Diagn. Cytopathol. 2019, 47, 1314–1320. [Google Scholar] [CrossRef]
- Bellizzi, A.M. An Algorithmic Immunohistochemical Approach to Define Tumor Type and Assign Site of Origin. Adv. Anat. Pathol. 2020, 27, 114–163. [Google Scholar] [CrossRef] [PubMed]
- Ruoff, C.; Hanna, L.; Zhi, W.; Shahzad, G.; Gotlieb, V.; Saif, M.W. Cancers of the Appendix: Review of the Literatures. ISRN Oncol. 2011, 2011, 1–6. [Google Scholar] [CrossRef]
- McGory, M.L.; Maggard, M.A.; Kang, H.; O’Connell, J.B.; Ko, C.Y. Malignancies of the Appendix: Beyond Case Series Reports. Dis. Colon Rectum 2005, 48, 2264–2271. [Google Scholar] [CrossRef]
- Wang, F.; Yi, T.; Liu, Y.; Tang, G. Primary signet ring cell carcinoma of the appendix: An interesting case. Am. J. Med. Sci. 2022, 364, e10–e11. [Google Scholar] [CrossRef]
- Vukovic, J.; Cindro, P.V.; Tomic, S.; Tonkic, A. Signet Ring Carcinoma of the Appendix Presenting as Crohn’s Disease in a Young Male. Case Rep. Gastroenterol. 2018, 12, 277–285. [Google Scholar] [CrossRef]
- Kulkarni, R.V.; Ingle, S.B.; Siddiqui, S. Primary signet ring cell carcinoma of the appendix: A rare case report. World J. Clin. Cases 2015, 3, 538–541. [Google Scholar] [CrossRef]
- Suzuki, J.; Kazama, S.; Kitayama, J.; Uozaki, H.; Miyata, T.; Nagawa, H. Signet ring cell carcinoma of the appendix manifesting as colonic obstruction and ovarian tumors: Report of a case. Surg. Today 2009, 39, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Abushalha, K.; Tuqan, W.E.; Albagoush, S.A.; Abulaimoun, S.; Silberstein, P.T. Clinicopathologic Features and Survival Outcomes of Signet Ring Cell Carcinoma of the Appendix: An Analysis of the Surveillance, Epidemiology, and End Results Database. Cureus 2020, 12, e8549. [Google Scholar] [CrossRef] [PubMed]
- Hugen, N.; Verhoeven, R.H.; E Lemmens, V.; van Aart, C.J.; Elferink, M.A.; Radema, S.A.; Nagtegaal, I.D.; de Wilt, J.H. Colorectal signet-ring cell carcinoma: Benefit from adjuvant chemotherapy but a poor prognostic factor. Int. J. Cancer 2015, 136, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Kolla, B.C.; Petersen, A.; Chengappa, M.; Gummadi, T.; Ganesan, C.; Gaertner, W.B.; Blaes, A. Impact of adjuvant chemotherapy on outcomes in appendiceal cancer. Cancer Med. 2020, 9, 3400–3406. [Google Scholar] [CrossRef]
- Strach, M.C.; Sutherland, S.; Horvath, L.G.; Mahon, K. The role of chemotherapy in the treatment of advanced appendiceal cancers: Summary of the literature and future directions. Ther. Adv. Med. Oncol. 2022, 14, 17588359221112478. [Google Scholar] [CrossRef] [PubMed]
- Flood, M.P.; Roberts, G.; Mitchell, C.; Ramsay, R.; Michael, M.; Heriot, A.G.; Kong, J.C. Impact of Neoadjuvant Sys-temic Chemotherapy Followed by Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy for Appen-diceal Adenocarcinoma. Asia Pac. J. Clin. Oncol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Munoz-Zuluaga, C.; Sardi, A.; King, M.C.; Nieroda, C.; Sittig, M.; MacDonald, R.; Gushchin, V. Outcomes in Peritoneal Dissemination from Signet Ring Cell Carcinoma of the Appendix Treated with Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy. Ann. Surg. Oncol. 2018, 26, 473–481. [Google Scholar] [CrossRef]

| Stage | Classification | ||
|---|---|---|---|
| Primary Tumor (T) | |||
| TX | Primary tumor cannot be assessed. | ||
| T0 | No evidence of primary tumor. | ||
| Tis | Carcinoma in situ refers to a condition where cancerous cells are present, but confined within the epithelial layer or the lamina propria. Specifically, the tumor remains restricted within the glandular basement membrane (intraepithelial) or within the lamina propria (intramucosal), and it does not extend through the muscularis mucosae into the submucosa. A new category, Tis (LAMN), has been introduced for low-grade appendiceal mucinous neoplasms. This category is used for those neoplasms that demonstrate a pushing margin but do not invade the muscularis propria. | ||
| T1 | Tumor invades the submucosa (through the muscularis mucosa but not into the muscularis propria). | ||
| T2 | Tumor invades the muscularis propria. | ||
| T3 | The tumor extends through the muscularis propria and invades into the subserosa or the mesoappendix. In this stage, acellular mucin or mucinous epithelium can be found within the subserosa. | ||
| T4 | The tumor breaches the visceral peritoneum, which may include the presence of mucinous peritoneal tumors within the right lower quadrant and/or direct invasion into other organs or structures. This stage also involves the presence of acellular mucin or mucinous epithelium in serosa. | ||
| T4a | Tumor invades through the visceral peritoneum, including the acellular mucin or mucinous epithelium involving the serosa of the appendix or serosa of the mesoappendix. | ||
| T4b | Tumor directly invades or adheres to adjacent organs or structures. | ||
| Regional lymph nodes (N) | |||
| NX | Regional lymph nodes cannot be assessed. | ||
| N0 | No regional lymph node metastasis (Note: regional lymph nodes include ileocolic nodes). | ||
| N1 | One to three regional lymph nodes are positive (tumor in lymph node measuring > 0.2 mm) or presence of tumor deposit(s) with negative lymph nodes. | ||
| N1a | One regional lymph node is positive. | ||
| N1b | Two or three regional lymph nodes are positive. | ||
| N1c | No regional lymph nodes are positive but there are tumor deposits in the subserosa or mesentery. | ||
| N2 | Four or more regional lymph nodes are positive. | ||
| Distant metastasis (M) | |||
| M0 | No distant metastasis. | ||
| M1 | Distant metastasis. | ||
| M1a | Presence of intraperitoneal acellular mucin. | ||
| M1b | Presence of intraperitoneal mucin with mucinous epithelium. | ||
| M1b | Nonperitoneal metastases. | ||
| Stage | T | N | M |
| Stage 0 | Tis | N0 | M0 |
| Stage I | T1 | N0 | M0 |
| T2 | N0 | M0 | |
| Stage IIA | T3 | N0 | M0 |
| Stage IIB | T4a | N0 | M0 |
| Stage IIC | T4b | N0 | M0 |
| Stage IIIA | T1 | N1 | M0 |
| T2 | N1 | M0 | |
| Stage IIIB | T3 | N1 | M0 |
| T4 | N1 | M0 | |
| Stage IIIC | any T | N2 | M0 |
| Stage IVA | any T | N0 | M1a |
| Stage IVB | any T | N1 | M1a |
| any T | N2 | M1a | |
| Stage IVC | any T | any N | M1b |
| Case Report/Study | Age/Gender | Clinical Presentation | Treatment | Prognosis | Key Takeaways |
|---|---|---|---|---|---|
| Sato A et al., 2022 [6] | 48/F * | Chronic abdominal pain, fullness, constipation, and diarrhea | Laparoscopic ileocecal resection, adjuvant chemotherapy (CAPOX) | Survived 2 years | Role of adjuvant chemotherapy in certain patients |
| Wang F et al., 2022 [29] | 66/F | Abdominal distension and discomfort | Refused surgical treatment, adjuvant chemotherapy | Survived 5 months | Early detection and prompt treatment |
| Caesar-Peterson S et al., 2020 [16] | 65/M * | Atypical abdominal pain | Appendectomy | N/A * | Early detection is crucial for improving outcomes |
| Vukovic J et al., 2018 [30] | 22/M | Vomiting, diarrhea, and cramps in abdomen | Right-sided hemicolectomy and diverting ileostomy | Died after 2 months | Importance of early diagnosis and intervention |
| Kulkarni RV et al., 2015 [31] | 45/F | Persistent right lower quadrant abdominal pain | Appendectomy and unilateral salphingo-oophorectomy | N/A | Multidisciplinary approach to management |
| Fusari M et al., 2012 [5] | 80/M | Acute appendicitis | Appendectomy and subsequent right hemicolectomy | N/A | Consider appendiceal cancer in acute appendicitis to plan appropriate treatment |
| Suzuki J et al., 2009 [32] | 66/F | Colonic obstruction and ovarian tumors | Hartmann’s operation, ileocecal resection, and bilateral salpingo-oophorectomy, refused postoperative chemotherapy | Survived 1 year | Importance of early recognition and appropriate surgical intervention |
| Ko YH et al., 2008 [15] | 67/F | Abdominal distention due to unresectable peritoneal dissemination and ovarian metastases | Appendectomy and bilateral salpingo-oophorectomy, palliative systemic chemotherapy (FOLFOX-4) | Survived 1 year | Consider appendiceal cancer in unexplained ascites |
| Present case | 65/F | Acute appendicitis | Appendectomy and subsequent right hemicolectomy, palliative systemic chemotherapy (5-fluorouracil (/leucovorin) | Survived 1 year | Accurate diagnosis and appropriate management are crucial for improving patient outcomes |
| Category | Key Findings and Considerations |
|---|---|
| Prevalence | -Rare; represents 4% of all appendiceal neoplasms |
| Age and Sex Distribution | -Mean age of occurrence: 62 years; male-to-female ratio: 1:11 |
| Clinical Presentation | -Symptoms often mimic acute appendicitis |
| -Possible atypical symptoms: weight loss, changes in bowel habits | |
| Histopathological Characteristics | -Malignant cells with abundant intracytoplasmic mucin |
| -Nucleus displaced to the periphery (signet ring appearance) | |
| -Immunohistochemical staining: CK20+, CDX-2+, CK7- | |
| Potential Pathogenesis | -Arising from genetic mutations in pluripotent intestinal crypt epithelial stem cells |
| Treatment Options | -Appendectomy for early stage disease |
| -Right hemicolectomy with regional lymphadenectomy for advanced disease or high-risk features | |
| -Cytoreductive surgery with HIPEC for peritoneal dissemination | |
| -Controversial role of adjuvant chemotherapy | |
| Prognostic Factors | -Advanced stage, lymph node involvement, lymphovascular/perineural invasion |
| -Positive resection margins, peritoneal dissemination | |
| -Poor, with a 5-year survival rate of 7%; high prevalence of distant metastases (60%) | |
| Diagnostic Challenges | -Nonspecific clinical presentation |
| -Overlap with acute appendicitis symptoms | |
| -Lack of specific CT findings, tumor spread to adjacent organs | |
| Management Strategies | -Early recognition and appropriate surgical intervention |
| -Multidisciplinary approach to management |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andjelkovic, B.; Stojanovic, B.; Stojanovic, M.D.; Milosevic, B.; Cvetkovic, A.; Spasic, M.; Jakovljevic, S.; Cvetkovic, D.; Stojanovic, B.S.; Milosev, D.; et al. Appendiceal Signet Ring Cell Carcinoma: An Atypical Cause of Acute Appendicitis—A Case Study and Review of Current Knowledge. Diagnostics 2023, 13, 2359. https://doi.org/10.3390/diagnostics13142359
Andjelkovic B, Stojanovic B, Stojanovic MD, Milosevic B, Cvetkovic A, Spasic M, Jakovljevic S, Cvetkovic D, Stojanovic BS, Milosev D, et al. Appendiceal Signet Ring Cell Carcinoma: An Atypical Cause of Acute Appendicitis—A Case Study and Review of Current Knowledge. Diagnostics. 2023; 13(14):2359. https://doi.org/10.3390/diagnostics13142359
Chicago/Turabian StyleAndjelkovic, Branko, Bojan Stojanovic, Milica Dimitrijevic Stojanovic, Bojan Milosevic, Aleksandar Cvetkovic, Marko Spasic, Stefan Jakovljevic, Danijela Cvetkovic, Bojana S. Stojanovic, Danijela Milosev, and et al. 2023. "Appendiceal Signet Ring Cell Carcinoma: An Atypical Cause of Acute Appendicitis—A Case Study and Review of Current Knowledge" Diagnostics 13, no. 14: 2359. https://doi.org/10.3390/diagnostics13142359
APA StyleAndjelkovic, B., Stojanovic, B., Stojanovic, M. D., Milosevic, B., Cvetkovic, A., Spasic, M., Jakovljevic, S., Cvetkovic, D., Stojanovic, B. S., Milosev, D., Mitrovic, M., & Stankovic, V. (2023). Appendiceal Signet Ring Cell Carcinoma: An Atypical Cause of Acute Appendicitis—A Case Study and Review of Current Knowledge. Diagnostics, 13(14), 2359. https://doi.org/10.3390/diagnostics13142359








